Abstract
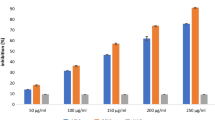
The increasing incidence of neurodegenerative diseases (NDDs) has stressed the need to develop new treatments. In this regard, alkaloids from medicinal plants are being identified and developed as inhibitors of acetylcholinesterase, other enzymes, and receptors associated with the onset of NDDs. Nardostachys jatamansi, a medicinal herb native to the Himalayan region and belonging to the Caprifoliaceae family, has long been used in Indian traditional medicine to treat neurobiological symptoms. In this study, we have isolated and identified the major alkaloids from N. jatamansi using LC–MS/MS analysis. The dried root extract of N. jatamansi contained actinidine and glaziovine as its major alkaloids. These compounds were identified using LC–MS/MS fragmentation pattern and purified by semi-preparative HPLC. The molecular docking analysis was performed for the purified alkaloids with 15 target proteins associated with NDDs pathology. Notably, actinidine and glaziovine showed better interaction energy with the acetylcholine esterase, VGF nerve growth factor, cyclin-dependent kinase, and glycogen synthase kinase when compared to the clinically used drugs memantine and tacrine. Glaziovine also showed better interaction energy when docking was performed with GluN1/GluN2B NMDA receptor, β-secretase, tyrosine phosphorylation regulation kinase, necrosis factor-kappa, adenosine A2A receptor, alpha-synuclein, beta-site amyloid precursor protein cleaving enzyme 1, c-Jun N terminal kinase, monoamine oxidase B, compared to tacrine, galantamine, and memantine. Furthermore, actinidine and glaziovine showed borderline cytotoxicity on PC12 and SH-SY 5Y cells with IC50 values ranging from 85.32 ± 0.87 μM, and 92.12 ± 0.56 μM, respectively, indicating that these alkaloids can be further developed as promising drug leads.




Similar content being viewed by others
Data availability
All data and materials are available upon request.
References
Slanzi A, Iannoto G, Rossi B, Zenaro E, Constantin G (2020) In vitro models of neurodegenerative diseases. Fron Cell Develop Bio 8:328. https://doi.org/10.3389/fcell.2020.00328
Moradi SZ, Momtaz S, Bayrami Z, Farzaei MH, Abdollahi M (2020) Nanoformulations of herbal extracts in treatment of neurodegenerative disorders. Front Bioeng Biotech 8:238. https://doi.org/10.3389/fbioe.2020.00238
Hussain R, Zubair H, Pursell S, Shahab M (2018) Neurodegenerative diseases: regenerative mechanisms and novel therapeutic approaches. Brain Sci 8:177. https://doi.org/10.3390/brainsci8090177
Nichols E, Steinmetz JD, Vollset SE, Fukutaki K, Chalek J, Abd-Allah F, Liu X (2022) Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the global burden of disease study 2019. Lanc Pub Healt 7:e105–e125. https://doi.org/10.1016/S2468-2667(21)00249-8
Kong YR, Tay KC, Su YX, Wong CK, Tan WN, Khaw KY (2021) Potential of naturally derived alkaloids as multi-targeted therapeutic agents for neurodegenerative diseases. Mol 26:728. https://doi.org/10.3390/molecules26030728
Venkateswaran V, Muralidharan S, Gopalakrishnan AV, Krishnan N, Velmurugan D, Raman P (2021) GC-MS analysis of guttation fluids from selected crop plants. J Crop Improve 1–15. https://doi.org/10.1080/15427528.2021.2018748
Pachaiappan R, Nagasathiya K, Singh PK, Gopalakrishnan AV, Velusamy P, Ramasamy K et al (2022) Phytochemical profile of black cumin (Nigella sativa L.) seed oil: identification of bioactive anti-pathogenic compounds for traditional Siddha formulation. Bio Conver Biorefin 1–13. https://doi.org/10.1007/s13399-022-02951-x
