Abstract
Summary
The mortality of elderly hip fracture patients is high. Eighty-five percent of all patients were followed until death. The three most protective factors for 1-year survival were ASA class; BMI; and age, and the four most protective factors for 14-year survival were age; BMI; ASA class; and subtrochanteric fracture type.
Objective
Hip fractures are associated with increased mortality. The purpose of this study was to evaluate the protective preoperative factors regarding the survival of short-term (1 year) and long-term (14 years) follow-up in a hip fracture cohort in Finland.
Methods
A total of 486 patients, operated on in 2005 and 2006, were retrospectively evaluated. Survival was analyzed using Bayesian multivariate analysis and relative survival with the life table method. All patients were followed for a minimum of 14 years.
Results
We analyzed 330 women and 156 men, whose mean ages were 82.4 and 72.0 years, respectively. The overall mortality rate was 7% at 1 month, 22% at 12 months, and 87% at 14 years. Protective factors against mortality at 1 year were ASA class (1–3), BMI ≥ 20 kg/m2, age < 85 years, alcohol involvement, Alzheimer’s disease, no comorbidities, certain operative methods, and female sex. Factors promoting survival at 14 years were age < 75 years, BMI ≥ 20 kg/m2, ASA class (1–2), subtrochanteric fracture, certain operative methods, alcohol involvement, and no comorbidities.
Conclusions
Protective factors for 1-year survival in order of importance were ASA class, BMI, and age, and, correspondingly, for 14-year survival, age, certain operative methods, BMI, and ASA class. The relative survival of hip fracture patients was lower than that of the general population.
Similar content being viewed by others
Introduction
Hip fractures are the most common fractures requiring surgical treatment among adults. The highest incidences of hip fractures around the world have been observed in Northern Europe and the USA [1]. The age-standardized incidence of hip fractures in women is roughly twice as high as that in men, with some variability across the world [1]. In recent decades, the age-adjusted incidence of hip fractures has continuously decreased in high-incidence countries [2, 3]. According to a recent report from the four-decade Framingham Heart Study with 10,552 participants, the main reason for the observed decrease in hip fractures was a reduction in smoking and heavy drinking, which were important risk factors for fractures [4]. However, due to the increased number of hip fractures in developing countries [1], the worldwide overall annual number of hip fractures is still rising. It has been estimated that, by the year 2050, a staggering 6.3 million hip fractures worldwide will occur annually [5].
Several studies have reported that mortality among elderly hip fracture patients is higher than that of the age-adjusted general population and also higher among males than females [6, 7]. The mortality is increased during the first postoperative year, and it remains high for the following years [8]. Hip fractures are associated with increased short-term and long-term mortality. The post-hip-fracture mortality is 7–8% at 30 days [9, 10], 16–24% at 1 year [11, 12], 32–56% at 5 years [13, 14], and 80% at 10 years [15]. Reports evaluating survival beyond 10 years are scarce [16, 17].
The reasons for the increased mortality and morbidity in low-energy hip fracture patients entail several pre-fracture conditions: older age, male sex, pre-fracture comorbidities, poor preoperative walking capacity and activities of daily living, fracture type, low body mass index (BMI), high ASA class, and non-multidisciplinary postoperative rehabilitation [8, 10, 11, 18]. Alcohol consumption is associated with higher hip fracture risk and postoperative complications [4, 15].
The aim of this study was to identify patient-specific factors affecting postoperative short- and long-term survival, to study the survival in relation to the mortality in the reference population, and to analyze the mortality of the patients over a period of 14 years.
Patients and methods
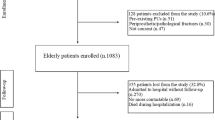
The study was approved by the local ethics committee. We retrospectively analyzed all patients with a hip fracture (n = 506) requiring operative treatment at Päijät-Häme Central Hospital in Southern Finland (61° N) from January 1, 2005, to December 6, 2006 (Supplementary Fig. 1). The exclusion criteria were a pathological fracture, age under 18 years, non-operative treatment, and an undefined time of the fracture (Supplementary Fig. 1). The data were collected from electronic medical records.
All hip fracture patients had a low-energy fracture as a result of slipping, tripping, or falling from standing height or lower, as documented in the medical records. Fractures caused by high-energy injuries were excluded.
A low-energy hip fracture was identified as one of the following diagnosis codes: femoral neck fractures (S72.0), pertrochanteric fractures (S72.1), or subtrochanteric fractures (S72.2). Adult patients with new low-energy hip fractures who underwent one of the following procedures were analyzed: NFB10 (uncemented hemiarthroplasty); NFB20 (cemented hemiarthroplasty); NFJ50 (osteosynthesis of the neck with cannulated screws); NFJ52 (osteosynthesis of the proximal femur with a DHS or Medoff plate); NFJ54 (osteosynthesis with an intramedullary nail); NFJ64 (osteosynthesis with additional screws or wires); NFB30 (uncemented primary total hip arthroplasty); NFB40 (hybrid total arthroplasty); or NFB50 (cemented primary total hip arthroplasty). The surgical procedure codes were collected according to the Nordic Medico-Statistical Committee’s classification of surgical procedures (NOMESCO). The medical records of all patients were checked manually (R.T.).
