Are there differences between a real C0-C1 mobilization and a sham technique in function and pressure pain threshold in patients with chronic neck pain and upper cervical restriction? A randomised controlled clinical trial
Abstract
BACKGROUND:
Chronic neck pain is one of the main reasons for visiting a healthcare professional. In recent years, it has been shown that upper cervical restriction may be a factor involved in neck pain.
OBJECTIVE:
To compare the immediate effects of a real cervical mobilization technique versus a sham cervical mobilization technique in patients with chronic neck pain and upper cervical restriction.
METHODS:
This was a randomised, controlled, double-blind clinical trial. Twenty-eight patients with chronic neck pain were recruited and divided into two groups (14
RESULTS:
In the between-groups comparison, statistically significant differences were found in favour of the real cervical mobilization group in upper cervical extension (
CONCLUSION:
The real cervical mobilization group generates improvements in upper cervical spine movement and pressure pain threshold of right trapezius and right splenius compared to the sham group in patients with chronic neck pain and upper cervical restriction.
1.Background
Neck pain is one of the most frequent causes of consultation for musculoskeletal problems [1] and a leading cause of global disability [2]. Neck pain prevalence in the adult population is 37.2% [3] and, 44% of patients suffering from neck pain develop chronic symptoms [4]. The risk of chronic neck pain and the severity of symptoms increase with age [5] and incidences of 50% are described in people over the age of 45, mainly affecting women [3].
Although neck pain can be caused by multiple aetiologies, including inflammatory, traumatic, infectious or psychosomatic factors, the mechanical component of neck pain is the most common [6]. It can be caused by sustained head and/or arm postures, static weight-bearing or carrying, or repetitive movements of the cervical spine or upper limbs [7].
The most common approaches are the physiotherapy and the pharmacological approach [11]. The most recommended physiotherapeutic techniques are electrotherapy, therapeutic exercise, health education and manual therapy [8],especially with mobilizations [9]. The term “mobilization” refers to low-speed manual therapy techniques that involve continuous passive movement of the joints and/or related soft tissues [10].
The upper cervical spine is characterised by the fact that it is responsible for more than 50% of all head rotation [11]. The International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT) recommends, in the initial treatment sessions, an indirect approach to cervical dysfunction. For example, the upper thoracic segments should be mobilized to increase cervical rotation [12]. In the case of the upper cervical spine, it would be advisable to minimise the risks associated with direct mobilization or manipulation on C1-C2 at the end of the range of rotation [12]. Hidalgo et al. demonstrated in vitro that C0-C1 segment stiffness reduced range of motion and increased resistance to upper cervical rotation [13]. This influence of C0-C1 on upper cervical rotation could mean that the kinematics of C0-C1 may be related to the tensioning of the alar ligament and, indirectly, to the range of motion of C1-C2 in the transverse plane [13].
Different studies have shown that applying a C0-C1 mobilization treatment versus a control/sham group or adding it to a standardized physiotherapy treatment generates benefits in patients with chronic neck pain and upper cervical rotation restriction in pain and range of motion [9, 14, 15, 16, 17, 18]. Also, increasing upper cervical mobility is associated with the improvement of deep muscle recruitment, since there is a linear relationship between the range of motion of the upper cervical spine and the contractile capacity of the deep cervical musculature [19]. However, there is no evidence that incorporates a comparison with a sham manual therapy technique versus C0-C1 mobilization. This study will allow us to understand whether the effects found with C0-C1 mobilization are due to the outcome of the technique itself or to potential expectations of its application in the patient.
This study hypothesizes that a real C0-C1 mobilization technique produces greater changes in upper cervical range of motion, pressure pain threshold and deep cervical flexor muscle activation compared to a sham technique in patients with chronic neck pain and upper cervical restriction.
The aim of this study is to compare if a single treatment of the upper cervical spine through a real C0-C1 mobilization produces changes in upper cervical range of motion, pressure pain threshold and deep cervical flexor muscle activation compared to a sham technique in patients with chronic neck pain and upper cervical restriction.
2.Material and methods
2.1Study design
A double-blind (evaluator and patient) randomised controlled clinical trial was designed, with a 1:1 allocation ratio. The study was conducted at the Universidad San Sebastián, Bío Bío Region, Chile. The study was registered at www.clinicaltrials.gov under no. NCT04351971 on April 16, 2020. The Scientific Ethical Committee of the Concepción Health Service (CESSC) approved this study (protocol number: 1909-91, date: 10 December, 2019). The study was conducted in accordance with the Declaration of Helsinki of 1964 and its later amendments and with the CONSORT guidelines. All patients in this study signed an informed consent form prior to participation.
2.2Inclusion and exclusion criteria
The inclusion criteria were the following: to present a neck pain lasting more than three months, to be over 18 years of age and to present a positive flexion-rotation test (FRT) [20, 21, 22, 23]. A positive FRT is considered if there is a 10
Subjects were excluded from the study when presenting a history of cervical trauma, vertigo syndrome, inability to tolerate the supine position, any cognitive impairment that hinders the understanding of the informed consent and the specific contraindications proposed by IFOMPT [12].
2.3Sample size calculation
The sample size was calculated using GRANMO v7.12, assuming an
2.4Randomisation and blinding
Patients who met the inclusion criteria of the Physiotherapy Centre of the Universidad San Sebastián, Bío Bío Region, Chile, were asked to participate between April and June 2021. Once the exclusion criteria were verified and the informed consent was signed, the subjects were assigned to an intervention group (Manual Therapy or sham technique). The physiotherapist (A) performed the assessments and assigned a correlative number to the participants. The physiotherapist (B) performed the technique and was the only one who had the randomisation list, generated with the Random.org programme. The physiotherapist (A) was thus blinded to the intervention technique performed. The patients remained blinded as they did not know whether the procedure they received was real (C0-C1) or sham (C0-C0).
The intervention was performed by a single physiotherapist with more than 10 years of clinical experience and specialisation in orthopaedic manual therapy. Both groups received a single 5-minute treatment session.
