Abstract
Ritonavir-boosted nirmatrelvir (RBN) has been authorized recently in several countries as an orally active anti-SARS-CoV-2 treatment for patients at high risk of progressing to severe COVID-19 disease. Nirmatrelvir is the active component against the SARS-CoV-2 virus, whereas ritonavir, a potent CYP3A inhibitor, is intended to boost the activity of nirmatrelvir by increasing its concentration in plasma to ensure persistence of antiviral concentrations during the 12-hour dosing interval. RBN is involved in many clinically important drug–drug interactions both as perpetrator and as victim, which can complicate its use in patients treated with antiseizure medications (ASMs). Interactions between RBN and ASMs are bidirectional. As perpetrator, RBN may increase the plasma concentration of a number of ASMs that are CYP3A4 substrates, possibly leading to toxicity. As victims, both nirmatrelvir and ritonavir are subject to metabolic induction by concomitant treatment with potent enzyme-inducing ASMs (carbamazepine, phenytoin, phenobarbital and primidone). According to US and European prescribing information, treatment with these ASMs is a contraindication to the use of RBN. Although remdesivir is a valuable alternative to RBN, it may not be readily accessible in some settings due to cost and/or need for intravenous administration. If remdesivir is not an appropriate option, either bebtelovimab or molnupiravir may be considered. However, evidence about the clinical efficacy of bebtelovimab is still limited, and molnupiravir, the only orally active alternative, is deemed to have appreciably lower efficacy than RBN and remdesivir.
Similar content being viewed by others
Ritonavir-boosted nirmatrelvir (RBN), a newly approved medication to prevent progression of COVID-19 to severe disease, can be a victim and perpetrator of many clinically important drug–drug interactions. |
When used in patients with epilepsy on antiseizure medications (ASMs), RBN can inhibit the metabolism of ASMs which are CYP3A4 substrates, resulting potentially in manifestations of ASM toxicity. |
Inhibition of midazolam and everolimus metabolism by RBN is a special concern and their co-administration is best avoided in patients requiring RBN. If intravenous midazolam is required, a reduction in dose requirements should be considered and use should be in a setting where potentially serious adverse effects can be managed adequately. |
RBN is currently contraindicated in patients taking carbamazepine and other potent enzyme-inducing ASMs because the reduction in plasma levels of nirmatrelvir due to enzyme induction can result in loss of antiviral effect and selection of RBN-resistant SARS-CoV-2 strains. |
1 Introduction
On December 22, 2021, the Food and Drug Administration (FDA) issued an Emergency Use Authorization (EUA) for the combination of nirmatrelvir and low-dose ritonavir or ritonavir-boosted nirmatrelvir (RBN, Paxlovid®) for the treatment of patients (≥ 12 years and body weight ≥ 40 kg) with mild-to-moderate COVID-19 who are within 5 days of symptom onset and are at high risk of progression to severe disease [1]. The oral dose for patients with normal renal function is nirmatrelvir 300 mg (2 × 150-mg tablets) plus ritonavir 100 mg (1 × 100-mg tablet), twice daily for 5 days [1]. On January 28, 2022 the European Commission also authorized the marketing of RBN for the treatment of COVID-19 in adults who do not require supplemental oxygen and who are at increased risk of the disease becoming severe [2].
In the RBN combination, the component active against the SARS-Cov-2 virus is nirmatrelvir, which exerts its therapeutic effect by blocking viral replication through inhibition of the SARS-CoV-2 main protease. The role of ritonavir, a potent inhibitor of the CYP3A-mediated metabolism of nirmatrelvir, is solely to boost the activity of nirmatrelvir by increasing its concentration in plasma and ensuring persistence of effective nirmatrelvir concentrations throughout the 12-h dosing interval [2,3,4]. In fact, ritonavir is an inhibitor, inducer and substrate of various cytochrome P450 (CYP) enzymes and other metabolizing enzymes as well as drug transporters [3,4,5], leading to several clinically relevant drug interactions. This raises a number of concerns when RBN is administered concomitantly with antiseizure medications (ASMs) that are susceptible to being victims or perpetrators of metabolic drug–drug interactions.
Interactions between RBN (or its components) and ASMs can occur bi-directionally (Tables 1, 2) [3, 6, 7]. First, ritonavir’s potent inhibition of CYP3A increases the plasma exposure of ASMs primarily cleared through CYP3A-mediated metabolism, potentially leading to toxicity. Second, induction of CYP2C9, CYP2C19 and uridine 5′-diphospho-glucuronosyl-transferases (UGTs) by ritonavir can decrease the plasma exposure of ASMs metabolized by these enzymes, an interaction which is, however, unlikely to be clinically relevant due to the delay in onset of enzyme induction and the short (5-day) duration of RBN treatment. Third, use of RBN in patients receiving chronic treatment with enzyme-inducing ASMs such as carbamazepine, phenytoin or phenobarbital may result in subtherapeutic plasma concentrations of nirmatrelvir. Accordingly, FDA and EMA prescribing information contraindicates the co-administration of RBN with potent CYP3A4 inducers, as they may substantially reduce nirmatrelvir/ritonavir concentrations, leading to a potential loss of virological effect and related development of resistance [1, 2]. Some health professional organizations, such as the Israeli Chapter of the International League against Epilepsy (ILAE), have aligned with these recommendations [29]. The regulatory contraindications to the use of RBN could be problematic for many individuals with epilepsy, because there are no orally administered anti-COVID-19 medications as effective as RBN currently available [3].
This article provides an assessment of clinically relevant interactions between RBN and concomitant ASMs, and discusses therapeutic strategies for ASM-treated patients who acquire COVID-19 and are at risk for progression to severe disease.
2 Literature Search
We conducted a literature search in PubMed using the key words ‘antiepileptic drugs’ and ‘drug interactions’ and ‘nirmatrelvir’ or ‘ritonavir’ and 'human'. For the compilation of Tables 1 and 2 and for additional information, we searched PubMed using the key words ‘ritonavir’ or ‘nirmatrelvir’ associated with each of the following ASMs: brivaracetam, cannabidiol, carbamazepine, cenobamate, clobazam, clonazepam, diazepam, eslicarbazepine acetate, ethosuximide, felbamate, fenfluramine, gabapentin, lacosamide, lamotrigine, levetiracetam, lorazepam, midazolam, oxcarbazepine, perampanel, phenytoin, phenobarbital, pregabalin, primidone, rufinamide, stiripentol, topiramate, valproic acid, vigabatrin, and zonisamide. References cited in the relevant publications identified by the search and authors’ files were reviewed. We also reviewed European and US prescribing information for each of the ASMs and antiviral medicines discussed in this article.
3 Pharmacokinetic Characteristics of Ritonavir and Nirmatrelvir
Ritonavir absolute bioavailability following oral dosing is unknown, but based on mass balance studies the extent of absorption is estimated to be > 60% [5, 30]. Absorption is not affected to a major extent by intake with food [5, 30]. Ritonavir is 98–99% bound to plasma proteins. Its half-life is in the order of 3–5 hours and its average oral clearance (CL/F) following multiple dosing is in the range of 7–9 L/h [5]. Ritonavir appears to induce its own clearance (CL) following multiple dosing compared to its single-dose CL [5]. Ritonavir is extensively metabolized primarily by CYP3A; four metabolites have been identified in humans but are unlikely to contribute to the antiviral effect [5]. Ritonavir CL is minimally affected by other CYP3A inhibitors [5], including ketoconazole [31]. Rifampicin, a potent CYP3A inducer, when co-administered with a booster dose of ritonavir (100 mg twice daily [BID]), decreases ritonavir plasma exposure (AUC) and trough plasma ritonavir concentration by about 90% [32, 33].
