Abstract
De novo missense mutations in SCN8A gene encoding voltage-gated sodium channel NaV1.6 are linked to a severe form of early infantile epileptic encephalopathy named early infantile epileptic encephalopathy type13 (EIEE13). The majority of the patients with EIEE13 does not respond favorably to the antiepileptic drugs (AEDs) in clinic and has a significantly increased risk of death. Although more than 60 EIEE13-associated mutations have been discovered, only few mutations have been functionally analyzed. In this study we investigated the functional influences of mutations N1466T and N1466K, two EIEE13-associated mutations located in the inactivation gate, on sodium channel properties. Sodium currents were recorded from CHO cells expressing the mutant and wide-type (WT) channels using the whole-cell patch-clamp technique. We found that, in comparison with WT channels, both the mutant channels exhibited increased window currents, persistent currents (INaP) and ramp currents, suggesting that N1466T and N1466K were gain-of-function (GoF) mutations. Sodium channel inhibition is one common mechanism of currently available AEDs, in which topiramate (TPM) was effective in controlling seizures of patients carrying either of the two mutations. We found that TPM (100 µM) preferentially inhibited INaP and ramp currents but did not affect transient currents (INaT) mediated by N1466T or N1466K. Among the other 6 sodium channel-inhibiting AEDs tested, phenytoin and carbamazepine displayed greater efficacy than TPM in suppressing both INaP and ramp currents. Functional characterization of mutants N1466T and N1466K is beneficial for understanding the pathogenesis of EIEE13. The divergent effects of sodium channel-inhibiting AEDs on INaP and ramp currents provide insight into the development of therapeutic strategies for the N1466T and N1466K-associated EIEE13.
Similar content being viewed by others
Introduction
Voltage-gated sodium channels (NaV) are widely expressed in the central and peripheral nervous systems that play critical roles in modulating neuronal excitability [1]. Pathogenic genetic variations in NaV channels induce irregular neuronal activity and are associated with several epileptic syndromes [2,3,4]. The sodium channel NaV1.6, encoded by the gene SCN8A, is one of the major voltage-gated channels in human brain neurons and is highly concentrated at the distal axon initial segment (AIS) and Ranvier nodules. The unique localization of NaV1.6 is essential for the efficient initiation and propagation of action potential firing [5,6,7]. De novo mutations in SCN8A are associated with early infantile epileptic encephalopathy type 13 (EIEE13) which may make up to 1% of all epileptic encephalopathies [8]. Children with EIEE13 have early seizure onset with a median age of 4 months, and nearly 10% of patients may die from sudden unexpected death in epilepsy (SUDEP) [9,10,11].
To date, more than 60 mutations have been identified in patients with EIEE13, and most of them are gain-of-function (GoF) mutations [12]. The observed GoF for these mutations usually includes premature opening or impaired inactivation [10, 11, 13,14,15]. A shift of channel activation towards hyperpolarizing direction may promote channel opening, while a shift of channel inactivation towards depolarizing direction may delay channel closing, both resulting in increased Na+ influx and enhanced neuronal firing [15,16,17,18]. As window currents mean the small range of voltage where NaV channels can open but not inactivate completely, thus a shift of the channel activation and/or inactivation generally leads to a change in the window currents. Notably, persistent currents (INaP) and ramp currents, which reflect incomplete inactivation and slow closed-state inactivation, respectively, are also linked to impaired inactivation. INaP is defined as a non-inactivating current after a long-lasting stimulus and is associated with action potential bursting, which has great significance to the normal repertoire of neuronal excitability [19,20,21]. Abundant evidence exists to prove that an abnormally large INaP may enhance neuronal hyperexcitability and is linked to epilepsy [10, 15, 16, 22,23,24,25]. As ramp current is a response to slow and subthreshold depolarizing inputs, an increase in the ramp current of the NaV1.6 channel will facilitate the susceptibility to excitatory stimulus and thereby enhance neuronal excitability also [8, 22]. Together, alterations in both channel activation and inactivation could be involved in the pathogenesis of SCN8A epileptic encephalopathy [17, 24].
Due to the key roles of impaired channel kinetics in the pathogenesis of EIEE13, targeting the aberrant channel activity of SCN8A GoF mutations was supposed to be beneficial to the therapy of patients with SCN8A encephalopathy. Recurrent mutations N1768D and R1872W located at the C-terminus of the NaV1.6 channel significantly increased INaP and resulted in spontaneous early-onset seizures and death in knock-in mice [10, 23, 26]. GS967 is a novel sodium channel modulator specifically developed to inhibit INaP with a 42-fold preference for the current as opposed to peak current inhibition. Treatment of SCN8AN1768D/+ and SCN8AR1872W/+ mice with GS967 substantially suppressed the convulsant ratio in vivo and prolonged the survival ratio [26, 27]. Nevertheless, the response of EIEE13 mutations located in other domains to AEDs remains unclear. The residue N1466 at the inactivation gate is a recurrent mutation point [8, 12, 28]. Two de novo mutations (N1466T and N1466K) occurred at the same residue were identified in patients with EIEE13 [28]. The clinical study showed that patients with the N1466T/K mutations have different onset times and clinical features. Tonic-clonic attacks start at 3 days for N1466K whereas partial seizures occur at 4 months for N1466T [28]. A previous study reported that the patient with N1466T variant was sensitive to topiramate (TPM) and carbamazepine (CBZ), while the patient with N1466K was temporarily controlled with phenytoin (PHT) combined gabapentin (GBP), adrenocorticotrophic hormone (ACTH), TPM, midazolam (MDL), and lidocaine (LD) [28]. Among these relatively sensitive AEDs, some of them are common sodium channel-inhibiting AEDs, such as TPM, CBZ and LD. In the current study, the functional influences of mutations N1466T and N1466K on channel activity were examined and the sensitivity of the two mutant channels to multiple sodium channel-inhibiting AEDs was evaluated.
