Abstract
Purpose
To evaluate the trends and patterns of cervical degenerative disc disease in the cervical spine in different age groups of symptomatic patients.
Methods
Overall, 1300 symptomatic patients who had undergone cervical spine MRI from February 2019 to November 2021 were included. Pfirrmann grading was used to evaluate the IVD degeneration. Patients were divided into five groups based on age: group 1 from 20 to 29 years, group 2 from 30 to 39 years, group 3 from 40 to 49 years, group 4 from 50 to 59 years, and group 5 from 60 years and above. The patterns, severity, and the number of degenerated levels in each age group were analysed.
Results
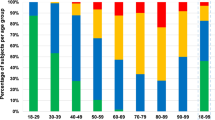
The total number of degenerated IVDs (grades IV and V) increased significantly with age, ranging from 76 (4.9%) in group 1 to 677 (43.4%) in group 5. The most common degenerated levels were C2/3 (25% of the total degenerated levels) in group 1, C5/6 (29.0%) in group 2, C5/6 (33.1%) in group 3, C5/6 (31.3%) in group 4, C5/6 (24.8%), in group 5. The number of degenerated IVDs increased significantly with age (P < 0.001). In patients with two or more degenerated levels, contiguous-level disc degeneration was more common than skip lesions.
Conclusion
This study evaluated the severity and pattern of cervical disc degeneration at each level in different age groups. The severity and number of degenerated levels increased significantly with increased age. Adjacent-level degeneration is more common than skip lesions in patients with more than one-level degeneration.





Similar content being viewed by others
References
Bogduk N, Mercer S (2000) Biomechanics of the cervical spine. I: Normal kinematics. Clin Biomech (Bristol, Avon) 15(9):633–648
Tan LA, Riew KD, Traynelis VC (2017) cervical spine deformity-part 1: Biomechanics, radiographic parameters, and classification. Neurosurgery 81(2):197–203. https://doi.org/10.1093/neuros/nyx249
Yang L, Chen J, Yang C, Pang X, Li D, Wu B, Wu Y, Lu X, Xu J, Chen X, Peng B (2018) Cervical intervertebral disc degeneration contributes to dizziness: a clinical and immunohistochemical study. World Neurosurg 119:e686–e693. https://doi.org/10.1016/j.wneu.2018.07.243
Safiri S, Kolahi AA, Hoy D, Buchbinder R, Mansournia MA, Bettampadi D, Ashrafi-Asgarabad A, Almasi-Hashiani A, Smith E, Sepidarkish M, Cross M, Qorbani M, Moradi-Lakeh M, Woolf AD, March L, Collins G, Ferreira ML (2020) Global, regional, and national burden of neck pain in the general population, 1990–2017: systematic analysis of the Global Burden of Disease Study 2017. BMJ 368:m791. https://doi.org/10.1136/bmj.m791
Miyazaki M, Hong SW, Yoon SH, Morishita Y, Wang JC (2008) Reliability of a magnetic resonance imaging-based grading system for cervical intervertebral disc degeneration. J Spinal Disord Tech 21(4):288–292. https://doi.org/10.1097/BSD.0b013e31813c0e59
Schubert AK, Smink JJ, Arp M, Ringe J, Hegewald AA, Sittinger M (2018) Quality assessment of surgical disc samples discriminates human annulus fibrosus and nucleus pulposus on tissue and molecular level. Int J Mol Sci. https://doi.org/10.3390/ijms19061761
Dowdell J, Erwin M, Choma T, Vaccaro A, Iatridis J, Cho SK (2017) Intervertebral Disk Degeneration and Repair. Neurosurgery 80(3S):S46–S54. https://doi.org/10.1093/neuros/nyw078
Weidenbaum M, Foster RJ, Best BA, Saed-Nejad F, Nickoloff E, Newhouse J, Ratcliffe A, Mow VC (1992) Correlating magnetic resonance imaging with the biochemical content of the normal human intervertebral disc. J Orthop Res 10(4):552–561. https://doi.org/10.1002/jor.1100100410
Benneker LM, Heini PF, Alini M, Anderson SE, Ito K (2005) 2004 Young Investigator Award Winner: vertebral endplate marrow contact channel occlusions and intervertebral disc degeneration. Spine 30(2):167–173. https://doi.org/10.1097/01.brs.0000150833.93248.09 (Phila Pa 1976)
Adams MA, Roughley PJ (2006) What is intervertebral disc degeneration, and what causes it? Spine 31(18):2151–2161. https://doi.org/10.1097/01.brs.0000231761.73859.2c (Phila Pa 1976)
Daffner SD, Xin J, Taghavi CE, Hymanson HJ, Mudiyam C, Hongyu W, Wang JC (2009) Cervical segmental motion at levels adjacent to disc herniation as determined with kinetic magnetic resonance imaging. Spine 34(22):2389–2394. https://doi.org/10.1097/BRS.0b013e3181b20054 (Phila Pa 1976)
Kim CH, Hwang JM, Park JS, Han S, Park D (2018) Predictability of severity of disc degeneration and disc protrusion using horizontal displacement of cervical dynamic radiographs: a retrospective comparison study with MRI. Medicine (Baltimore) 97(25):e11098. https://doi.org/10.1097/MD.0000000000011098
Suzuki A, Daubs MD, Hayashi T, Ruangchainikom M, Xiong C, Phan K, Scott TP, Wang JC (2018) Patterns of cervical disc degeneration: analysis of magnetic resonance imaging of over 1000 symptomatic subjects. Global Spine J 8(3):254–259. https://doi.org/10.1177/2192568217719436
Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, Halabi S, Turner JA, Avins AL, James K, Wald JT, Kallmes DF, Jarvik JG (2015) Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol 36(4):811–816. https://doi.org/10.3174/ajnr.A4173
Gore DR, Sepic SB, Gardner GM (1986) Roentgenographic findings of the cervical spine in asymptomatic people. Spine 11(6):521–524. https://doi.org/10.1097/00007632-198607000-00003 (Phila Pa 1976)
Lehto IJ, Tertti MO, Komu ME, Paajanen HE, Tuominen J, Kormano MJ (1994) Age-related MRI changes at 0.1 T in cervical discs in asymptomatic subjects. Neuroradiology 36(1):49–53. https://doi.org/10.1007/bf00599196
Matsumoto M, Fujimura Y, Suzuki N, Nishi Y, Nakamura M, Yabe Y, Shiga H (1998) MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br 80(1):19–24. https://doi.org/10.1302/0301-620x.80b1.7929
Simpson AK, Biswas D, Emerson JW, Lawrence BD, Grauer JN (2008) Quantifying the effects of age, gender, degeneration, and adjacent level degeneration on cervical spine range of motion using multivariate analyses. Spine 33(2):183–186. https://doi.org/10.1097/BRS.0b013e31816044e8 (Phila Pa 1976)
Wilder FV, Fahlman L, Donnelly R (2011) Radiographic cervical spine osteoarthritis progression rates: a longitudinal assessment. Rheumatol Int 31(1):45–48. https://doi.org/10.1007/s00296-009-1216-9
Nakashima H, Yukawa Y, Suda K, Yamagata M, Ueta T, Kato F (2015) Cervical Disc Protrusion Correlates With the Severity of Cervical Disc Degeneration: A Cross-Sectional Study of 1211 Relatively Healthy Volunteers. Spine 40(13):E774-779. https://doi.org/10.1097/BRS.0000000000000953 (Phila Pa 1976)
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26(17):1873–1878. https://doi.org/10.1097/00007632-200109010-00011 (Phila Pa 1976)
Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S (1990) Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. a prospective investigation. J Bone Joint Surg Am 72(8):1178–1184
Virk SS, Niedermeier S, Yu E, Khan SN (2014) Adjacent segment disease. Orthopedics 37(8):547–555. https://doi.org/10.3928/01477447-20140728-08
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4(6 Suppl):190S-194S. https://doi.org/10.1016/j.spinee.2004.07.007
Tobert DG, Antoci V, Patel SP, Saadat E, Bono CM (2017) Adjacent segment disease in the cervical and lumbar spine. Clin Spine Surg 30(3):94–101. https://doi.org/10.1097/BSD.0000000000000442
Shifflett GD, Iyer S, Derman PB, Louie PK, An HS (2018) Upper cervical radiculopathy: the hidden pathology of the spine. Spine Surg Relat Res 2(2):93–97. https://doi.org/10.22603/ssrr.2017-0077
Kalichman Leonid, Hunter David J (2008) The genetics of intervertebral disc degeneration.Familial predisposition and heritability estimation. Joint Bone Spine 75(4):383–387. https://doi.org/10.1016/j.jbspin.2007.11.003
Elfering A, Semmer N, Birkhofer D, Zanetti M, Hodler J, Boos N (2002) Risk factors for lumbar disc degeneration: a 5-year prospective MRI study in asymptomatic individuals. Spine 27(2):125–134. https://doi.org/10.1097/00007632-200201150-00002 (Phila Pa 1976)
Battie MC, Videman T, Gill K, Moneta GB, Nyman R, Kaprio J, Koskenvuo M (1991) Volvo Award in clinical sciences Smoking and lumbar intervertebral disc degeneration: an MRI study of identical twins. Spine 16(9):1015–1021 (Phila Pa 1976)
Samartzis D, Karppinen J, Chan D, Luk KD, Cheung KM (2012) The association of lumbar intervertebral disc degeneration on magnetic resonance imaging with body mass index in overweight and obese adults: a population-based study. Arthritis Rheum 64(5):1488–1496. https://doi.org/10.1002/art.33462
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest related to this study. Disclosures outside of submitted work: ZB- consultancy: Cerapedics (past); Research Support: SeaSpine (past, paid to the institution), Next Science (past, paid directly to institution), Medical Metrics (past, paid directly to institution), NIH SBIR Subaward (past, paid to institution); North American Spine Society: committee member; Lumbar Spine Society: Co-chair Educational Committee, AOSpine Knowledge Forum Degenerative: Associate member; AOSNA Research committee- committee member; JCW - royalties: SeaSpine, Depuy, Zimmer; consulting - Precision OS (no money paid); expert testimony; AO Foundation Board (honorarium), National Spine Health Foundation (volunteer); stocks/personal investment: PearlDiver, Bone Biologics, Surgitech; Fellowship Funding (paid to institution): AO Foundation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mesregah, M.K., Repajic, M., Mgbam, P. et al. Trends and patterns of cervical degenerative disc disease: an analysis of magnetic resonance imaging of 1300 symptomatic patients. Eur Spine J 31, 2675–2683 (2022). https://doi.org/10.1007/s00586-022-07336-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07336-2