When it is administered alone, nirmatrelvir is absorbed relatively rapidly from the gastrointestinal tract, with peak plasma concentration occurring about 3 hours after dosing [1]. The plasma protein binding of nirmatrelvir is estimated at 69%. Nirmatrelvir is metabolized by CYP3A-mediated metabolism. Co-administration with the CYP3A inhibitor ritonavir increases plasma nirmatrelvir concentrations several-fold and prolongs its half-life, resulting in persistence of effective antiviral concentrations throughout a 12-h dosing interval [34]. During repeated co-administration, ritonavir inhibits nirmatrelvir metabolism so effectively as to reduce nirmatrelvir metabolic clearance to negligible values. In pharmacokinetic studies following co-administration with ritonavir, the only nirmatrelvir-related entity detected in plasma was unchanged nirmatrelvir [2]. Following multiple oral dosing of RBN (300/100 mg BID) to 12 healthy subjects, nirmatrelvir’s mean half-life was 6.05 hours and its mean CL/F was 9 L/h [1], with nirmatrelvir being mainly eliminated unchanged in the feces (28–50% of the oral dose) and in the urine [1, 2].
4 Impact of Inhibition-Based Drug Interactions Caused by Ritonavir-Boosted Nirmatrelvir (RBN) on the Management of Patients Receiving Antiseizure Medications (ASMs)
Enzyme inhibition-based drug interactions in patients receiving RBN can be ascribed primarily to ritonavir’s ability to act as a potent inhibitor of CYP3A enzymes, most importantly CYP3A4 [1, 2]. There is conflicting information on whether nirmatrelvir can affect CYP3A activity and no evidence of its impact on CYP3A inhibition caused by ritonavir [1, 2]. Indeed, a phase I study that used oral midazolam as a CYP3A4 probe substrate found that nirmatrelvir did not affect the prominent inhibition of midazolam first-pass metabolism caused by ritonavir [35].
Following oral dosing with ritonavir in humans, CYP3A inhibition is rapid, mechanism-based, dose- and exposure duration-dependent, with maximal inhibition being reached after 2 days of exposure [15]. The rate of disappearance of CYP3A inhibition after ritonavir withdrawal can be highly variable, with appreciable inhibition being generally still present 3 days after discontinuation of the drug [15, 36]. The increase in plasma concentration of CYP3A substrates when given concomitantly with ritonavir can be quite large. For example, ritonavir (500 mg BID for 7 days) increased rifabutin plasma exposure at steady-state (AUCss) by 4-fold [37]. The ritonavir-induced increase in the plasma concentration of other drugs is especially prominent for medications, such as midazolam (Table 2), nirmatrelvir, lopinavir, and saquinavir, that undergo extensive CYP3A-mediated first-pass metabolism in the gut or the liver. The reason for this is that inhibition of first-pass metabolism can result in several-fold increases in oral bioavailability. The prominent increase in plasma exposure of CYP3A4 substrates following co-administration with ritonavir has been utilized to boost the activity not only of nirmatrelvir, but also of various human immunodeficiency virus (HIV) and hepatitis C virus (HCV) protease inhibitors [38,39,40,41]. An observation relevant to the potential use of RBN in patients with epilepsy and comorbid COVID-19 is that clinically relevant inhibition of CYP3A-mediated drug metabolism occurs as early as after intake of a single dose of ritonavir [38]. Most ASMs that are CYP3A substrates (Table 3) are not subject to extensive first-pass metabolism, and therefore the decrease of their metabolic clearance by a 5-day course of RBN treatment is likely to be of a smaller magnitude than that reported for orally administered midazolam or protease inhibitors. Yet, the possibility of RBN causing a clinically significant elevation in the plasma concentration of these ASMs should be considered [42].
Because the authorized RBN regimen limits duration of treatment to 5 days, enzyme-inhibition mediated interactions could be expected to have greater clinical relevance for ASMs with relatively short half-lives, such as midazolam and tiagabine, because for these drugs the increase in plasma concentration following metabolic inhibition will occur rapidly. Should RBN be used in patients on chronic therapy with ASMs that are CYP3A substrates, monitoring for potential adverse effects (and plasma concentration elevation) is advisable. This recommendation is in line with a case report from Japan, where a 20-year-old man with epilepsy and HIV infection treated with carbamazepine developed signs of carbamazepine toxicity (vomiting, vertigo and transient liver dysfunction) within 12 h of taking a single oral 200-mg dose of ritonavir [43]. These symptoms were associated with a high plasma carbamazepine concentration, twice the value found before ritonavir was administered. In the same patient, plasma carbamazepine levels declined following ritonavir discontinuation, and rose again (with re-appearance of clinical signs of toxicity) when ritonavir was re-introduced. Another case report described a 49-year-old HIV-infected woman with epilepsy treated with carbamazepine, who developed severe ataxia with inability to walk within 4 days of starting a regimen that included ritonavir (400 mg BID), saquinavir (400 mg BID), and efavirenz (600 mg QD) [44]. Her serum carbamazepine concentration was 20.4 µg/mL, compared with 6.9 µg/mL prior to starting antiviral treatment. Her symptoms remitted after reducing the carbamazepine dose to 100 mg/day, resulting in a serum carbamazepine concentration comparable to that measured before starting antiviral therapy. The interaction was ascribed to rapid inhibition of the CYP3A4-mediated metabolism of carbamazepine by ritonavir. Several other similar cases have been reported [45]. Although not directly applicable to RBN-treated patients because RBN is contraindicated in patients receiving carbamazepine, these reports illustrate the clinical relevance of inhibition-based drug interactions caused by ritonavir. For ASMs that have longer half-lives than carbamazepine, such as zonisamide and perampanel, the increase in their plasma concentrations following addition of a CYP3A4 inhibitor would take place more gradually, but could still be clinically significant.
Special considerations apply to everolimus, a mammalian target of rapamycin (mTOR inhibitor) used as an immunosuppressant which is also approved for the treatment of seizures associated with tuberous sclerosis complex. Everolimus is a CYP3A4 substrate, and its plasma levels have been shown to be increased 15-fold by co-administration of the CYP3A4-inhibitor ketoconazole [6]. Ritonavir could be expected to cause a similar interaction, as confirmed by a recent case report [46]. Accordingly, based on prescribing information and different guidelines, co-administration of everolimus with strong enzyme inhibitors, including ritonavir [6, 47, 48] and RBN [3, 6, 7], should be avoided [46, 47]. A management option in COVID-19 patients requiring RBN therapy consists of withholding everolimus for the duration of RBN treatment and for the subsequent 3 days [6, 49], but for people with epilepsy, potential adverse consequences on seizure control could be a concern. For transplant patients receiving everolimus who require treatment to prevent progression of COVID-19 to severe disease, the American Society of Transplantation (AST) does not encourage prescription of RBN, and recommends use of an alternative antiviral treatment [50] which, based on current evidence, should preferably be remdesivir [4]. It might be wise to extend this recommendation to patients receiving everolimus as an antiseizure treatment.
