Abstract
Background
Technology and its use within mental health services has advanced dramatically over recent years. Opportunities for mental health services to utilise technology to introduce novel, effective, and more efficient means of delivering assessment, and treatment are increasing.
Objective
The current rapid-evidence paper reviews evidence regarding the introduction of novel technology to support young people’s mental health and psychological well-being.
Methods
A rapid evidence review was conducted. PSYCHINFO and CINAHL were searched for research articles between 2016 and 2021 that were specific to young people, mental health, and technology developments within this domain. N = 27 studies which explored the introduction, feasibility, and value of technology for mental health purposes were included in a narrative synthesis. Quality or risk of bias analyses were not completed.
Results
Overall, technological advancements in young people’s care were considered positive and engaging for young people. Factors including resources, efficiency of care, engagement, therapeutic effectiveness, ethical considerations, therapeutic alliance, and flexibility were considered within this review. Nevertheless, potential barriers include clinician concerns, socioeconomic factors, and motivation.
Conclusion
Effective and sustained use of technology within young people’s mental health services will depend on the technology’s usability, efficiency, and ability to engage young people. This paper expands on existing research by reviewing a broader range of technology proposed to support young people’s mental health and well-being. This will assist in the application of novel technological advancements by indicating effectiveness, preferences, potential barriers, and recommendations for the feasibility and efficacy of introducing technology into young people’s services.
Similar content being viewed by others
Introduction
Technology and its use within psychiatric services has advanced dramatically since the infamous television link between Nebraska Psychiatric Institute and Norfolk State Hospital was established for psychiatric consultations over fifty years ago (Nesbitt, 2012). Technological developments have also become increasingly necessary due to the effects of the COVID-19 pandemic (Comer et al., 2021). ‘Telehealth’ or ‘tele-psychotherapy’ is well established within mental health services and is a validated method of conducting psychotherapy, as measured by the National Institute of Mental Health (Magnavita, 2018).
Services can now use devices to collect biometric data, such as heart rate or sleep, and electronic health record apps are now used routinely to collate and securely store data exchanges between service-users and health practitioners (Magnavita, 2018). The frequency of publications regarding ‘connected mental health’ examining electronic methods of delivering mental-health orientated support has increased from fewer than five publications per year in 2011, to over 70 publications in the year of 2019; with researchers anticipating that this trend will continue (Ouhbi et al., 2020). Abundant opportunities are available for mental health services to introduce novel, effective, and more efficient means of delivering assessment, intervention, and treatment using technology.
Mobile-based technologies have increasingly been examined for supporting the care of both young people and adults (Inal et al., 2020). Systematic reviews and meta-analyses have provided evidence for the effectiveness of internet-based Cognitive Behavioural Therapy (iCBT) for the treatment of depression and anxiety in adults (e.g., Etzelmueller et al., 2020; Luo et al., 2020). Similarly, a systematic review examining online mental health support for young people found that 64% of telehealth interventions were effective in managing anxiety and depression in young people, in comparison to control conditions (Zhou et al., 2021).
In a review conducted by Hollis and colleagues (2017) it was argued that out of all of the fields within mental health, the opportunities in relation to digital transformation are the greatest within child and adolescent services. Young people are increasingly being invited to be involved in testing new technology that could support or assist with psychosocial provision (Drissi et al. 2020). A systematic review of randomised control trials (RCTs) also found that digital interventions supporting treatment of depression in young people were more effective than no treatment (Garrido et al., 2019). Despite concerns that technology may have socially isolating effects, there are now evolving applications (apps) for supporting with loneliness (Ramo & Lim, 2021).
Practitioners are also encouraged to implement internet-based technology into their work in supporting youth mental health, as it can be a valuable forum for enabling and maintaining social connectedness (Wu et al., 2016). This is further emphasised within the NHS Long Term Plan (NHS, 2019) which highlights the importance of technology development within healthcare. The NHS Long Term Plan refers to technology as the digitisation of care using computers and smartphones to provide patients with fast and convenient access to care. Virtual services can be used to provide advice and connect people to healthcare professionals. The plan also highlights the use of apps and online resources for mental health provision. With this in mind, the current paper defines technology as the use of digital resources to promote engagement in the context of mental health care. The Division of Clinical Psychology (DCP) Guidelines also indicate the necessity of technology developments within the context of COVID-19 (DCP, 2020).
A previous systematic review examining how technology has been used in mental health settings highlighted services can adopt novel advancements to support with obtaining patients’ attitudes, to support patient learning, reminders for service users, information, supportive messages, self-monitoring procedures, and to facilitate the operation of mental health services generally (Berrouiguet et al., 2016; Inal et al., 2020).
Not only can novel technology support individuals with health and social care needs, but technologies such as phone apps can also be used for psychological interventions (Inal et al., 2020). One example of this is the Wellness Recovery Action Plan (WRAP, Copeland, 2002) app. WRAP was developed by individuals with mental health difficulties and is currently recognised as an evidence-based practice designed to support individuals to develop strategies to create and maintain wellness within their lives. In 2018, the WRAP app was introduced to promote global implementation of WRAP wellness strategies, and has received positive feedback from users (WRAP, 2018). Mobile-based procedures have also been examined in relation to supporting people with schizophrenia, affective disorders, suicide prevention, substance abuse, eating disorders, anger, psychosis, headaches, sleep problems, stress, and neurodevelopmental disabilities among other psychiatric concerns (Inal et al., 2020). This further highlights the growing evidence-base in this area.
Analysis of user reviews, interviews and surveys has found that depression, technical issues, and fatigue can be barriers to use of technology that is designed to support mental health (Bourgouts et al., 2021). Contrastingly, having positive beliefs about mental health and help-seeking, the ability to integrate the technology into one’s daily life, as well as participating in user-research are known to facilitate engagement (Bourgouts et al., 2021; Jagosh et al., 2012; Orlowski et al., 2015). Customisable information, the ability to connect with others, guided interventions, activities of an appropriate length, good understanding of how to use technology, and confidence in the privacy and anonymity of the site are also factors that encourage engagement (Bourghouts et al., 2021).
One especially pertinent challenge for young people in terms of introducing new pieces of technology is ensuring that they are accessible and engaging. Engagement and adherence rates from young people can be low, and young people have been found to enjoy a “game-like” interactivity when using a device or app. Despite services promoting the use of technology to teach young people about mental health topics, educational materials can be perceived as less engaging by young people (Garrido et al., 2019). Although the “gamification” of mental health and wellbeing apps commonly overlaps with behaviour change frameworks, most of the gamification is not theory-driven (Cheng et al., 2019). It is important, therefore, that services do not focus only on the engagement and accessibility of the technology, at the detriment of theoretical integrity.
The emergence of the COVID-19 pandemic has precipitated rapid technological adaptation by many mental health services, as stipulated by the DCP COVID-19 guidance (DCP, 2020). Using video technology, team meetings and consultations have been able to continue remotely throughout the pandemic, with enhanced efficiency and attendance for some (DeFilippis et al., 2020; Oz & Crooks, 2020).
