Abstract
Purpose
The aim of this study was to determine the effect of age on the psoas and posterior paraspinal muscles (PPM; multifidus muscle and erector spinae) and to evaluate potential sex-related differences.
Methods
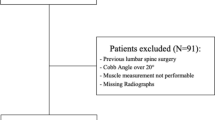
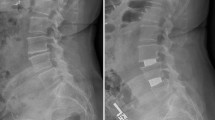
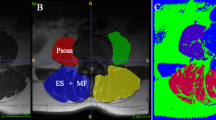
MRI-based quantitative assessments of the cross-sectional area (CSA), the functional cross-sectional area (fCSA), the fat area (FAT) and the proportion of intramuscular fat (FI) were conducted on patients undergoing lumbar fusion surgery between 2014 and 2021. The regions of interest were the psoas muscle and the PPM at the superior endplate of L4. The left and right sides of the muscle groups were summarized and normalized by the patient’s height (cm2/m2). The relationships between age and muscular parameters were analyzed stratified by sex.
Results
A total of 195 patients (57.9%female) with a median age of 64.2 years and a body mass index of 28.3 kg/m2 were analyzed. The CSAPsoas was 7.7 cm2/m2 and differed significantly between females and males (p < 0.001); likewise, the fCSAPsoas differed significantly between the sexes. The CSAPPM was 18.8 cm2/m2 with no sex-specific differences. Significant differences were found in the FIPPM (males: 41.1% vs. females: 47.9%; p < 0.001), but not in the FIPsoas (males: 3.7% vs. females: 4.5%; p = 0.276). Considering the effect of age on FI, a significant positive correlation was observed for the PPMs for both sexes. Only in women, there was a negative correlation between age and CSAPsoas (ρ = − 0.248; p = 0.008), FATPsoas (ρ = − 0.421; p < 0.001) and FIPsoas (ρ = − 0.371; p < 0.001).
Conclusion
This study demonstrated sex-specific differences in spinal muscle morphology in relation to patient age. With increasing age there was a decrease in FIPsoas in women only, unlike in the PPMs in which there was increased FI that was significantly higher in women compared to men.


Similar content being viewed by others
References
Driscoll T, Jacklyn G, Orchard J, Passmore E, Vos T, Freedman G, Lim S, Punnett L (2014) The global burden of occupationally related low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 73:975–981. https://doi.org/10.1136/annrheumdis-2013-204631
Smith E, Hoy DG, Cross M, Vos T, Naghavi M, Buchbinder R, Woolf AD, March L (2014) The global burden of other musculoskeletal disorders: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 73:1462–1469. https://doi.org/10.1136/annrheumdis-2013-204680
Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, Williams G, Smith E, Vos T, Barendregt J, Murray C, Burstein R, Buchbinder R (2014) The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 73:968–974. https://doi.org/10.1136/annrheumdis-2013-204428
Sebbag E, Felten R, Sagez F, Sibilia J, Devilliers H, Arnaud L (2019) The world-wide burden of musculoskeletal diseases: a systematic analysis of the World Health Organization Burden of Diseases Database. Ann Rheum Dis 78:844–848. https://doi.org/10.1136/annrheumdis-2019-215142
Roux CH, Guillemin F, Boini S, Longuetaud F, Arnault N, Hercberg S, Briancon S (2005) Impact of musculoskeletal disorders on quality of life: an inception cohort study. Ann Rheum Dis 64:606–611. https://doi.org/10.1136/ard.2004.020784
Maher C, Underwood M, Buchbinder R (2017) Non-specific low back pain. Lancet 389:736–747. https://doi.org/10.1016/S0140-6736(16)30970-9