Another medication that requires special consideration is midazolam, a CYP3A4 substrate which, as an ASM, is used mostly by the buccal, intranasal or intravenous (i.v.) routes for the acute (emergency) treatment of prolonged seizures, seizure clusters or status epilepticus. RBN (300/100 mg BID for 5 days) has been found to increase the plasma exposure (AUC) to orally administered midazolam by 14-fold, and to increase midazolam half-life by 2-fold (Table 2) [1, 2, 35]. As a result, based on European and US prescribing information, use of oral midazolam is contraindicated in patients receiving RBN treatment [1, 2]. The impressive increase in midazolam exposure by RBN after oral intake of midazolam is mostly due to inhibition of its gastrointestinal and hepatic first-pass metabolism by ritonavir. When midazolam is used buccally or intranasally for seizure control, its first-pass metabolism is largely avoided and the magnitude of interaction with RBN may be attenuated, but it is most likely to remain clinically significant (Table 2). Accordingly, Noyman et al. [29] recommended that rescue therapy with buccal midazolam should be avoided in RBN-treated patients, and that an alternative rescue ASM, such as rectal diazepam (an ASM metabolized not only by CYP3A4, but also by CYP2C19) be used instead, at least in the out-of-hospital setting. Intranasal diazepam or intranasal lorazepam can also be valuable alternative rescue medications, with lorazepam having the advantage of being cleared by glucuronide conjugation. Of note, diazepam is listed in European [2] but not US [1] prescribing information among the medications contraindicated in RBN-treated patients. This is presumably due to the risk of excessive sedation which, however, would not be a major concern when diazepam is used as a single dose as rescue ASM.
Midazolam, diazepam, and lorazepam are also used for the i.v. treatment of status epilepticus. In patients receiving RBN therapy, lorazepam is advantageous because its metabolism is not mediated by CYP3A4. Should i.v. midazolam be required in RBN-treated patients, patients should be closely monitored in a hospital setting where any serious adverse effects such as respiratory depression can be adequately managed [2]. A reduction in midazolam dose requirements should also be considered, especially when more than a single dose of midazolam (or a prolonged infusion) is required [2].
Ritonavir administered as a boosting dose is a weak inhibitor of CYP2D6 [51]. Ritonavir can also act as an inhibitor of P-glycoprotein (P-gp) and nirmatrelvir is known to inhibit several drug transporters in vitro (P-gp, MATE1, OCT1, and OATP1B1) [34]. There is insufficient information to determine whether these effects can lead to clinically relevant interactions with ASMs.
5 Impact of Induction-Based Drug Interactions Caused by RBN on the Management of Patients Receiving ASMs
At clinically relevant concentrations, nirmatrelvir appears to be devoid of enzyme-inducing properties [1]. Conversely, ritonavir, in addition to being a CYP3A inhibitor, acts as an inducer of CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, and other enzymes, including UGTs [1, 2, 5, 34]. Therefore, it has the potential to stimulate the metabolism of ASMs that are substrates of these enzymes. Evidence for this has been provided by studies with ritonavir-containing anti-HIV treatment regimens (Table 2). In particular, ritonavir given in combination with atazanavir (300/100 mg/day atazanavir/ritonavir) or lopinavir (400/100 mg BID lopinavir/ritonavir) for 13 days reduced the mean plasma exposure of lamotrigine, a UGT substrate, by 32 and 50%, respectively [27, 28]. In another study, ritonavir given in combination with lopinavir (400/100 mg BID lopinavir/ritonavir) for 10 days reduced the mean steady-state plasma exposure of phenytoin, a CYP2C9 and CYP2C19 substrate, by 32% (90% CI 16–43) [8]. There is also evidence that relatively long-term ritonavir treatment can stimulate diazepam metabolism [26], though the initial prevailing effect of RBN is likely to be inhibition of diazepam metabolism and potentiation of diazepam effects [7]. In a case report, treatment with ritonavir (99 mg TID) in combination with other anti-HIV medications was associated with a 48% decrease in plasma concentrations of valproic acid (a UGT substrate) and exacerbation of mania in a patient with bipolar disorder on valproic acid therapy [52].
Because ritonavir has a short half-life (3–5 h), steady-state plasma ritonavir concentrations are expected to be reached soon after starting treatment. However, unlike enzyme inhibition that occurs as soon as the inhibitor appears in circulation at sufficient concentrations, enzyme induction requires a few days to develop fully, because its time-course depends on the turnover times of the induced enzymes which are generally longer than the half-lives of most ASMs [53]. Therefore, when ritonavir (with nirmatrelvir) is used only for 5 days as recommended, its induction potential is likely to be far less relevant clinically compared with its enzyme inhibiting activity [1]. In spite of this, European RBN prescribing information states that "ritonavir dosed as a pharmacokinetic enhancer induces oxidation by CYP2C9 and glucuronidation and as a result is expected to decrease the plasma concentrations of anticonvulsants. Careful monitoring of serum levels or therapeutic effects is recommended when these medicines are co-administered with ritonavir." [2]. Monitoring plasma ASM levels, however, can be difficult considering that RBN treatment is primarily administered outside the hospital setting and for a short duration.
In fact, the effect of a 5-day course of RBN on the plasma levels of ASMs that are metabolized by CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, and UGTs has not been investigated. As discussed above, ritonavir used in combination with anti-HIV medications for 10–13 days (a treatment period longer than that recommended for RBN) reduces the plasma exposure of lamotrigine, phenytoin, and valproic acid. Although these interactions are unlikely to be clinically significant given the short duration of RBN treatment [1], patients receiving other ASMs that are substrates of enzymes induced by ritonavir (Table 3) may be advised to report any unexpected change in seizure control [2, 35].
6 Effects of ASMs on the Pharmacokinetics of RBN and Its Antiviral Effectiveness in Patients with COVID-19
6.1 Effect of Potent Enzyme-Inducing ASMs on RBN Pharmacokinetics
Because nirmatrelvir and ritonavir are extensively metabolized by CYP3A, their clearance is influenced by concomitant treatment with ASMs affecting the activity of this enzyme. The main concern relevant to epilepsy management which was raised during RBN development was the possibility of decreased plasma concentration of nirmatrelvir, the RBN component active against the anti-SARS-CoV-2 virus, in patients receiving enzyme inducing ASMs. This concern was justified by a considerable body of evidence indicating that potent enzyme-inducing ASMs, particularly phenytoin, carbamazepine, and phenobarbital, markedly reduce the plasma concentrations of anti-HIV drugs (Table 1) [54, 55] to levels below those required to suppress viral replication [54,55,56]. A decrease in plasma nirmatrelvir exposure in patients taking enzyme inducing ASMs is expected to occur as a result of two processes, namely a direct increase in nirmatrelvir metabolic clearance as a well a reduced inhibition of nirmatrelvir metabolism by ritonavir, because plasma ritonavir concentration is also expected to be reduced by enzyme induction.