Psychologists have been advised to use digital alternatives to continue clinical work, but to be aware of any disadvantages that this could pose to different client groups. (The British Psychological Society, 2020). For example, psychologists are encouraged to facilitate access to relevant technology for service-users in instances where they do not have the correct equipment available, to use social media appropriately, and to ensure apps are safe, secure, and confidential (The British Psychological Society, 2020).
Undoubtedly, technological developments are occurring at a rapid rate within mental health care. In combination, the above evidence implies that the rapid adoption of novel technology should proceed with caution; considering both the utility and potential barriers involved in using technology to support young people’s care. Given the increasingly rapid adoption of technology due to the COVID-19 pandemic, and the drive for digitalisation of mental health care (NHS, 2019), services will benefit from an awareness of the existing literature prior to the implementation of new technologies within their services. The current rapid evidence review sought to collate existing research regarding the introduction of new technology for young people’s mental health and social care services. It was anticipated that the research will indicate any potential barriers, preferences, and recommendations for the feasibility and efficacy of introducing new technology into young people’s services.
Method
The qualitative rapid evidence review design used in the current study is based upon the provisional recommendations suggested by the Cochrane Rapid Reviews Methods Group (Garritty et al., 2020). Such recommendations originate from a team of methodologists with experience in review methods such as rapid reviews and systematic reviews. Rapid evidence reviews are a form of data synthesis that follow similar steps to systematic reviews but are designed to be completed under limited time constraints.
This study met criteria for service evaluation under criteria outlined by the Health Research Authority (HRA, 2021) and therefore did not require NHS Research Ethics Committee (REC) approvals. The study received local approval from CNTW NHS Foundation Trust Research, Innovation & Clinical Effectiveness team (Reference: SER-21–045). There are no conflicts of interest identified within this paper.
Inclusion Criteria
The following inclusion criteria was used to screen relevant research:
-
(i)
Must be a published research or evaluation article within a peer-reviewed journal that is relevant to child health and social care, or child psychology,
-
(ii)
Must be published within the last five years (July 2016–July 2021),
-
(iii)
Must be written in English language,
-
(iv)
Authors must be able to access the full text publicly or via their institution,
-
(v)
Must have a focus upon the introduction of technology that is new to a service (i.e., technology such as an App or tablet that a service has not used before) or technological developments (e.g., a different way of using a piece of technology within a service), that are designed to assist or support with mental health, or psychosocial care,
-
(vi)
Must be specific to young people (samples within the ages of school age to eighteen years, with an extension of this to twenty-five years for intellectual disability services).
Due to the aim of obtaining generalisable findings, the following studies were excluded:
-
(i)
Studies examining technology for specific health conditions (e.g., diabetes) and sensory impairments (e.g., hearing impairments or blindness).
-
(ii)
Studies examining technology for physical disabilities, or multiple and severe disabilities.
Search Terms
The following search terms were used for the two different databases searched: (‘child*’ or ‘young pe*’ or ‘adolescent*’) and (‘New’ or ‘Novel’) and (‘Technol*’ or ‘Device*’)r and (‘psychiatr*’ or ‘mental health’ or ‘psychol*’ or ‘learn*’).
Search Strategy
The search was limited to two databases: PSYCHINFO and CINAHL. One author conducted the search and screening process to prioritise time constraints for completion of the study. Using guidance from NHS trust Clinical Effectiveness Librarians, the search of the databases was conducted using the NICE Healthcare Databases Advanced Search resource. Search limits were applied in relation to date (July 2016–July 2021), format (research articles only), and language (English only). Titles and abstracts were screened to gauge whether the study met the inclusion criteria. The studies that were left after this process were screened as a full text. Full texts that could not be obtained via the trust resources were excluded. Reasons for exclusion during the full text screening phase were recorded.
Analysis
Quality appraisal of the included research was not conducted due to the limited time available within an active clinical service.
Data was extracted using the following categories: design; setting; aims; participants; type of technology; whether the study was focusing upon feasibility/acceptability/efficacy or exploring how the piece of technology could be used; intervention (if applicable); outcome measures, and results. The extracted data was tabulated using the categories as headings. Studies that had similarities in relation to technology or outcomes were grouped together during the tabulation process. Due to the heterogeneous nature of the research, findings were collated within the form of a narrative synthesis, following the guidelines of the Cochrane Rapid Reviews Methods Group (Garritty et al., 2020). The authors chose not to conduct a meta-analysis due to the anticipation that there would be insufficient quantitative data utilising the same outcome measures.
Findings
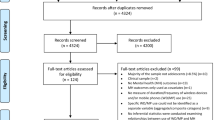
A total of n = 27 studies met the inclusion criteria and were included within the narrative synthesis. An overview of the included studies can be found within Appendix A. Appendix B outlines the number of studies excluded via a PRISMA flow chart. Studies explored the introduction, feasibility, and value of technology for mental health purposes. Studies excluded at the full-text stage of screening (n = 19) were excluded mostly due to the age group of the participants, including individuals that were older than eighteen years, and younger than UK school age (four years). One study was excluded as it examined technology specifically for the assessment of young people within countries experiencing war (Hashemi et al., 2017). The environmental specificities of this were not deemed sufficiently generalisable to include within this review.
Online platforms and websites appeared to be the most frequently examined within the literature for young people in relation to mental health, with 11 studies examining online platforms or websites specifically. Other studies utilised apps/games (n = 7), video-related technology (n = 2), SMS/phone calls (n = 2), other PC software (n = 1), a mixture of technology (n = 3), or other technology (n = 1). Most technologies facilitated some form of assessment, psychoeducation, mental health-oriented activities for young people, or a structured therapy.
For online and virtual therapies, interventions were mostly Cognitive Behavioural Therapy (CBT)-oriented. For example, Babiano-Espinosa and colleagues (2019) examined the feasibility and efficacy of internet-based CBT for young people with obsessive compulsive disorder (OCD), whilst Wozney and colleagues (2017) focused upon treatment outcomes for internet-based CBT and interpersonal therapy for young people with depression.
Young Person Engagement
Resources and Activities
One of the most apparent uses and benefits of the mental health-oriented technologies examined was the ability for young people to engage in interactive therapeutic activities, and in some instances to do this within their own time and space. Two studies described exercises to support coping skills and self-reflection on a web-based platform (Gabrielli et al., 2020; Kurki et al., 2018). For a wellness-promoting chatbot, such activities were oriented around emotional self-awareness, social awareness, interpersonal relationships, assertive communication, and other life skills (Gabrielli et al., 2020). General mental wellness activities were also featured, such as breathing techniques, muscle relaxation, and affective regulation (Davidson et al., 2019). Further activities were designed to solidify learning material, which was observed in relation to substance misuse prevention (Snijder et al., 2021), and in learning Dialectical Behaviour Therapy (DBT) skills (O’Grady et al., 2020).