The baseline characteristics of patients are shown in Table 1. Patient-specific variables included the patient’s personal ID number, sex, age, date of injury, American Society of Anesthesiologists (ASA) class [19], body mass index (BMI; kg/m2), selected comorbidities, fracture type, date of operation, type of operation and implant, date of discharge, and death. BMI was divided into four groups: < 20, 20–24.9, 25–29.9, and > 30 kg/m2. Pre-existing selected comorbidities increasing the risk of falling were identified from the medical records individually (alcohol involvement [AI], Alzheimer’s disease, dementia, stroke, Parkinson’s disease, previous intracranial hemorrhages [ICH], transient ischemic attack [TIA], and severe psychiatric diseases with ongoing medication [e.g., schizophrenia]).
In this study, alcohol involvement (AI) denotes that the patient was under the influence of alcohol when attended to at the emergency department for a hip fracture. This information was documented in the medical records of the patient. Furthermore, no alcohol-related disease, such as alcohol dependence, alcoholic liver disease, or alcoholic psychoses, was documented. The medical records of all patients were checked manually (R.T.).
The patient’s age at the time of injury was recorded. Patients were divided into six age groups: ≤ 59.9, 60–69.9, 70–79.9, 80–85.9, 86–89.9, and ≥ 90 years.
We defined short-term and long-term mortality as death occurring within 12 months after a hip fracture and as death occurring more than 12 months after a hip fracture, respectively.
Fracture classification
The type of hip fracture was analyzed from the preoperative radiographs by the study group (RT, JPK). The fractures were classified as femoral neck fractures (S72.0), pertrochanteric fractures (S72.1), and subtrochanteric fractures (S72.2). Femoral neck fractures were further classified according to the Garden classification [20]. The type of trochanteric (S72.1) and subtrochanteric (S72.2) hip fractures was graded according to the AO classification [21]. We also evaluated the number of basicervical hip fractures [22]. Basicervical fractures were classified as pertrochanteric fractures (S72.1). One radiograph in group S72.1 and 8 radiographs in group S72.2 were missing for AO classification (Supplementary Table 1).
Hip fracture treatment protocol
Femoral neck fractures were operated on using total hip arthroplasty (THA), hemiarthroplasty (HA), or cannulated screws. Trochanteric hip fractures were operated on with intramedullary nail (IMN) or dynamic hip screw (DHS) systems. Some trochanteric fractures were stabilized with a DHS and a lateral buttress plate or a DHS and cannulated screws. Subtrochanteric fractures were operated on using IMNs. A single-dose antibiotic prophylaxis cefuroxime 3 g i.v. (or 1.5 g i.v. for patients < 50 kg) was administered 30–60 min prior to the incision. Low molecular weight heparin (enoxaparin 40 mg once a day s.c., starting at 6 h after the operation) for 3 weeks was administered to all patients for antithrombotic prophylaxis. Mobilization and weight bearing were allowed according to the surgeon’s evaluation, and all patients were mobilized under the supervision of a physical therapist.
Survival
Dates of death were collected from the national administrative register, the Causes-of-Death Register of Statistics Finland, using the unique personal identification numbers of the patients.
The survival follow-up time was from January 1, 2005, to September 9, 2021. All patients were followed for a minimum of 14 years. The variables explaining survival were assessed at 1 and 14 years after the index fracture. In addition, the variables explaining mortality at 14 years among AI patients were assessed.
Statistical methods
Differences between two groups were tested with chi-squared (χ2) test, Fisher’s exact test, or the Wilcoxon rank test, and between three groups with the Kruskal–Wallis test. Differences in mean values between groups were tested using two-way analysis of variance (ANOVA).
In the univariate analyses, likelihood ratios (LR) were calculated for all classes of each variable and compared with each other within the variable. In univariate analysis on the mortality of AI patients vs other patients, ORs (odds ratios) were calculated. Statistical dependency within each variable was analyzed using the chi-squared (χ2) or Wilcoxon signed rank test.
Multivariate analysis was performed using an optimizing stepwise procedure based on the Bayesian approach to determine posterior probabilities and likelihood ratios and to ascertain the sensitivity and specificity of the rule [23]. The optimizing procedure has been developed mainly for categorized variables and it does not need a perfect variable matrix. Following a heuristic approach, the procedure selects the combination of variables that best explains the selected outcome variable. The Bayesian approach is applied by calculating posterior probability ratios for each combination. The aim is to find an optimal set of variables that provides a better explanation than all of the variables together. The relationship between the true positives and true negatives was expressed as the area under the curve (AUC) that approximately describes the explanatory power of the model.
Survival and excess mortality
Furthermore, survival was analyzed according to sex and the involvement of alcohol in relation to the reference population using the life table method [24]. In this method, the observed survival rates of the groups were compared with the survival rates based on age-, sex-, and time-specific life tables for the entire population of Finland (reference population). The calculated survival of the reference population is 1.00. If the survival curve of the study group remains below the survival of the reference population, there is excess mortality in the study group.
We performed the univariate analyses and multivariate analyses for 1-year and 14-year survival for the following seven variables: sex, age, ASA class, BMI, comorbidity, fracture type, and operation method, including the type of implant. In addition, we performed the univariate analyses and multivariate analyses for 14-year mortality among patients with AI for the following preoperative factors: age, sex, ASA class, and fracture type.