Based on this background, the RBN manufacturer conducted a pre-authorization study to assess the influence of carbamazepine on the pharmacokinetics of nirmatrelvir in nine healthy individuals. The study has not been published, and only limited information is accessible through regulatory documents. According to these documents, participants received RBN (300 mg/100 mg) on two occasions, in a control session (RBN alone) and during the last 5 days of a 15-day treatment with carbamazepine (100 mg BID days 1–3, 200 mg BID days 4–7, and 300 mg BID days 8–15). There seems to be a discrepancy in regulatory files as to whether RBN was given as a single dose [57] or multiple doses [1, 35]. In spite of this uncertainty, co-administration with carbamazepine was associated with a reduction in mean nirmatrelvir AUC to 44.50% (90% CI 33.77–58.65) of the AUC value recorded when RBN was given alone [1, 2, 57, 58]. In parallel, peak plasma nirmatrelvir concentration (Cmax) was reduced to 56.80% (90% CI 47.0–68.6) of the value recorded in the control session.
These results and their potential clinical implications were discussed in EMA’s preliminary public assessment report issued on December 16, 2021 which recognized the need “to take into consideration a risk of efficacy loss caused by carbamazepine induction, and an urgent medical need to treat patients with epilepsy at high risk for progression to severe COVID-19. Because ASMs treatment in this population cannot be easily interrupted, even for a short period of time, further discussion is needed on the expected efficacy at the proposed therapeutic dose (i.e. 300 mg /100 mg nirmatrelvir/ritonavir) and the therapeutic margin in this particular population” [57]. The report concluded that the impact of carbamazepine on RBN efficacy at a 300/100 mg dose is ‘uncertain’, and that it is difficult to predict whether “a dose increase would enable to strictly avoid a sub-optimal concentration with a critical risk of resistance” [57]. This reasoning led European regulators to further conclude that a dose increase cannot be proposed, and that treatment with carbamazepine should be conservatively listed as a contraindication to the use of RBN [2, 35]. Similarly to US prescribing information [1], the contraindication is also extended to phenytoin and phenobarbital, which are also potent enzyme inducers. Interestingly, neither European nor US prescribing information lists primidone as a contraindicated comedication, despite evidence that primidone is extensively converted to phenobarbital and shows enzyme-inducing properties similar to those of potent enzyme-inducing ASMs [59]. Presumably, failure to list primidone among potentially interacting ASMs is due to the fact that, currently, primidone is rarely used in the treatment of epilepsy. In any case, it would appear reasonable to consider primidone as equivalent to phenobarbital for the purpose of COVID-19 management in patients with epilepsy, as also suggested by the COVID-19 Treatment Guidelines Panel of the National Institutes of Health (NIH) [3].
It is worth emphasizing that withdrawal of potent enzyme-inducing ASMs is not an option for patients requiring RBN treatment, not only because of the risk of loss of seizure control but also because enzyme induction persists for at least several days after discontinuation of the inducer. This implies that the interaction with nirmatrelvir/ritonavir cannot be prevented by stopping carbamazepine, primidone, phenytoin, or phenobarbital. It also implies that the contraindication to RBN use applies not only to patients being treated with potent enzyme-inducing ASMs, but also to those who received the same ASMs in the previous 14 days [7].
6.2 Effects of Other ASMs on RBN Pharmacokinetics
Other ASMs, most notably oxcarbazepine, eslicarbazepine acetate, and rufinamide, are less potent inducers than carbamazepine, phenytoin, and phenobarbital [60, 61]. Additionally, there are ASMs (namely felbamate [60] and cenobamate [62]) that can have both inducing and inhibiting activities on CYP3A. The effects of these ASMs on RBN pharmacokinetics is unknown, although based on their interaction profile with other medications [60,61,62], a moderate enzyme-inducing effect can be expected. US and European prescribing information does not specifically contraindicate the use of RBN in patients with epilepsy receiving these ASMs as comedication. The COVID-19 Advisory for Ontario, however, does list oxcarbazepine and eslicarbazepine acetate (together with carbamazepine, phenytoin, phenobarbital, and primidone) among the ASMs which, if used within past 14 days, contraindicate use of RBN [7]. On the other hand, the University of Liverpool Drug Interaction Checker considers the potential for interaction of oxcarbazepine and eslicarbazepine acetate with RBN as ‘weak’ (not warranting a contraindication), stating that these medications “could potentially decrease nirmatrelvir/ritonavir exposure, although to a limited extent” [6]. Of note, in a preliminary report oxcarbazepine has been suggested not to affect the antiviral response to the anti-HIV drug dolutegravir [63]. On the contrary, the metabolism of dolutegravir is induced to a clinically significant extent by carbamazepine [55].
Some ASMs, most notably stiripentol, can inhibit CYP3A [64] and therefore can potentially increase the plasma concentration of RBN. Interactions with ASMs that inhibit CYP3A such as stiripentol are unlikely to have major clinical significance for two sets of reasons. First, co-administration of RBN with the potent CYP3A4 inhibitor itraconazole (200 mg/day for 8 days) was only associated with a modest (38%) increase in nirmatrelvir plasma exposure (AUC), which was not regarded to be clinically significant [35]. Accordingly, prescribing information does not contraindicate the concurrent use of RBN and itraconazole, although careful monitoring for potential side effects of the antiviral treatment is advised. Second, ritonavir is a potent CYP3A inhibitor, and it is likely that CYP3A is already maximally inhibited by ritonavir.
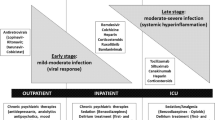
7 Management of COVID-19 in Patients Receiving ASMs Contraindicating Use of RBN
The approach to anti-SARS-CoV-2 therapy requires consideration of several factors, including characteristics of the affected individual, vaccination and immune status, presence of any interacting comedications, stage of COVID-19 disease and its clinical manifestations, the SARS-CoV-2 variant prevailing at the time, and the healthcare resources available in each specific setting [3]. This section focuses mostly on treatment options for non-hospitalized adults with epilepsy receiving enzyme-inducing ASMs contraindicating the use of RBM. Recommendations concerning treatment choices in these patients are based primarily on current NIH guidelines for the management of COVID-19 in the US and areas where the Omicron BA.2 subvariant has become prevalent [4]. For updates, and for recommendations concerning other regions or the management of COVID-19 in children and in patients hospitalized because of COVID-19, health professionals should refer to other available comprehensive guidelines [3, 65,66,67,68,69].
For non-hospitalized adults from areas where Omicron BA.2 is the dominant subvariant, three alternative anti-SARS-CoV-2 medications, namely remdesivir, bebtelovimab, and molnupiravir, should be considered whenever RBN is unavailable or contraindicated due to the risk of drug interactions (Table 4). A fourth previously considered medication, the monoclonal antibody sotrovimab, is no longer recommended because of its substantially decreased in vitro activity against the Omicron BA.2 subvariant [4].
