Abstract
Background
Although multiple individual immune parameters have been demonstrated to predict the occurrence of secondary infection after critical illness, significant questions remain with regards to the selection, timing and clinical utility of such immune monitoring tests.
Research question
As a sub-study of the REALISM study, the REALIST score was developed as a pragmatic approach to help clinicians better identify and stratify patients at high risk for secondary infection, using a simple set of relatively available and technically robust biomarkers.
Study design and methods
This is a sub-study of a single-centre prospective cohort study of immune profiling in critically ill adults admitted after severe trauma, major surgery or sepsis/septic shock. For the REALIST score, five immune parameters were pre-emptively selected based on their clinical applicability and technical robustness. Predictive power of different parameters and combinations of parameters was assessed. The main outcome of interest was the occurrence of secondary infection within 30 days.
Results
After excluding statistically redundant and poorly predictive parameters, three parameters remained in the REALIST score: mHLA-DR, percentage of immature (CD10− CD16−) neutrophils and serum IL-10 level. In the cohort of interest (n = 189), incidence of secondary infection at day 30 increased from 8% for patients with REALIST score of 0 to 46% in patients with a score of 3 abnormal parameters, measured ad D5–7. When adjusted for a priori identified clinical risk factors for secondary infection (SOFA score and invasive mechanical ventilation at D5–7), a higher REALIST score was independently associated with increased risk of secondary infection (42 events (22.2%), adjusted HR 3.22 (1.09–9.50), p = 0.034) and mortality (10 events (5.3%), p = 0.001).
Interpretation
We derived and presented the REALIST score, a simple and pragmatic stratification strategy which provides clinicians with a clear assessment of the immune status of their patients. This new tool could help optimize care of these individuals and could contribute in designing future trials of immune stimulation strategies.
Graphical Abstract

Similar content being viewed by others
Introduction
For patients with critical illness, occurrence of secondary infection is a major and frequent complication, affecting between 15 and 40% of patients after an Intensive Care Unit (ICU) admission [1,2,3,4,5,6]. Such infections are associated with increased morbidity and mortality and represent a high burden of care with longer ICU length of stay and overall greater healthcare costs [2, 7]. In addition, they contribute to higher rates of microbial resistance through extensive use of antibiotic and antifungal agents, a pressing and worldwide issue [8,9,10] which has recently been further highlighted amidst the COVID-19 pandemic [11].
Among factors leading to acquisition of secondary infection in the ICU, the contribution of critical illness-induced immune dysfunction is now well recognized. Although this phenomenon, which affects both innate and adaptive immune responses, has been mainly described in sepsis [12, 13], similar immune alterations have been described in various aetiologies of critical illness [14,15,16], suggesting a somewhat common immune pathway. The REALISM study [17] (REAnimation Low Immune Status Marker) was performed to describe deep immune profiling of injury-induced immune response in a variety of critical illnesses, and among other findings has further reinforced the concept of a common global immune response to various types of severe injury.
Although multiple immune parameters have been shown to have some degree of predictive power for occurrence of secondary infection, significant heterogeneity exists regarding which test to use, with which cutoff values, at which timepoint and in which population [14, 18]. As such, there is a need for clinically relevant stratification tools to assess the occult immune status of critically ill patients to better tailor care of such fragile individuals. Of note, in REALISM, the occurrence of secondary infection was somehow late (median day 9 [6–15] after ICU admission) and predominantly occurred in patients who were still in the ICU.
As a sub-study of REALISM, the REALIST score was thus developed as a pragmatic approach to help clinicians better identify and stratify patients at high risk for secondary infection after the initial phase of resuscitation, using a simple set of relatively commonly available and technically robust biomarkers. The main objective of this study is to explore the predictive power of the REALIST score regarding subsequent secondary infection.
Methods
This is a sub study of REALISM [17], for which a detailed protocol has been previously published [19]. In summary, REALISM is a prospective, observational cohort study of critically ill patients admitted with sepsis, severe trauma or planned surgery, which was performed from 2015 to 2018 at the Edouard Herriot Hospital (Hospices Civils de Lyon, France). The study protocol was approved by institutional review board (Comité de Protection des Personnes Sud-Est II) under number 2015-42-2.