Boruta T (2021) A bioprocess perspective on the production of secondary metabolites by Streptomyces in submerged co-cultures. World J Micro Biotech 37:1–15. https://doi.org/10.1007/s11274-021-03141-z
De Lima BR, Lima JM, Maciel JB, Valentim CQ, Nunomura RD, Lima ES, Koolen HH, de Souza AD, Pinheiro ML, Cass QB, da Silva FM (2019) Synthesis and inhibition evaluation of new benzyltetrahydroprotoberberine alkaloids designed as acetylcholinesterase inhibitors. Front Chem 7:629. https://doi.org/10.3389/fchem.2019.00629
Kim KW, Yoon CS, Park SJ, Bae GS, Kim DG, Kim YC, Oh H (2021) Chemical analysis of the ingredients of 20% aqueous ethanol extract of Nardostachys jatamansi through phytochemical study and evaluation of anti-neuroinflammatory component. Evid Bas Complement Alternat Med 202–226. https://doi.org/10.1155/2021/5901653
Krishnan N, Devadasan V, Raman P (2020) Plant-derived alkaloids as anti-viral agents. Int J Res Pharma Sci 6174–6182. https://doi.org/10.26452/ijrps.v11i4.3291
Ng YP, Or TC, Ip NY (2015) Plant alkaloids as drug leads for Alzheimer’s disease. Neurochem Intern 89:260–270. https://doi.org/10.1016/j.neuint.2015.07.018
Sahoo AK, Dandapat J, Dash UC, Kanhar S (2018) Features and outcomes of drugs for combination therapy as multi-targets strategy to combat Alzheimer’s disease. J Ethnopharma 215:42–73. https://doi.org/10.1016/j.jep.2017.12.015
Fan J, Zhang K, Jin Y, Li B, Gao S, Zhu J, Cui R (2019) Pharmacological effects of berberine on mood disorders. J Cell Mol Med 23:21–8. https://doi.org/10.1111/jcmm.13930
Dhiman N, Bhattacharya A (2020) Nardostachys jatamansi—the challenges and opportunities of harnessing the untapped pharmaceutical resources. J Ethnopharmacol 246:112–211. https://doi.org/10.1016/j.jep.2019.112211
Liu QF, Jeon Y, Sung YW, Lee JH, Jeong H, Kim YM, Yun HS, Chin YW, Jeon S, Cho KS, Koo BS (2018) Nardostachys jatamansi ethanol extract ameliorates Aβ42 cytotoxicity. Bio Phar Bullet 41:470–477. https://doi.org/10.1248/bpb.b17-00750
Takemoto H, Ito M, Asada Y, Kobayashi Y (2015) Inhalation administration of the sesquiterpenoid aristolen-1 (10)-en-9-ol from Nardostachys chinensis has a sedative effect via the GABAergic system. Planta Med 81:343–347. https://doi.org/10.1055/s-0035-1545725
Joshi H, Parle M (2006) Nardostachys jatamansi improves learning and memory in mice. J Med Food 9:113–118. https://doi.org/10.1007/BF00988079
Di Francesco A, Zajc J, Gunde-Cimerman N, Aprea E, Gasperi F, Placì N et al (2020) Bioactivity of volatile organic compounds by Aureobasidium species against gray mold of tomato and table grape. World J Micro Biotech 36:1–11. https://doi.org/10.1007/s11274-020-02947-7
Li R, Wang ZM, Wang Y, Dong X, Zhang LH, Wang T, Zhu Y, Gao XM, Wu HH, Xu YT (2021) Antidepressant activities and regulative effects on serotonin transporter of Nardostachys jatamansi DC. J Ethnopharma 268:113601. https://doi.org/10.1016/j.jep.2020.113601
Velusamy P, Su CH, Ramasamy P, Arun V, Rajnish N, Raman P et al (2022) Volatile organic compounds as potential biomarkers for noninvasive disease detection by nanosensors: a comprehensive review. Crit Rev Analyt Chem 1–12. https://doi.org/10.1080/10408347.2022.2043145
Pilerood SA, Prakash J (2013) Nutritional and medicinal properties of valerian (Valeriana officinalis) herb: a review. Int J Food Nutri Diet 1:25–33
Parthasarathy S, Soundararajan P, Krishnan N, Karuppiah KM, Devadasan V, Prabhu D, Rajamanikandan S, Velusamy P, Gopinath SC, Raman P (2022) Detection of adulterants from common edible oils by GC–MS. Bio Conver Bioref 1–21. https://doi.org/10.1007/s13399-022-02913-3