Results
During the study period, a total of 486 patients with a new low-energy hip fracture were enrolled in the study (Supplementary Fig. 1). Table 1 and Supplementary Table 1 list the patient characteristics. Of the patients, 67.9% were women, with a mean age of 82.4 years (SD 8.9 years, range: 49–102 years). The mean age of men was 72.0 (SD 14.8, range: 36–99 years). In cases where alcohol was involved (AI; n = 39, 8%), the patients differed significantly from the other patients regarding age, ASA class, and comorbidities, but not regarding the type of fracture. Most of the patients with AI (n = 35/39; 90%) were men (age range: 35–69 years). The age range in the four women with AI, correspondingly, was 56–73 years.
When analyzing the age differences among AI patients and non-AI patients according to the different age groups (40 years; 50 years; 60 years; 70 years; 80 years; and 90 + years), we found that the patients with AI were significantly younger than the non-AI patients (Wx = − 9.40, p < 0.001). The mean age of all patients with AI was 55.7 (SD 8.3) years and that of all patients 79.0 (SD 12.1) years. Patients with AI mainly had an ASA class of 1–2 (67%), whereas the non-AI patients mainly had an ASA class of 3–4 (80.5%; Kruskal–Wallis 113.3, d.f.2, p < 0.001). Patients with AI also had fewer comorbidities (χ2 = 27.83, p < 0.05). No association was found between BMI categories and ASA scores (Kruskal–Wallis 2.13, d.f.3, n.s.). The hip fractures were distributed as follows: 59% were femoral neck fractures, 36% pertrochanteric fractures, and 5% subtrochanteric fractures (Supplementary Table 1).
Mortality
The mortality of both sexes in all patients (n = 486) during the 14-year follow-up time is shown in Table 2. There were no differences in the mortality between different fracture types (χ2 = 1.16, n.s.). In addition, we studied the mortality of hip fracture patients who were sober (n = 447, 326 females, 121 males) and of those with AI (n = 39) (Supplementary Table 2). At the end of the survival follow-up period (14 years), 11% of the patients who were sober (50/447) and 33% (13/39) of the patients with AI were alive; out of the overall study cohort, 13% (63/486) of the patients were alive.
After 4 years, over half of the patients with no AI (235/447) had died. A statistically significant difference in mortality between the sexes in the non-AI group was noticed between the first and fifth year and at 14 years, and during the 14 postoperative years, the mortality among patients with AI was lower than among the other patients (Supplementary Table 2). Patients who survived were approximately 19.5 years younger than those who died during the 14-year follow-up: 62 (SD 13.3) vs 81 (SD 9.7) years.
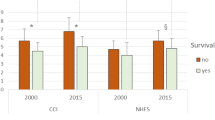
Survival and excess mortality
The 1-year and 14-year univariate analyses are shown in Tables 3 and 4, respectively. Two out of the 63 (3.1%) patients with a BMI of < 20 kg/m2 and 47 out the of 297 (15.8%) patients with a BMI of ≥ 20 kg/m2 were alive at 14 years postoperatively (Fisher’s exact p = 0.0007) (Tables 3 and 4). The multivariate analysis (Table 5) demonstrated that ASA class (1–3) at the time of fracture was the most important factor explaining 1-year survival, followed by BMI ≥ 20 kg/m2; age under 85 years; no comorbidity; AI; and Alzheimer’s disease; operative methods NFB20, NFJ54, NFJ50, or NFB30-50; as well as female sex (Table 5). In the multivariate analysis regarding 14-year survival, age under 75 years at the time of fracture was the most protective factor, followed by BMI ≥ 20 kg/m2, ASA class (1–2), fracture type (S72.2), operative method (NFJ50, NFJ54, or NFB30-50), and no comorbidity or AI (Table 5).
The 1-year model correctly predicted 76% of the cases, and the 14-year model, correspondingly, predicted 88% of the cases. The optimum results of the multivariate survival models at 1 and at 14 years are shown in Supplementary Table 3. The kappa (κ) value for the 1-year survival model was 0.39 (95% CI 0.29–0.49; fair), and the AUC was 0.78. The κ for the 14-year survival model was 0.56 (moderate; 95% CI 0.45–0.66), and the AUC was 0.90.
In the mortality analyses on patients with AI vs other patients, the most important factors were age < 54 years and male sex, followed by ASA class (1–2) and trochanteric fractures (Supplementary Tables 4 and 5).
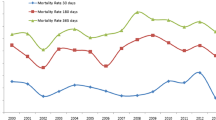
In the total population, the excess mortality was higher among men than women during the first 10 years. After 10 years, the excess mortality was nearly equal in both sexes. In men, excess mortality subsided and remained steady after 7.5 years (Fig. 1). However, the lowest excess mortality was among patients (90% men) with AI because of their significantly lower mean age compared to the mean age of the other male patients.