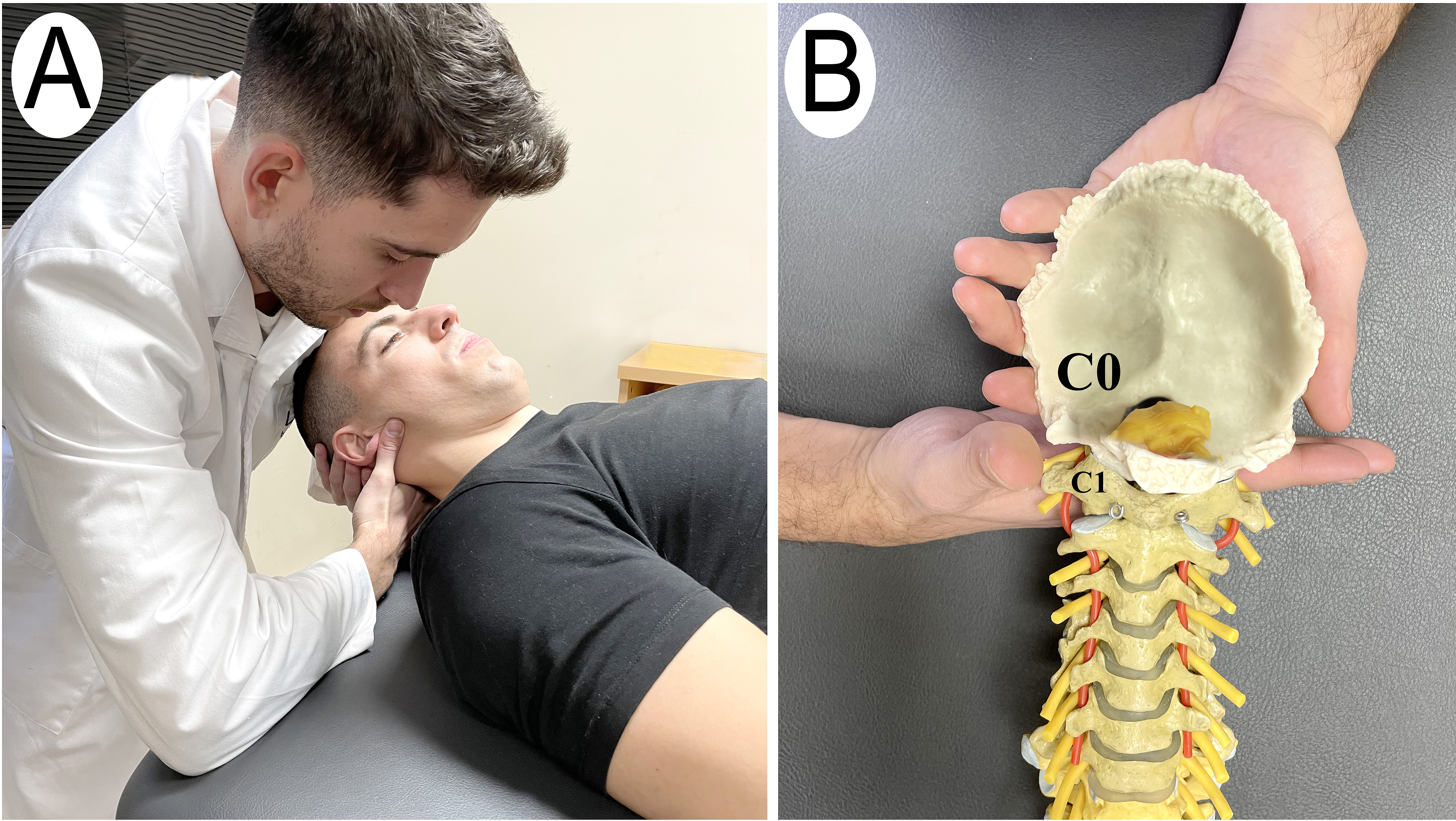
2.4.1Manual therapy C0-C1 group (MT)
Subjects assigned to this group, received the C0-C1 dorsal gliding technique described by Kaltenborn [27] and Krauss [28]. Having the subject in supine position with the head at the upper edge of the table, the physiotherapist positioned the radial edge of his hand with the fingers extended under the posterior arch of the atlas (C1) and with the other hand under the occipital (C0), performed a dorsal pressure on the patient’s forehead using the anterior part of his shoulder. The dorsal mobilization force was applied until a marked resistance was felt and then the pressure was slightly increased to perform a stretching mobilisation (grade III according to Kaltenborn) [29]. The technique was performed in 15 second cycles of gliding and 3 seconds of rest, with a total duration of 5 minutes (Fig. 1).
Figure 1.
Manual therapy C0-C1 group. A) C0-C1 dorsal gliding manual therapy technique. B) Model technique.
2.4.2Sham C0-C0 Technique group (ST)
The “sham technique” group received a C0-C0 sham dorsal mobilization technique. In order to carry out this approach, the subject was supine. The physiotherapist placed both hands under the occipital (C0) and the anterior part of his shoulder on the patient’s forehead and made a slight dorsal pressure with the anterior part of his shoulder. This dorsal pressure was exerted without any therapeutic intention. The technique was performed in 15 second cycles of gliding and 3 seconds of rest, with a total duration of 5 minutes (Fig. 2).
Figure 2.
Sham C0-C0 Technique group. A) Sham technique intervention C0-C0. B) Model technique.