Remdesivir is a prodrug ultimately converted to an active nucleoside triphosphate metabolite (GS-443902), which is incorporated into the SARS-CoV-2 RNA and prevents viral replication by inhibiting RNA-dependent RNA polymerase [70]. Remdesivir has very low oral bioavailability due to extensive first-pass metabolism, and therefore needs to be administered by the i.v. route. In non-hospitalized high-risk patients, remdesivir’s efficacy rate in reducing progression to severe COVID-19 disease was 87% [71], a rate similar to that reported for RBN [4]. In vitro, remdesivir can affect the activity of various CYP enzymes and transporters (Table 4), but the clinical significance of these effects is unclear. The risk of interactions leading to inhibition or induction of enzymes involved in remdesivir metabolism, or interactions affecting remdesivir transporters (Table 4), is also unknown [72]. Although only a minor proportion of remdesivir is metabolized by CYP3A, European prescribing information states that co-administration of remdesivir with strong enzyme inducers is not recommended, though not formally contraindicated [73]. In fact, the strong inducer rifampicin has been predicted to have only a modest effect on remdesivir exposure [74], suggesting that co-administration with carbamazepine and other enzyme-inducing ASMs should not be associated with any major interaction.
Bebtelovimab is an anti-SARS-CoV-2 monoclonal antibody that received FDA emergency use authorization for the treatment of non-hospitalized patients with mild to moderate COVID-19 who are at high risk of progressing to severe disease [75]. Evidence for its efficacy comes from laboratory data showing potent activity against the Omicron variant and its BA.1, BA1.1 and BA.2 subvariants, and from a single phase II, randomized, placebo-controlled trial in COVID-19 individuals who were at low risk of progressing to severe disease [3]. The risk of interactions between bebtelovimab and ASMs is considered to be low. However, in some disease states, treatment with monoclonal antibodies can result in altered plasma concentrations of concomitant medications [76], suggesting that careful monitoring of response and/or plasma ASM levels is desirable should bebtelovimab be used in patients receiving ASMs.
Molnupiravir is, like remdesivir, an ester prodrug which undergoes rapid hydrolysis to the ribonucleoside analogue N4-hydroxycytidine, the primary entity found in blood. N4-hydroxycytidine distributes into cells where it is phosphorylated to the pharmacologically active entity N4-hydroxycytidine triphosphate, which is eliminated by similar metabolic pathways as endogenous pyrimidines [77, 78]. In a pivotal clinical trial in non-hospitalized high-risk COVID-19 patients, molnupiravir reduced the risk of progression to severe disease by 30% [79], which is a lower efficacy rate than that associated with RBN and remdesivir [4, 80]. Molnupiravir, however, has the advantage over bebtelovimab and remdesivir of being suitable for oral administration. Molnupiravir metabolism is also not CYP-mediated and is not susceptible to inhibition- or induction-based drug interactions with concomitant medications. Additionally, neither molnupiravir nor its metabolite N4-hydroxycytidine affect the activity of CYP enzymes and transporters [78].
Taking all evidence into account, current NIH guidelines for the management of non-hospitalized adults with COVID-19 who are at high risk of disease progression recommend that, when RBN is not available or cannot be used because of drug interactions, remdesivir should be used as a first option [4]. According to the same guidelines, bebtelovimab or molnupiravir should only be used when RBN or remdesivir are clinically inappropriate, unavailable, or unfeasible to use. These recommendations are justified by the putatively greater efficacy of remdesivir compared with molnupiravir, and the greater level of evidence for the efficacy of remdesivir compared with bebtelovimab. With respect to logistical constraints, molnupiravir is the only medication that is administered orally. Bebtelovimab is given as a single i.v. infusion, and remdesivir as i.v. infusions for 3 consecutive days.
8 Summary and Conclusions
Use of RBN in COVID-19 patients receiving chronic treatment with ASMs requires consideration of bidirectional interactions between these drugs. Specifically, RBN may increase the plasma concentration of some ASMs that are CYP3A4 substrates with a risk of ASM toxicity. The risk of serious adverse effects is particularly high for buccal/intranasal midazolam and for everolimus, which should not be co-administered with RBN (i.v. midazolam may be used, but only in a setting where respiratory depression can be adequately managed). In addition to inhibiting CYP3A4 activity, RBN may induce the metabolism of ASMs that are metabolized by CYP2C9, CYP2C19, or UGTs, leading to a decrease in their plasma concentrations. Because of the short duration of RBN therapy (5 days), some of these interactions, particularly those involving induction of ASM metabolism, are likely to be of limited clinical significance. In any case, careful assessment of potential changes in ASM response is advisable when RBN is added on to pre-existing treatment with potentially affected ASMs, and monitoring of plasma ASM concentrations may be especially indicated for ASMs which are CYP3A4 substrates.
A specific group of interactions causing major concern are those resulting in induction of nirmatrelvir/ritonavir metabolism by ongoing treatment with potent enzyme-inducing ASMs, namely carbamazepine, phenytoin, phenobarbital, and primidone. Treatment with these ASMs is a contraindication to the use of RBN.
Patients with epilepsy who are at high risk of progression to severe COVID-19 disease and in whom RBN is contraindicated need to be treated with alternative anti-SARS-CoV-2 agents. Although remdesivir is a valuable alternative, in some settings it may not be readily accessible due to lack of availability, cost considerations, and/or logistic difficulties related to its i.v. route of administration. If remdesivir is not an appropriate option, either bebtelovimab or molnupiravir may be considered. However, evidence about bebtelovimab clinical efficacy is still limited, and molnupiravir (the only orally active alternative anti-SARS-CoV-2 medication) is deemed to have appreciably lower efficacy than RBN and remdesivir.
References
FDA (Food and Drug Administration). Fact sheet for healthcare providers: emergency use authorization for Paxlovid. Revised April 14, 2022. Available at: https://www.fda.gov/media/155050/download. Accessed 4 June 2022.
EMA (European Medicines Agency). Paxlovid. Annex 1. Summary of product characteristics. Updated January 28, 2022. Available at: https://www.ema.europa.eu/en/documents/product-information/paxlovid-epar-product-information_en.pdf. Accessed 26 Feb 2022.
COVID-19 Treatment Guidelines Panel. Coronavirus disease 2019 (COVID-19) treatment guidelines. Ritonavir-boosted nirmatrelvir. National Institutes of Health. Updated May 31, 2022. Available at https://www.covid19treatmentguidelines.nih.gov/management/clinical-management/. Accessed 3 June 2022.
COVID-19 Treatment Guidelines Panel. Coronavirus disease 2019 (COVID-19) treatment guidelines. Therapeutic management of nonhospitalized adults with COVID-19. Updated April 8, 2022. Available at: https://www.covid19treatmentguidelines.nih.gov/management/clinical-management/nonhospitalized-adults--therapeutic-management/. Accessed 3 June 2022.
Hsu A, Granneman GR, Bretz RJ. Ritonavir. Clinical pharmacokinetics and interactions with other anti HIV agents. Clin Pharmacokinet. 1998;35:275–91.
University of Liverpool. Drug interaction checker. Available at: https://www.covid19-druginteractions.org/checker. Accessed 5 June 2022.
COVID-19 Advisory for Ontario. Science Table. Nirmatrelvir/ritonavir (paxlovid): what prescribers and pharmacists need to know. Published and updated: February 23, 2022. Available at: https://covid19-sciencetable.ca/wp-content/uploads/2022/02/NirmatrelvirRitonavir-Paxlovid-What-Prescribers-and-Pharmacists-Need-to-Know-with-Appendix_20220223.pdf. Accessed 4 June 2022.