Wieser S, Horisberger B, Schmidhauser S, Eisenring C, Brugger U, Ruckstuhl A, Dietrich J, Mannion AF, Elfering A, Tamcan O, Muller U (2011) Cost of low back pain in Switzerland in 2005. Eur J Health Econ 12:455–467. https://doi.org/10.1007/s10198-010-0258-y
Picavet HS, Struijs JN, Westert GP (2008) Utilization of health resources due to low back pain: survey and registered data compared. Spine (Phila Pa 1976) 33:436–444. https://doi.org/10.1097/BRS.0b013e318163e054
Wong AYL, Karppinen J, Samartzis D (2017) Low back pain in older adults: risk factors, management options and future directions. Scoliosis Spinal Disord 12:14. https://doi.org/10.1186/s13013-017-0121-3
Ranger TA, Cicuttini FM, Jensen TS, Peiris WL, Hussain SM, Fairley J, Urquhart DM (2017) Are the size and composition of the paraspinal muscles associated with low back pain? A systematic review. Spine J 17:1729–1748. https://doi.org/10.1016/j.spinee.2017.07.002
Goubert D, De Pauw R, Meeus M, Willems T, Cagnie B, Schouppe S, Van Oosterwijck J, Dhondt E, Danneels L (2017) Lumbar muscle structure and function in chronic versus recurrent low back pain: a cross-sectional study. Spine J 17:1285–1296. https://doi.org/10.1016/j.spinee.2017.04.025
Hildebrandt M, Fankhauser G, Meichtry A, Luomajoki H (2017) Correlation between lumbar dysfunction and fat infiltration in lumbar multifidus muscles in patients with low back pain. BMC Musculoskelet Disord 18:12. https://doi.org/10.1186/s12891-016-1376-1
D’Hooge R, Cagnie B, Crombez G, Vanderstraeten G, Dolphens M, Danneels L (2012) Increased intramuscular fatty infiltration without differences in lumbar muscle cross-sectional area during remission of unilateral recurrent low back pain. Man Ther 17:584–588. https://doi.org/10.1016/j.math.2012.06.007
Teichtahl AJ, Urquhart DM, Wang Y, Wluka AE, Wijethilake P, O’Sullivan R, Cicuttini FM (2015) Fat infiltration of paraspinal muscles is associated with low back pain, disability, and structural abnormalities in community-based adults. Spine J 15:1593–1601. https://doi.org/10.1016/j.spinee.2015.03.039
Ranger TA, Cicuttini FM, Jensen TS, Heritier S, Urquhart DM (2019) Paraspinal muscle cross-sectional area predicts low back disability but not pain intensity. Spine J 19:862–868. https://doi.org/10.1016/j.spinee.2018.12.004
Dallaway A, Kite C, Griffen C, Duncan M, Tallis J, Renshaw D, Hattersley J (2020) Age-related degeneration of the lumbar paravertebral muscles: systematic review and three-level meta-regression. Exp Gerontol 133:110856. https://doi.org/10.1016/j.exger.2020.110856
Marcus RL, Addison O, Kidde JP, Dibble LE, Lastayo PC (2010) Skeletal muscle fat infiltration: impact of age, inactivity, and exercise. J Nutr Health Aging 14:362–366. https://doi.org/10.1007/s12603-010-0081-2
Dahlqvist JR, Vissing CR, Hedermann G, Thomsen C, Vissing J (2017) Fat replacement of paraspinal muscles with aging in healthy adults. Med Sci Sports Exerc 49:595–601. https://doi.org/10.1249/MSS.0000000000001119
Goubert D, Oosterwijck JV, Meeus M, Danneels L (2016) Structural changes of lumbar muscles in non-specific low back pain: a systematic review. Pain Physician 19:E985–E1000
Kalichman L, Carmeli E, Been E (2017) The association between imaging parameters of the paraspinal muscles, spinal degeneration, and low back pain. Biomed Res Int 2017:2562957. https://doi.org/10.1155/2017/2562957
Pernik MN, Hicks WH, Akbik OS, Nguyen ML, Luu I, Traylor JI, Deme PR, Dosselman LJ, Hall K, Wingfield SA, Aoun SG, Bagley CA (2022) Psoas muscle index as a predictor of perioperative outcomes in geriatric patients undergoing spine surgery. Global Spine J. https://doi.org/10.1177/21925682211072626