Inclusion criteria for REALISM were: adult patients admitted to the ICU with a clinical diagnosis of sepsis as defined by 2016 SEPSIS-3 consensus guidelines [20]; or severe trauma with injury severity score (ISS) > 15; or surgical patients undergoing major surgeries, such as eso-gastrectomy, bladder resection with Brickers’ reconstruction, cephalic pancreaticoduodenectomy and abdominal aortic aneurysm surgery by laparotomy. Exclusion criteria were any of the following: presence of a pre-existent condition or under treatment that could influence patients’ immune status, pregnancy, institutionalized patients and inability to obtain informed consent. Written informed consent was obtained from every patient or their representative upon inclusion in this protocol. In the event that only the informed consent of a third party has been sought at the time of inclusion, the patients were informed as soon as possible of their participation in this study and asked to give their own consent to continue the study.
Sampling and clinical data collection
Regarding the present sub-study, samples were collected three times during the first week after enrollment: at day 1 or 2 (D1–2), D3–4 and D5–7, with the latter pre-emptively selected as the timepoint of interest. Peripheral whole blood was collected in one ethylenediaminetetraacetic acid (EDTA) tube at each timepoint for each patient. Tubes were immediately transferred to the lab and processed within 3 h after blood sampling for flow cytometry immune phenotyping and plasma cytokine level measurements.
The main cohort consisted of all patients initially enrolled in the REALISM study. As most secondary infections in the ICU occur more than 1 week after admission (median 9 [6–15] days in the REALISM study) and in an effort to select patients with persistently high risk of events, a predefined cohort of interest was formed, consisting of all patients who were still alive and in the ICU at D5–7. Patients who developed a secondary infection prior to their sampling day were excluded.
Patients’ demographics, comorbidities, diagnosis, severity and clinical outcomes were prospectively collected and longitudinal follow-up was performed for 90 days. The following data were recorded: demographic information (age, gender, body mass index (BMI)), disease severity measured by the Simplified Acute Physiological Score (SAPS) II at ICU admission [21] and the Sequential Organ Failure Assessment (SOFA) score [22] measured at D1, D3–4 and D5–7. ISS was collected for trauma patients [23]. Hospital and ICU lengths of stay and survival were measured until day 90 after admission. Follow-up location after ICU discharge was recorded. During hospital stay, patients were screened daily for exposure to invasive mechanical ventilation and for secondary infection occurrence. The main outcome of interest was the occurrence of secondary infection within day 30 after ICU admission and prespecified secondary outcomes were mortality at day 30, days free from ICU at 30 days and days free from hospital at 30 days.
Definition of secondary infections
Information related to infections were collected by research nurses and reviewed and validated by a dedicated adjudication committee composed of 3 clinicians not involved in patients’ recruitment or care and scrutinizing data simultaneously. Confirmation of secondary infection occurrence by this committee was based on guidelines defined by the European Center for Disease Prevention and Control [24] and Infectious Diseases Society of America [25]. “Definite” and “likely” infections were included and only the first secondary infection episode was considered in the analyses. Adjudication committee was blinded for results of immune parameters. Patients who died without being identified as having a “definite” or “likely” secondary infection were not censored from analysis.
Score derivation
Five biological parameters were initially selected for analysis, based on their established association with critical illness immune perturbations, availability and cost in the clinical setting and technical robustness and reproducibility outside expert centers. These 5 parameters were: monocyte HLA-DR by flow cytometry, percentage of immature neutrophils by flow cytometry (CD10−CD16low) [26], IL-6 and IL-10 concentration by enzyme-linked immunosorbent assay (ELISA) and total lymphocytes count by hemocytometer. Technical details may be found in the main study protocol [19].
Determination of cutoff points
Receiver operating characteristic (ROC) curves were constructed for each of the 5 parameters at each timepoint, with the relevant clinical endpoint defined as secondary infection at day 30. Parameters with poor predictive ability (area under the curve (AUC) < 0.6 at each timepoint) were removed from the model and excluded from further analysis. For remaining parameters, optimal cutoff points were derived using the top left index (minimal distance to top left corner) and each parameter was further binarized into “low risk” and “high risk” at each timepoint.
Finally, pairwise Cox association models were performed, “adjusting” parameters with each other, thus giving a model for each pair of parameters to identify complementary or redundant ones. Redundant parameters were excluded from the model and from further analysis, to ensure that each parameter independently brought information to the model (excluding the redundant parameter with the lowest individual HR). A score was thus constructed as the combined sum of the binarized remaining parameters (with 1 point for “high risk”, and 0 point for “low risk” markers).
Score
The predictive power of the resulting combination (score) was evaluated at the prespecified timepoint of interest D5–7 in patients still in ICU at that timepoint (cohort of interest), with absolute risk of secondary infection presented in each category. Univariate and adjusted Cox proportional hazards models were performed to adjust for a priori identified clinical risk factors for secondary infection, i.e. the physiological severity of illness (SOFA score at timepoint of interest), and disruption of normal barriers by invasive mechanical ventilation at timepoint of interest. Unadjusted and adjusted hazard ratios were computed.