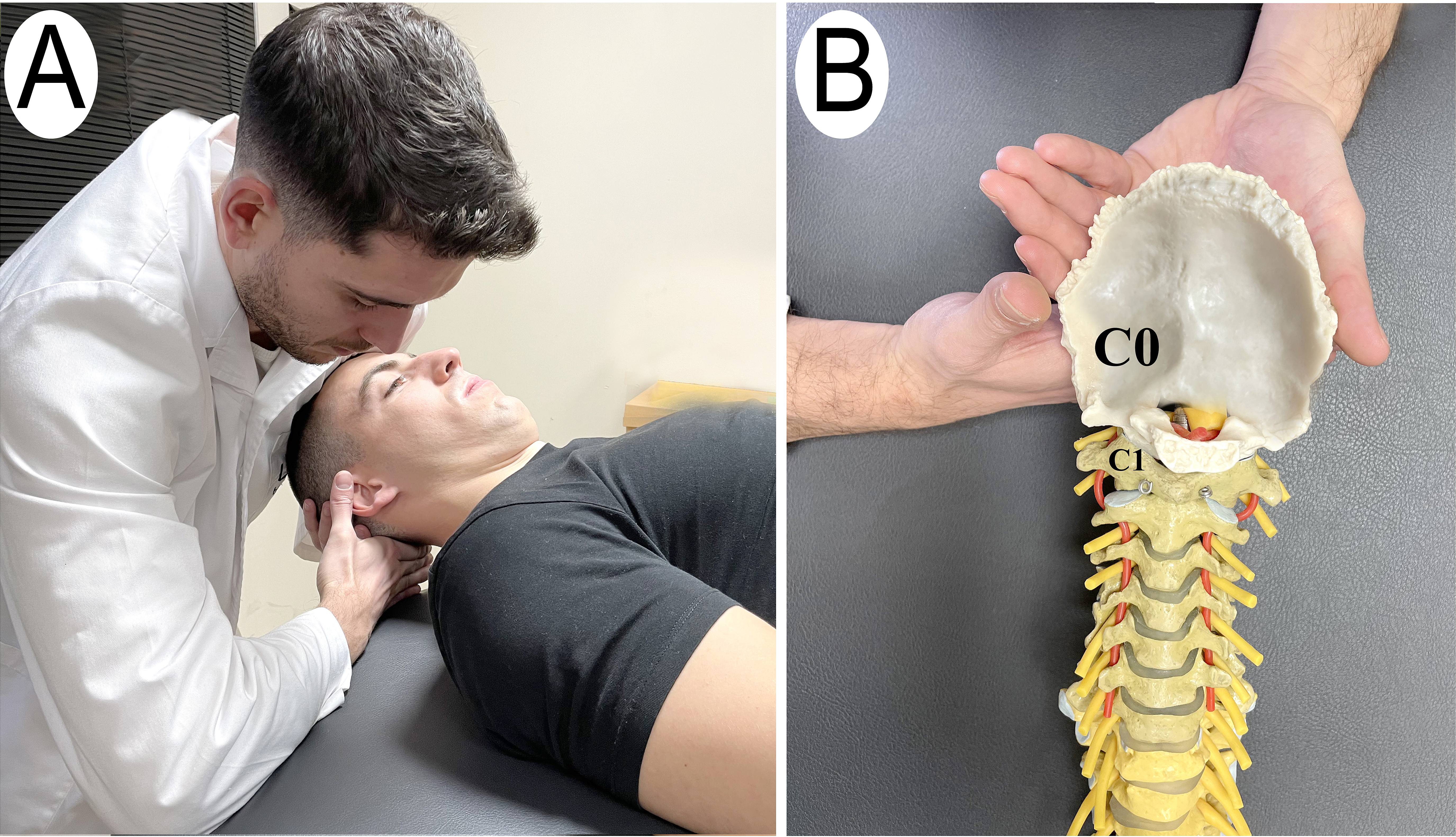
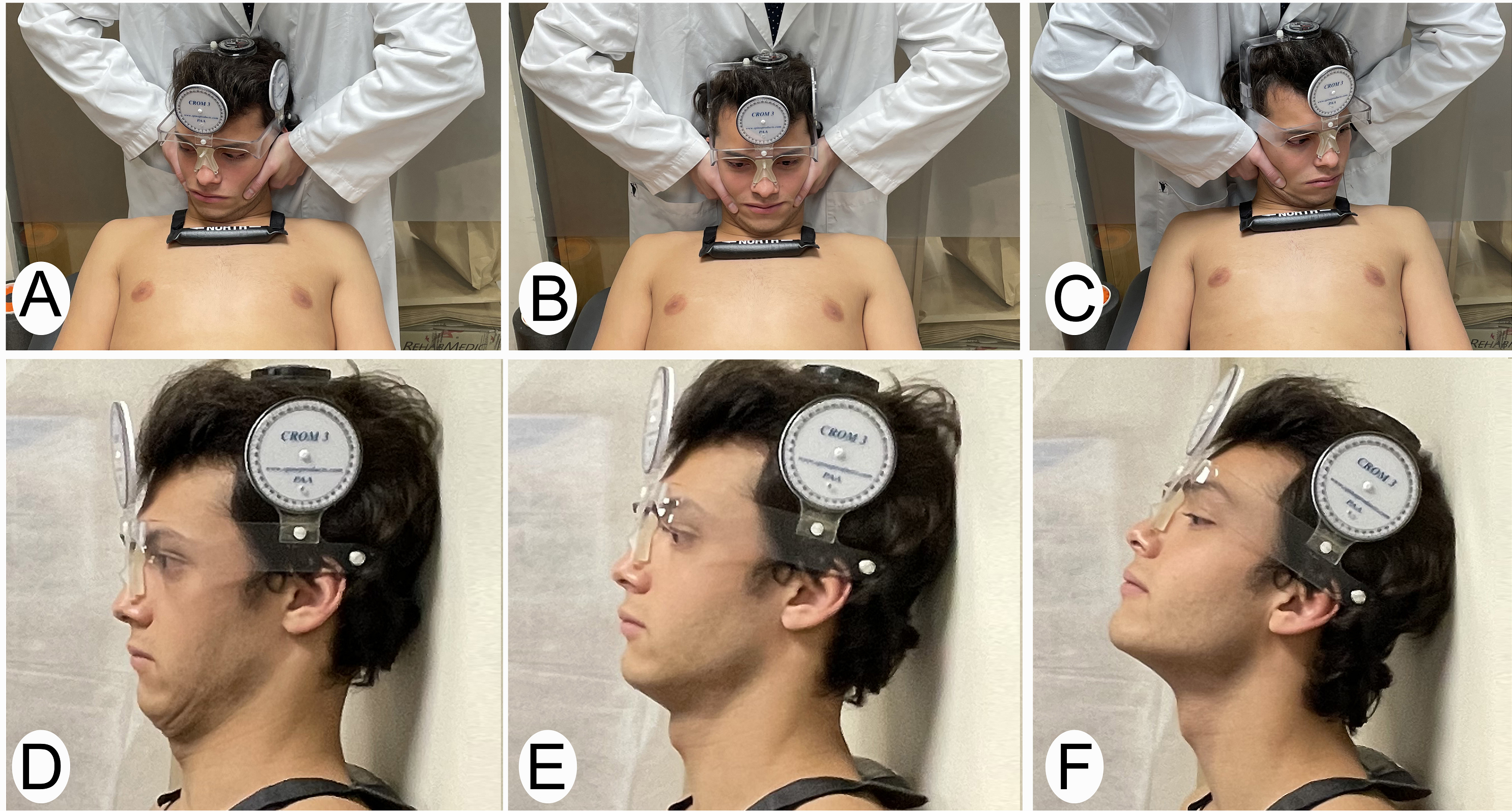
Figure 3.