Hirase T, Haghshenas V, Bratescu R, Dong D, Kuo PH, Rashid A, Kavuri V, Hanson DS, Meyer BC, Marco RAW (2021) Sarcopenia predicts perioperative adverse events following complex revision surgery for the thoracolumbar spine. Spine J 21:1001–1009. https://doi.org/10.1016/j.spinee.2021.02.001
Tee YS, Cheng CT, Wu YT, Kang SC, Derstine BA, Fu CY, Liao CH, Su GL, Wang SC, Hsieh CH (2021) The psoas muscle index distribution and influence of outcomes in an Asian adult trauma population: an alternative indicator for sarcopenia of acute diseases. Eur J Trauma Emerg Surg 47:1787–1795. https://doi.org/10.1007/s00068-020-01360-x
Kurumisawa S, Kawahito K (2019) The psoas muscle index as a predictor of long-term survival after cardiac surgery for hemodialysis-dependent patients. J Artif Organs 22:214–221. https://doi.org/10.1007/s10047-019-01108-4
Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, Gerig G (2006) User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 31:1116–1128. https://doi.org/10.1016/j.neuroimage.2006.01.015
Otsu N (1979) A threshold selection method from gray-level histograms. IEEE Trans Syst Man Cybern 9:62–66. https://doi.org/10.1109/TSMC.1979.4310076
Moser M, Adl Amini D, Jones C, Zhu J, Okano I, Oezel L, Chiapparelli E, Tan ET, Shue J, Sama AA, Cammisa FP, Girardi FP, Hughes AP (2022) The predictive value of psoas and paraspinal muscle parameters measured on MRI for severe cage subsidence after standalone lateral lumbar interbody fusion. Spine J. https://doi.org/10.1016/j.spinee.2022.03.009
Gladstone JN, Bishop JY, Lo IK, Flatow EL (2007) Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med 35:719–728. https://doi.org/10.1177/0363546506297539
Wong AYL, Harada G, Lee R, Gandhi SD, Dziedzic A, Espinoza-Orias A, Parnianpour M, Louie PK, Basques B, An HS, Samartzis D (2021) Preoperative paraspinal neck muscle characteristics predict early onset adjacent segment degeneration in anterior cervical fusion patients: a machine-learning modeling analysis. J Orthop Res 39:1732–1744. https://doi.org/10.1002/jor.24829
Kim JY, Ryu DS, Paik HK, Ahn SS, Kang MS, Kim KH, Park JY, Chin DK, Kim KS, Cho YE, Kuh SU (2016) Paraspinal muscle, facet joint, and disc problems: risk factors for adjacent segment degeneration after lumbar fusion. Spine J 16:867–875. https://doi.org/10.1016/j.spinee.2016.03.010
Kirkland JL, Tchkonia T, Pirtskhalava T, Han J, Karagiannides I (2002) Adipogenesis and aging: does aging make fat go MAD? Exp Gerontol 37:757–767. https://doi.org/10.1016/s0531-5565(02)00014-1
Talbot J, Maves L (2016) Skeletal muscle fiber type: using insights from muscle developmental biology to dissect targets for susceptibility and resistance to muscle disease. Wiley Interdiscip Rev Dev Biol 5:518–534. https://doi.org/10.1002/wdev.230
Lemieux S, Prud’homme D, Bouchard C, Tremblay A, Despres JP (1993) Sex differences in the relation of visceral adipose tissue accumulation to total body fatness. Am J Clin Nutr 58:463–467. https://doi.org/10.1093/ajcn/58.4.463
Janssen I, Heymsfield SB, Wang ZM, Ross R (2000) Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J Appl Physiol 89:81–88. https://doi.org/10.1152/jappl.2000.89.1.81
Sions JM, Elliott JM, Pohlig RT, Hicks GE (2017) Trunk muscle characteristics of the Multifidi, Erector Spinae, Psoas, and Quadratus Lumborum in older adults with and without chronic low back pain. J Orthop Sports Phys Ther 47:173–179. https://doi.org/10.2519/jospt.2017.7002