Materials and methods
Plasmid constructions
The cDNA constructs for wild-type (WT) human NaV1.6 channels (NP_055006.1) were synthesized by Beijing Genomics Institute and were subcloned into pcDNA5/FRT/TO vector. Mutations N1466T and N1466K were introduced into the WT cDNA construct using the QuikChange II XL site-directed mutagenesis kit from Agilent Technologies, according to the manufacturer’s manual [11]. The mutant channel was verified by fully sequencing before use.
Cell culture and transfection
Chinese hamster ovary (CHO) cells were cultured in Dulbecco’s modified Eagle’s medium/F12 (Gibco, Grand Island, USA) supplemented with 10% fetal bovine serum (Gibco) and grown under standard culture conditions. To express WT or mutant channels, the cells were transiently transfected using Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA). Briefly, a mixture of 3.6 μg WT or mutant channel plasmids and 0.4 μg enhanced green fluorescent protein plasmids were transfected into cells for 4–6 h according to the manufacturer’s instructions. The cells with green fluorescence were chosen for the electrophysiological recordings 36–72 h after transfection.
Drugs and solutions
TPM, lacosamide (LCM), valproic acid (VPA), lamotrigine (LTG), PHT, CBZ and oxcarbazepine (OXC) were purchased from Med Chem Express (NJ, USA). Drugs were dissolved in dimethyl sulfoxide (DMSO) and stored at −20 °C, except for VPA which was dissolved in extracellular patch-clamp solution due to its high hydrophilicity. The final concentration of DMSO was less than 1%, at which it did not affect sodium currents. All other chemicals were obtained from Sigma-Aldrich (St. Louis, MO, USA).
Electrophysiology
Whole-cell patch-clamp recordings were performed at room temperature (22–25 °C) using an Axopatch 200B amplifier (Axon Instruments, Burlingame, CA, USA) and a Digitata 1440 A digitizer software (Axon Instruments, Burlingame, CA, USA). Pipettes were pulled from borosilicate glass capillaries (World Precision Instruments, Sarasota, FL, USA) with an electrode resistance ranging from 1.0 to 3.0 MΩ by a P-1000 Micropipette puller (Sutter Instrument, Novato, CA, USA). The extracellular solution contained (in mmol/L): 140 NaCl, 3 KCl, 1 CaCl2, 1 MgCl2•6H2O, 20 glucose and 10 HEPES, pH 7.30. The pipette solution contained (in mmol/L): 140 CsF, 10 NaCl, 1.1 EGTA, 20 glucose and 10 HEPES, pH 7.30. All recordings were performed at a holding potential of −120 mV and the series resistance was compensated by 80%. Currents were acquired at a 50 kHz sampling frequency and filtered at 2 kHz. To measure the current-voltage relationship, cells were depolarized ranging from -80 mV to +15 mV in 5 mV increments for 50 ms with a stimulus frequency of 0.5 Hz. The mean current amplitude at the last 1 ms during the depolarizing steps was normalized to maximal INaT to calculate INaP. To evaluate the steady-state fast inactivation, cells were depolarized from −130 mV to +20 mV in 10 mV increments for 500 ms, followed by a pulse at 0 mV for 20 ms to measure the number of available channels. To examine the steady-state slow inactivation, cells were stepped to inactivating potentials ranging from −140 mV to +20 mV in 10 mV increments for 10 s, followed by a 20 ms pulse hyperpolarization pulse to −120 mV before 0 mV for 10 ms to test channel availability. To assess the recovery from inactivation, cells were activated by a 20 ms depolarization prepulse at 0 mV and then hyperpolarized to −80 mV with variable durations (0 ms to 30 ms). To test the ramp current, cells were depolarized from −100 mV to +40 mV in 3 s (46 mV/s) to evoke inward current. INaP and ramp currents were normalized to the maximal INaT recorded under activation protocol.
Statistical analysis
Patch clamp data were processed using Clampfit 10.3 (Molecular Device, Sunnyvale, CA, USA) and analyzed with GraphPad Prism 7.0 (GraphPad Software, San Diego, CA, USA). Sodium conductance was used to determine the current-voltage relationship: G(Na)= I(Na) / (V − VRev). The activation curves were fitted to the Boltzmann function: G = I / (1 + exp [(V −V1/2) / k]). The inactivation curves were fitted to the Boltzmann function: I / Imax = 1/ (1 + exp [(V50, inact − V) / kinact]). The data are presented as mean ± SEM. The significance was evaluated using one-way analysis of variance (ANOVA). When necessary, unpaired Student’s t-test was applied. A P value < 0.05 was considered statistically significant. Detailed information about the number of analyzed cells and P values are provided in the results section.
