Abstract
Objectives
Medication errors can happen at any phase of the medication process at health care settings. The objective of this study is to identify the characteristics of severe prescribing errors at a pediatric hospital in the inpatient setting and to provide recommendations to improve medication safety and rational drug use.
Methods
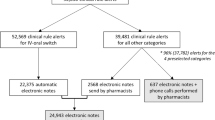
This descriptive retrospective study was conducted at a tertiary pediatric hospital using data collected from Jan. 1st, 2019 to Dec. 31st, 2020. During this period, the Prescription Pre-audit Intelligent Decision System was implemented. Medication orders with potential severe errors would trigger a Level 7 alert and would be intercepted before it reached the pharmacy. Trained pharmacists maintained the system and facilitated decision making when necessary. For each order intercepted by the system the following patient details were recorded and analyzed: patient age, patient’s department, drug classification, dosage forms, route of administration, and the type of error.
Results
A total of 2176 Level 7 medication orders were intercepted. The most common errors were associated with drug dosage, administration route, and dose frequency, accounting for 35.2%, 32.8% and 13.2%, respectively. Of all the intercepted oerrors. 53.6% occurred in infants aged < 1 year. Administration routes involved were mainly intravenous, oral and external use drugs. Most alerts came from the neonatology department and constituted 40.5% of the total alerts, followed by the nephrology department 15.9% and pediatric intensive care unit (PICU) 11.3%. As to dosage forms, injections accounted for 50.4% of alerts, with 21.3% attributable to topical solutions, 9.1% to tablets, and 5.7% to inhalation. Anti-infective agents were the most common therapeutic drugs prescribed with errors.
Conclusions
The Prescription Pre-audit Intelligent Decision System, with the supervision of trained pharmacists can validate prescriptions, increase prescription accuracy, and improve drug safety for hospitalized children. It is a medical service model worthy of consideration.

Similar content being viewed by others
References
Ben Natan M, Sharon I, Mahajna M, Mahajna S. Factors affecting nursing students’ intention to report medication errors: an application of the theory of planned behavior. Nurse Educ Today. 2017;58:38–42.
Björkstén KS, Bergqvist M, Andersén-Karlsson E, Benson L, Ulfvarson J. Medication errors as malpractice-a qualitative content analysis of 585 medication errors by nurses in Sweden. BMC Health Serv Res. 2016;16(1):431.
Dirik HF, Samur M, Seren Intepeler S, Hewison A. Nurses’ identification and reporting of medication errors. J Clin Nurs. 2019;28(5–6):931–8.
Wittich CM, Burkle CM, Lanier WL. Medication errors: an overview for clinicians. Mayo Clin Proc. 2014;89(8):1116–25.
Elshayib M, Pawola L. Computerized provider order entry-related medication errors among hospitalized patients: an integrative review. Health Inform J. 2020;26(4):2834–59.
Tariq RA, Vashisht R, Sinha A, Scherbak Y. Medication dispensing errors and prevention. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2021, StatPearls Publishing LLC.; 2021.
Yi ZM, Sun SS, Li XX, Lu M, Zhai SD. An evaluation of clinical pharmacist service on a neurology care unit. Int J Clin Pharm. 2016;38(1):30–3.
Pevnick JM, Nguyen C, Jackevicius CA, Palmer KA, Shane R, Cook-Wiens G, et al. Improving admission medication reconciliation with pharmacists or pharmacy technicians in the emergency department: a randomised controlled trial. BMJ Qual Saf. 2018;27(7):512–20.
Naseralallah LM, Hussain TA, Jaam M, Pawluk SA. Impact of pharmacist interventions on medication errors in hospitalized pediatric patients: a systematic review and meta-analysis. Int J Clin Pharm. 2020;42(4):979–94.
Rodrigues JPV, Marques FA, Gonçalves A, Campos MSA, Reis TMD, Morelo MRS, et al. Analysis of clinical pharmacist interventions in the neurology unit of a Brazilian tertiary teaching hospital. PLoS ONE. 2019;14(1): e0210779.
Huynh C, Wong ICK, Correa-West J, Terry D, McCarthy S. Paediatric patient safety and the need for aviation black box thinking to learn from and prevent medication errors. Paediatr Drugs. 2017;19(2):99–105.
Kaushal R, Bates DW, Landrigan C, McKenna KJ, Clapp MD, Federico F, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285(16):2114–20.
Cuzzolin L, Atzei A, Fanos V. Off-label and unlicensed prescribing for newborns and children in different settings: a review of the literature and a consideration about drug safety. Expert Opin Drug Saf. 2006;5(5):703–18.
Stephenson T. How children’s responses to drugs differ from adults. Br J Clin Pharmacol. 2005;59(6):670–3.
Benjamin L, Frush K, Shaw K, Shook JE, Snow SK. Pediatric medication safety in the emergency department. Ann Emerg Med. 2018;71(3):e17–e24.
Sakuma M, Ida H, Nakamura T, Ohta Y, Yamamoto K, Seki S, et al. Adverse drug events and medication errors in Japanese paediatric inpatients: a retrospective cohort study. BMJ Qual Saf. 2014;23(10):830–7.
Prgomet M, Li L, Niazkhani Z, Georgiou A, Westbrook JI. Impact of commercial computerized provider order entry (CPOE) and clinical decision support systems (CDSSs) on medication errors, length of stay, and mortality in intensive care units: a systematic review and meta-analysis. J Am Med Inform Assoc. 2017;24(2):413–22.
Nuckols TK, Smith-Spangler C, Morton SC, Asch SM, Patel VM, Anderson LJ, et al. The effectiveness of computerized order entry at reducing preventable adverse drug events and medication errors in hospital settings: a systematic review and meta-analysis. Syst Rev. 2014;3:56.