Interactive and engaging activities also supported young person involvement and motivation. One study described engaging activities in relation to mood monitoring, encouraging young people to reflect upon their emotional triggers and the activities they had engaged in so far (Wozney et al., 2017). Similarly, O’Grady and colleagues (2020) described how the utilisation of a diary was adopted within their app for self-reflection during a therapeutic programme. In relation to activities, young people appeared to request motivational messages, relaxing videos, less text, and less detailed information generally (O’Grady et al., 2020). Activities that were game-like received particularly positive feedback from the young people; for instance, one young person described, “I liked this one [‘Affective Modulation’ chapter] because I got to spin the wheel and act the feeling … I really liked that one! I also liked the card game [‘What Do You Know?’] because they helped me get my feelings out.” (pg. 9–10, Davidson et al., 2019).
Enhancing Engagement
When considering engagement, there were apparent advantages in relation to technology’s ability to enhance therapeutic engagement when used as an adjunct to face-to-face therapy sessions. For example, this was pertinently demonstrated during an intervention examining TechConnect—an SMS messaging and telephone initiative for young people with depression who were receiving structured therapy sessions (Gearing et al., 2021). The initiative involved young people receiving SMS personalised messaging, consisting of eight weekly messages designed to target health beliefs that influence decision making in relation to engagement (e.g., self-efficacy and perceived barriers). This also involved three telephone calls made by facilitators to the young person’s parents following a semi-structured script. Almost all (90 percent) of the young people receiving TechConnect attended all eight therapy sessions, in comparison to 40 percent of young people that were part of a control group, illustrating the potential positive impact of technology on engagement.
Using technology to facilitate psychological assessment could also promote greater engagement from young people. An app for tablets was used to deliver the WellSEQ (Wellbeing in Special Education Questionnaire), a novel questionnaire for individuals with special educational needs, which examines mental health, peer relations and conflict, school environment, and the family environment (Boström et al., 2016). High response rates were received from the young people when testing the app, indicating positive engagement. Technology-assisted interactions may also reduce feelings of embarrassment or shame. For example, a review of technology-empowered CBT for individuals with OCD highlighted that parents and practitioners believed this would be a useful tool for young people that were embarrassed to talk to a practitioner about their problems (Wolters et al., 2017). It was thought that the technology could enhance adherence via enriching the therapeutic experience and supporting motivation.
Technological interventions can also offer enhanced engagement due to the game-like nature that can be adopted, contrasting what can be perceived as invasive traditional paper methods. For example, a wellness initiative created as an online game was specifically designed to offer non-invasive and effective assessment of socio-emotional functioning without the laboriousness of standard traditional psychometrics (Day et al., 2019). Encouragingly, the authors concluded that the game appeared successful in serving this function. Similarly, digital phenotyping has been highlighted as a non-invasive measure, demonstrating how assessment and intervention can occur without the need for interview-style questioning (Sequeira et al., 2019). This method uses accelerometers and other smart devices to support in the prediction of depression relapses in young people, without the need for invasive or time-consuming psychometric assessments. The review highlighted that the current research on digital phenotyping is too diverse in terms of outcome measures for results to be conclusive, however, the potential advantages of this method appear to warrant further research (Sequeira et al., 2019).
The development of the technology itself also relied on the engagement of young people in some cases. For instance, co-production from young people of specific ethnic origin enabled an informative substance-misuse prevention app to be culturally sensitive (Aboriginal and Torres Strait Islander young people; Snijder et al., 2021). A life-skills and wellness coaching intervention was also developed from young person input and focus groups (Gabrielli et al., 2020). Young people also supported in the development of a platform incorporating assessment, shared decision making, and routine evaluations (Rowe et al., 2020). Input from young people who access services can also facilitate the accessibility and personalisation of substance misuse online platforms or websites (Marsch & Borodovsky, 2016).
Nevertheless, technology-based interventions are not exempt from the challenges of non-adherence and drop-out. Wolters et al., (2017) listed compliance and non-respondence as pertinent challenges of technologically empowered CBT interventions. Additionally, social media was described as an untapped resource that could be valuable in capturing the engagement of young people, however, it does not appear to be widely used currently (Marsch & Borodovsky, 2016). Thus, there are several advantages in relation to technology for engagement of young people, however this requires further exploration and the existing engagement issues are not completely resolved.
Efficiency of Care
Technologies such as apps, websites, and other online platforms were described as effectively assessing and managing risk for vulnerable young people, in some ways in a superior manner to traditional methods. Practitioners described being able to identify risk factors rapidly and alert necessary professionals with post-assessment notifications (Rowe et al., 2020). Faster responding was also highlighted as an advantage for technology-based monitoring and assessment (Marsch & Borodovsky, 2016). Through using apps, young people can access urgent support when there is not a therapist present, potentially enhancing safety. For instance, the SafePlan App which has passed initial usability testing was designed for individuals that are of high-risk regarding suicidality (O’Grady et al., 2020), whilst the WRAP App promotes general wellbeing for individuals with various life experiences and mental health difficulties (WRAP, 2018). Young people can also access therapeutic support from a distance, which could be significant for settings that may struggle with accessibility of clinical provision (Batastini, 2016; Wolters et al., 2017). Certain technologies were also identified as valuable when there is insufficient staff, with benefits in relation to reducing cost and time (Marsch & Borodovsky, 2016).
Through data being stored online, it was identified how technologies such as apps can enable multiple teams, for example healthcare services at schools, to access the same server and hence access the same information. This was described by Merry and colleagues (2020) who detailed an app that could be flexibly developed to meet the changing needs of young people, for example, through providing pandemic-oriented support. Evidence suggests that having a clinically governed approach to information sharing resources can be advantageous within settings where there could be multiple systems. This is reflected within the Healthcare Standards for Children and Young People in Secure Settings (Royal College of Paediatrics and Child Health, 2019) which highlights the importance of appropriate information sharing between multi-disciplinary teams.
On the other hand, implementing novel technology into mental health services that are facing high-stress and high-pressure could be perceived as burdensome. Owens and Charles (2016) discovered this when conducting a feasibility study researching a novel SMS text-messaging intervention for young self-harmers. The feasibility study was unable to recruit sufficient numbers due to the CAMHSFootnote 1 service being ‘in crisis’, and staff experiencing heavy workloads.
Therapeutic Effectiveness
The effectiveness of technology-assisted therapeutic interventions has received mixed results. A systematic review examining internet-based CBT for young people found that all but one of their included studies demonstrated significant relative symptom reduction, and overall displayed high feasibility and good acceptability (Babiano-Espinosa et al., 2019). Two examples were self-help resources, whilst the rest were in conjunction with one-to-one therapist sessions (i.e., after or between sessions with a therapist). Further, a long-term study within a custodial setting found that psychiatric care delivered by videoconferencing was effective in reducing symptoms of distress (Batastini, 2016). Nevertheless, this is only a small number of studies, and a different review summarised that the effectiveness of technology-assisted CBT is not well established (Wolters et al., 2017). This review also found that having the physical presence of a therapist was deemed to be more beneficial for young people in comparison to technology-based alternatives. For other technological modalities, such as those used for digital phenotyping, the outcomes within the literature are too heterogeneous to summarise into a coherent conclusion regarding effectiveness (Sequeira et al., 2019).