Discussion
Increased mortality following hip fractures during the first postoperative year is well documented [25]. In our study, the statistically significant preoperative variables in the univariate analysis that predicted significantly higher survival at 12 months after hip fracture surgery were female sex, age < 85 years, ASA class 1–3, BMI ≥ 20 kg/m2, preoperative comorbidities (no comorbidity, AI, or Alzheimer’s disease), certain fracture types (femoral neck or subtrochanteric fracture), and certain operative methods (cemented hemiarthroplasty, osteosynthesis of the neck with cannulated screws, osteosynthesis with an intramedullary nail, or total arthroplasty). According to a Swedish national data register from January 2014 to December 2016, including 10,548 patients with trochanteric and subtrochanteric fractures, there were no significant differences in the 1-year mortality between simple (26%), multifragmented (27%), and reverse oblique and subtrochanteric fractures (24%) [26]. The more complex fractures did not affect the survival at 1 year.
In a Swedish retrospective registry-based cohort study (n = 1493) regarding 1-year mortality, results similar to our present study were found [10]. Mortality was significantly associated with age, male sex, and ASA class 3–5, but the type of fracture or operation method did not affect the mortality estimates [10]. Different results have also been reported. A recent Finnish prospective study on home-dwelling hip fracture patients (n = 538) showed no sex-related differences in mortality at 4 and 12 months postoperatively [27]. Furthermore, one opposite result had been published—in an earlier prospective study (n = 106) from Finland, the 1-year mortality was higher in women than in men (34% vs 28%), although the difference was not significant [28].
Furthermore, a Norwegian study (n = 942, mean age 81.2 years) reported that the elevated mortality at 1 year and 5 years postoperatively was significantly associated with male sex and age over 80 years [7]. The overall mortality after the first year was 21% and after 5 years 59% [7]. In the present study (mean age 79 (SD 12.1 years), the corresponding results were similar, 22% and 57%, respectively.
A Danish national register study [17] showed that the postoperative mortality after hip fractures varied between 2000 and 2013 but did not decline. The mortality rate was 10% at 30 days, 16% at 90 days, and 27% at 1 year [17]. In Denmark, the median length of the postoperative acute hospital stay in 2014 (8 days) [17] was similar to that of our study (9 days).
A Spanish study (n = 359) reported an overall in-hospital mortality rate of 6% and an overall mortality rate of 27% at 1 year after the index fracture (38% in men and 24% in women) [29]. In the present study, the 30-day mortality was 7%, the 90-day mortality 14%, and the 1-year mortality 22%, and there were no significant differences between the sexes during the first year or between 4 and 9 years postoperatively. However, the mortality was significantly higher among men during the 2nd and 3rd postoperative years. However, during the 10th–14th postoperative years, the mortality was significantly higher among women. When the mortality during the first 14 postoperative years was analyzed only among patients without alcohol involvement (n = 447), there was a significant difference between women and men at the first to fifth postoperative year. The corresponding mortality rates among patients with AI (39/486, 8%) at 30 days, at 90 days, and 1 year were lower: 5%, 10%, and 15%, respectively. The difference was not significant.
An earlier Finnish hip fracture study (n = 221) showed that the survival at 11 years postoperatively was better among men than women according to the concomitant use of prescribed calcium plus vitamin D and anti-osteoporotic drugs. A similar result was observed among non-users (men vs women) [14].
In the literature on low-energy hip fractures, all hip fracture patients are usually included in the study reports without separately analyzing the consumption of alcohol before the injury (10, 17, 30). However, the age distribution of patients with acute alcohol intoxication differed from other hip fracture patients [31], as was shown in our present data. In this study, the mean age of patients under the influence of alcohol (8% of total) at the time of presenting at the emergency department was significantly lower than that of the other patients.
The relative survival among patients with AI in the present study (90% male patients) during the 14-year follow-up was quite similar to that of female patients, although slightly higher. A large American study showed an opposite result: the 1-year post-fracture mortality among hip fracture patients with an alcohol-related disease was significantly higher than that of hip fracture patients with no history of alcohol abuse [32]. However, that study included hip fracture patients with alcohol-related diseases: alcohol dependence (59%), alcoholic liver disease (17%), alcoholic psychoses (10%), and chronic alcohol abuse (10%) [32]. Their ASA class was higher, at least class 3. In the present study, the patients with AI had no alcohol-related diseases, and their ASA class was mainly 1–2.
According to a recent European analysis carried out in 22 countries, the mean 1-year mortality was 23.3% (SD 6.3%, median 23.4%) [30], which is similar to our study.
Longer follow-up studies suggesting that the excess mortality associated with hip fractures may persist for several years are scarce [16, 33]. Opposite results have also been published. A study from the USA (1116 hip fracture cases with 4464 age-matched controls) showed that the mortality risks for fracture and non-fracture participants were generally similar after the first year [34].
In the present study, male sex, age < 75 years, some operative methods (osteosynthesis with intramedullary nail, with cannulated screws, total arthroplasty), preoperative comorbidities (no comorbidities, AI), a subtrochanteric fracture, ASA class 1–2, and BMI ≥ 20 kg/m2 explained survival at 14 years. The reasons for the better survival of patients with AI in the present study were their significantly lower age and significantly fewer comorbidities compared to the other patients. The third reason was that two-thirds of them had an ASA class of 1–2. However, relatively young male AI patients with a good preoperative condition had the highest mortality risk at 14 years.
According to an earlier study with the same patients, 34% of all reoperations occurred during the first postoperative months and roughly 73% during the first postoperative year. The observed survival of the reoperated women was higher than that of the non-reoperated women during a 10-year follow-up [15]. At the end of the 10-year follow-up, 37% of the reoperated patients were alive and only 17% of the non-reoperated patients were alive [15].