Results
Impaired inactivation of N1466T and N1466K mutants
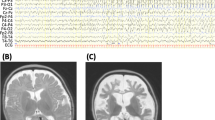
Asparagine residue 1466 (N1466) located at the inactivation gate is evolutionarily conserved among species and across human NaV isoforms (Fig. 1a, b). The mutations from asparagine to threonine (T) and lysine (K) at this point were identified in EIEE13 patients. To probe the influences of the two mutations on channel functions, we first examined the INaT obtained from WT, N1466T and N1466K mutant channels expressed in CHO cells using the whole-cell patch-clamp technique. The peak density of INaT failed to show statistically significant differences among WT and two mutants (Fig. 1d, Table 1, one-way ANOVA with Tukey’s multiple comparisons test, P = 0.93, P = 0.95 and P > 0.99 for WT-N1466T, WT-N1466K, N1466T-N1466K, respectively). INaP is a non-inactivating current generated by a fraction of sodium channels that are resistant to inactivation during a prolonged depolarization. Unlike the negligible currents observed in WT channels, the INaP recorded from N1466T and N1466K mutant channels remarkably increased and displayed a voltage-dependent feature (Fig. 1c). The enlargement of INaP was probably ascribed to the damaged channel inactivation [11]. Indeed, as illustrated in Fig. 1e, steady-state fast inactivation of the two mutant channels shifted toward the depolarized direction, while steady-state activation remained unchanged. Consistently, larger window currents of N1466T and N1466K mutant channels appeared also, which were different from WT channels (Fig. 1f). Intriguingly, steady-state slow inactivation of the N1466T and N1466K mutant channels shifted toward hyperpolarized direction (Fig. 1g).
a Topologic representation of NaV1.6 α subunit, showing the four domains, the six transmembrane segments and the linkers. The blue dot indicates the location of the investigated variants. b Sequence alignment within the inactivation gate of the indicated NaV channels. Asparagine 1466 (N1466) is evolutionarily conserved among species and across NaV isoforms. c Representative traces of transient currents recorded in CHO cells transfected with NaV1.6 WT, N1466T and N1466K mutant channels. d Averaged current-voltage relationship for cells expressing the WT and mutant channels. e Voltage dependence of activation and steady-state fast inactivation for cells transfected with WT (black), N1466T (blue) and N1466K (red) channels. The curves were fitted with Boltzmann equation. f An enlargement of window current by overlapping the Boltzmann fitted curves. g Voltage dependence of steady-state slow inactivation. The curves were fitted with Boltzmann equation. Data are presented as mean ± SEM; data were analyzed by one-way ANOVA. Detailed information about the values and the statistical significance are presented in Table 1.
To better understand the impacts of the damaged inactivation on channel kinetics, the decay of the elicited currents was fitted to a single exponential function. Compared to WT channels, mutant N1466K prominently increased the time constant of fast inactivation (Fig. 2a), which would finally slow the transition from the open state back to the closed state. For the steady-state slow inactivation, mutant N1466K exhibited a larger time constant than that of WT channels also (P = 0.004) (Fig. 2b). In comparison with that of WT channels, recovery from fast inactivation of N1466T and N1466K mutant channels was much faster (Fig. 2c). Additionally, Western blot assays revealed that CHO cells transfected with WT, N1466T or N1466K plasmids exhibited a similar band with the expected molecular weight (220 kDa) (Supplementary Fig. S1a). No significant difference in protein expression levels among the WT and mutant channels was observed (Supplementary Fig. S1b). Together, our data showed that N1466T and N1466K are GoF mutations with impaired channel inactivation.
a Representative traces showing the fast inactivation recorded from cells transfected WT, N1466T, and N1466K channels. Averaged time constants were obtained by fitting the fast inactivation to a single exponential equation. b Representative traces showing steady-state slow inactivation recorded from cells transfected WT, N1466T, and N1466K channels. Averaged time constants were obtained by fitting steady-state slow inactivation to a single exponential equation. c Recovery from the fast inactivation with recovery durations from 0 to 30 ms. Data are presented as mean ± SEM; data were analyzed by one-way ANOVA. The values and the statistical significance are presented in Table 1.
Increased persistent and ramp currents of N1466T and N1466K mutants
Impaired channel inactivation was generally accompanied by abnormally large INaP and ramp currents. The impacts of N1466T and N1466K on INaP and ramp currents were then investigated individually. Compared to WT channels, INaP recorded from N1466T and N1466K mutant channels remarkably increased, and the current amplitudes of the INaP obtained from the N1466K were much larger than that from the N1466T (P < 0.001 for N1466T-N1466K, Fig. 3a and Table 1). To visualize the ramp current, we applied slow depolarizations from −100 mV to +40 mV at a rate of 46 mV/s which allowed the full inactivation of the fast-decaying sodium current component. The N1466T and N1466K mutant channels generated typical ramp currents, which were significantly larger than that of WT channels (Fig. 3b, one-way ANOVA with Games-Howell’s multiple comparisons test, P < 0.001, P < 0.001 and P = 0.002 for WT-N1466T, WT-N1466K and N1466T-N1466K, respectively). To test whether the obtained INaP and ramp currents were mediated by the mutant channels, GS967, a selective INaP inhibitor, was used. As the IC50 value of GS967 on the INaT of WT channels was 86.69 ± 0.04 nM (n = 4), a fixed concentration of 100 nM was used in the following experiments (Supplementary Fig. S2a, b). The inhibitory efficacy of 100 nM GS967 on the INaT of WT channels was similar to those of the N1466T and N1466K mutant channels (unpaired t-test, P > 0.99 and P > 0.99 for WT-N1466T, WT-N1466K) (Supplementary Fig. S2c, d). As a potent INaP inhibitor, the INaP of the two mutant channels was reduced after the application of 100 nM GS967. The percentage of INaP was reduced from 3.56% ± 0.24% to 1.02% ± 0.11% (n = 10, P < 0.001) by 100 nM GS967 for the N1466T, and was decreased from 8.36% ± 0.67% to 2.52% ± 0.21% for the N1466K (n = 10, P < 0.001) (Fig. 3c, d). Expectedly, the ramp currents were also significantly suppressed by GS967, which were similar to its effects on the INaP of N1466T and N1466K mutant channels. The ramp currents were reduced from 3.73% ± 0.36% to 1.11% ± 0.08% for N1466T (n = 10, P < 0.001), and from 7.36% ± 0.74% to 2.42% ± 0.35% for N1466K (n = 10, P < 0.001), respectively (Fig. 3e, f). These data showed that mutations N1466T and N1466K increased INaP and ramp currents.