Haizlip KM, Harrison BC, Leinwand LA (2015) Sex-based differences in skeletal muscle kinetics and fiber-type composition. Physiology (Bethesda) 30:30–39. https://doi.org/10.1152/physiol.00024.2014
Brown LM, Clegg DJ (2010) Central effects of estradiol in the regulation of food intake, body weight, and adiposity. J Steroid Biochem Mol Biol 122:65–73. https://doi.org/10.1016/j.jsbmb.2009.12.005
Staron RS, Hagerman FC, Hikida RS, Murray TF, Hostler DP, Crill MT, Ragg KE, Toma K (2000) Fiber type composition of the vastus lateralis muscle of young men and women. J Histochem Cytochem 48:623–629. https://doi.org/10.1177/002215540004800506
Mannion AF, Dumas GA, Cooper RG, Espinosa FJ, Faris MW, Stevenson JM (1997) Muscle fibre size and type distribution in thoracic and lumbar regions of erector spinae in healthy subjects without low back pain: normal values and sex differences. J Anat 190(Pt 4):505–513. https://doi.org/10.1046/j.1469-7580.1997.19040505.x
Sirca A, Kostevc V (1985) The fibre type composition of thoracic and lumbar paravertebral muscles in man. J Anat 141:131–137
Arbanas J, Klasan GS, Nikolic M, Jerkovic R, Miljanovic I, Malnar D (2009) Fibre type composition of the human psoas major muscle with regard to the level of its origin. J Anat 215:636–641. https://doi.org/10.1111/j.1469-7580.2009.01155.x
Wan Q, Lin C, Li X, Zeng W, Ma C (2015) MRI assessment of paraspinal muscles in patients with acute and chronic unilateral low back pain. Br J Radiol 88:20140546. https://doi.org/10.1259/bjr.20140546
Battie MC, Niemelainen R, Gibbons LE, Dhillon S (2012) Is level- and side-specific multifidus asymmetry a marker for lumbar disc pathology? Spine J 12:932–939. https://doi.org/10.1016/j.spinee.2012.08.020
Seyedhoseinpoor T, Taghipour M, Dadgoo M, Sanjari MA, Takamjani IE, Kazemnejad A, Khoshamooz Y, Hides J (2022) Alteration of lumbar muscle morphology and composition in relation to low back pain: a systematic review and meta-analysis. Spine J 22:660–676. https://doi.org/10.1016/j.spinee.2021.10.018
Crawford RJ, Filli L, Elliott JM, Nanz D, Fischer MA, Marcon M, Ulbrich EJ (2016) Age- and level-dependence of fatty infiltration in lumbar paravertebral muscles of healthy volunteers. AJNR Am J Neuroradiol 37:742–748. https://doi.org/10.3174/ajnr.A4596
Shahidi B, Parra CL, Berry DB, Hubbard JC, Gombatto S, Zlomislic V, Allen RT, Hughes-Austin J, Garfin S, Ward SR (2017) Contribution of lumbar spine pathology and age to paraspinal muscle size and fatty infiltration. Spine (Phila Pa 1976) 42:616–623. https://doi.org/10.1097/brs.0000000000001848
Hunter GR, Gower BA, Kane BL (2010) Age related shift in visceral fat. Int J Body Compos Res 8:103–108
Zhang P, Peterson M, Su GL, Wang SC (2015) Visceral adiposity is negatively associated with bone density and muscle attenuation. Am J Clin Nutr 101:337–343. https://doi.org/10.3945/ajcn.113.081778
Hung CS, Lee JK, Yang CY, Hsieh HR, Ma WY, Lin MS, Liu PH, Shih SR, Liou JM, Chuang LM, Chen MF, Lin JW, Wei JN, Li HY (2014) Measurement of visceral fat: should we include retroperitoneal fat? PLoS ONE 9:e112355. https://doi.org/10.1371/journal.pone.0112355
Swainson MG, Batterham AM, Hind K (2020) Age- and sex-specific reference intervals for visceral fat mass in adults. Int J Obes (Lond) 44:289–296. https://doi.org/10.1038/s41366-019-0393-1
Faron A, Luetkens JA, Schmeel FC, Kuetting DLR, Thomas D, Sprinkart AM (2019) Quantification of fat and skeletal muscle tissue at abdominal computed tomography: associations between single-slice measurements and total compartment volumes. Abdom Radiol (NY) 44:1907–1916. https://doi.org/10.1007/s00261-019-01912-9
