Abstract
Background
Among the surgical methods for femoral fractures, the Ortho-Bridge System (OBS) appears to heal fractures via an uncommon process. We compared its effectiveness and biomechanical aspects to those of a locking compression plate (LCP) and explained the healing process demonstrated by the OBS.
Methods
Eleven femoral shaft fracture cases treated with OBS between July 2017 and May 2020 were retrospectively reviewed. Clinical and radiographic data were collected during regular postoperative follow-up visits and assessed via the Harris Hip Score and Knee Society Score. We performed biomechanical experiments of OBS. We simulated different fracture conditions and selected appropriate screw holes at the fracture’s far and near segments. The OBS module was placed according to the position of LCP’s locking hole at both ends of the fracture; then, a static three-point bending test was performed.
Results
All patients had contralateral callus growth with secondary fracture healing. Healing time was 3–5 months with excellent hip and knee function. When the key screw distance was 22–34 mm, the OBS was significantly less stiff than the LCP (P < 0.05). The stiffness of LCP and OBS decreased significantly when the key screw distance was 49–82 mm, with the LCP being slightly stronger (P < 0.05).
Conclusions
Femoral shaft fracture treatment with OBS demonstrated secondary healing. When the distance between the key screws was 20–40 mm, the elasticity was higher in OBS than in LCP, possibly producing axial micro-motion to stimulate callus formation and promote fracture healing, which differ from the plate’s primary healing process.
Similar content being viewed by others
Introduction
The femoral shaft is a common fracture site in trauma patients [1]. According to epidemiological statistics, femoral fracture occurs in a typical bimodal age distribution and most commonly among young adult men with high-energy injury mechanisms. Proximal femoral fractures are more common in postmenopausal elderly women, who are prone to accidental walking injuries [2]. There have been many surgical methods employed for femoral fractures, including anterograde and retrograde intramedullary nails, various types of steel plates, and external fixators. However, each treatment method has its own advantages and disadvantages [3,4,5,6,7,8].
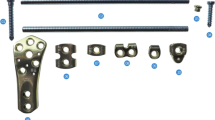
In this article, we introduce another internal fixation instrument for these fractures—the Ortho-Bridge System (OBS). This was developed and designed in China with independent intellectual property rights (Walkman Biomaterial Co., Ltd., Tianjin, China, patent number: ZL200510010654.3), and it consists of different types of single-rod fixation blocks, double-rod fixation blocks, anatomical modules, connecting rods, screws, and locking nuts. The single-rod fixed block is divided into single-rod single-hole block and single-rod double-hole block; double-rod fixed block is divided into double-rod single-hole and double-rod double-hole block; the anatomical blocks are divided into proximal humerus, proximal and distal femur, lateral and medial proximal tibia, and distal tibial fixation block according to the location; the length of the connecting rod can be freely selected and pre-bent shaping; the screws include locking screws and compression screws [9]. The OBS is a new type of fracture fixation device, which incorporates the structural concepts of a locking steel plate, an external fixation bracket, and a spine screw-rod system. The connecting clamp has a rod hole and a locking screw hole, and the fixing rod can rotate and slide freely through the rod hole. The locking screw is double-threaded; the front thread is screwed into the bone and the rear thread is screwed into the locking hole of the connecting clamp. When the rear thread is screwed into the locking hole, the nail tail directly presses on the fixing rod, locking the rod, the clamp, and the nail, thereby forming a locking integral connection. During the operation, the fixed block, anatomical block, and connecting rod can be flexibly selected according to different parts to be freely assembled to complete the fixation of fractures such as cadres or joints. We are in favor of this free combination, and can even complete the full-length fixation of long stem bones such as femur and tibia. According to the fracture situation of each patient, single connecting rod fixation, double connecting rod fixation, or three connecting rod fixation can be designed, which truly realizes personalized fixation (Fig. 1). OBS is suitable for limb and pelvic orthopedics and internal fixation of traumatic fractures. This kind of fixation is an elastic fixation, which can effectively reduce the stress shielding and protect the blood supply of the fractured end, and promote fracture healing [10]. Since 2013, the treatment of simple or complex fractures in limbs, the pelvis, the scapula, and other parts has been performed via this technique, and fracture healing has been achieved. In addition, we found that there was a different process of fracture healing between the OBS and a locking compression plate (LCP). To further study the different healing processes, we reviewed cases that used the OBS for internal fixation of femoral fractures and performed biomechanical analysis of the OBS and LCP. This study aimed to further explain the healing process demonstrated by the application of the OBS in the treatment of simple femoral fractures and analyze its mechanism.