Data are presented as numbers and percentages (qualitative variables) and medians and 25th/75th percentiles (quantitative variables). Chi square or Fisher’s exact test were used for qualitative variables assessment. Quantitative variables were compared with Mann–Whitney U test. The level of significance was set at 5%. Statistical analyses were computed with R software v3.6.2.
Results
Out of 1079 screened patients, 353 (33%) were included in the main REALISM study [17]. The overall study population consisted primarily of males (65.4%) with a median age of 60 [47–71] years and an admission SAPS 2 score of 29 [20–43]. Of these, 278 patients (78.8%), 261 (73.9%) and 191 (54.1%) were still alive and in the ICU at timepoint D1–2, D3–4 and D5–7, respectively.
The cohort of interest (patients alive and still in ICU at D5–7) consisted of 189 patients after excluding individuals with missing data. From this cohort of interest, 42 (22.0%) developed subsequent secondary infections at D30 (Additional file 1: Table S1). The detailed description of patients’ characteristics is presented in Table 1.
Predictive power of individual parameters
ROC curves were computed for each prespecified immune parameter (mHLA-DR, percentage of immature neutrophils, IL-6 and IL-10 concentration and total lymphocytes count, see e-Table 1). All parameters had an AUC above 0.6 at least at one timepoint except for lymphocyte count (AUC 0.46, 0.56 and 0.52, respectively), which was thus excluded from further analysis. Cutoffs values were computed for the four remaining parameters (mHLA-DR, percentage of immature neutrophils, IL-6 and IL-10). For consistency, we only used the cutoff values computed at D5–7 from the cohort of interest. Values were dichotomized (“high-risk” vs “low-risk”). When adjusted for each other through pairwise association, every parameter brought complementary information to the models except for IL-6 and IL-10, which were considered redundant. Because IL-6 had the lowest predictive power for occurrence of secondary infection (unadjusted HR 1.82 (0.95–3.45), p = 0.069), it was excluded from further analysis.
The three remaining parameters were thus mHLA-DR, percentage of immature neutrophils and IL-10 (Table 2). When measured at days 5–7 from the cohort of interest, all three parameters had excellent predictive power for occurrence of secondary infection at day 30, with percentage of immature neutrophils performing best (unadjusted HR 2.55 (1.38–4.73) p = 0.003), followed by mHLA-DR (unadjusted HR 2.52 (1.31–4.85) p = 0.006), and IL-10 levels (HR 2.18 (1.07–4.45) p = 0.031).
Predictive power for these three parameters was also computed for other prior timepoints (D1–2 and D3–4, see Additional file 1: Table S3). None of the individual parameters had significant predictive power for occurrence of secondary infection at D1–2. When measured at D3–4, parameters only had moderate predictive power for occurrence of secondary infection at day 30 (mHLA-DR, unadjusted HR 1.85, CI [1.15–2.98], p = 0.01; percentage of immature neutrophils, unadjusted HR 1.83 [1.12–3.00] p = 0.01); IL-10 levels, unadjusted HR 1.72, CI [1.07–2.77], p = 0.02).
The REALIST score
For these remaining parameters (mHLA-DR, immature neutrophils and IL-10), a point was given for each “high-risk” results as measured at D5–7. As such, for each patient still in the ICU at D5–7 (n = 189), a score between 0 and 3 was obtained, with 3 representing the highest risk of secondary infection. Incidence of secondary infection increased from 8% for patients with score of 0 to 46% in patients with a score of 3 (Fig. 1). Higher REALIST score was also associated with increased mortality at 30 days (p = 0.001 by Fisher's Exact Test).
When adjusted for a priori identified clinical risk factors for secondary infection, (SOFA score and invasive mechanical ventilation at timepoint of interest) a higher REALIST score was independently associated with increased risk of secondary infection (Table 3). For instance, patients with a score of 3 were 3.2 times more likely to develop secondary infection than patients with a score of 0, independent of clinical risk factors (adjusted HR 3.22 (1.09–9.50), p = 0.034).
Discussion
As a sub-study of the REALISM project, the REALIST score was developed as a pragmatic and clinically applicable stratification strategy to identify patients with occult immune dysfunction. In our cohort of mixed ICU patients, the REALIST score was able to identify patients at high risk of secondary infections, an association that was independent from major clinical risk factors for infection. As such, this approach demonstrated that genuinely occult immune dysfunction can be identified in ICU patients with tools that are quite potentially available to the frontline critical care physician outside expert research centers [27, 28].