Acknowledgements
Dr. Sama reports royalties from Ortho Development, Corp.; private investments for Vestia Ventures MiRUS Investment, LLC, IVY II, LLC, ISPH 3, LLC, and VBros Venture Partners X Centinel Spine; consulting fee from Clariance, Inc., Kuros Biosciences AG, and Medical Device Business Service, Inc.; speaking and teaching arrangements of DePuy Synthes Products, Inc.; membership of scientific advisory board of Clariance, Inc., and Kuros Biosciences AG; and trips/travel of Medical Device Business research support from Spinal Kinetics, Inc., outside the submitted work. Dr. Cammisa reports royalties from NuVasive, Inc. Accelus; private investments for 4WEB Medical/4WEB, Inc., Bonovo Orthopedics, Inc., Healthpoint Capital Partners, LP, ISPH II, LLC, ISPH 3 Holdings, LLC, Ivy Healthcare Capital Partners, LLC, Medical Device Partners II, LLC, Medical Device Partners III, LLC, Orthobond Corporation, Spine Biopharma, LLC, Synexis, LLC, Tissue Differentiation Intelligence, LLC, VBVP VI, LLC, VBVP X, LLC (Centinel) and Woven Orthopedics Technologies; consulting fees from 4WEB Medical/4WEB, Inc., DePuy Synthes Spine, NuVasive, Inc., Spine Biopharma, LLC, and Synexis, LLC, Accelus; membership of scientific advisory board/other office of Healthpoint Capital Partners, LPIVY, Medical Device Partners III, LLC, Orthobond Corporation, Spine Biopharma, LLC, Synexis, LLC, and Woven Orthopedic Technologies; and research support from 4WEB Medical/4WEB, Inc., Mallinckrodt Pharmaceuticals, Camber Spine, and Centinel Spine, outside the submitted work. Dr. Girardi reports royalties from Lanx, Inc., and Ortho Development Corp.; private investments for Centinel Spine, and BCMID; stock ownership of Healthpoint Capital Partners, LP; and consulting fees from NuVasive, Inc., and DePuy Synthes Spine, outside the submitted work. Dr. Hughes reports research support from NuVasive, Inc. and Kuros Biosciences AG; and fellowship support from NuVasive, Inc. and Kuros Biosciences AG, outside the submitted work.
Funding
Research reported in this publication was supported by the National Center for Advancing Translational Science of the National Institute of Health Under Award Number UL1TR002384.
Author information
Authors and Affiliations
Contributions
M contributed to conception and design. M, C, H, M, and AA performed acquisition of data. M and H carried out analysis and interpretation of data. M drafted the article. All authors critically revised the article and reviewed submitted version of manuscript. H performed study supervision and approved the final version of the manuscript on behalf of all authors. M and Z performed statistical analysis. T, C, and S provided administrative/technical/material support.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding this work.
Ethical approval
The institutional review board of the Hospital for Special Surgery approved this study. The investigation was approved by the institutional review board (IRB 2019-2137).
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The work was performed at the Hospital for Special Surgery, New York City, NY, USA
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muellner, M., Chiapparelli, E., Moser, M. et al. The effect of age on psoas and paraspinal muscle morphology in patients undergoing posterior lumbar fusion surgery. Eur Spine J 31, 2619–2628 (2022). https://doi.org/10.1007/s00586-022-07346-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07346-0