The Ortho-Bridge system. a Components of the OBS; b schematic diagram of the OBS of the distal femur composed of various components in figure a; c introduction of specific types of connecting clamp, special clamp, and screws of OBS. Images were selected from the website of Walkman Biomaterial Co., Ltd. OBS Ortho-Bridge system
Materials and Methods
Clinical Data
This retrospective analysis of existing clinical cases was approved by the institutional review board. There were 11 patients (nine men and two women) enrolled between July 2017 and May 2020. Detailed clinical patient parameters are shown in Table 1. The average age at enrollment was 37.7 years (range 18–54 years). All patients had closed fractures with the following causes of injury: (i) traffic accidents (nine patients) and (ii) falls from a significant height (two patients). Two patients had other fractures with multiple rib fractures and traumatic pneumonia, one had subarachnoid hemorrhage, one had a traumatic renal contusion, and one had traumatic contusions of the liver and spleen. According to the AO Foundation/Orthopaedic Trauma Association classification, there were seven type-A and four type-B femoral shaft fractures. All the patients were diagnosed by clinical symptomatology and radiography.
Preoperative Preparation
After admission, all the patients completed routine blood coagulation, blood biochemistry, and other blood tests. Tibial tubercle traction was performed prior to surgical treatment upon patient stabilization, except for three patients with craniocerebral injury, liver and spleen contusion, and severe hemopneumothorax. The remaining eight patients underwent surgery on the second day after the injury.
Surgical Procedure
The patient was placed in the supine position with general or epidural anesthesia. The center of the femoral posterolateral approach incision was the femoral fracture site, which was made layer by layer to expose the space and compartment between the lateral femoral muscles. The lateral femoral muscle was pulled up and sharply separated from its attachment point to expose the fracture site without stripping the periosteum. Blood clots were cleared at the fracture site and the soft tissue of the clamp. Longitudinal traction was used to correct the overlapping displacement, and the fracture was reduced and maintained via bone holding forceps. According to the fixation principle that the length of the plate should be 8–10 times that of the fracture area of the simple fracture, the appropriate bridging rod was selected. The sliding module was placed at the distal and proximal ends of the fracture according to the position of the LCP nail holder. Furthermore, key screws were inserted into the proximal and distal nail holes of the adjacent fractures after applying compression forceps. These were screwed into the clamps to tighten the connection rod and clamp, and the final fixation effect is shown in Fig. 2. Anatomical reduction of the femur fractures was confirmed through C-arm fluoroscopy. Finally, the wound was flushed and sutured while placing the drainage tube.
Postoperative Management
Drainage was removed on the second postoperative day. Weight-bearing function exercise began 1-month post-operation. Weight-bearing was gradually increased with regular radiography review. Once the callus passed through the fracture gap, it could be completely loaded.
Evaluation Criteria
X-ray examinations were performed every month post-operation to assess fracture healing until a solid continuous callus appeared. Radiographic union was defined as the presence of bridging callus at three of the following four cortices: (i) anteroposterior medial, (ii) lateral, (iii) lateral anterior, and (iv) posterior cortices [11]. Joint function and knee function were measured using the Harris Hip Score (HHS) [12] and Knee Society Score (KSS) [13], respectively, to evaluate subjective and objective quality of life.