a Representative activation current traces showing INaP from WT (black), N1466T (blue) and N1466K (red) channels. Currents were elicited at 0 mV and normalized to the maximal transient currents during the 50 ms stimulus. This curve was measured during the last 1 ms of the 50 ms activation protocol. b Representative traces showing ramp currents recorded from cells transfected WT, N1466T, and N1466K channels. Currents were elicited by a slow ramp from −100 mV to −40 mV in 3 s and normalized to the maximum of transient peak currents (INaT) as an inward current. c, d Traces and graphs showing the INaP before and after the treatment of 100 nM GS967 for cells expressing N1466T and N1466K mutant channels. e, f Traces and graphs showing ramp currents before and after the treatment of 100 nM GS967 for cells transfected with N1466T and N1466K channels. Data are presented as mean ± SEM and analyzed by one-way ANOVA or two-tailed paired Student’s t-test (***P < 0.001).
TPM inhibited persistent and ramp currents generated by N1466T and N1466K mutant channels
Suppression of INaT, INaP or ramp currents has been proposed to be a feasible way of developing AEDs targeted on NaV channels [29]. Thus, we set out to explore which factor facilitates block by NaV1.6 channel inhibitors. TPM was reported to be effective in the relief of epileptic attacks in the patient carrying N1466T or N1466K mutations. The effects of TPM on INaT, INaP and ramp currents of the mutant channels were examined. A fixed 100 μM TPM was applied, which has been widely used in the mechanism studies of TPM [30]. We firstly examined the effects of 100 μM TPM on INaT generated by WT, N1466T and N1466K channels. The inhibitory efficacies of 100 μM TPM on the INaT of N1466T (11.56% ± 1.82%, n = 10, P = 0.69) and N1466K (9.78% ± 1.52%, n = 10, P = 0.29 via unpaired t-test) channels were similar to that of the WT channel (13.00% ± 0.71%, n = 3) (Fig. 4a). Unlike WT channels, both of the two mutant channels generate INaP and we found that TPM dramatically reduced the INaP mediated by the two mutant channels. The percentage of INaP was reduced from 4.84% ± 0.47% to 3.45% ± 0.40% (P < 0.001, n = 10) for N1466T, and was decreased from 10.53% ± 1.58% to 6.94% ± 1.12% (P < 0.001, n = 9) for N1466K (Fig. 4c, d). In addition, the ramp currents were remarkably suppressed by TPM for both N1466T (from 5.29% ± 0.62% to 3.66% ± 0.41%, P < 0.001, n = 10) and N1466K (from 9.30% ± 0.73% to 4.76% ± 0.57%, P < 0.001, n = 9) mutant channels (Fig. 4e, f). Notably, the block of the INaP by TPM for N1466K channel (34.30% ± 1.87%, n = 9) was much stronger than that for N1466T channel ( 29.25% ± 3.5%, n = 10) (P = 0.004 via unpaired t-test) (Figs. 5b and 6b). These results revealed that TPM suppressed both INaP and ramp currents mediated by N1466T and N1466K mutant channels.
a Representative current traces showing the effects of 100 μM TPM (black) on INaT of WT, N1466T, and N1466K channels. Currents were recorded by a depolarizing step to −40 mV for 300 ms from a holding potential of −70 mV. b Plot showing the remaining current amplitudes after the treatment of 100 μM TPM. c, d Traces and graphs showing INaP before and after treating 100 μM TPM for N1466T and N1466K mutants. e, f Representative traces showing ramp currents before and after treating 100 μM TPM in N1466T and N1466K mutants. Data are presented as mean ± SEM, *P < 0.05, **P < 0.01 and ***P < 0.001 (Control vs. drug via two-tailed paired Student’s t-test).
a Representative traces showing the INaP of N1466T channel before and after application of 100 μM LCM, VPA, LTG, PHT, CBZ, and OXC. b Bar graph showing the inhibition ratios of INaP following treatment with AEDs in N1466T mutant. c Representative traces showing the ramp currents of N1466T channel before and after the treatment of 100 μM AEDs. d Bar graph showing the inhibition ratios of the ramp currents of N1466T mutant by AEDs. Data are presented as mean ± SEM; **P < 0.01 and ***P < 0.001 (TPM vs. drug via one-way ANOVA).
a Representative traces showing the INaP of N1466K channel before and after treatment with 100 μM LCM, VPA, LTG, PHT, CBZ, and OXC. b Bar graph showing the inhibition ratios of INaP following the treatment of AEDs in N1466K mutant. c Representative traces and graphs showing the ramp currents of N1466K channel before and after the treatment of 100 μM AEDs. d Bar graph showing the inhibition ratios of the ramp currents of N1466K mutant by AEDs. Data are presented as mean ± SEM; *P < 0.05, **P < 0.01 and ***P < 0.001 (TPM vs. drug via one-way ANOVA).