Previously, in a 10-year follow-up study from Estonia, a number of factors, such as advanced age, male sex, poor health status, and preoperative comorbidities, were associated with excess mortality following hip fractures [35]. The excess risk of death was highest within 3–6 months after fracture and persisted for the full 10-year follow-up period [35]. The immediate excess risk of death was high in older age groups (≥ 80 years), and there was a gradually accumulating excess risk in younger age groups (50–79 years) [35].
The present results differ from several other studies [6, 7] in which men had a higher overall mortality rate than women. The univariate analysis in the present study showed that male sex explained higher survival at 14 years postoperatively. The present study indicated that a low BMI (< 20 kg/m2) was an inverse factor for long-term survival. At 14 years, the mortality of patients with a low BMI (< 20 kg/m2) was six-fold compared to those with a BMI of ≥ 20 kg/m2. Similarly, in a Swiss study, hip fracture patients with a BMI of < 22 kg/m2 had seven-fold mortality compared to those with a BMI of > 25 kg/m2 at 1 year postoperatively [36]. Malnutrition is very prevalent among older people with hip fractures, and it negatively influences functional recovery during rehabilitation. Postoperative nutritional assessments and the treatment of malnutrition improve the functional recovery and decrease mortality [37].
According to the present results, the excess mortality was higher among men during the first 9 years, but it was nearly equal in both sexes after 10 years. At the end of the follow-up time, the excess mortality in both sexes remained quite stable. A similar result was found in a Norwegian 5-year follow-up study (n = 942) [7]. An over 12-year follow-up study on eight cohorts in Europe and the USA (n = 122,808) showed that hip fracture patients had the highest risk of dying during the first year after the fracture and an almost two-fold increase in mortality, which persisted even 8 years or more after the injury [38]. However, the sex-related difference in excess mortality was minimal in this study [38]. In a Swedish 22-year follow-up study (n = 1013), the survival among women was better than among men, and the excess mortality was higher over two decades of follow-up compared to the control population [39].
A Danish national register study (n = 113,721) conducted over 15 years from 2000 to 2014 reported that male sex, increasing age, a higher Charlson Comorbidity Index, a per- and subtrochanteric fracture, and an operation type other than total hip arthroplasty were independently associated with postoperative mortality [17]. The results were in line with those of the present study regarding age under 75 years, some comorbidities, and total hip arthroplasty. However, in the present study, the univariate analysis showed that male sex, subtrochanteric fractures, and some operative methods, such as osteosynthesis with an intramedullary nail or osteosynthesis of the femoral neck with screws, were associated with better survival at 14 years postoperatively.
Several studies indicate that heavy alcohol consumption is associated with an increased risk of hip fractures due to an increased tendency to fall [40,41,42]. According to an earlier Finnish study on male femoral neck fracture patients with alcohol dependence syndrome (ICD 10 code F10.2; mean age 64 years, range 29–94 years), approximately 50% of the patients were under 70 years old. The survival rate was 62% at 1 year and 49% at 2 years [42].
The Finnish national hip fracture database study revealed a higher risk of an early readmission due to surgical complications among patients with alcohol abuse issues [43]. Our previous 10-year follow-up study on hip fracture patients showed that over a third of the patients with recorded alcohol involvement needed reoperations after their primary operation [15].
In Finland, the incidence of hip fractures among elderly individuals has declined during the twenty-first century [3]. However, because of the rapid aging of the Finnish population, the burden of hip fractures leads to an increase in the absolute number of hip fractures. Efforts to prevent low-energy fractures, such as the prevention of falls and the treatment of osteoporosis at least after the first fragility fracture, are cost-effective [44]. The treatment of malnutrition is also important among elderly hip fracture patients [41].
Strengths and limitations
The strength of this study is the long follow-up, reporting the survival and excess mortality of hip fracture patients. The study consists of detailed patient-specific data, with a large number of consecutive patients treated at a single hospital. All medical records and radiographs were reviewed by one of the authors (R.T.). A strength also is the Bayesian multivariate method, which takes into account all factors available. Furthermore, we were able to compare the patients’ survival to that of the age- and sex-adjusted population in Finland.
The present study is representative for Finland. In 2006, the population of the hospital district in question was approximately 210,000, which represented 4% of the Finnish population (5256 million) and 4.2% of the Finnish population aged ≥ 50 years (Statistics Finland). The rate of hip fractures (n = 486; 68% females) in the present study represented 4.2% of the total number of hip fractures in Finland in 2005 and 2006 (n = 11,662; 68% females). The mean age of these patients nationally was 79 years, as in the present study. The national rate of femoral neck fractures was 63%, of trochanteric fractures 31%, and of subtrochanteric fractures 6% [45, 46]. In the present study, the corresponding rates were 58%, 36%, and 5%. The first Finnish National Care Guidelines on hip fracture patients were published in January 2006. However, the operative treatment of hip fractures in Finland was already carried out in the beginning of 2000 according to the first guidelines and the operative treatment has not significantly changed in the two revised guidelines in 2011 and 2017 [47]. Thus, the hip fracture treatment in the present study is still up to date. Although some surgical methods have been improved since our data, the choice of surgical methods does not seem to affect mortality after hip fractures. According to a recent Finnish dissertation, there was no statistically significant difference in mortality for cemented or uncemented hemiarthroplasty at 1 year postoperatively (national register data: n = 25,174) [48]. The dissertation also showed that the more expensive intramedullary implants did not lead to better clinical outcomes than extramedullary implants for the treatment of trochanteric fractures (national register data: n = 14,915) [48]. Also, the choice of implant in femoral neck fractures (total hemiarthroplasty or hemiarthroplasty) does not affect the mortality of these patients [49].