Biomechanical Experiment
Experimental Materials The experimental control group used a 12-hole 4.5-mm LCP, which is commonly used for femoral shaft fractures (DePuy Synthes, Raynham, MA). Its unique combination hole is useful for placing common cortical bone screws in the sliding hole depending on the need for sliding compression. It can also be used to place locking screws for fixation, which better reflects the real clinical situation. Tianjin Walkman Biomaterials Co., Ltd. manufactured the OBS, which is composed of connecting rods and fixed blocks. The connecting rod of the experimental group was cut to the same length as the 12-hole LCP.
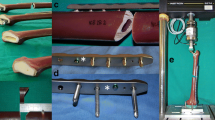
Method Both OBS and LCPs were randomly divided into four groups, each with six pieces. The LCP group was randomly divided into the following: (i) empty hole group, (ii) empty two-hole group, (iii) empty three-hole group, and (iv) empty four-hole group. The OBS experimental group was set up according to the distance between the two screws, and the sliding module was placed and fixed with the screws in the same position as the LCP group. The distance between the two screws is referred to as the critical screw distance. Each construct was placed in an MTS E45.105 microcomputer-controlled electronic universal testing machine (EA-002; MTS, Eden Prairie, MN) for static three-point bending tests while maintaining temperature at 20 °C. The position of the lower fulcrum of this machine is similar to that of the two key screws of each group, and its midpoint is referred to as the force application point. The initial bending load was 50 N, which was gradually increased to 1000 N at a displacement speed of 2 mm/min (Fig. 3). The sensor is linked to a computer, which displays the displacement and bending force synchronously. The fixed stiffness value (N/mm) was recorded for each group. Stiffness refers to the ability of a material or structure to resist elastic deformation when force is applied. It also characterizes the material’s degree of elastic deformation.
Biomechanics three-point bending test. a Two screws are simulated to be placed in the bilateral sliding compression holes of LCP. OBS places screws according to the distribution of LCP screws with a key screw distance of 23 mm; b two screws are placed in locking holes on both sides of fracture ends with a distance of two holes from each other, and OBS screw positioning is performed according to the position of the LCP screws with a key screw distance of 49 mm; c, d static three-point bending test for LCP and OBS, respectively. OBS Ortho-Bridge system, LCP locking compression plate
Statistics
Statistical analysis was completed using Microsoft Excel 2013 (Microsoft, Redmond, WA) and the R statistical environment (R Foundation, Vienna, Austria). The t test and χ2 test were used to compare continuous outcomes and categorical variables, respectively. Statistical significance was established at P < 0.05.
Results
The average operation time and blood loss were 82 min (62–106 min) and 252.8 mL (212–326 mL), respectively. After OBS surgery, no complications (i.e., necrosis of incision, infection, or loosening and breakage of the implants) were found. All 11 patients were followed for an average of 12.6 months (8–20 months) and showed excessive callus growth on the contralateral side of the OBS at the first review (1–1.8 months post-surgery). All the patients presented with second fracture healing with an average fracture healing time of 4.5 months (3–5 months). The evaluation of limb function was performed according to the HHS and KSS; nine cases were excellent, and two cases were good. The typical case is shown in Fig. 4 (patient 1).