Sensitivity of N1466T and N1466K mutant channels to other sodium channel-inhibiting AEDs
As inhibition of INaP and ramp currents was observed by TPM, an effective antiepileptic drug for patients carrying N1466T or N1466K mutations in clinic, we asked whether the sodium channel-inhibiting AEDs affect the two mutant channels similarly. Total 6 AEDs (LCM, VPA, LTG, PHT, CBZ, OXC) were evaluated [3, 23]. Considering the inhibitory efficacy and solubility of these AEDs, we examined their effects on mutant channels at a fixed concentration of 100 µM [14, 30,31,32]. As shown in Supplementary Fig S3a and b, 100 μM LTG (30.53% ± 2.61%, n = 7, P < 0.001) and PHT (56.03% ± 4.42%, n = 7, P < 0.001) showed greater inhibition efficacy against the INaT of N1466T mutant channel than that of TPM (11.56% ± 1.83%, n = 10). The inhibition efficacy of the INaP of N1466T channel by the 6 selected AEDs was different (Fig. 5a, b). Compared to TPM (29.25% ± 3.50%, n = 10), four AEDs showed strong inhibition effects on the INaP, which were LTG (56.84% ± 1.34%, n = 7, P < 0.001), PHT (67.09% ± 2.36%, n = 7, P < 0.001), CBZ (69.42% ± 2.76%, n = 8, P < 0.001) and OXC (54.16% ± 4.49%, n = 8, P = 0.003). The inhibitory efficacies of LCM (36.53% ± 3.96%, n = 6, P = 0.60) and VPA (28.99% ± 3.95%, n = 9, P > 0.99) on the INaP were similar to that of TPM (29.25% ± 3.50%, n = 10). Moreover, we assessed the influences of the AEDs on the ramp currents of N1466T mutant channels. As shown in Fig. 5c and d, the inhibitory efficacies of the ramp currents by 100 µM AEDs are as follows: 31.21% ± 6.95% for LCM (n = 6, P > 0.99 vs. TPM (29.83% ± 4.52%, n = 10) via one-way ANOVA with Dunnett’s Multiple Comparison Test), 23.44% ± 4.72% for VPA (n = 9, P = 0.85), 62.73% ± 2.67% for LTG (n = 7, P < 0.001), 66.19% ± 3.95% for PHT (n = 7, P < 0.001), 60.72% ± 4.60% for CBZ (n = 8, P = 0.001), 61.97% ± 3.58% for OXC (n = 8, P < 0.001).
Similarly, the effects of these AEDs on N1466K mutant channel were also examined. As shown in Fig. S3c and d, LTG, PHT and OXC shows greater inhibition efficacy against the INaT of N1466K mutant channel than other selected AEDs and TPM (38.96% ± 2.02% for LTG, n = 7, P < 0.001 vs TPM (9.23% ± 1.48%, n = 11); 61.15% ± 5.91% for PHT, n = 5, P < 0.001; 27.17% ± 2.10% for OXC, n = 7, P < 0.001). Dramatic reductions in INaP of N1466K mutant channel in the presence of 100 µM OXC, PHT, CBZ and LTG were observed (Fig. 6a). The inhibitory efficacies of the INaP by 100 µM AEDs are as follows: 20.89% ± 3.32% for LCM (n = 8, P = 0.02), 24.01% ± 6.53% for VPA (n = 7, P = 0.53), 58.71% ± 2.33% for LTG (n = 7, P < 0.001), 66.36% ± 4.96% for PHT (n = 7, P = 0.002), 76.99% ± 1.33% for CBZ (n = 7, P < 0.001), 54.71% ± 2.07% for OXC (n = 7, P < 0.001). The inhibitory efficacies of the ramp currents by 100 µM AEDs are as follows: 28.00% ± 2.14% for LCM (n = 7, P < 0.001), 2.66% ± 0.89% for VPA (n = 7, P < 0.001), 56.19% ± 2.59% for LTG (n = 7, P = 0.42), 64.20% ± 2.98% for PHT (n = 7, P = 0.02), 72.82% ± 2.96% for CBZ (n = 7, P < 0.001), 52.86% ± 6.80% for OXC (n = 7, P > 0.99) (Fig. 6b). Finally, 100 µM PHT and CBZ prominently suppressed the ramp currents of N1466K compared to TPM, which was not observed with OXC and LTG. Collectively, among the tested 6 AEDs, only PHT and CBZ exhibited greater inhibitory effects on the epilepsy-associated INaP and ramp currents mediated N1466T and N1466K mutant channels compared to TPM.
Discussion
Although over 60 NaV1.6 mutations have been linked to EIEE13, only few mutations have ever been functionally characterized [12]. One-third of the mutations are recurrent mutations that occurred in two or more unrelated individuals [8]. The intracellular loop connecting domains III and IV forms the fast inactivation gate, which binds to the intracellular side and then occludes the pore during channel inactivation [33]. Residue N1466 is a recurrent spot located at the inactivation gate of the NaV1.6 channel. In the current study, we first characterized the biophysical properties of N1466T and N1466K mutant channels. Compared to WT channels, no significant change in the INaT amplitudes of the mutants was detected after the constructs were transiently expressed in the CHO cells (Fig. 1c, d, Table 1). However, the mutations N1466T and N14466K prominently increased INaP and ramp currents but had little effect on voltage-dependent activation (Figs. 1c and 3). These results were similar to other GoF variations in SCN8A such as the N1768D, which displayed a right-shifted steady-state fast inactivation and remarkably increased ramp and persistent currents [10, 23]. Unexpectedly, the slow inactivation of N1466T and N1466K largely shifted toward the hyperpolarization direction (Fig. 1g). These effects were similar to R853Q of SCN2A, which enhanced the entry of NaV1.2 channel into slow inactivation state and led to a marked reduction in action potential firing [2]. Aside from these properties, the time constants for the onset of and recovery from inactivation were also modified by mutations N1466T and N1466K. The development of both fast and slow inactivation of N1466K was significantly slower than that of WT channels (Fig. 2a, b). The recovery from the inactivated state of the N1466T and N1466K mutant channels was faster compared to the WT channels (Fig. 2c). Notably, the changes in the channel kinetics of N1466T and N1466K were different from previously reported mutations including those located at the inactivation gate, in which modifications on INaP and ramp currents were simultaneously identified [23, 34,35,36]. These findings increased the diversity of the mutations in SCN8A. The biophysical effects of mutations N1466T and N1466K were largely congruent with GoF mutations.