Insights from the REALISM study
The REALISM study outlined how the immune response to injury engages all components of the immune system and does not significantly vary with the type of injury (infectious vs sterile). The initial response is not associated with increased risk of death and secondary infection, illustrating that the initial pro-inflammatory immune response induced by injury should not necessarily be seen as a deleterious factor per se but rather represents an adaptive response to the injury. As induction of the pro-inflammatory effector response is associated with the concomitant development of regulatory mechanisms to protect the host from such overwhelming immune response, this also illustrates the complex interplay between the effector and regulatory mechanisms of the immune system to set up a coordinated immune response to injury. This initial host response likely aims at controlling the aggression and at protecting the host from deleterious off-targets effects of this tremendous immune response.
Thus, after the initial physiologic immune response to injury, it is the persistence (or delayed recovery) of immune alterations that predisposes patients to deleterious infectious events, independently of usual confounding factors. In this subgroup of patients, this persistently dysregulated immune profile cannot be considered as part of the physiologic response to injury but rather as a maladaptive evolution of the immune response.
Therefore, as tempting it might be to try to predict subsequent infection in patients soon after ICU admission, this might not be neither practical nor pertinent. A promising approach to immune monitoring, therefore, seems to be to target the persistence of immune alterations at the end of the first week of ICU stay, identifying patients in which immune homeostasis is pathologically compromised. Knowledge of such occult immune dysfunction is not only interesting, it can also directly influence and hopefully optimize patients’ care, either through enhanced clinical surveillance, accelerated start of antimicrobials in case of infection suspicion, removal of potentially superfluous invasive device, and eventually through immune stimulation strategies [29]. In parallel, a REALIST score of 0 in an otherwise clinically stable patient would provide further reassurance and possibly support deescalating antimicrobial treatment in the right clinical context, for instance. Finally, such immune function scoring could be used to enrich a study population with patients at high risk for secondary infection in the context of an eventual immune stimulation randomized controlled trial.
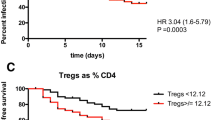
Our study echoes the work of Conway-Moris et al.in the important INFECT study [14], in which the authors elegantly presented an immune score based on levels of mHLA-DR, Treg lymphocytes (CD4+/CD25++/CD127−) and dysfunctional neutrophils (nCD88) by flow cytometry after strict standardization within different centers. Their score was shown to predict secondary infection in critically ill patients with organ dysfunction (unadjusted HR 4.30 [CI 1.70–10.20] when measured at days 4–6), which interestingly is quite similar to the performance of the REALIST score (unadjusted HR 4.41 [CI 1.63–11.98] at D5–7). Even though Conway-Morris et al. selected different immune parameters than ours and even though patients in the INFECT study had higher illness severity than patients in REALISM, these similar results tend to validate the concept and pertinence of combining parameters to tackle immune monitoring in the ICU across a wide range of patients, even those whom clinical status might seem somewhat reassuring.
Recently, Fang et al. described and validated a similar immune dysfunction score performed at day 1 of ICU admission to help predict mortality in critically ill patients. In that study [30], the combination of monocyte HLA-DR, Il-10 levels, G-CSF levels and ratio of segmented neutrophils to monocyte allowed predicted 28 day mortality with an AUC of 0.789. Interestingly, even though the timepoint and outcome of interest are different than those in the REALIST score, there is significant similarities between chosen immune parameters, further reinforcing the rationale behind immune monitoring in the critically ill.
Choice of immune parameters
Besides mHLA-DR, which is the most studied and validated biomarker in the field with widespread standardization across laboratories [31, 32], Conway-Morris et al. also used the level of Treg (CD4+/CD25++/CD127−) and neutrophils surface expression of CD88. Neutrophil CD88, a receptor for complement anaphylatoxin C5a, has been relatively scarcely described in the critical care context and has only been reported in expert research centers [33,34,35]; it has not been performed in the REALISM study. In parallel, the phenotypical identification of Treg lymphocytes is notoriously problematic and the standardization of their staining by flow cytometry is challenging even with modern techniques in expert centers [36,37,38]. Of note, in the REALISM study, percentage of Treg lymphocytes was not associated with occurrence of secondary infection at D30 through univariate analysis, whether measured at days 1–2, 3–4 or 5–7 (best HR at D3–4: 1.08 (0.84–1.38), p = 0.552).