Typical case of a femoral fracture. a Preoperative X-ray analysis of B2 fracture of femoral shaft. b During the operation, the OBS sliding module is placed, and screws are inserted according to the distribution of nail holes of LCP. c Intraoperative C-arm fluoroscopy shows that the distribution of OBS screws is consistent with that of screw holes. d, e AP and LAT X-ray immediately after operation. f One month after the surgery, AP X-ray showed obvious callus growth of the contralateral side of OBS. g, h AP and LAT X-rays showed fracture healing at 3.5 months after surgery. OBS Ortho-Bridge system, LCP locking compression plate
Analysis of Static Three-Point Bending Test Results
Once the key screws were placed in the compression holes on both sides of the LCP at the fracture end (distance: 22 mm), a three-point static test was performed. The stiffness of the OBS and LCP was 10,637.7 ± 714.2 and 11,903.5 ± 1047.0 N/mm, respectively. The stiffness of the OBS and LCP was 7709.0 ± 200.1 and 7107.1 ± 263.3 N/mm, respectively, when placed at both ends of the fracture, 1 hole apart (distance: 34 mm). When the key screw distance was 22–34 mm, the stiffness of the OBS was significantly lower than that of the LCP (P < 0.05). When the screw was placed at both ends of the fracture, two holes apart (distance: 49 mm), the stiffness of the OBS and LCP was 2946.4 ± 91.3 and 3870.2 ± 67.3 N/mm, respectively. When placed at both ends of the fracture, three holes apart (distance: 66 mm), the stiffness of the OBS and LCP was 2065.3 ± 35.8 and 1494.1 ± 92.2 N/mm, respectively. When the key screw was placed at both ends of the fracture, four holes apart (distance: 82 mm), the stiffness of the OBS and LCP was 750.8 ± 6.3 and 973.9 ± 9.3 N/mm, respectively. According to these results, it can be concluded that the stiffness of the LCP and OBS decreased significantly when the key screw distance was more than two holes (i.e., 49–82 mm), and the LCP was slightly stronger than the OBS (P < 0.05) (Table 2).
Discussion
In this study, following the treatment of simple femoral shaft fractures with the OBS, we found that the process of fracture healing was different from that of plate fixation. We noticed that the callus grew rapidly, and all patients achieved secondary fracture healing.
Intramedullary nailing fixation is the gold standard of treatment for adult femoral shaft fractures; however, internal plate fixation is particularly advantageous when intramedullary nailing is contraindicated or when there is a lack of surgical experience and image intensifier [14,15,16]. For patients with head and chest injuries, the best treatment for fractures of the lower limbs is still controversial [17]. Considering the technical difficulty of closed reduction, anatomically reducing fractures and the gaps between fracture fragments cannot be eliminated, especially severe comminuted or segmental fractures, which are still significant challenges for orthopedic surgeons [18, 19]. Locking plates are recommended as they can bridge major fractures and avoid excessive gaps between fragments [20].
The OBS adopts a locking bracket structure with rod connection and a nail–clamp combination, which can evenly distribute stress in the working area through the elastic and stress conduction characteristics of the rod to effectively alleviate the stress concentration and shielding, reducing the rupture risk of the internal fixation, and achieving a micro-motion effect of the fracture end. The OBS does not require, or rarely requires, stripping of the periosteum to fix the fracture. The OBS is like a built-in external fixator, which directly spans the fracture site and avoids compression of the periosteum and cortical bone. In the case of weight-bearing, this technique is in a state of continuous and dynamic compression, and the longitudinal compressive stress stimulates the formation of callus to avoid stress shielding and prevent osteoporosis. The healing time and healing process of OBS and femoral intramedullary nail are basically similar [21, 22]. The healing time of OBS for femoral shaft fractures was not significantly different from that of intramedullary nailing, and it was not inferior to intramedullary nailing for femoral shaft fractures.
The size of the fracture fragment gap and the initial stability of the fracture site are key factors that determine the type of healing (i.e., primary or secondary) and time of recovery. The stiffness of the fixation structure is the main determinant of the movement of the fracture site, thus affecting the mechanism and progress of fracture healing. Therefore, fracture fixation should follow the following principles: (i) if secondary healing is the purpose of simple fracture healing, the movement of fragments along the axial direction is conducive to the formation of cartilage callus [23], and (ii) the gap and movement amplitude should be kept small (range 0.2–1 mm; fracture gap < 2 mm). Other fracture modes (i.e., spiral fracture and multiple fragments) can withstand higher strain amplitudes.