Lim ML, Min SS, Eron JJ, Bertz RJ, Robinson M, Gaedigk A, et al. Coadministration of lopinavir/ritonavir and phenytoin results in two-way drug interaction through cytochrome P-450 induction. Acquir Immune Defic Syndr. 2004;36:1034–40.
Sekar VJ, Tomaka F, Lavreys L, Meyvisch P, Bleys C, De Pauw M et al. Pharmacokinetic interaction between darunavir in combination with low–dose ritonavir and carbamazepine. Poster Presented at the XVIIth International AIDS Conference, Mexico City, Mexico, August 3–8 2008. Available at http://www.medadvocates.org/resources/conferences/international_aids_conferences/17/darunavir/JD126111Seka%20PosterP'trait.pdf. Accessed 5 June 2022.
Menon RM, Badri PS, Wang T, Polepally AR, Zha J, Khatri A, et al. Drug–drug interaction profile of the all—oral anti-hepatitis C virus regimen of paritaprevir/ritonavir, ombitasvir, and dasabuvir. J Hepatol. 2015;63:20–9.
DiCenzo R, Peterson DR, Cruttenden K, Mariuz P, Rezk NL, Hochreiter J, et al. Effects of minocycline and valproic acid coadministration on atazanavir plasma concentrations in human immunodeficiency virus-infected adults receiving atazanavir–ritonavir. Antimicrob Agents Chemother. 2008;52:3035–9.
Greenblatt DJ, Peters DE, Oleson LE, Harmatz JS, MacNab MW, Berkowitz N, et al. Inhibition of oral midazolam clearance by boosting doses of ritonavir, and by 4,4-dimethyl-benziso-(2H)-selenazine (ALT-2074), an experimental catalytic mimic of glutathione oxidase. Br J Clin Pharmacol. 2009;68:920–7.
Mathias AA, German P, Murray BP, Wei L, Jain A, West S, et al. Pharmacokinetics and pharmacodynamics of GS-9350: a novel pharmacokinetic enhancer without anti-HIV activity. Clin Pharmacol Ther. 2010;87:322–9.
Kirby BJ, Collier AC, Kharasch ED, Whittington D, Thummel KE, Unadkat JD. Complex drug interactions of HIV protease inhibitors 1: inactivation, induction, and inhibition of cytochrome P450 3A by ritonavir or nelfinavir. Drug Metab Dispos. 2011;39:1070–8.
Katzenmaier S, Markert C, Riedel KD, Burhenne J, Haefeli1 WE, Mikus G. Determining the time course of CYP3A inhibition by potent reversible and irreversible CYP3A inhibitors using a limited sampling strategy. Clin Pharmacol Ther. 2011;90:666–73.
Ancrenaz V, Déglon J, Samer C, Staub C, Dayer P, Daali Y, et al. Pharmacokinetic interaction between prasugrel and ritonavir in healthy volunteers. Basic Clin Pharmacol Toxicol. 2013;112:132–7.
Eichbaum C, Cortese M, Blank A, Burherne J, Mikus G. Concentration effect relationship of CYP3A inhibition by ritonavir in humans. Eur J Clin Pharmacol. 2013;69:1795–800.
Ieiri I, Tsunemitsu S, Maeda K, Ando Y, Izumi N, Kimura M, et al. Mechanisms of pharmacokinetic enhancement between ritonavir and saquinavir; micro/small dosing tests using midazolam (CYP3A4), fexofenadine (p-glycoprotein), and pravastatin (OATP1B1) as probe drugs. J Clin Pharmacol. 2013;53:654–61.
Stoll F, Burhenne J, Lausecker B, Weiss J, Thomsen T, Haefeli WE, et al. Reduced exposure variability of the CYP3A substrate simvastatin by dose individualization to CYP3A activity. J Clin Pharmacol. 2013;53:1199–204.
Yeh RF, Gaver VE, Patterson KB, Rezk NL, Baxter-Meheux F, Blake MJ, et al. Lopinavir/ritonavir induces the hepatic activity of cytochrome P450 enzymes CYP2C9, CYP2C19, and CYP1A2 but inhibits the hepatic and intestinal activity of CYP3A as measured by a phenotyping drug cocktail in healthy volunteers. J Acquir Immune Defic Syndr. 2006;42:52–60.
Wyen C, Fuhr U, Frank D, Aarnoutse RE, Klaassen T, Lazar A, et al. Effect of an antiretroviral regimen containing ritonavir boosted lopinavir on intestinal and hepatic CYP3A, CYP2D6 and P-glycoprotein in HIV-infected patients. Clin Pharmacol Ther. 2008;84:75–82.
Schmitt C, Hofmann C, Riek M, Patel A, Zwanziger E. Effect of saquinavir–ritonavir on cytochrome P450 3A4 activity in healthy volunteers using midazolam as a probe. Pharmacotherapy. 2009;29:1175–81.
Mathias AA, West S, Hui J, Kearney BP. Dose-response of ritonavir on hepatic CYP3A activity and elvitegravir oral exposure. Clin Pharmacol Ther. 2009;85:64–70.
Dumond JB, Vourvahis M, Rezk NL, Patterson KB, Tien HC, White N, et al. A phenotype–genotype approach to predicting CYP450 and P-glycoprotein drug interactions with the mixed inhibitor/inducer tipranavir/ritonavir. Clin Pharmacol Ther. 2010;87:735–42.
Morcos PN, Chang L, Kulkarni R, Giraudon M, Shulman N, Brennan BJ, et al. A randomised study of the effect of danoprevir/ritonavir or ritonavir on substrates of cytochrome P450 (CYP) 3A and 2C9 in chronic hepatitis C patients using a drug cocktail. Eur J Clin Pharmacol. 2013;2013(69):1939–49.
Polepally AR, King JR, Ding B, Shuster DL, Dumas EO, Khatri A, et al. Drug-Drug Interactions between the anti-hepatitis C virus 3D regimen of ombitasvir, paritaprevir/ritonavir, and dasabuvir and eight commonly used medications in healthy volunteers. Clin Pharmacokinet. 2016;55:1003–14.
van der Lee MJ, Dawood L, ter Hofstede HJ, de Graaff-Teulen MJ, van Ewijk-Beneken Kolmer EW, et al. Lopinavir/ritonavir reduces lamotrigine plasma concentrations in healthy subjects. Clin Pharmacol Ther. 2006;80:159–68.
Burger DM, Huisman A, Van Ewijk N, Neisingh H, Van Uden P, Rongen GA, et al. The effect of atazanavir and atazanavir/ritonavir on UDP-glucuronosyltransferase using lamotrigine as phenotypic probe. Clin Pharmacol Ther. 2008;84:698–703.
Noyman I, Ekstein D, Fahoum F, Herskovitz M, Linder I, Ben Zeev B, et al. Using nirmatrelvir/ritonavir in patients with epilepsy: an update from the Israeli chapter of the International League Against Epilepsy. Epilepsia. 2022;63:1276–8.
FDA (Food and Drug Administration). Norvir. Prescribing information. Updated June 2017. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/209512lbl.pdf. Accessed 24 March 2022.
Bertz R, Wong C, Carothers L, Lauva L, Dennis S, Valdes J. Evaluation of the pharmacokinetics of multiple dose ritonavir and ketoconazole in combination. Clin Pharmacol Ther. 1998;63:230.