The results from studies examining general wellness initiatives rather than specific psychological intervention appear more ubiquitously positive. For example, an online life skills coaching intervention co-designed by young people and delivered by cartoon avatars was rated easy to use by 90 percent of the young people that participated, with 76 percent identifying it as useful (Gabrielli et al., 2020). Another non-specific wellness initiative in the form of an online game assessing socio-emotional functioning in young people at school was also found to be well received and accepted by young people from various backgrounds (Day et al., 2019), highlighting positive feedback for general wellbeing technologies.
Ethical Considerations
There are several possible ethical barriers to using technology in mental health services (e.g., data protection, right to withdraw, transparent instructions), which were considered by some of the reviewed papers. Positively, one study concluded that the use of tablets was in fact more beneficial in relation to superior data protection security than traditional paper and pen recording methods (Wall et al., 2018). Tablets can also enable young people to skip questions and withdraw from any online application discretely (Wall et al., 2018).
In relation to conducting mental health research, it was highlighted within a review that young people that have witnessed violence are more likely to experience additional challenges in relation to engagement with technology (Wall et al., 2018). There may also be additional ethical barriers to consider when conducting technology-based research for this population, and the authors advised greater scrutiny of app developers in relation to ensuring instructions are clear for young people. Using technology to facilitate mental health research should also be interactive and enable young people to exit the application when they desire. Within a research context, the authors also recommended that services conduct needs-based assessments and consider whether they have the capacity and resources to use an app that may need to be updated and developed over time (Wall et al., 2018).
Within custodial settings, reportedly tele-mental health care can be readily implemented and provides advantages from a security perspective (Batastini, 2016). For example, workers reported being able to monitor group conversations more effectively if they were tech-facilitated. However, there are considerations needed in relation to confidentiality—if the young person cannot be left unsupervised with the technology, then this could limit the privacy of the therapeutic session (Batastini, 2016).
Risks in Relation to Therapeutic Alliance
It has been suggested that therapeutic alliance (Crum & Comer, 2016) and the emotional connectedness between the professional and the service-user could be compromised by use of technology (Batastini, 2016). For family-orientated therapy in particular, consideration is needed in relation to therapeutic alliance, privacy, safety, childcare logistics, and technological literacy varying across generations (Crum & Comer, 2016). Eapen et al. (2021) also highlighted the importance of considering privacy and internet access. Therapeutic alliance was listed as a particular difficulty for individuals with challenging behaviour, when facilitating technology-augmented therapies (Wolters et al., 2017), and when conducting psychiatric assessments for young people (Eapen et al., 2021). Clinicians expressed a need for therapies to be tailored to each individual, and voiced concerns in relation to the feasibility or effectiveness of technology-assisted therapy for individuals with more severe needs (Wolters et al., 2017).
Application of Technology to Mental Health Care
Flexible Application of Technology
Evidence suggests that some practitioners appear to have philosophical and personal challenges with using technology to facilitate one-to-one therapeutic sessions. When the domain of staff non-engagement with a community mental health online platform for young people was explored, CAMHSweb practitioners expressed that the platform interfered with the therapeutic process and was challenging to implement into their daily practice. It was detailed that the platform interfered with the therapists’ personal style of therapy and their ability to be spontaneous during therapeutic sessions. Difficulty of use was not a complaint, suggesting that the barriers appeared to be more values-oriented towards how the therapists’ believed therapy should be conducted (Town et al., 2017). When comparing CAMHSweb to other CBT-oriented interventions that were perceived to be feasible and acceptable (e.g., Babiano-Espinosa et al., 2019), the difference appears to be whether the technology dictates the therapeutic session or whether the technology is perceived as an adjunct to the therapeutic session. In Babiano-Espinosa and colleagues’ (2019) review for instance, the online platforms were used in conjunction to the therapist’s own sessions with the young person, or as the sole delivery of therapy through self-help (i.e., without therapist involvement). Therefore, the use of technology to collaborate in-session may be challenging in some cases to the values of some practitioners.
These concerns were mirrored in a review conducted by Wolters and colleagues (2017), where practitioner views illustrated a reluctance to the standardised nature of technology-assisted structured interventions. Alternatively, an app for trauma-focused CBT was found to have high acceptability and satisfaction from providers and families during a pilot study, during which practitioners were informed that the chapters were non-prescriptive and that they could flexibly utilise any activities that they felt may be useful for a specific young person (Davidson et al., 2019). This highlights that flexibility may indeed be an important factor.
Optimising the Use of Technology
It has been suggested that particularly for vulnerable young people, using technology for psychological purposes should not be a time-burden (Wall et al., 2018). Young people and practitioners suggested short sessions as the optimum for this medium (e.g., 5 to 10 min for a cartoon chat box intervention; Gabrielli et al., 2020). Regarding improving usability and user-experience for young people, it was recommended in a review that touch screen be adopted as opposed to using a mouse, and text-based input should be minimised or avoided (Schueller et al., 2017). Providing challenges and feedback during the online interventions facilitates ‘flow’, sustaining engagement and motivation to engage for young people. It is also beneficial if the challenges and feedback are tailored to the young person’s needs and goals. Interaction with other young people on the online platform, or a remote agent, is also a valuable tool to enhance motivation and prevent drop-out (Schueller et al., 2017).
A systematic review highlighted that studies that resulted in positive therapeutic outcomes and engagement had a tendency to incorporate specific technological elements onto their online platform or website. This included a competent look and feel that was aesthetically pleasing for young people in-person supportive dialogue during the intervention, interventions that reduced therapeutic content into simple tasks, and the inclusion of self-monitoring tools (Wozney et al., 2017). Gamification appeared to be popular within the therapeutic forums deemed more acceptable by young people. For instance, a gaming programme that followed structures of CBT and Interpersonal Therapy for young people with depression was deemed positive by young people and practitioners, who believed it would be a useful addition to existing in-person therapy (Carrasco, 2016).
A further systematic review examining multiple modes of digital mental health interventions, (including websites, apps, games and computer-assisted programs, robots, digital devices, virtual reality, and text messaging) found that young people preferred digital interventions that included videos, less text, personalisation, having the ability to connect with other people, and text message reminders (Liverpool et al., 2020). Barriers included whether the technology was suitable, usable, the acceptability of the intervention, and patient motivation. Additional barriers to engagement included practical difficulties for individuals who may not have access to the technology in their younger years and may not have family members that can respond with technology (Batastini, 2016).
From a psychiatry perspective, clinicians disclosed concerns in relation to their ability to conduct comprehensive assessments of a young person, their development, and any risk factors when this was conducted through a technological medium such as videoconference (Eapen et al., 2021). Negative professional attitudes towards structured online courses were also a potential barrier to engagement (Kurki et al., 2018). These barriers should be considered when attempting to optimise the use of technology to support young people’s care.