Pons-Mesquida M, Oms-Arias M, Figueras A, Diogène-Fadini E. Impact of a system to assist in clinical decision-making in primary healthcare in Catalonia: prescription Self Audit. BMC Med Inform Decis Mak. 2022;22(1):70.
Rovira-Simón J, Sales ICM, Pozo-Rosich P, Gates D, Patt C, Hennessey I, et al. Introduction to the cognitive hospital. Future Healthc J. 2022;9(1):34–40.
Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med. 2020;3:17.
Li R, Niu Y, Scott SR, Zhou C, Lan L, Liang Z, et al. Using Electronic Medical Record Data for Research in a Healthcare Information and Management Systems Society (HIMSS) analytics electronic medical record adoption model (EMRAM) Stage 7 hospital in Beijing: cross-sectional Study. JMIR Med Inform. 2021;9(8): e24405.
van Poelgeest R, Heida JP, Pettit L, de Leeuw RJ, Schrijvers G. The association between eHealth Capabilities and the Quality and Safety of Health Care in the Netherlands: comparison of HIMSS analytics EMRAM data with Elsevier’s “The Best Hospitals” data. J Med Syst. 2015;39(9):90.
Kharrazi H, Gonzalez CP, Lowe KB, Huerta TR, Ford EW. Forecasting the maturation of electronic health record functions among US hospitals: retrospective analysis and predictive model. J Med Internet Res. 2018;20(8): e10458.
Dan W, Ying X, Xu-hui Z, Feng Z, Hao C, Zhi-ping L. The construction of pediatric prescription knowledge database facilitates prescription pre-audit intelligent decision. Chin Pharm J. 2020;55(12):1046–50.
Jinyang X, Zhirong W, Changshou M, inventors; Automatic extraction method of drug name card based on NLP. patent CN112926331A. 2021-03-26.
Rishoej RM, Almarsdóttir AB, Christesen HT, Hallas J, Kjeldsen LJ. Medication errors in pediatric inpatients: a study based on a national mandatory reporting system. Eur J Pediatr. 2017;176(12):1697–705.
Eslami K, Aletayeb F, Aletayeb SMH, Kouti L, Hardani AK. Identifying medication errors in neonatal intensive care units: a two-center study. BMC Pediatr. 2019;19(1):365.
Al-Jeraisy MI, Alanazi MQ, Abolfotouh MA. Medication prescribing errors in a pediatric inpatient tertiary care setting in Saudi Arabia. BMC Res Notes. 2011;4:294.
Todd SE, Thompson AJ, Russell WS. Retrospective review for medication dose errors in pediatric emergency department medication orders that bypassed pharmacist review. Pediatr Emerg Care. 2021;37(12):e1308–10.
Zirpe KG, Seta B, Gholap S, Aurangabadi K, Gurav SK, Deshmukh AM, et al. Incidence of medication error in critical care unit of a tertiary care hospital: where do we stand? Indian J Crit Care Med. 2020;24(9):799–803.
Alghamdi AA, Keers RN, Sutherland A, Ashcroft DM. Prevalence and nature of medication errors and preventable adverse drug events in paediatric and neonatal intensive care settings: a systematic review. Drug Saf. 2019;42(12):1423–36.
Conn RL, Tully MP, Shields MD, Carrington A, Dornan T. Characteristics of reported pediatric medication errors in northern ireland and use in quality improvement. Paediatr Drugs. 2020;22(5):551–60.
Brennan-Bourdon LM, Vázquez-Alvarez AO, Gallegos-Llamas J, Koninckx-Cañada M, Marco-Garbayo JL, Huerta-Olvera SG. A study of medication errors during the prescription stage in the pediatric critical care services of a secondary-tertiary level public hospital. BMC Pediatr. 2020;20(1):549.
Campino A, Santesteban E, Pascual P, Sordo B, Arranz C, Unceta M, et al. Strategies implementation to reduce medicine preparation error rate in neonatal intensive care units. Eur J Pediatr. 2016;175(6):755–65.
Zeleke A, Chanie T, Woldie M. Medication prescribing errors and associated factors at the pediatric wards of Dessie Referral Hospital, Northeast Ethiopia. Int Arch Med. 2014;7:18.
Acknowledgements
The authors thank all the clinical pharmacists at the Children’s Hospital of Fudan University for prescription checking.
Author information
Authors and Affiliations
Contributions
GFW designed the study, analyzed the data, drafted the initial manuscript, and revised the manuscript. GYZ, YX, FZ, XHZ and YDH collected the data and searched the literature. XJZ, QFY and XYL revised the manuscript. ZPL and XBZ designed the study and acquired funding. All authors agreed on the journal to which the article was submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Funding
This study was supported by the National Natural Science Foundation of China (No. 81874325), Scientific Research Project of Science and Technology Commission of Shanghai Municipality (No.18DZ1910604).
Conflict of interest
The authors have no other conflicts of interest to declare. No financial or nonfinancial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethics approval
This study protocol follows the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the Ethics Committee of Children’s Hospital of Fudan University. This study was exempted from written form informed consent due to its retrospective nature.
Consent to participate
Not applicable.
Consent for publication
Not applicable
Availability of data and material
All the original data for this study can be accessed by contacting the corresponding author.
Code Availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, G., Zheng, F., Zhang, G. et al. Intercepting Medication Errors in Pediatric In-patients Using a Prescription Pre-audit Intelligent Decision System: A Single-center Study. Pediatr Drugs 24, 555–562 (2022). https://doi.org/10.1007/s40272-022-00521-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-022-00521-2