As immunophenotyping has historically suffered from lack of standardization and reproducibility [39], particular importance must be attributed to these aspects if one hopes for immune monitoring tools to permeate into clinical practice. Thus, for the REALIST score, we purposely and pre-emptively chose immune parameters based on their immediate applicability in clinical practice outside expert centers. As such, technical robustness and reproducibility were major drivers for selecting otherwise relevant immune parameters from the REALISM study.
To complement mHLA-DR, we selected the expression of CD10 and CD16 on neutrophils as a technically simple marker of dysregulated granulopoiesis and inadequate granulocyte maturation. In other words, CD10lowCD16low neutrophils are immature and quite probably the immunophenotypic equivalent of band cells [26, 40, 41], although variability and impreciseness in band cell measurement [42] has precluded such a definite association. Like band cells [43], an increase in CD10lowCD16low neutrophils has been associated with poor outcomes in sepsis patients, namely, occurrence of secondary infection and death [41], and might also directly contribute to impaired T cell function [40]. Our study supports these past findings, as higher proportion of circulating CD10lowCD16low neutrophils at days 5–7 was independently associated with occurrence of secondary infection at day 30.
Lymphopenia has been found to be associated with poor outcome after sepsis and in other clinical illnesses, and therapeutic interventions to increase lymphocytes levels after sepsis have been proposed and are under investigation [44]. Surprisingly, low lymphocytes levels were not associated with secondary infection or mortality at any timepoint in the REALISM cohort, a finding that might be due to lower severity of illness and relatively low event rate.
IL-6 and IL-10 levels were both associated with occurrence of secondary infection in our study, although they brought redundant information in pairwise analysis. As IL-6 is a pro-inflammatory cytokine and IL-10 a globally anti-inflammatory cytokine, it was somewhat expected that elevated IL-10 levels would be associated with immune dysfunction, which was confirmed in this study. Of note, IL-10 levels are strongly correlated with IL-6 levels at all timepoints, as shown in the REALISM study [17], a finding that reflects the intricate and immediate interplay between effector and regulatory limbs of the immune system. As such, IL-6 levels that fail to return towards normal at days 5–7 suggest either immune dysfunction through impaired homeostasis mechanisms and/or uncontrolled inflammatory focus with associated higher disease severity. Of note, the latter hypothesis is supported by the finding that the association between higher IL-6 levels at days 5–7 and secondary infection was not statistically significant after controlling for SOFA score and presence of invasive device.
Strengths and limitations
In our study, we assessed the performance of multiple parameters at multiple timepoints in a relatively large cohort of mixed critically ill patients. We tailored our score to be easily applicable in clinical practice, with a fixed and clear timepoint, reliable and technically robust parameters with a strong track record, and simple computation by bedside clinicians. We also demonstrated strong association with secondary infections even after controlling for SOFA score and presence of invasive mechanical ventilation. We elected to control for both of these variables, even though they are partially redundant (as respiratory support is included in the SOFA score) because of the strong and clinically important association between invasive mechanical ventilation and risk of infection (namely, pneumonia). This thus represents a more stringent statistical correction than seen in other similar studies, further supporting the claim that our score is not a mere marker of disease severity but really an immune monitoring tool that provides genuinely new and previously occult information to the clinician.
Among significant limitations, our study was single-centre and suffers from a relatively low disease severity and low event rate. Although this reduced the strength of association between parameters and outcome, it also suggests that the score is applicable to a wide array of patients with varying disease severity, as secondary infections can occur even in patients with low disease severity with genuinely occult immune dysfunction. Importantly, the REALIST score will have to be further validated in a separate multicentric cohort.
Interpretation
In conclusion, we derived and presented the REALIST score, a simple and pragmatic stratification strategy which provides critical care clinicians with a clear and useful assessment of the occult immune status of their patient. This new tool could help optimize care of these fragile individuals and could contribute in designing future trials of immune stimulation strategies. Ultimately, we believe this score, in conjunction with the main REALISM study, provides important didactic value, as the question of critical illness induced immune dysfunction warrants widespread discussion within the critical care community if we are to adapt our practice to this complex phenomenon and lastingly provide better care.
Availability of data and materials
Original data will be made available upon adequate request to the corresponding author.
Abbreviations
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- EDTA:
-
Ethylenediaminetetraacetic acid
- ELISA:
-
Enzyme-linked immunosorbent assay
- ICU:
-
Intensive care unit
- mHLA-DR:
-
Monocyte human leucocyte antigen-DR\
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- ROC:
-
Receiver operating characteristic
- SAPS:
-
Simplified Acute Physiological Score
- SOFA:
-
Sequential Organ Failure Assessment
References
Vincent JL, Rello J, Marshall J, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302(21):2323–9.