A, B, C) Sequence of flexion-rotation test to determine the most restricted side. A) Right rotation. B) Neutral position. C) Left rotation. D) Upper flexion movement. E) Neutral position. F) Upper extension movement.
2.5Measurements
Measurements were performed by a physiotherapist (A) who was blinded to the applied technique. The main variable of the study was the FRT variable. The secondary variables were upper flexion-extension mobility, pain pressure threshold and the activation of the deep flexor muscles of the cervical spine. All variables were measured before and after treatment in the above order.
For the upper cervical rotation range, the CROM device (floating compass; Plastimo Airguide, Inc, Buffalo Groove, IL, USA) [30] was used, using the FRT (Fig. 3). The CROM device is a reliable and valid instrument for measuring active and passive ranges of cervical mobility [31, 32, 33, 34].
The FRT test was accomplished with the patient in supine position and with the CROM device. Maximum cervical flexion was performed, followed by rotation, which was stopped if marked resistance was detected and/or the patient felt symptoms [24]. The measurement was carried out three times on each side, being the average of the three measurements the value used for the analysis. The degrees of the most restricted side rotation and the least restricted side rotation of the FRT were registered.
For the measurement of the upper flexion-extension mobility of the upper cervical spine, the measurement was conducted in the standing position according to the method described by Strimpakos et al. [35] (Fig. 3). The CROM device was used, and the patient was positioned with his head against the wall. The patient was asked to perform flexion and extension without taking his head off the wall. The procedure was repeated three times, being the mean of the three measurements the value used for the analysis.
The pain pressure threshold was recorded using a JTECH
The activation of the deep flexor muscles of the cervical spine was carried out with the device (Stabilizer Pressure Biofeedback, Chattanooga Group Inc., USA). With the subject in supine position, the device was placed on the back of the cervical spine, inflating the device to a pressure of 20 mmHg. Subjects were instructed to “nod their head gently as if saying “yes”” to perform the deep muscle contraction. The contraction of the superficial muscles was monitored by observation and palpation. The patient was then instructed to perform this isometric craniocervical flexion for 10 seconds. The procedure was repeated 3 times at each level in which the pressure could be progressively increased by 2 mmHg until a value of 30 mmHg was reached [37]. The test was stopped in case of inability to maintain the contraction without contracting the superficial musculature and/or pain [37].
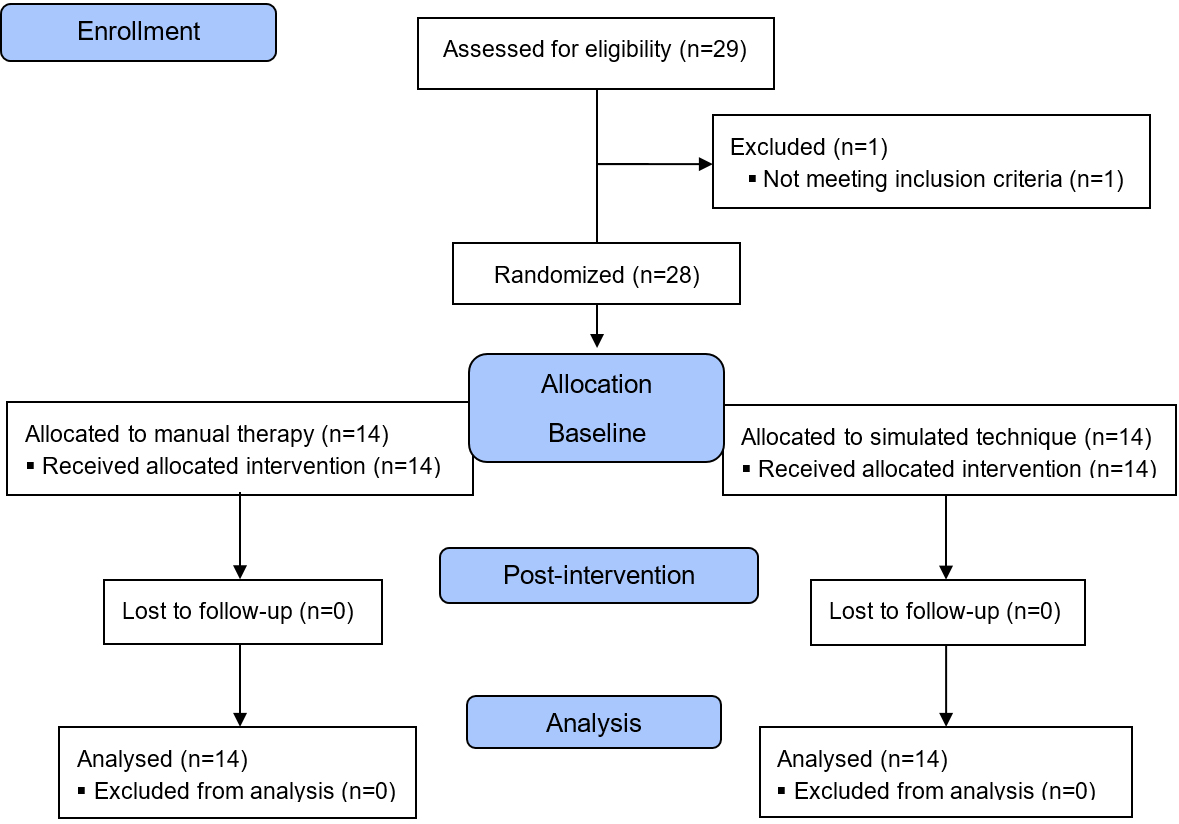
Figure 4.
CONSORT. (Consolidated Standards of Reporting Trial) flow diagram.
2.6Statistical analysis
SPSS Statistics for Windows version 20.0. (IBM Corp., Armonk, NY, USA) was used for all statistical analyses. Descriptive statistics (mean and standard deviations, or number and percentage) were calculated to describe the demographic characteristics of sample.
The Wilcoxon signed-rank test was used for the within-group analysis and, for the between-group analysis the differences were previously calculated. Subsequently, the Mann Whitney U test was performed. In order to estimate the magnitude of the difference between two conditions, the effect size was calculated in the main variables, using Cohen’s coefficient (d). Cohen’s coefficients were interpreted as follows: large effect sizes,
3.Results
Twenty-eight participants with chronic neck pain and upper cervical restriction (Fig. 4) who met the inclusion criteria were recruited with a mean age of 41.9
Table 1
Baseline features for both groups
| MT ( | ST ( | |
| Mean | Mean | |
| Age (years) | 39.93 | 43.93 |
| Pain time (months) | 9.64 | 16.71 |
| Gender | ||
| Female | 10 (71.4%) | 8 (57.1%) |
| Male | 4 (28.6%) | 6 (42.9%) |
Abbreviations: SD: Standard deviation; MT: Manual therapy C0-C1 group; ST: Sham C0-C0 Technique group.