Primary healing occurs once the fracture is stable and refers to intramembrane ossification, which is the direct transition of mesenchymal cells to osteoblasts [24]. Type A and B femoral fractures were fixed with the OBS, and excessive callus formation was found on the contralateral side of the internal fixator. This was quite different from plate fixation, which piqued our curiosity. Therefore, OBS fixation was performed in suitable patients with simple femoral fracture, and the sliding module of the OBS was screwed according to the layout of plates and screws. All patients presented with excessive contralateral callus growth. Thus, we conducted the biomechanical static three-point bending test to compare the biomechanics of the OBS and LCPs. The results showed that the OBS was less stiff than the LCP when the distance between the compression screw hole and the remaining hole is selected at both ends of the fracture. Specifically, the key screw distance (i.e., the distance between the screws less proximal and distal to the fracture) of the OBS was 3 ± 1 cm, which was significantly different from that of the LCP. The OBS was significantly more elastic than the LCP when using this distance. OBS application for fracture fixation was relatively stable. In the early stage of fracture fixation, axial stimulation and mechanical movement of the fracture end would be produced during partial load bearing, which stimulates callus growth and fracture healing. During the follow-up period, abundant callus formed during OBS fracture fixation according to the principle of relative stability. Due to the plate-screw connection’s rigidity, the locking plate produced less bone stress, which may inhibit interfragmentary movement to a range inappropriate for optimal indirect fracture healing. The stiffness of the fixation construct is the principal determinant of fracture site movement, which mainly affects the mechanism and progress of fracture healing [25, 26]. This can be achieved by applying axial micro-movements on the implant and changing the mechanical strain on healing tissues [27]. When a simple fracture is fixed with the OBS, its stiffness is lower than that of the LCP within a certain distance of the key screw. This can also produce axial micro-motion to stimulate fracture healing and lead to secondary healing with rich callus growth.
However, several limitations are acknowledged in this study. The study is a single-center retrospective case study, the sample number is relatively small, and with a short follow-up time, thus, the results of this study may not adequately reveal the characteristics of OBS in the treatment of femoral fractures. In future research, with the continuous improvement of patients' recognition, there will be more and more cases, which can better improve the clinical efficacy of OBS in the treatment of femoral fractures.
Conclusion
Applying OBS at the femoral shaft fracture site reduced the time for bone consolidation and promoted earlier and tri-plane uniform callus formation that could indicate faster reconstruction of the fracture site. This is particularly interesting for simple fracture patterns. Thus far, these fracture patterns are completely different from the healing process of LCP construct fixation. These are instances of secondary fracture healing or other healing patterns, which necessitate further investigation.
Availability of Data and Materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Enninghorst, N., McDougall, D., Evans, J. A., Sisak, K., & Balogh, Z. J. (2013). Population-based epidemiology of femur shaft fractures. Journal of Trauma and Acute Care Surgery, 74, 1516–1520. https://doi.org/10.1097/TA.0b013e31828c3dc9
Mills, L., Tsang, J., Hopper, G., Keenan, G., & Simpson, A. H. (2016). The multifactorial aetiology of fracture nonunion and the importance of searching for latent infection. Bone & Joint Research, 5, 512–519. https://doi.org/10.1302/2046-3758.510.BJR-2016-0138
Wu, K. J., Li, S. H., Yeh, K. T., Chen, I. H., Lee, R. P., Yu, T. C., et al. (2019). The risk factors of nonunion after intramedullary nailing fixation of femur shaft fracture in middle age patients. Medicine (Baltimore), 98, e16559. https://doi.org/10.1097/MD.0000000000016559
Šmejkal, K., Lochman, P., Trlica, J., Novotný, P., Šimek, J., & Dědek, T. (2015). Impaired healing after surgery for femoral fractures. Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca, 82, 358–3563. in Czech.