Nirmal SA, Pal SC, Otimenyi SO, Aye T, Elachouri M, Kundu SK, Mandal SC (2013) Contribution of herbal products in global market. Pharma Rev 95–104
Singh V, Dubey P, Srivastava S, Rawat AKS (2011) Botanical standardization of the Jatamansi, their substitute and adulterant species. Indian J Tradit Knowl 10:599–603
Kayani WK, Kiani BH, Dilshad E, Mirza B (2018) Biotechnological approaches for artemisinin production in Artemisia. World J Micro Biotech 34:1–14. https://doi.org/10.1007/s11274-018-2432-9
Harborne JB (1984) Methods of plant analysis. Phytochem Meth 1–36
Krishnan N, Raman P, Mariappanadar V (2015) Simple mass spectrometric method for the estimation of boron and aluminum in water at the parts per billion level. Eur J Mas Spec 21:481–486. https://doi.org/10.1255/ejms.1349
De Andrade JP, Pigni NB, Torras-Claveria L, Berkov S, Codina C, Viladomat F, Bastida J (2012) Bioactive alkaloid extracts from Narcissus broussonetii: mass spectral studies. J Pharm Biomed Ana 70:13–25. https://doi.org/10.1016/j.jpba.2012.05.009
O'Boyle NM, Banck M, James CA, Morley C, Vandermeersch T, Hutchison GR (2011) Open babel: an open chemical toolbox. J Chem Inform 3:33
Schrodinger L (2009) Schrodinger Suite 2009, Glide version 5.5
Bathula R, Muddagoni N, Lanka G, Dasari M, Potlapally SR (2021) Glide docking, autodock, binding free energy and drug-likeness studies for prediction of potential inhibitors of cyclin-dependent kinase 14 protein in wnt signaling pathway. Biointer Res Appl Chem 12:2473–2488. https://doi.org/10.33263/BRIAC122.24732488
Pachaiappan R, Rajamuthu TP, Sarkar A, Natrajan P, Krishnan N, Sakthivelu M, Gopinath SC (2022) N-acyl-homoserine lactone mediated virulence factor (s) of Pseudomonas aeruginosa inhibited by flavonoids and isoflavonoids. Proc Biochem 116:84–93. https://doi.org/10.1016/j.procbio.2022.02.024
Zhang S, Duangjan C, Tencomnao T, Liu J, Lin J, Wink M (2020) Neuroprotective effects of oolong tea extracts against glutamate-induced toxicity in cultured neuronal cells and β-amyloid-induced toxicity in Caenorhabditis elegans. Food Func 11:8179–8192. https://doi.org/10.1039/D0FO01072C
Lima JM, Leme GM, Costa EV, Cass QB (2021) LC-HRMS and acetylcholinesterase affinity assay as a workflow for profiling alkaloids in Annona salzmannii extract. J Chromato 1164:122493. https://doi.org/10.1016/j.jchromb.2020.122493
Torssell K, Wahlberg KE (1967) Isolation, structure and synthesis of alkaloids from Valeriana officinalis L. Acta Chem Scand 21:53–62. https://doi.org/10.3891/acta.chem.scand.21-0053
Qiao K, Fang C, Chen B, Liu Z, Pan N, Peng H et al (2020) Molecular characterization, purification, and antioxidant activity of recombinant superoxide dismutase from the Pacific abalone Haliotis discus hannai Ino. World J Micro Biotech 36:1–14. https://doi.org/10.1007/s11274-020-02892-5
Levanon SS, Aharonovitz O, Maor-Shoshani A, Abraham G, Kenett D, Aloni Y (2018) An efficient method to control high mannose and core fucose levels in glycosylated antibody production using deoxymannojirimycin. J Biotech 276:54–62. https://doi.org/10.1016/j.jbiotec.2018.04.006
Gao K, Zheng C, Wang T, Zhao H, Wang J, Wang Z, Zhai X, Jia Z, Chen J, Zhou Y, Wang W (2006) 1-Deoxynojirimycin: occurrence, extraction, chemistry, oral pharmacokinetics, biological activities and in silico target fishing. Mol 21:1600. https://doi.org/10.3390/molecules21111600
Bol S, Caspers J, Buckingham L, Anderson-Shelton GD, Ridgway C, Buffington CA, Schulz S, Bunnik EM (2017) Responsiveness of cats (Felidae) to silver vine (Actinidia polygama), Tatarian honeysuckle (Lonicera tatarica), valerian (Valeriana officinalis) and catnip (Nepeta cataria). BMC Vet Res 13:1–6. https://doi.org/10.1186/s12917-017-0987-6