For implementation within primary care, due to GPs having minimal capacity, practitioners from primary care recommended that online platforms, specifically ones that target engagement with therapeutic intervention for young people with anxiety and depression, should be advertised through physical patient reminders, and the use of champions in surgeries (Radovic et al., 2020). This highlights that consideration in relation to the practicalities of buy-in are important. Prior to implementing technology such as videoconferencing into a mental health service, considerations are also needed in relation to installation, maintenance, data storage and cost (Chou et al., 2016).
Discussion
This review identified 27 papers examining the use of technology to support young people’s care, the majority focusing on technology which facilitated some form of assessment, psychoeducation, mental health activity, or structured therapy. In combination, the evidence presented suggests that the introduction of technology to support young people’s care has the potential to enhance engagement, increase efficiency of care and improve therapeutic effectiveness. Indeed, the increase of sophisticated technology into young people’s lives in modern society offers an opportunity to utilise these advancements to support mental health and wellbeing (Wolters et al., 2017). The findings presented within this review support Babiano-Espinosa and colleagues’ (2019) hypothesis that the use of technological modalities could address barriers for therapy by adjusting treatment to the technologically advanced modern life of young people and enhancing opportunities to improve cost-effectiveness. As argued by Day and colleagues (2019), technological advancements offer first-stage approaches for multiple-level assessments, or the opportunity to collect research data to inform practice. The evidence presented in this rapid review supports this claim.
It has been suggested that in order for technology to fully support young people’s care, it must be feasible and engaging to young people, whilst upholding validity and reliability (Day et al., 2019). Encouragingly, the majority of papers included in this review examined aspects of the acceptability, feasibility and efficacy of technology and highlighted several positive characteristics.
Young people provided positive feedback regarding the acceptability of technology (e.g., Davidson et al., 2019; Gabrielli et al., 2020; Snijder et al., 2021) and several studies also highlighted good reliability (e.g., Boström et al., 2016; Day et al., 2019). The current review also builds on recommendations made by Liverpool and colleagues (2020) for future research to investigate engagement as a component of effectiveness and to consider young people’s preferences relating to the various modes of delivery.
This review highlighted potential barriers, preferences, and recommendations for the feasibility and efficacy of introducing new technology into young people’s services. Barriers which should be considered when attempting to optimise the use of technology include service user motivation (Liverpool et al., 2020), socioeconomic factors relating to access to technology (Batastini, 2016), clinician concerns in relation to their ability to conduct comprehensive assessments using technology (Eapen et al., 2021), and negative professional attitudes (Kurki et al., 2018). Young people also offered useful suggestions to enhance engagement, such as using less text, personalisation, having the ability to connect with other people, and text message reminders (Liverpool et al., 2020). Motivational messages and relaxing videos were also a request from young people (O’Grady et al., 2020).
Strengths and Limitations
This review adhered to established guidelines for conducting rapid evidence reviews and highlighted 27 papers contributing to the research base on the use of technology to support young people’s care. Positively, this review highlighted the range of available methods of delivery, factors influencing engagement, and recommendations based on young person preferences. The findings provide a useful foundation to understand the potential benefits involved in introducing technology to support young people’s care.
However, the current paper is limited in that the review includes findings from before and during the COVID-19 pandemic. The impact of the pandemic on the use of technology in care settings is not yet fully understood. It is possible that this could have had some impact on the current findings, and post-pandemic research would be useful to further explore this. Additionally, a rapid evidence review was conducted in place of a meta-analysis due to the anticipation that there would be insufficient quantitative data or consistency of outcome measures. It has been argued that shortening the review process in the form of a rapid review could result in publication bias or inconsistencies being overlooked (Grant & Booth, 2009). As the current search was limited to only two databases, this is a potential limitation of the current review. Nevertheless, as argued by Grant and Booth (2009), it is important that producing the evidence within a rapid timescale is balanced against the risk of bias.
Quality appraisal was not conducted due to the limited time constraints of the authors. This limits the strength of the findings and clinicians should note that the quality of the studies included within this review may not have been to an equal standard. One author conducted the literature search and screening. The findings were therefore potentially at risk of greater bias as a result of this limitation. Future research with greater time and funding may have value in conducting a more comprehensive review with a method that mitigates against such limitations.
Implications and Recommendations
New technology is continually and rapidly being developed and implemented for therapeutic purposes. The current review highlights the value in collating and summarising recent evidence within this domain to inform mental health services and provision for young people. Effective and sustained use of technology within young people’s mental health services will depend on the technology’s usability, efficiency, and ability to engage young people.
Attention should be given to the design of the technology to ensure it is simple and engaging, making use of videos and motivational content. Clinicians’ concerns should also be taken into account, and professionals should be supported to use technology to enhance the services they offer. Consideration of socioeconomic factors is also needed, particularly with regards to supporting young people and their families to access technology. Developers should work collaboratively with clinicians and service users to create technology which is accessible, engaging, and suitable for young people.
In relation to generalisability and diversity, despite most of the research captured in the current review being predominantly from Westernised cultures, a diverse range of backgrounds and developmental needs were recruited. For instance, Hollis et al. (2017) conducted a systematic review including any young people accessing mental health services (including diagnoses such as Attention Deficit Hyperactivity Disorder [ADHD], Autism Spectrum Disorder [ASD], psychosis, eating disorders, and Post Traumatic Stress Disorder [PTSD]). The research included also indicated that technology can be specifically developed to be culturally sensitive and appropriate (Snijder et al., 2021). Additional research in relation to other cultures is needed to consolidate the efficacy of this approach. Intuitively, some of the benefits witnessed with the introduction of technology into young people’s mental health services, such as reductions in costing (Marsch & Borodovsky, 2016).), and reducing travel for appointments (Batastini, 2016; Wolters et al., 2017), may be beneficial for marginalised communities, or individuals that face more challenges in accessing appropriate mental health care.
Further research is needed to understand the long-term impact of using technology to support young people’s care. Enhanced understanding of whether the advantages acquired by using technology to support treatment will be maintained over time would be beneficial.
It would also be useful for future research to further investigate the possible adverse effects of technology use, for example, relating to confidentiality and patient safety. Additional research could further investigate the impact of the COVID-19 pandemic on technology use in care settings. It is possible that restrictions on social interaction could have increased young people’s reliance on technology, resulting in individuals being more likely to engage with treatment via apps or online forums.
Conclusion
As argued by Comer and colleagues (2021), the COVID-19 pandemic has created a sense of urgency to resolve the issues that have previously limited technological advancements within the public health sector. The current review suggests that the introduction of technology to support young people’s care is feasible, acceptable, and engaging. Factors that affect engagement were identified alongside young person preferences, allowing for future consideration of strategies to overcome barriers and successfully implement technology to enhance young people’s care. Further research is needed to investigate the long-term benefits of using technology to enhance young people’s care.