Neumann, M. V., Südkamp, N. P., & Strohm, P. C. (2015). Management of femoral shaft fractures. Acta Chirurgiae Orthopaedicae et Traumatologiae Cechoslovaca, 82, 22–32.
El Beaino, M., Morris, R. P., Lindsey, R. W., & Gugala, Z. (2019). Biomechanical evaluation of dual plate configurations for femoral shaft fracture fixation. BioMed Research International, 2019, 5958631. https://doi.org/10.1155/2019/5958631
Testa, G., Aloj, D., Ghirri, A., Petruccelli, E., Pavone, V., & Massé, A. (2017). Treatment of femoral shaft fractures with monoaxial external fixation in polytrauma patients. F1000Res, 6, 1333. https://doi.org/10.12688/f1000research.11893.1
Alhammoud, A., Maaz, B., Alhaneedi, G. A., & Alnouri, M. (2019). External fixation for primary and definitive management of open long bone fractures: The Syrian war experience. International Orthopaedics, 43, 2661–2670. https://doi.org/10.1007/s00264-019-04314-0
Kang, L., Liu, H., Ding, Z., Ding, Y., Hu, W., & Wu, J. (2020). Ipsilateral proximal and shaft femoral fractures treated with bridge-link type combined fixation system. Journal of Orthopaedic Surgery and Research, 15, 399. https://doi.org/10.1186/s13018-020-01929-7
Wang, D. X., Xiong, Y., Deng, H., Jia, F., Gu, S., Liu, B. L., et al. (2014). Biomechanical analysis and clinical effects of bridge combined fixation system for femoral fractures. Proceedings of the Institution of Mechanical Engineers. Part H, 228, 899–907. https://doi.org/10.1177/0954411914548866
Morshed, S. (2014). Current options for determining fracture union. Advances in Medicine. https://doi.org/10.1155/2014/708574
Dettoni, F., Pellegrino, P., La Russa, M. R., Bonasia, D. E., Blonna, D., Bruzzone, M., et al. (2015). Validation and cross cultural adaptation of the Italian version of the Harris Hip Score. Hip International, 25, 91–97. https://doi.org/10.5301/hipint.5000184
Acharya, K. N., & Rao, M. R. (2006). Retrograde nailing for distal third femoral shaft fractures: A prospective study. Journal of Orthopaedic Surgery (Hong Kong), 14, 253–258. https://doi.org/10.1177/230949900601400305
Rollo, G., Ronga, M., Bonura, E. M., Erasmo, R., Bisaccia, M., Pichierri, P., et al. (2020). Surgical treatment of multifragmentary segmental femur shaft fractures with ORIF and bone graft versus MIPO: a prospective control-group study. Med Glas (Zenica), 17, 498–508. https://doi.org/10.17392/1150-20
Adeel, M., Zardad, S., Jadoon, S. M., Younas, M., & Shah, U. (2020). Outcome of open interlocking nailing in closed fracture shaft of femur. Journal of Ayub Medical College Abbottabad, 32(4), 546–550.