Agodi A, Barchitta M, Auxilia F, et al. Epidemiology of intensive care unit-acquired sepsis in Italy: results of the SPIN-UTI network. Ann Ig. 2018;30(5):15–21.
van Vught LA, Klein Klouwenberg PM, Spitoni C, et al. Incidence, risk factors, and attributable mortality of secondary infections in the intensive care unit after admission for sepsis. JAMA. 2016;315(14):1469–79.
Zhao GJ, Li D, Zhao Q, et al. Incidence, risk factors and impact on outcomes of secondary infection in patients with septic shock: an 8-year retrospective study. Sci Rep. 2016;6:38361.
Abulhasan YB, Rachel SP, Chatillon-Angle MO, et al. Healthcare-associated infections in the neurological intensive care unit: Results of a 6-year surveillance study at a major tertiary care center. Am J Infect Control. 2018;46(6):656–62.
Vincent JL, Sakr Y, Singer M, et al. Prevalence and outcomes of infection among patients in intensive care units in 2017. JAMA. 2020;323(15):1478–87.
Schmier JK, Hulme-Lowe CK, Semenova S, et al. Estimated hospital costs associated with preventable health care-associated infections if health care antiseptic products were unavailable. Clinicoecon Outcomes Res. 2016;8:197–205.
Lemmen SW, Hafner H, Kotterik S, Lutticken R, Topper R. Influence of an infectious disease service on antibiotic prescription behavior and selection of multiresistant pathogens. Infection. 2000;28(6):384–7.
Zilahi G, Artigas A, Martin-Loeches I. What’s new in multidrug-resistant pathogens in the ICU? Ann Intensive Care. 2016;6(1):96.
De Waele JJ, Boelens J, Leroux-Roels I. Multidrug-resistant bacteria in ICU: fact or myth. Curr Opin Anaesthesiol. 2020. https://doi.org/10.1097/ACO.0000000000000830.
Ghosh S, Bornman C, Zafer MM. Antimicrobial resistance threats in the emerging COVID-19 pandemic: where do we stand? J Infect Public Health. 2021;14(5):555–60.
Monneret G, Lepape A, Voirin N, et al. Persisting low monocyte human leukocyte antigen-DR expression predicts mortality in septic shock. Intensive Care Med. 2006;32(8):1175–83.
van Vught LA, Wiewel MA, Hoogendijk AJ, et al. The host response in patients with sepsis developing intensive care unit-acquired secondary infections. Am J Respir Crit Care Med. 2017;196(4):458–70.
Conway Morris A, Datta D, Shankar-Hari M, et al. Cell-surface signatures of immune dysfunction risk-stratify critically ill patients: INFECT study. Intensive Care Med. 2018;44(5):627–35.
Torrance HD, Pearse RM, O’Dwyer MJ. Does major surgery induce immune suppression and increase the risk of postoperative infection? Curr Opin Anaesthesiol. 2016;29(3):376–83.
Efron PA, Mohr AM, Bihorac A, et al. Persistent inflammation, immunosuppression, and catabolism and the development of chronic critical illness after surgery. Surgery. 2018;164(2):178–84.
Venet F, Textoris J, Blein S, et al. Immune profiling demonstrates a common immune signature of delayed acquired immunodeficiency in patients with various etiologies of severe injury. Crit Care Med. 2022;50(4):565–75.
Misra AK, Levy MM, Ward NS. Biomarkers of immunosuppression. Crit Care Clin. 2020;36(1):167–76.
Rol ML, Venet F, Rimmele T, et al. The REAnimation Low Immune Status Markers (REALISM) project: a protocol for broad characterisation and follow-up of injury-induced immunosuppression in intensive care unit (ICU) critically ill patients. BMJ Open. 2017;7(6): e015734.
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10.
Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–63.
Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10.
Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96.
European Center for Disease Prevention and Control. Incidence and attributable mortality of healthcare-associated infections in intensive care units in Europe 2008–2012. Stockholm: ECDC; 2018.
Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the infectious diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61–111.
Orr Y, Taylor JM, Bannon PG, Geczy C, Kritharides L. Circulating CD10-/CD16low neutrophils provide a quantitative index of active bone marrow neutrophil release. Br J Haematol. 2005;131(4):508–19.
Liu G, Jiang C, Lin X, Yang Y. Point-of-care detection of cytokines in cytokine storm management and beyond: significance and challenges. View (Beijing). 2021;2:20210003.