Disruption of the size, net charge or hydrophobicity of the residues at the inactivation gate commonly affected the inactivation kinetics of NaV channels [37, 38]. For example, charge reversing mutation D1309R in the inactivation gate of hNaV1.4 channel significantly changes the channel inactivation kinetics including shifting the steady-state fast inactivation to the depolarized direction and slowing the recovery from fast inactivation [39]. The effect of D1309R on the steady-state fast inactivation was similar to the charge substituting mutation D1309E [39]. In addition, fast inactivation of charge neutralizing mutations EE1314,1315KK and KK1317,1318QQ in the inactivation gate of the hNaV1.4 channel was shifted towards hyperpolarized potentials, whereas the activation potential remained unchanged [40]. In hNaV1.6 channels, de novo mutations G1475R and A1491V which change the size and/or net charge of the residues located at the inactivation gate prominently impaired the channel inactivation properties including a dramatic increase in the persistent currents and ramp currents [23]. Mutations N1466T/K which respectively change the size and net charge might affect the inactivation process similar to these previously reported mutants. However, the exact mechanism of the development of fast inactivation is unclear, scientific studies on voltage-sensing and electromechanical coupling are needed to clarify the allosteric process.
Channel dysfunction generally appears to correlate with clinical severity. An increase in INaP facilitates channel reopening and thereby facilitates repetitive neuronal firing [4]. Studies on the recurrent epilepsy-related NaV1.6 mutations like R1872L/W/Q suggested that dysfunction in INaP plays a much more important role in pathogenic mechanisms than other parameters do [15, 24, 41]. As a low threshold channel, the ramp current elicited in NaV1.6 is a response to slow and subthreshold depolarizing inputs [42,43,44]. Enhanced ramp currents of the N1768D and other GoF mutations resulted in neuronal hyperexcitability, including increased spontaneous firing frequency and PDS-like complexes [10, 16, 22, 23]. Compared to N1466T, the increase of INaP and ramp currents in N1466K was much larger (Fig. 3). Consistently, the onset time of epileptic attacks for the patient carrying N1466K was earlier than that for patients carrying N1466T mutation. The onset time was at the age of 3 days for N1466K, whereas the first attack occurred at four months for N1466T. Thus, aberrant channel properties associated with N1466T and N1466K gene mutations might be correlated with disease phenotype.
Patients carrying N1466T or N1466K were sensitive to TPM therapy in clinic. In the present study, we revealed that TPM normalized epilepsy-associated pathological INaP and ramp currents of the N1466T/K mutants (Fig. 4). Our findings indicated that suppression of the INaP and ramp currents may be more effective for SCN8A encephalopathy than the other biophysical properties of N1466T/K mutants. Consistently, inhibition of endogenous INaP of striatal neurons was suggested to be implicated in the antiepileptic activity of FDA-approved cannabidiol [45]. The application of GS967, a potent INaP inhibitor, provided dose-dependent protection against the maximal electroshock-induced seizures in mice carrying N1768D mutation [27, 46]. Together, our study supported that inhibition of NaV1.6 channel INaP and ramp currents may be a feasible strategy to develop antiepileptic drugs.
Providing the finding that inhibition of INaP and ramp current may contribute to the treatment of NaV1.6-associated epilepsy by TPM, we tested other classical AEDs targeting NaV channels [25]. Intriguingly, the INaP and ramp currents of N1466T and N1466K mutants displayed a divergent sensitivity to these AEDs. For the N1466T mutant channel, LTG, PHT, OXC, and CBZ exhibited a more substantial suppression effect on both INaP and ramp currents compared to TPM (Fig. 5b, d). The effects of LCM and VPA on the mutant channel were similar to that of TPM (Fig. 5b, d). For the N1466K mutant channel, enhanced inhibition of the INaP and ramp currents by PHT and CBZ was observed, while the sensitivity of ramp currents of N1466K to VPA was diminished compared to TPM (Fig. 6). Our results showed that N1466T and N1466K are more sensitive to PHT and CBZ. Consistent with previous studies, high-dose PHT displayed remarkable sensitivity in patients with a missense SCN8A mutation and epilepsy [14, 47]. Our findings provided additional evidence that PHT and CBZ may have the potential for the treatment of patients with SCN8A-related epilepsy.
In conclusion, our study showed that N1466T and N1466K are GoF mutations with altered features predicted to increase neuronal excitability and seizure susceptibility. The effectiveness of TPM inhibiting the mutant channels provided additional evidence that suppression of INaP and ramp currents may benefit the treatment for SCN8A encephalopathy. Among the available AEDs targeting NaV channels, PHT and CBZ may act as alternative therapies for epilepsy patients, particularly for those carrying N1466T and N1466K mutations. Additionally, inhibition of INaP and ramp currents might be a promising strategy to develop AEDs targeting NaV1.6 channel.
References
O’Brien JE, Meisler MH. Sodium channel SCN8A (Nav1.6): properties and de novo mutations in epileptic encephalopathy and intellectual disability. Front Genet. 2013;4:213.
Berecki G, Howell KB, Deerasooriya YH, Cilio MR, Oliva MK, Kaplan D, et al. Dynamic action potential clamp predicts functional separation in mild familial and severe de novo forms of SCN2A epilepsy. Proc Natl Acad Sci USA. 2018;115:E5516–25.