The retrospective study design can be regarded as a limitation of the study; however, all required patient-specific data were available due to standardized treatment protocols and the short patient enrolment period.
In the present study, we did not ask the patients whether they used calcium and/or vitamin D supplementation and/or anti-osteoporotic drugs on a daily basis before the injury or postoperatively. Neither did we measure the serum level of 25-hydroxyvitamin D after admission to the hospital. Economic reasons related to the study group restricted such measurements, as well as the use of the national prescription database maintained by the Social Insurance Institution to obtain data on the use of anti-osteoporotic drugs. Moreover, for the present study, the use of vitamin D and calcium supplements could not be obtained from the national prescription register because, since 2006, these supplements have been available over the counter in Finland.
Conclusions
In this comprehensive study on survival after hip fractures among the elderly, we followed 85% of the patients until their death. The three most protective factors for 1-year survival in order of importance were ASA class, BMI, and age, and the four most protective factors for 14-year survival were age, BMI, ASA class, and a subtrochanteric fracture type. The study showed an elevated mortality risk among hip fracture patients compared with that of the general population during the 14 post-fracture years.
Finally, the first SARS-CoV-2 virus infection in Finland was reported on January 19, 2020. The first death due to SARS-CoV-2 virus in Finland occurred on March 20, 2020. A total of 558 (1% of all deaths) persons, with a median age of 84 years, died of a SARS-CoV-2 viral infection in Finland in 2020 (Statistics Finland). The mortality and life table analyses did not reveal any sudden decrease in survival rates in this cohort in 2020 and in 2021.
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by RT, J-PK, and PL. MK performed the statistical analysis. PL, TH, IN-L, and RT wrote the initial draft. All authors have given final approval of the version to be published and agree to be accountable for all aspects of the work. RT is the guarantor for the article.
References
Dhanwal DK, Dennison EM, Harvey NC, Cooper C (2011) Epidemiology of hip fracture worldwide geographic variation. Indian J Orthop 45:15–22. https://doi.org/10.4103/0019-5413.73656
Bergström U, Jonsson H, Gustafson Y, Pettersson U, Stenlund H, Svensson O (2009) The hip fracture incidence curve is shifting to the right. Acta Orthop 80:520–524. https://doi.org/10.3109/17453670903278282
Kannus P, Niemi S, Parkkari J, Sievänen H (2018) Continuously declining incidence of hip fracture in Finland: analysis of nationwide database in 1970–2016. Arch Geriatr Geront 77: 64–67. https://www.sciencedirect.com/science/journal/01674943
Swayambunathan J, Dasgupta A, Rosenberg PS, Hannan MT, Kiel DP, Bhattacharyya T (2020) Incidence of hip fracture over 4 decades in the Framingham Heart Study JAMA. Intern Med 180:1225–1231. https://doi.org/10.1001/jamainternmed.2020.2975
Sambrook P, Cooper C (2006) Osteoporosis. Lancet 367:2010–2018. https://doi.org/10.1016/S0140-6736(06)68891-0
Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390. https://doi.org/10.1059/0003-4819-152-6-201003160-00008
Diamantopoulos AP, Hoff M, Skoie IM, Hochberg M, Haugeberg G (2013) Short- and long-term mortality in males and females with fragility hip fracture in Norway A population-based study. Clin Interv Aging 8:817–823. https://doi.org/10.2147/CIA.S45468
Lüthje P, Helkamaa T, Kaukonen J-P, Nurmi-Lüthje I, Kataja M (2012) A long-term follow-up of 221 hip fracture patients in southeastern Finland analysis of survival and prior or subsequent fractures. Archiv Gerontol Geriatr 54:e294–e299. https://doi.org/10.1016/j.archger.2011.12.002
Reito A, Kuoppala M, Pajulampi H, Hokkinen L, Kyrölä K, Paloneva J (2019) Mortality and comorbidity after non-operatively managed, low-energy pelvic fracture in patients over age 70: a comparison with an age-matched femoral neck fracture cohort and general population. BioMed Central Geriatrics 19. https://doi.org/10.1186/s12877-019-1320-y
Åhman R, Siverhall PF, Snygg J, Fredrikson M, Enlund G, Björnström K, Chew MS (2018) Determinants of mortality after hip fracture surgery in Sweden a registry-based retrospective cohort study. Sci rep 8:15695. https://doi.org/10.1038/s41598-018-33940-8