Tamulyte S, Kopplin J, Brenner T, Weigand MA, Uhle F. Monocyte HLA-DR assessment by a novel point-of-care device is feasible for early identification of ICU patients with complicated courses-a proof-of-principle study. Front Immunol. 2019;10:432.
Venet F, Monneret G. Advances in the understanding and treatment of sepsis-induced immunosuppression. Nat Rev Nephrol. 2018;14(2):121–37.
Fang WF, Douglas IS, Chen YM, et al. Development and validation of immune dysfunction score to predict 28-day mortality of sepsis patients. PLoS ONE. 2017;12(10): e0187088.
Monneret G, Gossez M, Aghaeepour N, Gaudilliere B, Venet F. How clinical flow cytometry rebooted sepsis immunology. Cytom A. 2019;95(4):431–41.
Torres LK, Pickkers P, van der Poll T. Sepsis-Induced Immunosuppression. Annu Rev Physiol. 2022;84:157–81.
Furebring M, Hakansson LD, Venge P, Nilsson B, Sjolin J. Expression of the C5a receptor (CD88) on granulocytes and monocytes in patients with severe sepsis. Crit Care. 2002;6(4):363–70.
Guo RF, Riedemann NC, Ward PA. Role of C5a–C5aR interaction in sepsis. Shock. 2004;21(1):1–7.
Unnewehr H, Rittirsch D, Sarma JV, et al. Changes and regulation of the C5a receptor on neutrophils during septic shock in humans. J Immunol. 2013;190(8):4215–25.
Seddiki N, Santner-Nanan B, Martinson J, et al. Expression of interleukin (IL)-2 and IL-7 receptors discriminates between human regulatory and activated T cells. J Exp Med. 2006;203(7):1693–700.
Pitoiset F, Barbie M, Monneret G, et al. A standardized flow cytometry procedure for the monitoring of regulatory T cells in clinical trials. Cytometry B Clin Cytom. 2018;94(5):621–6.
Rodriguez-Perea AL, Arcia ED, Rueda CM, Velilla PA. Phenotypical characterization of regulatory T cells in humans and rodents. Clin Exp Immunol. 2016;185(3):281–91.
Venet F, Lepape A, Monneret G. Clinical review: flow cytometry perspectives in the ICU - from diagnosis of infection to monitoring of injury-induced immune dysfunctions. Crit Care. 2011;15(5):231.
Guerin E, Orabona M, Raquil MA, et al. Circulating immature granulocytes with T-cell killing functions predict sepsis deterioration*. Crit Care Med. 2014;42(9):2007–18.
Demaret J, Venet F, Friggeri A, et al. Marked alterations of neutrophil functions during sepsis-induced immunosuppression. J Leukoc Biol. 2015;98(6):1081–90.
Cornbleet PJ. Clinical utility of the band count. Clin Lab Med. 2002;22(1):101–36.
Cavallazzi R, Bennin CL, Hirani A, Gilbert C, Marik PE. Is the band count useful in the diagnosis of infection? An accuracy study in critically ill patients. J Intensive Care Med. 2010;25(6):353–7.
Francois B, Jeannet R, Daix T, et al. Interleukin-7 restores lymphocytes in septic shock: the IRIS-7 randomized clinical trial. JCI Insight. 2018. https://doi.org/10.1172/jci.insight.98960.
Acknowledgements
REALISM study group.