Angelini, A. J., Livani, B., Flierl, M. A., Morgan, S. J., & Belangero, W. D. (2010). Less invasive percutaneous wave plating of simple femur shaft fractures: A prospective series. Injury, 41(6), 624–628. https://doi.org/10.1016/j.injury.2010.01.101
Mrozek, S., Gaussiat, F., & Geeraerts, T. (2013). The management of femur shaft fracture associated with severe traumatic brain injury. Annales Francaises d’Anesthesie et de Reanimation, 32, 510–515. https://doi.org/10.1016/j.annfar.2013.07.010
Lin, S. J., Chen, C. L., Peng, K. T., & Hsu, W. H. (2014). Effect of fragmentary displacement and morphology in the treatment of comminuted femoral shaft fractures with an intramedullary nail. Injury, 45, 752–756. https://doi.org/10.1016/j.injury.2013.10.015
Krappinger, D., Wolf, B., Dammerer, D., Thaler, M., Schwendinger, P., & Lindtner, R. A. (2019). Risk factors for nonunion after intramedullary nailing of subtrochanteric femoral fractures. Archives of Orthopaedic and Trauma Surgery, 139, 769–777. https://doi.org/10.1007/s00402-019-03131-9
Cheng, T., Xia, R., Yan, X., & Luo, C. (2018). Double-plating fixation of comminuted femoral shaft fractures with concomitant thoracic trauma. Journal of International Medical Research, 46, 440–447. https://doi.org/10.1177/0300060517720317
Timmerman, L. A., & Rab, G. T. (1993). Intramedullary nailing of femoral shaft fractures in adolescents. Journal of Orthopaedic Trauma, 7(4), 331–337. https://doi.org/10.1097/00005131-199308000-00008
Zhou, Z. T., Song, Y. C., Zhou, X. Z., Zhou, H. B., Luo, Z. P., & Dong, Q. R. (2015). Femoral midshaft fractures: Expandable versus locked nailing. Orthopedics, 38(4), e314–e318. https://doi.org/10.3928/01477447-20150402-60
Hente, R., Füchtmeier, B., Schlegel, U., Ernstberger, A., & Perren, S. M. (2004). The influence of cyclic compression and distraction on the healing of experimental tibial fractures. Journal of Orthopaedic Research, 22, 709–715. https://doi.org/10.1016/j.orthres.2003.11.007
Bahney, C. S., Zondervan, R. L., Allison, P., Theologis, A., Ashley, J. W., Ahn, J., et al. (2019). Cellular biology of fracture healing. Journal of Orthopaedic Research, 37, 35–50. https://doi.org/10.1002/jor.24170
Hoffmann, M. F., Burgers, T. A., Mason, J. J., Williams, B. O., Sietsema, D. L., & Jones, C. B. (2014). Biomechanical evaluation of fracture fixation constructs using a variable-angle locked periprosthetic femur plate system. Injury, 45, 1035–1041. https://doi.org/10.1016/j.injury.2014.02.038
Ma, C. H., Wu, C. H., Jiang, J. R., Tu, Y. K., & Lin, T. S. (2017). Metaphyseal locking plate as an external fixator for open tibial fracture: clinical outcomes and biomechanical assessment. Injury, 48/2, 501–505. https://doi.org/10.1016/j.injury.2017.06.008 published correction appears in Ma CH, Wu CH, Jiang JR, Tu YK, Lin TS. Injury 2017;48:1861.
Iobst, C. A., Milne, E., Khoury, A., Ingwer, Z., & Latta, L. (2021). A novel way to dynamize a spatial frame and optimize fracture healing. Injury, 52, 106–108. https://doi.org/10.1016/j.injury.2020.10.007
Acknowledgements
The biomechanical analysis was completed in Tianjin Walkman Biomaterial Co., Ltd. (Newton Laboratory).
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YQ: writing the paper, data analysis, and collection. YL: writing the paper, literature search, and data analysis.LY:data collection and literature search. GZ: data collection. QZ: designing the biomechanical experiment. ZL: participated in designing and conducting the biomechanical experiment. WW: data collection, performed surgeries, and managed the research team. All authors of this original work have directly participated in its conception and authorship and have read and approved the final version submitted.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Ethics Approval and Consent to Participate
All methods were performed in accordance with the relevant guidelines and regulations. This study was a retrospective and clinical study and approved by The First Affiliated Hospital of Shandong First Medical University institutional review board. Written informed consent was obtained from individual participants or their guardians.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Qi, Y., Yao, L., Long, Y. et al. Effectiveness and Biomechanical Analysis of the Ortho-Bridge System on Femoral Fracture Healing: A Retrospective Analysis. JOIO 56, 1795–1803 (2022). https://doi.org/10.1007/s43465-022-00687-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-022-00687-4