Prescott TA, Bramham J, Zompro O, Maciver SK (2009) Actinidine and glucose from the defensive secretion of the stick insect Megacrania nigrosulfurea. Biochem System Eco 37:759–760. https://doi.org/10.1016/j.bse.2009.11.002
Díaz-Godínez C, Ontiveros-Rodríguez JC, Ríos-Valencia DG, Herbert-Pucheta JE, Zepeda-Vallejo LG, Carrero JC (2020) Anti-amoebic activity of leaf extracts and aporphine alkaloids obtained from Annona purpurea. Planta Medica 86:425–33. https://doi.org/10.1055/a-1111-9566
Pérez EG, Sáez J, Cassels BK (2005) A convenient, renewable source of the anxiolytic proaporphine alkaloid glaziovine: Duguetia vallicola leaves. J Chilean Chem Soc 50:553–557. https://doi.org/10.4067/S0717-97072005000300005
Wang Z, Jiang W, Liu Y, Meng X, Su X, Cao M, Peng D (2021) Putative genes in alkaloid biosynthesis identified in Dendrobium officinale by correlating the contents of major bioactive metabolites with genes expression between protocorm-like bodies and leaves. BMC Genom 22:1–17. https://doi.org/10.1186/s12864-021-07887-6
Rocha PR, De Freitas FA, Angolini CF, Vasconcelos LSF, da Silva AL, Costa EV, Koolen HH (2018) Statistical mixture design investigation for extraction and quantitation of aporphine alkaloids from the leaves of Unonopsis duckei RE Fr. by HPLC–MS/MS. Phytochem Ana 29:569–576. https://doi.org/10.1002/pca.2768
Li HT, Li WJ, Wu HM, Chen CY (2012) Alkaloids from Cinnamomum philippinense. Nat Prod Com 7(12):1581–1582. https://doi.org/10.1177/1934578X1200701209
Huth A, Dettner K (1990) Defense chemicals from abdominal glands of 13 rove beetle species of sub tribe Staphylinina (Coleoptera: Staphylinidae, Staphylininae). J Chem Eco 16:2691–2711. https://doi.org/10.1007/BF00988079
Auda H, Juneja HR, Eisenbraun EJ, Waller GR, Kays WR, Appel HH (1967) Biosynthesis of methylcyclopentane monoterpenoids. I Skytanthus alkaloids. J Amer Chem Soc 89:2476–2482. https://doi.org/10.1021/ja00986a041
Patocka J, Jakl J (2010) Biomedically relevant chemical constituents of Valeriana officinalis. J Appl Biomedicine 8:11–18. https://doi.org/10.2478/v10136-009-0002-z
Gilbert B, Gilbert MEA, De Oliveira MM, Ribeiro O, Wenkert E, Wickberg B, Rapoport H (1964) The aporphine and isoquinolinedienone alkaloids of Ocotea glaziovii. J Am Chem Soc 86:694–696
Galeone M, Cacioli D, Moise G, Gherardi G, Quadro G (1981) Glaziovine as anti-ulcer a double blind short term controlled clinical trial in comparison with cimetidine. Cur Therap Res Clinic Exp 30:44–49
Cordell GA, Quinn-Beattie ML, Farnsworth NR (2001) The potential of alkaloids in drug discovery. Phytothera Res 15:183–205. https://doi.org/10.1002/ptr.890
Chang FR, Wei JL, Teng CM, Wu YC (1998) Antiplatelet aggregation constituents from Annona purpurea. J Nat Products 61:1457–61. https://doi.org/10.1021/np9800046
Cheng P, Ma YB, Yao SY, Zhang Q, Wang EJ, Yan MH, Zhang XM, Zhang FX, Chen JJ (2007) Two new alkaloids and active anti-hepatitis B virus constituents from Hypserpa nitida. Bioorg Med Chem Let 17:5316–20. https://doi.org/10.1016/j.bmcl.2007.08.027
Castro OC (1993) Chemical and biological extractives of Lauraceae species in Costa Rican tropical forests. In: Downum KR, Romeo JT, Stafford HA (eds) Phytochemical potential of tropical plants. Recent advances in phytochemistry, vol 27. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-1783-6_3