3.1Upper cervical mobility (Flexion, extension and FRT)
In the within-group analysis no difference in the ST group for upper cervical range of motion was found. However, in the MT group, all movements showed statistically significant differences with large effect sizes except for the flexion movement which was moderate (
Table 2
Within-group analysis results
| MT group | ST group | |||||||
| Baseline | Post-intervention | Baseline | Post-intervention | |||||
| Mean | Mean |
| ES | Mean | Mean |
| ES | |
| UCROM( | ||||||||
| Flexion | 5.64 | 8.71 | 0.028 | 0.67 | 8.36 | 8.64 | 0.420 | 0.06 |
| Extension | 34.36 | 40.29 | 0.003 | 1.23 | 34.29 | 34.57 | 0.512 | 0.06 |
| FRT more restricted | 28.71 | 41.14 | 0.002 | 1.74 | 27.57 | 27.57 | 0.916 | 0.00 |
| FRT less restricted | 35.00 | 46.71 | 0.001 | 1.83 | 38.71 | 39.36 | 0.673 | 0.09 |
| PPT (kg/cm | ||||||||
| Right Trapezius | 2.89 | 3.38 | 0.007 | 0.29 | 2.81 | 2.88 | 0.624 | 0.05 |
| Left Trapezius | 2.75 | 3.39 | 0.008 | 0.45 | 2.52 | 2.63 | 0.268 | 0.10 |
| Right Splenius | 2.52 | 3.31 | 0.023 | 0.65 | 2.37 | 2.52 | 0.113 | 0.13 |
| Left Splenius | 2.61 | 3.42 | 0.009 | 0.62 | 2.46 | 2.64 | 0.070 | 0.15 |
| Muscle Activation (mmHg) | ||||||||
| Activation | 28.39 | 28.86 | 0.249 | 0.20 | 27.44 | 27.79 | 0.345 | 0.11 |
Abbreviations: SD: Standard deviation; MT: Manual therapy C0-C1 group; ST: Sham C0-C0 Technique group; UCROM: Upper cervical range of motion; FRT: Flexion-rotation test; PPT: Pressure pain threshold; ES: Effect size.
In the between-group analysis, the MT group presented higher values than the ST, with statistically significant differences except for the cervical flexion movement (Table 3).
Table 3
Between-group analysis results
| MT group | ST group | ||
|---|---|---|---|
| Difference between baseline and post-intervention | Difference between baseline and post-intervention | ||
| Mean | Mean |
| |
| UCROM( | |||
| Flexion | 3.07 | 0.29 | 0.273 |
| Extension | 5.93 | 0.29 | 0.003 |
| FRT more restricted | 12.43 | 0.00 | 0.000 |
| FRT less restricted | 11.71 | 0.64 | 0.007 |
| PPT (kg/cm | |||
| Right Trapezius | 0.49 | 0.06 | 0.040 |
| Left Trapezius | 0.65 | 0.10 | 0.116 |
| Right Splenius | 0.79 | 0.15 | 0.049 |
| Left Splenius | 0.81 | 0.32 | 0.160 |
| Muscle Activation (mmHg) | |||
| Activation | 0.47 | 0.34 | 0.835 |
Abbreviations: SD: Standard deviation; MT: Manual therapy C0-C1 group; ST: Sham C0-C0 Technique group; UCROM: Upper cervical range of motion; FRT: Flexion-rotation test; PPT: Pressure pain threshold; ES: Effect size.
3.2Pressure pain threshold
When analysing the within-group, no statistically significant changes were reported in the pressure pain threshold for the trapezius and splenius muscles evaluated on each side of ST group. However, the MT group showed an increase in pressure tolerance in both muscles on both sides, and these values were statistically significant. The effect size was moderate for the splenius muscle and small for the trapezius muscle (Table 2).
In the between-group analysis, although the difference between baseline and post-intervention in the MT group was larger, statistically significant differences were only reached in the right trapezius muscle (
4.Discussion
The aim of the study was to compare the immediate effects of a real cervical mobilization of the C0-C1 segment with a sham C0-C0 technique on upper cervical range of motion, deep cervical flexor muscle activation and pressure pain threshold in patients with chronic neck pain and upper cervical restriction.
The results obtained suggest that the MT group had significant improvements in cervical range of motion and pressure pain threshold for the right trapezius and right splenius muscles compared to TS but not in the activation of the deep musculature.
The MT group achieved a significant improvement in FRT (1243
In recent years, different authors have demonstrated the indirect effects of manual treatment of segments such as C0-C1 and C2-C3 in the improvement of FRT in patients with chronic neck pain [9, 14, 16]. In terms of upper cervical flexion and extension, the MT achieved similar significant improvements as in other studies [9, 14, 16].
One possible explanation for these results may be due to the relationship between the joint and ligamentous tissue among the C0-C1, C1-C2 and C2-C3 segments [11], in particular, by the alar ligaments. The rotation of C1-C2 is limited by the alar ligament system and the occipital (C0) and C2 are the main bony attachment of these ligaments. Some authors have proposed that the dysfunction of C0-C1 [9, 11, 40] and/or C2-C3 [9, 41] may inhibit the normal rotational mobility of C1-C2. Also, other non-biomechanical mechanisms, such as those of the spinal cord and central nervous system, could explain this improvement [9], because a mechanical stimulus generated by manual therapy trigger neurophysiological responses within the periphery and the central nervous system [42, 43].
Regarding pressure pain threshold, differences between groups were found in the right trapezius and right splenius muscles in favour of the MT group. Different studies have found similar results when real mobilization techniques are applied to this region [9, 16, 17], however, no changes have been described with ST [43]. The minimum detectable change in patients with neck pain is 0.48 kg [44]. In the within-group results, the MT group obtained minimally detectable changes for all measurements of the right and left trapezius and right and left splenius.