Zaman T, Helbig I, Bozovic IB, DeBrosse SD, Bergqvist AC, Wallis K, et al. Mutations in SCN3A cause early infantile epileptic encephalopathy. Ann Neurol. 2018;83:703–17.
Meisler MH, Kearney JA. Sodium channel mutations in epilepsy and other neurological disorders. J Clin Invest. 2005;115:2010–7.
Royeck M, Horstmann MT, Remy S, Reitze M, Yaari Y, Beck H. Role of axonal NaV1.6 sodium channels in action potential initiation of CA1 pyramidal neurons. J Neurophysiol. 2008;100:2361–80.
Gasser A, Ho TS, Cheng X, Chang KJ, Waxman SG, Rasband MN, et al. An ankyrinG-binding motif is necessary and sufficient for targeting Nav1.6 sodium channels to axon initial segments and nodes of Ranvier. J Neurosci. 2012;32:7232–43.
Hu W, Tian C, Li T, Yang M, Hou H, Shu Y. Distinct contributions of Nav1.6 and Nav1.2 in action potential initiation and backpropagation. Nat Neurosci. 2009;12:996–1002.
Wagnon JL, Meisler MH. Recurrent and Non-Recurrent Mutations of SCN8A in Epileptic Encephalopathy. Front Neurol. 2015;6:104.
Kong W, Zhang Y, Gao Y, Liu X, Gao K, Xie H, et al. SCN8A mutations in Chinese children with early onset epilepsy and intellectual disability. Epilepsia. 2015;56:431–8.
Veeramah KR, O’Brien JE, Meisler MH, Cheng X, Dib-Hajj SD, Waxman SG, et al. De novo pathogenic SCN8A mutation identified by whole-genome sequencing of a family quartet affected by infantile epileptic encephalopathy and SUDEP. Am J Hum Genet. 2012;90:502–10.
Blanchard MG, Willemsen MH, Walker JB, Dib-Hajj SD, Waxman SG, Jongmans MC, et al. De novo gain-of-function and loss-of-function mutations of SCN8A in patients with intellectual disabilities and epilepsy. J Med Genet. 2015;52:330–7.
Menezes LFS, Sabia Junior EF, Tibery DV, Carneiro LDA, Schwartz EF. Epilepsy-related voltage-gated sodium channelopathies: a review. Front Pharmacol. 2020;11:1276.
Estacion M, O’Brien JE, Conravey A, Hammer MF, Waxman SG, Dib-Hajj SD, et al. A novel de novo mutation of SCN8A (Nav1.6) with enhanced channel activation in a child with epileptic encephalopathy. Neurobiol Dis. 2014;69:117–23.
Barker BS, Ottolini M, Wagnon JL, Hollander RM, Meisler MH, Patel MK. The SCN8A encephalopathy mutation p.Ile1327Val displays elevated sensitivity to the anticonvulsant phenytoin. Epilepsia. 2016;57:1458–66.
Wagnon JL, Barker BS, Hounshell JA, Haaxma CA, Shealy A, Moss T, et al. Pathogenic mechanism of recurrent mutations of SCN8A in epileptic encephalopathy. Ann Clin Transl Neurol. 2016;3:114–23.
Liu Y, Schubert J, Sonnenberg L, Helbig KL, Hoei-Hansen CE, Koko M, et al. Neuronal mechanisms of mutations in SCN8A causing epilepsy or intellectual disability. Brain. 2019;142:376–90.
Sole L, Wagnon JL, Tamkun MM. Functional analysis of three Nav1.6 mutations causing early infantile epileptic encephalopathy. Biochim Biophys Acta Mol Basis Dis. 2020;1866:165959.
Hargus NJ, Nigam A, Bertram EH 3rd, Patel MK. Evidence for a role of Nav1.6 in facilitating increases in neuronal hyperexcitability during epileptogenesis. J Neurophysiol. 2013;110:1144–57.
Yamada-Hanff J, Bean BP. Persistent sodium current drives conditional pacemaking in CA1 pyramidal neurons under muscarinic stimulation. J Neurosci. 2013;33:15011–21.
Tazerart S, Viemari JC, Darbon P, Vinay L, Brocard F. Contribution of persistent sodium current to locomotor pattern generation in neonatal rats. J Neurophysiol. 2007;98:613–28.
Khaliq ZM, Bean BP. Pacemaking in dopaminergic ventral tegmental area neurons: depolarizing drive from background and voltage-dependent sodium conductances. J Neurosci. 2010;30:7401–13.
Poulin H, Chahine M. R1617Q epilepsy mutation slows NaV1. 6 sodium channel inactivation and increases the persistent current and neuronal firing. J Physiol. 2021;599:1651–64.
Zaman T, Abou Tayoun A, Goldberg EM. A single-center SCN8A-related epilepsy cohort: clinical, genetic, and physiologic characterization. Ann Clin Transl Neurol. 2019;6:1445–55.
Pan Y, Cummins TR. Distinct functional alterations in SCN8A epilepsy mutant channels. J Physiol. 2020;598:381–401.
Wengert ER, Patel MK. The role of the persistent sodium current in epilepsy. Epilepsy Curr. 2021;21:40–7.
Bunton-Stasyshyn RKA, Wagnon JL, Wengert ER, Barker BS, Faulkner A, Wagley PK, et al. Prominent role of forebrain excitatory neurons in SCN8A encephalopathy. Brain. 2019;142:362–75.
Wengert ER, Saga AU, Panchal PS, Barker BS, Patel MK. Prax330 reduces persistent and resurgent sodium channel currents and neuronal hyperexcitability of subiculum neurons in a mouse model of SCN8A epileptic encephalopathy. Neuropharmacology. 2019;158:107699.