Amna U, Hasnan MH, Ahmad K, Abdul Manaf A, Awang K, Nafiah MA (2015) In vitro cytotoxic of aporphine and proaporphine alkaloids from Phoebe grandis (Ness) Merr. Int J Pharm Sci Rev Res 32:15–20
Meng XY, Zhang HX, Mezei M, Cui M (2011) Molecular docking: a powerful approach for structure-based drug discovery. Cur Com Aid Drug Design 7:146–157. https://doi.org/10.1248/bpb.b17-00750
Houghton PJ, Ren Y, Howes MJ (2006) Acetylcholinesterase inhibitors from plants and fungi. Nat Pro Rep 23:181–99. https://doi.org/10.1039/b508966m
Velmurugan D, Pachaiappan R, Ramakrishnan C (2020) Recent trends in drug design and discovery. Cur Top Med Chem 20:1761–1770. https://doi.org/10.2174/156802662066620062215003
Brown MR, Radford SE, Hewitt EW (2020) Modulation of β-amyloid fibril formation in Alzheimer’s disease by microglia and infection. Front Mol Neurosci 13:609073. https://doi.org/10.3389/fnmol.2020.609073
Sayad A, Najafi S, Hussen BM, Abdullah ST, Movahedpour A, Taheri M, Hajiesmaeili M (2022) The emerging roles of the β-Secretase BACE1 and the long non-coding RNA BACE1-AS in human diseases: a focus on neurodegenerative diseases and cancer. Fron Aging Neurosci 14:1–10. https://doi.org/10.3389/fnagi.2022.853180
Cai Z (2014) Monoamine oxidase inhibitors: promising therapeutic agents for Alzheimer’s disease. Mol Med Rep 9:1533–1541. https://doi.org/10.3892/mmr.2014.2040
Dumont M, Beal MF (2011) Neuroprotective strategies involving ROS in Alzheimer disease. Free Rad Bio Med 51:1014–26. https://doi.org/10.1016/j.freeradbiomed.2010.11.026
Parsons MP, Raymond LA (2014) Extrasynaptic NMDA receptor involvement in central nervous system disorders. Neuron 82:279–293. https://doi.org/10.1016/j.neuron.2014.03.030
Dansokho C, Heneka MT (2018) Neuroinflammatory responses in Alzheimer’s disease. J Neu Transm 125:771–9. https://doi.org/10.1007/s00702-017-1831-7
Nair JJ, Van SJ (2012) Acetylcholinesterase inhibition within the lycorine series of Amaryllidaceae alkaloids. Nat Prod Commun 7:959–962. https://doi.org/10.1177/1934578X1200700741
Acknowledgements
The authors gratefully acknowledge Dr. Mohinder Singh (Ministry of Ayush), District Nodal officer, State Medicinal Plant Board (SMDP) Himachal Pradesh, Shimla, India for providing the plant samples. We also thank the management of SRM Institute of Science and Technology, College of Engineering, and Department of Biotechnology for instrumentation facilities.
Author information
Authors and Affiliations
Contributions
Nagasathiya Krishnan: conceptualization, formal analysis, project administration, resources, supervision, investigation, funding acquisition, validation, writing original draft preparation, and writing-reviewing and editing. Vairamani Mariappanadar: resources, data curation, validation, visualization, and writing-reviewing and editing. Anantha Krishnan Dhanabalan: resources, validation, visualization, and writing-reviewing and editing. Velmurugan Devadasan: data curation, validation, visualization, and writing-reviewing and editing. Subash C. B. Gopinath: validation, visualization, and writing-reviewing and editing. Pachaiappan Raman: data curation, methodology, visualization, validation, writing original draft preparation, and writing-reviewing and editing.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Krishnan, N., Mariappanadar, V., Dhanabalan, A.K. et al. Purification, identification and in silico models of alkaloids from Nardostachys jatamansi — bioactive compounds for neurodegenerative diseases. Biomass Conv. Bioref. 13, 14889–14900 (2023). https://doi.org/10.1007/s13399-022-03237-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13399-022-03237-y