Data availability
For queries regarding data, contact the ‘author for correspondence’.
Notes
Children and Adolescent Mental Health Services.
References
Babiano-Espinosa, L., Wolters, L. H., Weidle, B., op de Beek, V., Pedersen, S. A., Compton, S., & Skokauskas, N. (2019). Acceptability, feasibility, and efficacy of Internet cognitive behavioral therapy (iCBT) for pediatric obsessive-compulsive disorder: A systematic review. Systematic Reviews, 8(1), 1–16.
Batastini, A. B. (2016). Improving rehabilitative efforts for juvenile offenders through the use of telemental healthcare. Journal of Child and Adolescent Psychopharmacology, 26(3), 273–277.
Berrouiguet, S., Baca-García, E., Brandt, S., Walter, M., & Courtet, P. (2016). Fundamentals for future mobile-health (mHealth): A systematic review of mobile phone and web-based text messaging in mental health. Journal of Medical Internet Research, 18(6), e135.
Borghouts, J., Eikey, E., Mark, G., De Leon, C., Schueller, S. M., Schneider, M., Stadnick, N., Zheng, K., Mukamel, D., & Sorkin, D. H. (2021). Barriers to and facilitators of user engagement with digital mental health interventions: systematic review. Journal of Medical Internet Research, 23(3), e24387.
Boström, P., Johnels, J. Å., Thorson, M., & Broberg, M. (2016). Subjective mental health, peer relations, family, and school environment in adolescents with intellectual developmental disorder: A first report of a new questionnaire administered on tablet PCs. Journal of Mental Health Research in Intellectual Disabilities, 9(4), 207–231.
Carrasco, Á. E. (2016). Acceptability of an adventure video game in the treatment of female adolescents with symptoms of depression. Research in Psychotherapy: Psychopathology, Process and Outcome, 19(1), 10–18.
Cheng, V. W. S., Davenport, T., Johnson, D., Vella, K., & Hickie, I. B. (2019). Gamification in apps and technologies for improving mental health and well-being: Systematic review. JMIR Mental Health, 6(6), e13717.
Chou, T., Comer, J. S., Turvey, C. L., Karr, A., & Spargo, G. (2016). Technological considerations for the delivery of real-time child telemental healthcare. Journal of Child and Adolescent Psychopharmacology, 26(3), 192–197.
Comer, J. S., Furr, J. M., del Busto, C., Silva, K., Hong, N., Poznanski, B., Sanchez, A., Cornacchio, D., Herrera, A., Coxe, S., Miguel, E., Georgiadis, C., Conroy, K., & Puliafico, A. (2021). Therapist-led, internet-delivered treatment for early child social anxiety: A waitlist-controlled evaluation of the iCALM telehealth program. Behavior Therapy, 52(2021), 1171–1187.
Copeland, M. E. (2002). Overview of WRAP: Wellness recovery action plan. Mental Health Recovery Newsletter, 3, 1–9.
Crum, K. I., & Comer, J. S. (2016). Using synchronous videoconferencing to deliver family-based mental healthcare. Journal of Child and Adolescent Psychopharmacology, 26(3), 229–234.
Davidson, T. M., Bunnell, B. E., Saunders, B. E., Hanson, R. F., Danielson, C. K., Cook, D., Chu, B. C., Dorsey, S., Adams, Z. W., Andrews III, A. R., Walker, J. H., Soltis, K. E., Cohen, J. A., Deblinger, E., & Ruggiero, K. J. (2019). Pilot evaluation of a tablet-based application to improve quality of care in child mental health treatment. Behavior Therapy, 50(2), 367–379.
Day, J., Freiberg, K., Hayes, A., & Homel, R. (2019). Towards scalable, integrative assessment of children’s self-regulatory capabilities: New applications of digital technology. Clinical Child and Family Psychology Review 22(1), 90–103.
DeFilippis, E., Impink, S. M., Singell, M., Polzer, J. T., & Sadun, R. (2020). Collaborating during coronavirus: The impact of COVID-19 on the nature of work. National Bureau of Economic Research. https://doi.org/10.3386/w27612
Division of Clinical Psychology. (2020, September). DCP Covid-19 strategy: A live document (version 1). https://www.bps.org.uk/sites/www.bps.org.uk/files/Member%20Networks/Divisions/DCP/DCP%20Covid-19%20Strategy.pdf
Drissi, N., Ouhbi, S., Idrissi, M. A. J., Fernandez-Luque, L., & Ghogho, M. (2020). Connected mental health: systematic mapping study. Journal of Medical Internet Research, 22(8), e19950.
Eapen, V., Dadich, A., Balachandran, S., Dani, A., Howari, R., Sequeria, A. Z., & Singer, J. D. (2021). E-mental health in child psychiatry during COVID-19: an initial attitudinal study. Australasian Psychiatry, 10398562211022748.
Etzelmueller, A., Vis, C., Karyotaki, E., Baumeister, H., Titov, N., Berking, M., Cuijpers, P., Riper, H., & Ebert, D. D. (2020). Effects of internet-based cognitive behavioral therapy in routine care for adults in treatment for depression and anxiety: Systematic review and meta-analysis. Journal of Medical Internet Research, 22(8), e18100.
Gabrielli, S., Rizzi, S., Carbone, S., & Donisi, V. (2020). A chatbot-based coaching intervention for adolescents to promote life skills: Pilot study. JMIR Human Factors, 7(1), e16762.
Garrido, S., Millington, C., Cheers, D., Boydell, K., Schubert, E., Meade, T., & Nguyen, Q. V. (2019). What works and what doesn’t work? A systematic review of digital mental health interventions for depression and anxiety in young people. Frontiers in Psychiatry, 10, 759.
Garritty, C., Gartlehner, G., Nussbaumer-Streit, B., King, V. J., Hamel, C., Kamel, C., Affengruber, L., & Stevens, A. (2020). Cochrane rapid reviews methods group offers evidence-informed guidance to conduct rapid reviews. Journal of Clinical Epidemiology, 130, 13–22.
Gearing, R. E., Attia-Guetta, R., Moore, K., Gorroochurn, P., Olson, L., & Malekoff, A. (2021). Tech connect: An intervention to promote treatment engagement for adolescents with depression. Community Mental Health Journal, 57(5), 880–883.
Grant, M. J., & Booth, A. (2009). A typology of reviews: An analysis of 14 review types and associated methodologies. Health Information & Libraries Journal, 26(2), 91–108.
Hashemi, B., Ali, S., Awaad, R., Soudi, L., Housel, L., & Sosebee, S. J. (2017). Facilitating mental health screening of war-torn populations using mobile applications. Social Psychiatry and Psychiatric Epidemiology, 52(1), 27–33.
Hollis, C., Falconer, C. J., Martin, J. L., Whittington, C., Stockton, S., Glazebrook, C., & Davies, E. B. (2017). Annual Research Review: Digital health interventions for children and young people with mental health problems—A systematic and meta-review. Journal of Child Psychology and Psychiatry, 58(4), 474–503.