HCL: Sophie Arnal, Caroline Augris-Mathieu, Frédérique Bayle, Liana Caruso, Charles-Eric Ber, Asma Ben-amor, Anne-Sophie Bellocq, Farida Benatir, Anne Bertin-Maghit, Marc Bertin-Maghit, André Boibieux, Yves Bouffard, Jean-Christophe Cejka, Valérie Cerro, Jullien Crozon-Clauzel, Julien Davidson, Sophie Debord-Peguet, Benjamin Delwarde, Robert Deleat-Besson, Claire Delsuc, Bertrand Devigne, Laure Fayolle-Pivot, Alexandre Faure, Bernard Floccard, Julie Gatel, Charline Genin, Thibaut Girardot, Arnaud Gregoire, Baptiste Hengy, Laetitia Huriaux, Catherine Jadaud, Alain Lepape, Véronique Leray, Anne-Claire Lukaszewicz, Guillaume Marcotte, Olivier Martin, Marie Matray, Delphine Maucort-Boulch, Pascal Meuret, Céline Monard, Florent Moriceau, Guillaume Monneret, Nathalie Panel, Najia Rahali, Thomas Rimmele, Cyrille Truc, Thomas Uberti, Hélène Vallin, Fabienne Venet, Sylvie Tissot, Abbès Zadam
bioMérieux: Sophie Blein, Karen Brengel-Pesce, Elisabeth Cerrato, Valerie Cheynet, Emmanuelle Gallet-Gorius, Audrey Guichard, Camille Jourdan, Natacha Koenig, François Mallet, Boris Meunier, Virginie Moucadel, Marine Mommert, Guy Oriol, Alexandre Pachot, Estelle Peronnet, Claire Schrevel, Olivier Tabone, Julien Textoris, Javier Yugueros Marcos
BIOASTER: Jeremie Becker, Frederic Bequet, Yacine Bounab, Florian Brajon, Bertrand Canard, Muriel Collus, Nathalie Garcon, Irene Gorse, Cyril Guyard, Fabien Lavocat, Philippe Leissner, Karen Louis, Maxime Mistretta, Jeanne Moriniere, Yoann Mouscaz, Laura Noailles, Magali Perret, Frederic Reynier, Cindy Riffaud, Mary-Luz Rol, Nicolas Sapay, Trang Tran, Christophe Vedrine
SANOFI: Christophe Carre, Pierre Cortez, Aymeric De Monfort, Karine Florin, Laurent Fraisse, Isabelle Fugier, Sandrine Payrard, Annick Peleraux, Laurence Quemeneur
ESPCI: Andrew Griffiths, Stephanie Toetsch
GSK: Teri Ashton, Peter J. Gough, Scott B. Berger, David Gardiner, Iain Gillespie, Aidan Macnamara, Aparna Raychaudhuri, Rob Smylie, Lionel Tan, Craig Tipple
Funding
JAT was funded by the Royal College of Physicians of Canada and by the Fonds de Recherche Québec Santé. FP is an employee of bioMérieux SA, an in vitro diagnostic company and works in a joint research unit, co funded by the Hospices Civils de Lyon and bioMérieux. LK works in a joint research unit, co funded by the Hospices Civils de Lyon and bioMérieux. JT is an employee of bioMérieux SA, an in vitro diagnostic company and works in a joint research unit, co funded by the Hospices Civils de Lyon and bioMérieux. KBP is an employee of bioMérieux SA, an in vitro diagnostic company. ACL works in a joint research unit, co funded by the Hospices Civils de Lyon and bioMérieux. LQ is an employee of Sanofi Pasteur. CV is an employee of BIOASTER. LKT is employee of and hold stock and shares in GlaxoSmithKline. FV works in a joint research unit, co funded by the Hospices Civils de Lyon and bioMérieux. TR works in a joint research unit, co funded by the Hospices Civils de Lyon and bioMérieux. GM works in a joint research unit, co funded by the Hospices Civils de Lyon and bioMérieux This study received funding from the Agence Nationale de la Recherche through a grant awarded to BIOASTER (Grant number #ANR-10-AIRT-03) and from bioMérieux, Sanofi and GSK.
Author information
Authors and Affiliations
Consortia
Contributions
JAT designed the study, analysed and interpreted the data and wrote the manuscript. FP and LK contributed substantially to the study design and performed the statistical analyses. JT, FV and TR contributed substantially to the study design, data analysis and in writing the manuscript. KBP, ACL, LQ, CV and LKT helped in data interpretation and in writing the manuscript. GM was the instigator of the study, contributed significantly to the study design, data analysis and interpretation and in writing the manuscript. JAT and GM are both guarantors of this manuscript, taking responsibility for the integrity of the work as a whole.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by institutional review board (Comité de Protection des Personnes Sud-Est II) under number 2015-42-2.
Consent for publication
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Secondary infection characteristics (n=42) in the cohort of interest. Table S2. Description of sites and types of initial infections in the subgroup of septic patients. Table S3. Individual predictive power (for occurrence of secondary infection) of immune parameters at different timepoints for patients still in the ICU at day 5–7 (n=189). Table S4. Sample of different cut-off points for mHLA-DR ROC-curve and their respective predictive power for secondary infection at D30. Table S5. Sample of different cut-off points for percentage of immature neutrophils ROC-curve and their respective predictive power for secondary infection at D30.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tremblay, JA., Peron, F., Kreitmann, L. et al. A stratification strategy to predict secondary infection in critical illness-induced immune dysfunction: the REALIST score. Ann. Intensive Care 12, 76 (2022). https://doi.org/10.1186/s13613-022-01051-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-022-01051-3