Stenvall M, Olofsson B, Nyberg L, Lundström M, Gustafson Y (2007) Improved performance in activities of daily living and mobility after a multidisciplinary postoperative rehabilitation in older people with femoral neck fracture a randomized controlled trial with 1-year follow-up. J Rehabil Med 8:232–239. https://doi.org/10.2340/16501977-0045
Weller I, Wai EK, Jaglal S, Kreder HJ (2005) The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br 87:361–366. https://doi.org/10.1302/0301-620x.87b3.15300
Lee YK, Lee YJ, Ha YC, Koo KH (2014) Five-year relative survival of patients with osteoporotic hip fracture. J Clin Endocrinol Metab 99:97–100. https://doi.org/10.1210/jc.2013-2352s
Nurmi-Lüthje I, Lüthje P, Kaukonen JP, Kataja M (2015) Positive effects of a sufficient pre-fracture serum vitamin D level on the long-term survival of hip fracture patients in Finland a minimum 11-year follow-up. Drugs Aging 32:477–486. https://doi.org/10.1007/s40266-015-0267-8
Tiihonen R, Alaranta R, Helkamaa T, Nurmi-Lüthjes I, Kaukonen JP, Lüthje P (2019) A 10-year retrospective study of 490 hip fracture patients reoperations, direct medical costs, and survival. Scand J Surg 108:178–184. https://doi.org/10.1177/1457496918798197
von Friesendorff M, Besjakov J, Akesson K (2008) Long-term survival and fracture risk after hip fracture a 22-year follow-up in women. J Bone Miner Res 23:1832–1841. https://doi.org/10.1359/jbmr.080606
Gundel O, Thygesen LC, Gögenur I, Ekelöf S (2020) Postoperative mortality after a hip fracture over a 15-year period in Denmark a national register study. Acta Orthop 91:58–62. https://doi.org/10.1080/17453674.2019.1680485
Smith T, Pelpola K, Ball M, Ong A, Myint PK (2014) Pre-operative indicators for mortality following hip fracture surgery a systematic review and meta-analysis. Age Ageing 43:464–471. https://doi.org/10.1093/ageing/afu065
American Society of Anesthesiologists. New classification of physical status. Anesthesiology 1963; 24: 111. http://journals.lww.com/anesthesiology/toc/1963/01000
Garden R S (1961) Low-angle fixation in fractures of the femoral neck. J Bone Jt Surg 43-B, 647–663. https://doi.org/10.1302/0301-620X.43B4.647
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L (2007) Fracture and dislocation classification compendium - 2007 Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 21(10 Suppl):S1-133. https://doi.org/10.1097/00005131-200711101-00001
Saarenpää I, Partanen J, Jalovaara P (2002) Basicervical fracture- a rare type of hip fracture. Arch Orthop Trauma Surg 122:69–72. https://doi.org/10.1007/s004020100306
Aine R, Kataja M, Alavaikko M (1984) Prognostic factors for non-cleaved follicular center-cell lymphomas and immunoblastic sarcoma. A Bayesian approach Scand J Haematol 32:475–87. https://doi.org/10.1111/j.1600-0609.1984.tb02188.x
Hakulinen T (1977) On long-term relative survival rates. J Chron Dis 30:431–443. https://doi.org/10.1016/0021-9681(77)90036-4
Hung LW, Tseng WJ, Huang GS, Lin J (2014) High short-term and long-term excess mortality in geriatric patients after hip fracture: a prospective cohort study in Taiwan. BMC Musculoskelet Disord 15:151. https://www.biomedcentral.com/1471-2474/15/151
Mattisson L, Bojan A, Enocson A (2018) Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord 19:369. https://doi.org/10.1186/s12891-018-2276-3
Lahtinen A, Leppilahti J, Vähänikkilä H, Kujala S, Ristiniemi J, Jalovaara P (2020) No major differences in recovery after hip fracture between home-dwelling female and male patients. Scand J Surg 109:250–264. https://doi.org/10.1177/1457496919847932
Nurmi I, Narinen A, Lüthje P, Tanninen S (2004) Functional outcome and survival after hip fracture in elderly: a prospective study in 106 consecutive patients. J Orthopead Traumatol 4:7–14. https://doi.org/10.1007/s10195-004-0033-x
Rey-Rodriguez MM, Vasquez-Gamez MA, Giner M, Garrachon-Vallo F, Fernandez-Lopez L, Colmenero MA, Montoya-Garcia MJ (2020) Incidence, morbidity and mortality of hip fractures over a period of 20 years in a health area of Southern Spain. BMJ Open 10:e037101. https://doi.org/10.1136/bmjopen-2020-037101
Downey C, Kelly M, Quinlan JF (2019) Changing trends in the mortality rate at 1-year post hip fracture-a systematic review. World J Orthop 10:166–175. https://doi.org/10.5312/wjo.v10.i3.166
Tiihonen R, Paattiniemi EL, Nurmi-Lüthje I, Kaukonen JP, Sarkkinen H, Lüthje P (2021) No change in the use of alcohol among hip fracture patients over a 12-year period: a prospective study in south-eastern Finland. Acta Orthop. Belg., 2021, 87 e-supplement 1, 89–97. http://www.actaorthopaedica.be/assets/3131/13-Tihonen.pdf
Yuan Z, Dawson N, Cooper GS, Einstadter D, Cebul R, Rimm AA (2001) Effects of alcohol-related disease on hip fracture and mortality a retrospective cohort study of hospitalized Medicare beneficiaries. Am J Public Health 9:1089–1093. https://doi.org/10.2105/ajph.91.7.1089