Justesen US, Andersen AB, Klitgaard NA, Brøsen K, Gerstoft J, Pedersen C. Pharmacokinetic interaction between rifampin and the combination of indinavir and low-dose ritonavir in HIV-infected patients. Clin Infect Dis. 2004;38:426–9.
de Gast M, Burger D, de Lange W, van Crevel R. Double-trouble: a pharmacokinetic study of indinavir ritonavir (800 + 100 mg bid) and rifampin for patients co-infected with TB and HIV. In: Second International Worskhop on Clinical Pharmacology of HIV Therapy, 2-4 April 2001, Noordwijk, The Netherlands, abstract 1–10.
Owen DR, Allerton CMN, Anderson AS, Aschenbrenner L, Avery M, Berritt S, et al. An oral SARS-CoV-2 Mpro inhibitor clinical candidate for the treatment of COVID-19. Science. 2021;274:1586–93.
EMA (European Medicines Agency), 27 January 2022 EMA/95110/2022—Rev.1 Committee for medicinal products for human use (CHMP) assessment report—paxlovid. Chemical name/international non-proprietary name: (1R,2S,5S)-N-((1S)-1-Cyano-2-((3S)-2-oxopyrrolidin-3-yl)ethyl)-3-((2S)-3,3-dimethyl-2-(2,2,2-trifluoroacetamido)butanoyl)-6,6-dimethyl-3-azabicyclo[3.1.0]hexane-2-carboxamide (PF-07321332)/ritonavir. Procedure No. EMEA/H/C/005973/0000. https://www.ema.europa.eu/en/documents/assessment-report/paxlovid-epar-public-assessment-report_en.pdf. Accessed 26 Feb 2022.
Stader F, Khoo S, Stoeckle M, Back D, Hirsch HH, Battegay M, Marzolini C. Stopping lopinavir/ritonavir in COVID-19 patients: duration of the drug interacting effect. J Antimicrob Chemother. 2020;70:3084–7.
Cato A 3rd, Cavanaugh J, Shi H, Hsu A, Leonard J, Granneman R. The effect of multiple doses of ritonavir on the pharmacokinetics of rifabutin. Clin Pharmacol Ther. 1998;63:414–21.
Hsu A, Granneman GR, Cao G, Carothers L, Japour A, El-Shourbagy T, et al. Pharmacokinetic interactions between two human immunodeficiency virus protease inhibitors, ritonavir and saquinavir. Clin Pharmacol Ther. 1998;63:453–64.
King JR, Wynn H, Brundage R, Acosta EP. Pharmacokinetic enhancement of protease inhibitor therapy. Clin Pharmacokinet. 2004;43:291–310.
Corbett AH, Lim ML, Kashuba AD. Kaletra (lopinavir/ritonavir). Ann Pharmacother. 2002;36:1193–203.
EMA (European Medicines Agency). Kaletra—Annex 1. Summary of product characteristics. Updated October 30, 2017. Available at: https://www.ema.europa.eu/en/documents/product-information/kaletra-epar-product-information_en.pdf. Accessed 5 March 2022.
Jain S, Potschka H, Chandra PP, Tripathi M, Vohora D. Management of COVID-19 in patients with seizures: mechanisms of action of potential COVID-19 drug treatments and consideration for potential drug–drug interactions with anti-seizure medications. Epilepsy Res. 2021;174: 106675. https://doi.org/10.1016/j.eplepsyres.2021.106675.
Kato Y, Fujii T, Mizoguchi N, Takata N, Ueda K, Feldman MD, Kayser SR. Potential interaction between ritonavir and carbamazepine. Pharmacotherapy. 2000;20:851–4.
Burman W, Orr L. Carbamazepine toxicity after starting combination antiretroviral therapy including ritonavir and efavirenz. AIDS. 2000;14:2793–4.
Liedtke MD, Lockhart SM, Rathbun RC. Anticonvulsant and antiretroviral interactions. Ann Pharmacother. 2004;38:482–9.
Meziyerh S, Zwart TC, van Etten RW, Janson JA, van Gelder T, Alwayn IPJ, et al. Severe COVID-19 in a renal transplant recipient: a focus on pharmacokinetics. Am J Transplant. 2020;20(7):1896–901.
Afinitor/Afinitor Dispertz. US prescribing information. Updated April 2018. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/022334s040,203985s013lbl.pdf. Accessed 9 June 2022.
Afinitor. US prescribing information. Updated October 2010. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022334s6lbl.pdf. Accessed 9 June 2022.
Salerno DM, Jennings DL, Lange NW, Kovac DB, Shertel T, Chen JK, et al. Early clinical experience with nirmatrelvir/ritonavir for the treatment of COVID-19 in solid organ transplant recipients. Am J Transplant. 2022. https://doi.org/10.1111/ajt.17027 (ahead of print).
Kumar D, Humar A, Ison MG, Kaul D, Blumberg E, Theodoropoulos N et al. AST statement on oral antiviral therapy for COVID-19 for organ transplant recipients. Available at: https://www.myast.org/sites/default/files/AST%20Statement%20on%20Oral%20Antiviral%20Therapy%20for%20COVID%20Jan%204%20%282%29.pdf. Accessed 9 June 2022.
Aarnoutse RE, Kleinnijenhuis J, Koopmans PP, Touw DJ, Wieling J, Hekster YA, Burger DM. Effect of low-dose ritonavir (100 mg twice daily) on the activity of cytochrome P450 2D6 in healthy volunteers. Clin Pharmacol Ther. 2005;78:664–74.
Sheehan NL, Brouillette MJ, Delisle MS, Allan J. Possible interaction between lopinavir/ritonavir and valproic aid exacerbates bipolar disorder. Ann Pharmacother. 2006;40:147–50.
Derendorf H, Schmidt S. Rowland and Tozer’s clinical pharmacokinetics and pharmacodynamics. 5th ed. South Holland: Wolters Kluwer; 2020. p. 531–70.
Birbeck GL, French JA, Perucca E, Simpson DM, Fraimow H, George JM, et al. Antiepileptic drug selection for people with HIV/AIDS: EVIDENCE-based guidelines from the ILAE and AAN. Epilepsia. 2012;53:207–14.
Song I, Weller S, Patel J, Borland J, Wynne B, Choukour M, et al. Effect of carbamazepine on dolutegravir pharmacokinetics and dosing recommendation. Eur J Clin Pharmacol. 2016;72:665–70.
Okulicz JF, Grandits GA, French JA, Perucca E, George JM, Landrum ML, et al. The impact of enzyme-inducing antiepileptic drugs on antiretroviral drug levels: a case–control study. Epilepsy Res. 2013;103:245–53.
EMA (European Medicines Agency) 16 December 2021 EMA/783153/2021 Committee for Medicinal Products for Human Use (CHMP) Assessment report—procedure under Article 5(3) of Regulation (EC) No 726/2004. Invented name: Paxlovid. INN/active substance: PF-07321332/ritonavir. Procedure number: EMEA/H/A-5(3)/1513 https://www.ema.europa.eu/en/documents/referral/paxlovid-pf-07321332-ritonavir-covid-19-article-53-procedure-assessment-report_en.pdf. Accessed 26 January 2022.