HRA (Health Research Authority, 2021), Is My Study Research? http://www.hra-decisiontools.org.uk/research/. Retrieved 29 Jan 21
Inal, Y., Wake, J. D., Guribye, F., & Nordgreen, T. (2020). Usability evaluations of mobile mental health technologies: Systematic review. Journal of Medical Internet Research, 22(1), e15337.
Jagosh, J., Macaulay, A. C., Pluye, P., Salsberg, J. O. N., Bush, P. L., Henderson, J. I. M., Sirett, E., Wong, G., Cargo, M., Herbert, C. P., Seifer, S. D., Green, L. W., & Greenhalgh, T. (2012). Uncovering the benefits of participatory research: implications of a realist review for health research and practice. The Milbank Quarterly, 90(2), 311–346.
Kurki, M., Anttila, M., Koivunen, M., Marttunen, M., & Välimäki, M. (2018). Nurses’ experiences of the use of an Internet-based support system for adolescents with depressive disorders. Informatics for Health and Social Care, 43(3), 234–247.
Liverpool, S., Mota, C. P., Sales, C. M., Čuš, A., Carletto, S., Hancheva, C., Edbrooke-Childs, J., et al. (2020). Engaging children and young people in digital mental health interventions: Systematic review of modes of delivery, facilitators, and barriers. Journal of Medical Internet Research, 22(6), e16317.
Luo, C., Sanger, N., Singhal, N., Pattrick, K., Shams, I., Shahid, H., ... & Samaan, Z. (2020). A comparison of electronically-delivered and face to face cognitive behavioural therapies in depressive disorders: A systematic review and meta-analysis. EClinicalMedicine, 24, 100442.
Magnavita, J. J. (2018). Introduction: How can technology advance mental health treatment? In J.J. Magnavita (Ed.), Using technology in mental health practice (pp. 3-10). American Psychological Association
Marsch, L. A., & Borodovsky, J. T. (2016). Technology-based interventions for preventing and treating substance use among youth. Child and Adolescent Psychiatric Clinics, 25(4), 755–768.
Merry, S. N., Cargo, T., Christie, G., Donkin, L., Hetrick, S., Fleming, T., Holt-Quick, C., Hopkins, S., Stasiak, K., & Warren, J. (2020). Debate: Supporting the mental health of school students in the COVID-19 pandemic in New Zealand–a digital ecosystem approach. Child and Adolescent Mental Health, 25(4), 267–269.
National Health Service. (2019, August 21). The NHS Long Term Plan. https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf
Nesbitt, T. S. (2012). The evolution of telehealth: Where have we been and where are we going. In The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary. Washington, DC: Institute of Medicine.
O’Grady, C., Melia, R., Bogue, J., O’Sullivan, M., Young, K., & Duggan, J. (2020). A mobile health approach for improving outcomes in suicide prevention (SafePlan). Journal of Medical Internet Research, 22(7), e17481.
Orlowski, S. K., Lawn, S., Venning, A., Winsall, M., Jones, G. M., Wyld, K., Damarell, R. A., Antezana, G., Schrader, G., Smith, D., Collin, P., & Bidargaddi, N. (2015). Participatory research as one piece of the puzzle: a systematic review of consumer involvement in design of technology-based youth mental health and well-being interventions. JMIR Human Factors, 2(2), e4361.
Ouhbi, S., Drissi, N., Idrissi, M. A. J., Luque, L. F., & Ghogho, M. (2020). Connected mental health: Systematic mapping study. Journal of Medical Internet Research, 22(8), e19950.
Owens, C., & Charles, N. (2016). Implementation of a text-messaging intervention for adolescents who self-harm (TeenTEXT): A feasibility study using normalisation process theory. Child and Adolescent Psychiatry and Mental Health, 10(1), 1–9.
Oz, T., & Crooks, A. (2020). Exploring the impact of mandatory remote work during the COVID-19 pandemic. George Mason University. https://doi.org/10.1111/bjop.12468
Radovic, A., Odenthal, K., Flores, A. T., Miller, E., & Stein, B. D. (2020). Prescribing technology to increase uptake of depression treatment in primary care: A Pre-implementation focus group study of SOVA (supporting our valued adolescents). Journal of Clinical Psychology in Medical Settings, 27(4), 766–782.
Ramo, D., & Lim, M. H. (2021). Technology Matters: Using apps to address loneliness in adolescents and young adults-leveraging tech engagement among digital natives. Child and Adolescent Mental Health, 26(2), 186–188.
Rowe, S. C., Davenport, T. A., Easton, M. A., Jackson, T. A., Melsness, J., Ottavio, A., Sinclair, J., & Hickie AM, I. B. (2020). Co-designing the InnoWell Platform to deliver the right mental health care first time to regional youth. Australian Journal of Rural Health, 28(2), 190–194.
Royal College of Paediatrics and Child Health (RCPCH). (2019, June). Healthcare Standards for Children and Young People in Secure Settings. www.rcpch.ac.uk/cypss
Schueller, S. M., Stiles-Shields, C., & Yarosh, L. (2017). Online treatment and virtual therapists in child and adolescent psychiatry. Child and Adolescent Psychiatric Clinics, 26(1), 1–12.
Sequeira, L., Battaglia, M., Perrotta, S., Merikangas, K., & Strauss, J. (2019). Digital phenotyping with mobile and wearable devices: Advanced symptom measurement in child and adolescent depression. Journal of the American Academy of Child & Adolescent Psychiatry, 58, 841–845.
Snijder, M., Stapinski, L., Ward, J., Lees, B., Chapman, C., Champion, K., ... & Newton, N. (2021). Strong and Deadly Futures: Co-Development of a Web-Based Wellbeing and Substance Use Prevention Program for Aboriginal and Torres Strait Islander and Non-Aboriginal Adolescents. International Journal of Environmental Research and Public Health, 18(4), 2176.
The British Psychological Society (2020). Adaptations to psychological practice: Continuing guidance during Covid-19 Pandemic. https://www.bps.org.uk/sites/www.bps.org.uk/files/Policy/Policy%20-%20Files/Adaptations%20to%20psychological%20practice%20-%20interim%20guidance%20during%20Covid-19.pdf
Town, R., Midgley, N., Ellis, L., Tempest, R., & Wolpert, M. (2017). A qualitative investigation of staff’s practical, personal and philosophical barriers to the implementation of a web-based platform in a child mental health setting. Counselling and Psychotherapy Research, 17(3), 218–226.
Wall, M. A., Jenney, A., & Walsh, M. (2018). Conducting evaluation research with children exposed to violence: How technological innovations in methodologies and data collection may enhance the process. Child Abuse & Neglect, 85, 202–208.
Wolters, L. H., op de Beek, V., Weidle, B., & Skokauskas, N. (2017). How can technology enhance cognitive behavioral therapy: The case of pediatric obsessive compulsive disorder. BMC Psychiatry, 17(1), 1–9.