The literature supports that manual mobilization techniques increase the pressure pain threshold in subjects with chronic neck pain [45, 46, 47, 48, 49]. These positive effects appear even if using interventions in remote segments such as the thoracic spine [26]. According to Bialosky et al. [42, 43], the mechanical stimulus generated by C0-C1 mobilization may provoke these neurophysiological responses within the nervous system for pain inhibition and consequently positive changes in pressure pain threshold in the upper trapezius and splenius muscles in MT group [42, 43]. It has been established that these changes occur immediately and stabilize over time [40], despite having no knowledge about this effect, as neither short- nor medium-term evaluations were carried out. In relation to the results obtained in the sham group, a similar study performing a sham cervical spine technique did not obtain significant changes in pain [18].
The clinical application of this study provides evidence that C0-C1 dorsal gliding mobilization is an effective approach for increasing upper cervical rotation measured by the FRT. Furthermore, it supports the indirect approach for the C1-C2 dysfunction avoiding end range mobilization and following IFOMPT recommendations for safety in the cervical spine approach [12]. In addition, we observed that a sham technique does not achieve the same results, so applying a manual technique in an appropriate way seems to be a determining factor.
Regarding muscular resistance, no within- or be-tween-group changes were observed. One study observed better deep musculature fibre recruitment and less activation of the superficial musculature in the craniocervical flexion test after specific cervical mobilization [50].
The subjects participating in this study started from near-normal values and, in this test, were assessed without cervical training treatment. Consequently, it is possible that the dose of treatment used and the immediate assessment of the effects were not sufficient to demonstrate a change. Other studies have shown that when patients with chronic neck pain and upper cervical restriction started from pathological values in this test (below 24 mmHg) and training protocols of several weeks were applied, improvements in activation and endurance occurred when combined with manual therapy techniques of the upper cervical spine [16, 17]. We have not observed these findings in our study. Perhaps, if a more precise instrument to measure muscle contraction (e.g. Electromyography) had been used in our study, these findings may have been observed.
The main limitation of this study is the application of a single treatment session and the evaluation of the immediate effects only. In addition, the treatment dose was a single 5-minute session so we do not know if more sessions or a higher dose can affect the results. Another limitation was that no questionnaire was conducted to ensure whether patients were aware of whether they belonged to the sham group or the real intervention group. Another possible limitation is that pain (with VAS or NPRS) was not measured as it could give more information on the effect of the treatments. Further studies with a medium-term follow-up would be necessary to identify whether the findings obtained with immediate effects perpetuate and if the values in the pressure pain threshold normalise with a greater number of sessions and follow-ups.
5.Conclusion
The real C0-C1 dorsal glide mobilization technique generates improvements in upper cervical spine range of motion and pressure pain threshold to right trapezius and right splenius. However, it does not provide significant changes in cervical deep musculature activation compared to the sham C0-C0 technique in patients with chronic neck pain and upper cervical restriction.
Author contributions
GAA: Idea design, writing of the introduction, did the intervention techniques.
MMB: Idea design, manuscript review, did the measurements.
CHG: Idea design, manuscript review.
KCL: Assistance in fieldwork, manuscript review.
APB: Manuscript review, management of research material.
CLdC: Writing of the results, statistical analysis, manuscript review.
JRS: Idea design, writing of the methods and discussion, work supervision, manuscript review.
Funding
This research received no external funding.
Informed consent
Informed consent was obtained from all subjects involved in the study. Subjects who appear in the images in this article have given their permission for the publication.
Acknowledgments
The authors thank patients who participated in this study. They give a special thank you to the Clinical Center of Universidad San Sebastián.
Conflict of interest
The authors declare no conflict of interest.
References
[1] | Ferracini GN, Florencio LL, Dach F, Bevilaqua Grossi D, Palacios-Ceña M, Ordás-Bandera C, et al. Musculoskeletal disorders of the upper cervical spine in women with episodic or chronic migraine. Eur J Phys Rehabil Med. (2017) Jun; 53: (3): 342-50. doi: 10.23736/S1973-9087.17.04393-3. |
[2] | Hoy D, March L, Woolf A, Blyth F, Brooks P, Smith E, et al. The global burden of neck pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. (2014) Jul; 73: (7): 1309-15. doi: 10.1136/annrheumdis-2013-204431. |
[3] | Fernández-de-las-Peñas C, Hernández-Barrera V, Alonso-Blanco C, Palacios-Ceña D, Carrasco-Garrido P, Jiménez-Sánchez S et al. Prevalence of neck and low back pain in community-dwelling adults in Spain: a population-based national study. Spine (Phila Pa 1976). (2011) ; 36: : 213-9. |
[4] | Gross A, Miller J, D’Sylva J, Burnie SJ, Goldsmith CH, Graham N, et al. Manipulation or mobilisation for neck pain: A Cochrane Review. Man Ther. (2010) ; 15: (4): 315-33. doi: 10.1016/j.math.2010.04.002. |