EMA (European Medicines Agency). Conditions of use, conditions for distribution and patients targeted and conditions for safety monitoring addressed to Member States for unauthorized product Paxlovid (PF-07321332 150 mg and ritonavir 100 mg). Available at https://www.ema.europa.eu/en/documents/referral/paxlovid-pf-07321332-ritonavir-covid-19-article-53-procedure-conditions-use-conditions-distribution_en.pdf. Accessed 26 Jan 2022.
Perucca E, Hedges A, Makki KA, Ruprah M, Wilson JF, Richens A. A comparative study of the relative enzyme inducing properties of anticonvulsant drugs in epileptic patients. Br J Clin Pharmacol. 1984;18:401–10.
Benedetti MS. Enzyme induction and inhibition by new antiepileptic drugs: a review of human studies. Fundam Clin Pharmacol. 2000;14:301–19.
Perucca E, Cloyd J, Critchley D, Fuseau E. Rufinamide: clinical pharmacokinetics and concentration-response relationships in patients with epilepsy. Epilepsia. 2008;49:1123–41.
FDA (Food and Drug Administration). Xcopri. Prescribing information. Updated November 2019. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/212839s000lbl.pdf. Accessed 27 Feb 2022.
Kandil MM, Badowski ME, Schriever CA. Sustained viral suppression with co-administration of oxcarbazepine and dolutegravir. Int J STD AIDS. 2018;29:831–3.
Chiron C. Stiripentol. Neurotherapeutics. 2007;4:123–5.
National Institute for Health and Clinical Excellence (NICE). COVID-19 rapid guideline: managing COVID-19. NICE guideline [NG191]. First published: 23 March 2021, last updated: May 19, 2022. Available at: https://www.nice.org.uk/guidance/ng191. Accessed 3 June 2022.
World Health Organization. Therapeutics and COVID-19. Living guidelines. Last updated: April 22, 2022. Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-therapeutics-2022.3. Accessed 3 June 2022.
European Respiratory Society. COVID-19: Guidelines and recommendations directory. Last Updated May 12, 2022. Available at: https://www.ersnet.org/covid-19/covid-19-guidelines-and-recommendations-directory/. Accessed 3 June 2022.
Infectious Diseases Society of America. IDSA Guidelines on the treatment and management of COVID-19. First published: November 4, 2020, last updated: May 27, 2022. Available at: https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/. Accessed 3 June 2022.
National COVID-19 Clinical Evidence Task Force (Australia). Caring for people with COVID 19: Living guidelines. Last updated: May 27, 2022. Available at: https://covid19evidence.net.au/#living-guidelines. Accessed 3 June 2022.
Deb S, Reeves AA, Hopefl R, Rejusca R. ADME and pharmacokinetic properties of remdesivir: its drug interaction potential. Pharmaceuticals. 2021;14:655.
Gottlieb RL, Vaca CE, Paredes R, Mera J, Wenn BJ, Perez G, et al. Early remdesivir to prevent progression to severe Covid-19 in outpatients. New Eng J Med. 2022;386:305–16.
FDA (Food and Drug Administration). Veklury® (remdesivir). Prescribing information. Revised April 2022. Available https://www.gilead.com/-/media/files/pdfs/medicines/covid-19/veklury/veklury_pi.pdf. Accessed 4 June 2022.
EMA (European Medicines Agency). Veklury®. Annex 1. Summary of product characteristics. Updated March 28, 2022. Available at: https://www.ema.europa.eu/en/documents/product-information/veklury-epar-product-information_en.pdf. Accessed 4 June 2022.
Humeniuk R, Mathias A, Kirby BJ, Lutz JD, Cao H, Osinusi A, et al. Pharmacokinetic, pharmacodynamic, and drug-interaction profile of remdesivir, a SARS-CoV-2 replication inhibitor. Clin Pharmacokinet. 2021;60:569–83.
FDA (Food and Drug Administration). Fact sheet for healthcare providers: emergency use authorization for bebtelovimab. Updated May 2022. Available at: https://www.fda.gov/media/156152/download. Accessed 4 June 2022.
Berman E, Noyman I, Medvedovsky M, Ekstein D, Eyal S. Not your usual drug-drug interactions: monoclonal antibody-based therapeutics may interact with antiseizure medications. Epilepsia. 2022;63:271–89.
FDA (Food and Drug Administration). Fact sheet for healthcare providers: emergency use authorization for molnupiravir. Revised March 2022. Available at: https://www.fda.gov/media/155054/download. Accessed 4 June 2022.
EMA (European Medicines Agency). Conditions of use, conditions for distribution and patients targeted and conditions for safety monitoring addressed to Member States for unauthorized product Lagevrio (molnupiravir). First published November 19, 2021. Available at https://www.ema.europa.eu/en/documents/referral/lagevrio-also-known-molnupiravir-mk-4482-covid-19-article-53-procedure-conditions-use-conditions_en.pdf. Accessed 4 June 2022.
Jayk Bernal A, Gomes da Silva MM, Musungaie DB, Kovalchuk EA, Gonzalez A, Delos Reyes V, et al. Molnupiravir for oral treatment of Covid-19 in nonhospitalized patients. New Eng J Med. 2022;386:509–52.
Brophy JM. Molnupiravir’s authorisation was premature. BMJ. 2022;376: o443. https://doi.org/10.1136/bmj.043.
Acknowledgements
Dr. Maor Wanounou is a PhD student at the Hebrew University–School of Pharmacy of the Faculty of Medicine, under the supervision of Prof. Yoseph Caraco and Prof. Meir Bialer. This paper is abstracted in part from the PhD thesis of Maor Wanounou in partial fulfillment of the PhD degree requirements for The Hebrew University of Jerusalem.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was not supported by any funding source.
Conflict of interest
MW, YC, and RHL do not have any conflict of interest to disclose. MB has received consultancy fees from Boehringer Ingelheim, Medison, Pharma 2B, Rekah-Vitamned, and Xenon Pharmaceuticals. EP has received speaker and/or consultancy fees from Angelini, Arvelle, Biogen, Biopas, Eisai, GW Pharma, PMI Life Sciences, Sanofi group of companies, SKL Life Science, Takeda, UCB Pharma, Xenon Pharma, and Zogenix, and royalties from Wiley, Elsevier, and Wolters Kluwers.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All authors consent to publication of this article.
Availability of data and material
Not applicable because this is a review article.
Code availability
Not applicable.
Author contributions
MW produced an initial draft of the manuscript and conducted a literature search under guidance and supervision from MB, YC, and EP. MB, YC, RHL, and EP contributed to critical evaluation of the data and to revision and finalization of the manuscript.
Compliance with ethical standards
We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Additional information
Note added in proof
In the latest revision of US prescribing information, dated July 6, 2022, primidone is added to the list of contraindicated comedications.
Rights and permissions
About this article
Cite this article
Wanounou, M., Caraco, Y., Levy, R.H. et al. Clinically Relevant Interactions Between Ritonavir-Boosted Nirmatrelvir and Concomitant Antiseizure Medications: Implications for the Management of COVID-19 in Patients with Epilepsy. Clin Pharmacokinet 61, 1219–1236 (2022). https://doi.org/10.1007/s40262-022-01152-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-022-01152-z