Wozney, L., Huguet, A., Bennett, K., Radomski, A. D., Hartling, L., Dyson, M., McGrath, P. J., & Newton, A. S. (2017). How do eHealth programs for adolescents with depression work? A realist review of persuasive system design components in internet-based psychological therapies. Journal of Medical Internet Research, 19(8), e7573.
WRAP. (2018). Wellness Recovery Action Plan: WRAP in action, WRAP App. https://www.wellnessrecoveryactionplan.com/wrap-in-action/wrap-app/
Wu, Y. J., Outley, C., Matarrita-Cascante, D., & Murphrey, T. P. (2016). A systematic review of recent research on adolescent social connectedness and mental health with internet technology use. Adolescent Research Review, 1(2), 153–162.
Zhou, X., Edirippulige, S., Bai, X., & Bambling, M. (2021). Are online mental health interventions for youth effective? A systematic review. Journal of Telemedicine and Telecare, 27(10), 638–666.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Financial support
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A
Author | Study Design | Setting | Participants | Type of Technology | Intervention | Outcome Measure |
|---|---|---|---|---|---|---|
Kurki et al. (2018) | Cohort study | Outpatient clinics & university hospitals, adolescent psychiatry services, Finland | N = 70 young people (13–17 years) N = 9 nurses | Online platform / website | Support platform (wellbeing, coping skills and self-reflection) | Exploration |
Rowe et al., (2020) | Cohort study | Primary mental health services, Australia | N = 120 young people | Online platform / website | n/a | Feasibility / usability |
Gabrielli et al. (2020) | Pilot feasibility evaluation | Secondary school | N = 20 young people (co-design workshop) N = 21 young people (evaluation) | Online platform / website | Co-design workshop | Feasibility |
Snijder et al., (2021) | Cross-sectional cohort study | Schools × 4, Australia | Aboriginal and Torres Strait Islander young people aged 12–14 years | Online platform / website | n/a | Design/acceptability/usability |
Marsch and Borodovsky (2016) | Review | Primary care, schools, homes, medical settings, and universities | Young people | Online platform / website | Substance misuse prevention (CLIMATE, Head On, Thinking Not Drinking, RealTeen) | Efficacy |
Crum and Comer (2016) | Review | Unspecified | Families accessing mental health care | Online platform / website | Various family-orientated psychological interventions | Feasibility |
Schueller et al. (2017) | Review | Unspecified | Young people | Online platform / website | n/a | Usability / engagement |
Town et al. (2017) | Cross-sectional qualitative interviews | London CAMHS team with a low utilisation of the platform | N = 6 practitioners with low utilisation of the platform | Online platform / website | n/a | Acceptability/ feasibility |
Wozney et al., (2017) | Review | Unspecified | Young people accessing psychotherapy | Online platform / website | Internet-based psychotherapy (IPT & CBT) | Efficacy |
Babiano-Espinosa et al., (2019) | Systematic review | Unspecified | Young people aged 4–18 with OCD | Online platform / website | Traditional CBT with Internet-based CBT | Acceptability/feasibility/ efficacy |
Radovic et al. (2020) | Case series | Primary care | n = 14 primary care providers/physicians | Online platform / website | Pre-intervention focus group | Implementation strategy development |
Wall et al. (2018) | Review | Unspecified | n/a | App / game | Use of technology for research with children | Exploration |
Day et al. (2019) | Review | Australian schools | Children aged 6–12. n = 3460 children have contributed to the data | App / game | Assessment administered via an interactive game played on computer or iPads | Acceptability/ feasibility |
Boström et al. (2016) | Cross-sectional feasibility and validity study | 18 schools in Sweden | n = 113 students in special education aged 12–16 and their parents and teachers | App / game | WellSEQ—wellbeing in special education questionnaire, an app for tablets | Feasibility/ acceptability/ validity |
O'Grady et al. (2020) | Cohort study | Secondary school in Ireland | Practitioners from mental health services and secondary school students | App / game | SafePlan app: Suicide prevention and wellness | Usability |
Wolters et al., (2017) | Review | Unspecified—mental health services | Young people experiencing OCD | App / game | Technology empowered CBT (tCBT) for paediatric OCD | Exploration |
Davidson et al., (2019) | Cross sectional pilot evaluation | Four different Community MH settings | n = 13 providers and n = 27 families | App / game | Novel tablet-based App designed to enhance trauma-focused CBT (TF-CBT) | Acceptability |
Carrasco (2016) | Cohort cross-sectional study | Two different schools, Chile | n = 5 therapists and n = 15 young women with depression aged 14–18 | App / game | Videogame following structures of CBT and IPT for depression. Private forum that includes information and self-care | Acceptability |
Merry et al., (2020) | Cross sectional cohort study | New Zealand, Child and young person mental health | Practitioners, young people | Other PC software | HABITS (Health Advances through Behavioural Interventional Technologies): e-health interventions, referral support and screening, participant pool for clinical trials | Feasibility/acceptability |
Chou et al. (2016) | Review | Unspecified | n/a | Video-related technology | Video-teleconferencing | Recommendations |
Eapen et al., (2021) | Case study | Psychiatry services, Australia | N = 5 child and adolescent psychiatry trainees | Video-related technology | Assessing clinician attitudes and thoughts after the introduction of e-mental health into a psychiatry service | Feasibility/ exploration |
Sequeira et al., (2019) | Review | Child and adolescent psychiatry | Children and young people | Other technology | Digital phenotyping as an assessment for adolescent depression | Exploration/ feasibility/ efficacy |
Liverpool et al., (2020) | Systematic review | Unspecified | Children and young people participating within digital mental health interventions | Mixed | n/a | Exploration |
Batastini (2016) | Review | Juvenile offending services | Juvenile offenders | Mixed | Various | Efficacy |
Hollis et al. (2017) | Systematic and meta-review | Unspecified—mental health services | Young people accessing mental health services (including ADHD, ASD, psychosis, eating disorders, and PTSD) | Mixed | Various | Efficacy |
Owens and Charles (2016) | Feasibility long-term cohort study | CAMHS England | 1 clinician/client dyad | SMS | SMS text messaging for young people that self-harm | Feasibility |
Gearing et al. (2021) | Randomised control trial | USA, young people accessing psychotherapy for depression | n = 20 young people with depression, with a mean age of 14 years | SMS/phone calls | Tech Connect -contacting individuals between sessions using SMS personalised messaging (8 weekly messages), and 3 telephone calls to parents | Feasibility / acceptability |
Appendix B
Flow Diagram detailing search numbers (PRISMA, 2009).

From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. https://doi.org/10.1371/journal.pmed1000097
For more information, visit www.prisma-statement.org
Rights and permissions
About this article
Cite this article
Ramshaw, G., McKeown, A., Lee, R. et al. Introduction of Technology to Support Young People’s Care and Mental Health—A Rapid Evidence Review. Child Youth Care Forum 52, 509–531 (2023). https://doi.org/10.1007/s10566-022-09700-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10566-022-09700-1