[5] | Delclòs J, Alarcón M, Casanovas A, Serra C, Fernández R, de Peray JL, et al. Identificación de los riesgos laborales asociados a enfermedad sospechosa de posible origen laboral atendida en el Sistema Nacional de Salud. Atención Primaria. (2012) Oct; 44: (10): 611-27. doi: 10.1016/j.aprim.2011.11.006. |
[6] | Buckle PW, Devereux JJ. The nature of work-related neck and upper limb musculoskeletal disorders. Appl Ergon. (2002) May; 33: (3): 207-17. |
[7] | Bot SDM, van der Waal JM, Terwee CB, van der Windt DAWM, Scholten RJPM, Bouter LM, et al. Predictors of Outcome in Neck and Shoulder Symptoms. Spine (Phila Pa 1976). (2005) Aug; 30: (16): E459-70. doi: 10.1097/01.brs.0000174279.44855.02. |
[8] | Sterling M, De Zoete RMJ, Coppieters I, Farrell SF. Best Evidence Rehabilitation for Chronic Pain Part 4: Neck Pain. J Clin Med. (2019) Aug 1; 8: (8). doi: 10.3390/JCM8081219. |
[9] | Rodríguez-Sanz J, Malo-Urriés M, Lucha-López MO, Pérez-Bellmunt A, Carrasco-Uribarren A, Fanlo-Mazas P, et al. Effects of the Manual Therapy Approach of Segments C0-1 and C2-3 in the Flexion-Rotation Test in Patients with Chronic Neck Pain: A Randomized Controlled Trial. Int J Environ Res Public Heal. (2021) ; 18: (2): 753. |
[10] | Gross AR, Kay TM, Kennedy C, Gasner D, Hurley L, Yardley K et al. Clinical practice guideline on the use of manipulation or mobilization in the treatment of adults with mechanical neck disorders. Man Ther. (2002) ; 7: (4): 193-205. |
[11] | Hidalgo García C, Fanlo Mazas P, Malo Urriés M, Pérez Guillén S, Tricás Moreno JM, Lucha López O, et al. Short term Efficacy of C0-C1 Mobilization in the Cervical Neutral Position in Upper Cervical Hypomobility: A Randomized Controlled Trial. J int acad phys ther res. (2016) . |
[12] | Rushton A, Rivett D, Carlesso L, Flynn T, Hing W, Kerry R. International framework for examination of the cervical region for potential of Cervical Arterial Dysfunction prior to Orthopaedic Manual Therapy intervention. Man Ther. (2014) Jun; 19: (3): 222-8. doi: 10.1016/j.math.2013.11.005. |
[13] | Hidalgo-García C, Lorente AI, López-de-Celis C, Lucha-López O, Malo-Urriés M, Rodríguez-Sanz J, et al. Effects of occipital-atlas stabilization in the upper cervical spine kinematics: an in vitro study. Sci Rep. (2021) Dec 1; 11: (1). doi: 10.1038/S41598-021-90052-6. |
[14] | González-Rueda V, Hidalgo-García C, Rodríguez-Sanz J, Bueno-Gracia E, Pérez-Bellmunt A, Rodríguez-Rubio PR, et al. Does upper cervical manual therapy provide additional benefit in disability and mobility over a physiotherapy primary care program for chronic cervicalgia? A randomized controlled trial. Int J Environ Res Public Health. (2020) Nov 2; 17: (22): 1-14. doi: 10.3390/ijerph17228334. |
[15] | González-Rueda V, López-de-Celis C, Bueno-Gracia E, Rodríguez-Sanz J, Pérez-Bellmunt A, Barra-López ME, et al. Short- and mid-term effects of adding upper cervical manual therapy to a conventional physical therapy program in patients with chronic mechanical neck pain. Randomized controlled clinical trial. Clin Rehabil. (2020) . doi: 10.1177/0269215520965054. |
[16] | Rodríguez-Sanz J, Malo-Urriés M, Corral-De-toro J, López-De-celis C, Lucha-López MO, Tricás-Moreno JM, et al. Does the addition of manual therapy approach to a cervical exercise program improve clinical outcomes for patients with chronic neck pain in short-and mid-term? A randomized controlled trial. Int J Environ Res Public Health. (2020) Sep 2; 17: (18): 1-20. doi: 10.3390/ijerph17186601. |
[17] | Rodríguez-Sanz J, Malo-Urriés M, Lucha-López MO, López-de-Celis C, Pérez-Bellmunt A, Corral-de-Toro J, et al. Comparison of an exercise program with and without manual therapy for patients with chronic neck pain and upper cervical rotation restriction. Randomized controlled trial. PeerJ. (2021) Nov 24; 9: : e12546. doi: 10.7717/PEERJ.12546. |
[18] | La Touche R, París-Alemany A, Mannheimer JS, Angulo-Díaz-Parreño S, Bishop MD, Lopéz-Valverde-Centeno A, et al. Does Mobilization of the Upper Cervical Spine Affect Pain Sensitivity and Autonomic Nervous System Function in Patients With Cervico-craniofacial Pain? Clin J Pain. (2013) Mar; 29: (3): 205-15. doi: 10.1097/AJP.0b013e318250f3cd. |
[19] | Falla DL, Campbell CD, Fagan AE, Thompson DC, Jull GA. Relationship between cranio-cervical flexion range of motion and pressure change during the cranio-cervical flexion test. Man Ther. (2003) May; 8: (2): 92-6. |
[20] | Budelmann K, von Piekartz H, Hall T. A normative study of cervical range of motion measures including the flexion-rotation test in asymptomatic children: side-to-side variability and pain provocation. J Man Manip Ther. (2016) Aug 7; 24: (4): 185-91. doi: 10.1179/2042618612Y.0000000026. |
[21] | Schãfer AGM, Schöttker-Königer T, Hall TM, Mavroidis I, Roeben C, Schneider M, et al. Upper cervical range of rotation during the flexion-rotation test is age dependent: an observational study. Ther Adv Musculoskelet Dis. (2020) ; 12: (6). doi: 10.1177/1759720X20964139. |
[22] | Hall TM, Robinson KW, Fujinawa O, Akasaka K, Pyne EA. Intertester Reliability and Diagnostic Validity of the Cervical Flexion-Rotation Test. J Manipulative Physiol Ther. (2008) May; 31: (4): 293-300. doi: 10.1016/j.jmpt.2008.03.012. |
[23] | Luedtke K, Schoettker-Königer T, Hall T, Reimer C, Grassold M, Hasselhoff-Styhler P, et al. Erratum: Concurrent validity and reliability of measuring range of motion during the cervical flexion rotation test with a novel digital goniometer. BMC Musculoskelet Disord. (2020) ; 21: (535): 12891. doi: 10.1186/s12891-020-03525-6. |
[24] | Hall T, Robinson K. The flexion-rotation test and active cervical mobility – A comparative measurement study in cervicogenic headache. Man Ther. (2004) Nov; 9: (4): 197-202. doi: 10.1016/j.math.2004.04.004. |
[25] | Ogince M, Hall T, Robinson K, Blackmore AM. The diagnostic validity of the cervical flexion-rotation test in C1/2-related cervicogenic headache. Man Ther. (2007) ; 12: (3): 256-62. doi: 10.1016/j.math.2006.06.016. |