Ohba C, Kato M, Takahashi S, Lerman-Sagie T, Lev D, Terashima H, et al. Early onset epileptic encephalopathy caused by de novo SCN8A mutations. Epilepsia. 2014;55:994–1000.
Eijkelkamp N, Linley JE, Baker MD, Minett MS, Cregg R, Werdehausen R, et al. Neurological perspectives on voltage-gated sodium channels. Brain. 2012;135:2585–612.
Sun GC, Werkman TR, Battefeld A, Clare JJ, Wadman WJ. Carbamazepine and topiramate modulation of transient and persistent sodium currents studied in HEK293 cells expressing the Nav1.3 α-subunit. Epilepsia. 2007;48:774–82.
Colombo E, Franceschetti S, Avanzini G, Mantegazza M. Phenytoin inhibits the persistent sodium current in neocortical neurons by modifying its inactivation properties. PLoS One. 2013;8:e55329.
Nakatani Y, Masuko H, Amano T. Effect of lamotrigine on Nav1.4 voltage-gated sodium channels. J Pharmacol Sci. 2013;123:203–6.
West JW, Patton DE, Scheuer T, Wang Y, Goldin AL, Catterall WA. A cluster of hydrophobic amino acid residues required for fast Na+-channel inactivation. Proc Natl Acad Sci USA. 1992;89:10910–4.
Gardella E, Marini C, Trivisano M, Fitzgerald MP, Alber M, Howell KB, et al. The phenotype of SCN8A developmental and epileptic encephalopathy. Neurology. 2018;91:e1112–e24.
Denis J, Villeneuve N, Cacciagli P, Mignon-Ravix C, Lacoste C, Lefranc J, et al. Clinical study of 19 patients with SCN8A-related epilepsy: Two modes of onset regarding EEG and seizures. Epilepsia. 2019;60:845–56.
Morton L, Seinfeld S, Hussain A. Genetic Association with Ictal Cardiorespiratory Phenomena: SCN8A Case Series. J Pediatr Neurol. 2016;14:151–5.
Patton DE, West JW, Catterall WA, Goldin AL. Amino acid residues required for fast Na (+)-channel inactivation: charge neutralizations and deletions in the III-IV linker. Proc Natl Acad Sci USA. 1992;89:10905–9.
Miller JR, Patel MK, John JE, Mounsey JP, Moorman JR. Contributions of charged residues in a cytoplasmic linking region to Na channel gating. Biochim Biophys Acta Biomembr. 2000;1509:275–91.
Groome JR, Fujimoto E, Ruben PC. Negative charges in the DIII–DIV linker of human skeletal muscle Na+ channels regulate deactivation gating. J Physiol. 2003;548:85–96.
Groome JR, Dice MC, Fujimoto E, Ruben PC. Charge immobilization of skeletal muscle Na+ channels: role of residues in the inactivation linker. Biophys J. 2007;93:1519–33.
Tidball AM, Lopez-Santiago LF, Yuan Y, Glenn TW, Margolis JL, Clayton Walker J, et al. Variant-specific changes in persistent or resurgent sodium current in SCN8A-related epilepsy patient-derived neurons. Brain. 2020;143:3025–40.
Cummins TR, Howe JR, Waxman SG. Slow Closed-State Inactivation: A Novel Mechanism Underlying Ramp Currents in Cells Expressing the hNE/PN1 Sodium Channel. J Neurosci. 1998;18:9607–19.
Estacion M, Waxman SG. The response of NaV1.3 sodium channels to ramp stimuli: multiple components and mechanisms. J Neurophysiol. 2013;109:306–14.
Lampert A, Hains BC, Waxman SG. Upregulation of persistent and ramp sodium current in dorsal horn neurons after spinal cord injury. Exp Brain Res. 2006;174:660–6.
Patel RR, Barbosa C, Brustovetsky T, Brustovetsky N, Cummins TR. Aberrant epilepsy-associated mutant Nav1.6 sodium channel activity can be targeted with cannabidiol. Brain. 2016;139:2164–81.
Baker EM, Thompson CH, Hawkins NA, Wagnon JL, Wengert ER, Patel MK, et al. The novel sodium channel modulator GS-458967 (GS967) is an effective treatment in a mouse model of SCN8A encephalopathy. Epilepsia. 2018;59:1166–76.
Boerma RS, Braun KP, van den Broek MP, van Berkestijn FM, Swinkels ME, Hagebeuk EO, et al. Remarkable phenytoin sensitivity in 4 children with SCN8A-related epilepsy: a molecular neuropharmacological approach. Neurotherapeutics. 2016;13:192–7.
Acknowledgements
This work was supported by the National Science Fund for Distinguished Young Scholars (81825021), the National Natural Science Foundation of China (81773707), the Youth Innovation Promotion Association of the Chinese Academy of Sciences (2020284), and the Fund of Science and Technology Commission of Shanghai Municipality (19431906000).
Author information
Authors and Affiliations
Contributions
ZBG and YMZ conceived and designed the experiments. QBG, LZ and HYX performed the experiments. QBG and YMZ analyzed the data. QBG, YMZ and ZBG wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary information
Rights and permissions
About this article
Cite this article
Guo, Qb., Zhan, L., Xu, Hy. et al. SCN8A epileptic encephalopathy mutations display a gain-of-function phenotype and divergent sensitivity to antiepileptic drugs. Acta Pharmacol Sin 43, 3139–3148 (2022). https://doi.org/10.1038/s41401-022-00955-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-022-00955-x
Keywords
This article is cited by
-
APS celebrates the 90th anniversary of SIMM
Acta Pharmacologica Sinica (2022)