Galler M, Zellner M, Roll C, Bäuml C, Füchtmeier B, Müller F (2018) A prospective study with ten years follow-up of two-hundred patients with proximal femoral fracture. Injury 49:841–845. https://doi.org/10.1016/j.injury.2018.02.026
LeBlanc ES, Hillier TA, Pedula KL et al (2011) Hip fracture and increased short-term but not long-term mortality in healthy older women. Arch Intern Med 171:1831–1837. https://doi.org/10.1001/archinternmed.2011.447
Jürisson M, Raag M, Kallikorm R, Lember M, Uusküla A (2017) The impact of hip fracture on mortality in Estonia a retrospective population-based cohort study. BMC Musculoskelet Disord 18:243. https://doi.org/10.1186/s12891-017-1606-1
Schaller F, Sidelnikov E, Theiler R, Egli A, Staehelin HB, Dick W, Dawson-Hughes B, Grob D, Platz A, Can U, Bischoff-Ferrari HA (2012) Mild to moderate cognitive impairment is a major risk factor for mortality and nursing home admission in the first year after hip fracture. Bone 51:347–352. https://doi.org/10.1016/j.bone.2012.06.004
Malafarina V, Reginster JY, Cabrerizo S, Bruyère O, Kanis JA, Martinez JA, Zulet MA (2018) Nutrients 10555 https://doi.org/10.3390/nu10050555
Katsoulis M, Benetou V, Karapetyan T, Feskanich D, Grodstein F, Pettersson-Kymmer U, Eriksson S, Wilsgaard T, Jørgensen L, Ahmed LA, Schöttker B, Brenner H, Bellavia A, Wolk A, Kubinova R, Stegeman B, Bobak M, Boffetta P, Trihopoulou A (2017) Excess mortality after hip fracture in elderly persons from Europe and the USA the CHANCES project. J Inter Med 281:300–310. https://doi.org/10.1111/joim.12586
von Friesendorff M, McGuigan FE, Wizert A, Rogmark C, Holmberg AH, Woolf AD, Akesson K (2016) Hip fracture, mortality risk, and cause of death over two decades. Osteoporos Int 27:2945–2953. https://doi.org/10.1007/s00198-016-3616-5
Trimpou P, Landin-Wilhelmsen K, Odén A, Rosengren A, Wilhelmsen L (2010) Male risk factors for hip fracture-a 30-year follow-up study in 7,495 men. Osteoporos Int 21:409–416. https://doi.org/10.1007/s00198-009-0961-7
Zhang X, Yu Z, Yu M, Qu X (2015) Alcohol consumption and hip fracture risk. Osteoporos Int 26:531–540. https://doi.org/10.1007/s00198-014-2879-y
Kosola J, Kaipia A, Laitinen MK, Nieminen J (2017) Complications after surgical treatment of femoral neck fractures in men with alcohol dependence syndrome retrospective register analysis of 154 cases. Arch Orthop Trauma Surg 137:967–973. https://doi.org/10.1007/s00402-017-2713-z
Yli-Kyyny TT, Sund R, Heinänen M, Malmivaara A, Kröger H (2019) Risk factors for early readmission due to surgical complications after treatment of proximal femoral fractures – a Finnish National Database study of 68,800 patients. Injury 50:403–408. https://doi.org/10.1016/j.injury.2018.10.030
Svedbom A, Hadji P, Hernlund E, Thoren R, McCloskey E, Stad R, Stollenwerk B (2019) Cost-effectiveness of pharmacological fracture prevention for osteoporosis as prescribed in clinical practice in France. Germany, Italy, Spain, and the United Kingdom, Osteoporos Int 30:1745–1754. https://doi.org/10.1007/s00198-019-05064-w
Sund R, Juntunen M, Lüthje P, Huusko T, Häkkinen U (2011) Monitoring the performance of hip fracture treatment in Finland. Ann Med 43(Suppl 1):S39-46. https://doi.org/10.3109/07853890.2011.586360
Pekonen SR, Kopra J, Kröger H, Rikkonen T, Sund R (2021) Regional and gender-specific analyses give new perspectives for secular trend in hip fracture incidence. Osteoporos Int 32:1725–1733. https://doi.org/10.1007/s00198-021-05906-6
Hip fracture: current care guidelines. Working group set up by the Finnish Medical Society Duodecim and the Finnish Orthopedic Society 2017. Available online at: www.kaypahoito.fi
Yli-Kyyny T (2022) Outcomes of hip fracture surgery. Dissertation. Publications of University of Eastern Finland 2022 http://urn.fi/URN:ISBN:978-952-61-4533-4
Rogmark C (2020) Further refinement of surgery will not necessarily improve outcome after hip fracture. Acta Orthop 91:123–124. https://doi.org/10.1080/17453674.2019.1706936
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the ethics committee of Päijät-Häme Central Hospital, Finland.
Informed consent
For this type of study, informed consent is not required.
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tiihonen, R., Helkamaa, T., Nurmi-Lüthje, I. et al. Patient-specific factors affecting survival following hip fractures—a 14-year follow-up study in Finland. Arch Osteoporos 17, 107 (2022). https://doi.org/10.1007/s11657-022-01148-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01148-z