[26] | Dunning JR, Cleland JA, Waldrop MA, Arnot C, Young I, Turner M, et al. Upper Cervical and Upper Thoracic Thrust Manipulation Versus Nonthrust Mobilization in Patients With Mechanical Neck Pain: A Multicenter Randomized Clinical Trial. J Orthop Sport Phys Ther. (2012) Jan; 42: (1): 5-18. doi: 10.2519/jospt.2012.3894. |
[27] | Fm K, Kaltenborn FM. Manual Mobilization of the Joints: The Spine. Orthopedic Physical Therapy & Rehabilitation Produ. (2009) ; p. 336. |
[28] | Krauss JR, Evjenth O, Creighton D. TSM: translatoric spinal manipulation. Lakeview Media L.L.C.; (2006) , p. 133. |
[29] | Kaltenborn F, Evjenth O, Kaltenborn T, Morgan DVE. Manual Mobilization of the Joints. Volume I: Joint examination and basic treatment: the extremities, (2015) . |
[30] | Lantz CA, Chen JBD. Clinical validity and stability of active and passive cervical range of motion with regard to total and unilateral uniplanar motion. Spine (Phila Pa 1976). (1999) ; 24: (11): 1082-9. |
[31] | Williams MA, McCarthy CJ, Chorti A, Cooke MW, Gates S. A systematic review of reliability and validity studies of methods for measuring active and passive cervical range of motion. J Manipulative Physiol Ther. (2010) Feb; 33: (2): 138-55. doi: 10.1016/j.jmpt.2009.12.009. |
[32] | Florêncio LL, Pereira PA, Silva ERT, Pegoretti KS, Gonçalves MC, Bevilaqua-Grossi D. Agreement and reliability of two non-invasive methods for assessing cervical range of motion among young adults. Rev Bras Fisioter. (2010) ; 14: (2): 175-81. |
[33] | Tousignant M, Smeesters C, Breton A-M, Breton E, Corriveau H. Criterion validity study of the cervical range of motion (CROM) device for rotational range of motion on healthy adults. J Orthop Sports Phys Ther. (2006) Apr; 36: (4): 242-8. doi: 10.2519/jospt.2006.36.4.242. |
[34] | Audette I, Dumas J-P, Côté JN, De Serres SJ. Validity and between-day reliability of the cervical range of motion (CROM) device. J Orthop Sports Phys Ther. (2010) May; 40: (5): 318-23. doi: 10.2519/jospt.2010.3180. |
[35] | Strimpakos N. The assessment of the cervical spine. Part 1: Range of motion and proprioception. J Bodyw Mov Ther. (2011) ; 15: (1): 114-24. |
[36] | MacDermid JC, Evenhuis W, Louzon M. Inter-instrument reliability of pinch strength scores. J Hand Ther. (2001) Jan; 14: (1): 36-42. doi: 10.1016/S0894-1130(01)80023-5. |
[37] | Chung S, Jeong YG. Effects of the craniocervical flexion and isometric neck exercise compared in patients with chronic neck pain: A randomized controlled trial. Physiother Theory Pract. (2018) ; 34: (12): 916-25. doi: 10.1080/09593985.2018.1430876. |
[38] | Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates, (1988) . |
[39] | Hall T, Briffa K, Hopper D, Robinson K. Long-Term Stability and Minimal Detectable Change of the Cervical Flexion-Rotation Test. J Orthop Sport Phys Ther. (2010) Apr; 40: (4): 225-9. doi: 10.2519/jospt.2010.3100. |
[40] | Malo-Urriés M, Tricás-Moreno JM, Estébanez-de-Miguel E, Hidalgo-García C, Carrasco-Uribarren A, Cabanillas-Barea S. Immediate Effects of Upper Cervical Translatoric Mobilization on Cervical Mobility and Pressure Pain Threshold in Patients With Cervicogenic Headache: A Randomized Controlled Trial. J Manipulative Physiol Ther. (2017) Nov; 40: (9): 649-58. doi: 10.1016/j.jmpt.2017.07.007. |
[41] | Hidalgo-García C, Tricás-Moreno J, Giner-Nicolás R, Giménez-Donoso C, Gómez-Díaz A, San Gumersindo-Lacasa S. Manipulación cervical: aproximación anatómico-biomecánica frente a los posibles riesgos e implicaciones prácticas. Fisioterapia. (2007) ; 29: (6): 298-303. |
[42] | Bialosky JE, Beneciuk JM, Bishop MD, Coronado RA, Penza CW, Simon CB, et al. Unraveling the Mechanisms of Manual Therapy: Modeling an Approach. J Orthop Sports Phys Ther. (2018) Jan; 48: (1): 8-18. doi: 10.2519/jospt.2018.7476. |
[43] | Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. (2009) Oct; 14: (5): 531-8. doi: 10.1016/j.math.2008.09.001. |
[44] | Walton D, Macdermid J, Nielson W, Teasell R, Chiasson M, Brown L. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J Orthop Sports Phys Ther. (2011) ; 41: (9): 644-50. doi: 10.2519/jospt.2011.3666. |
[45] | Line B, Practice FOR. Neck Pain Guidelines: Revision 2017: Using the Evidence to Guide Physical Therapist Practice. J Orthop Sports Phys Ther. (2017) Jul; 47: (7): 511-2. doi: 10.2519/jospt.2017.0507. |
[46] | Gross A, Langevin P, Burnie SJ, Bédard-Brochu M-S, Empey B, Dugas E, et al. Manipulation and mobilisation for neck pain contrasted against an inactive control or another active treatment. Cochrane database Syst Rev. (2015) Sep; (9): CD004249. doi: 10.1002/14651858.CD004249.pub4. |
[47] | Sterling M, Jull G, Wright A. Cervical mobilisation: concurrent effects on pain, sympathetic nervous system activity and motor activity. Man Ther. (2001) May; 6: (2): 72-81. doi: 10.1054/math.2000.0378. |
[48] | Lluch E, Schomacher J, Gizzi L, Petzke F, Seegar D, Falla D. Immediate effects of active cranio-cervical flexion exercise versus passive mobilisation of the upper cervical spine on pain and performance on the cranio-cervical flexion test. Man Ther. (2014) ; 19: (1): 25-31. doi: 10.1016/j.math.2013.05.011. |
[49] | González Rueda V, López de Celis C, Barra López ME, Carrasco Uribarren A, Castillo Tomás S, Hidalgo García C. Effectiveness of a specific manual approach to the suboccipital region in patients with chronic mechanical neck pain and rotation deficit in the upper cervical spine: study protocol for a randomized controlled trial. BMC Musculoskelet Disord. (2017) Dec 5; 18: (1): 384. doi: 10.1186/s12891-017-1744-5. |
[50] | Jesus-Moraleida FR, Ferreira PH, Pereira LSM, Vasconcelos CM, Ferreira ML. Ultrasonographic analysis of the neck flexor muscles in patients with chronic neck pain and changes after cervical spine mobilization. J Manipulative Physiol Ther. (2011) Oct; 34: (8): 514-24. doi: 10.1016/j.jmpt.2011.08.006. |



