Abstract
Purpose
Over the last decade, advances in understanding the pathophysiology, clinical presentation, systemic consequences and treatment responses in obstructive sleep apnea (OSA) have made individualised OSA management plausible. As the first step in this direction, this study was undertaken to identify OSA phenotypes.
Methods
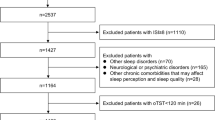
Patients diagnosed with OSA on level 1 polysomnography (PSG) were included. Clinical and co-morbidity profile, anthropometry and sleepiness scores were compiled. On PSG, apnea–hypopnea index, positional indices, sleep stages and desaturation indices (T90) were tabulated. Cluster analysis was performed to identify distinct phenotypes among included patients with OSA.
Results
One hundred patients (66 males) with a mean age of 49.5 ± 13.3 years were included. Snoring was reported by 94% subjects, and 50% were excessively sleepy. Two-thirds of subjects had co-morbidities, the most frequent being hypertension (55%) and dyslipidemia (53%). Severe OSA was diagnosed on PSG in 42%, while 29% each had mild and moderate OSA, respectively. On cluster analysis, 3 distinct clusters emerged. Cluster 1 consisted of older, obese subjects with no gender predilection, higher neck circumference, severe OSA with more co-morbidities and higher T90. Cluster 2 comprised of younger, less obese males with snoring, witnessed apnea, moderate and supine predominant OSA. Cluster 3 consisted of middle-aged, obese males with lesser co-morbidities, mild OSA and lower T90.
Conclusions
This study revealed three OSA clusters with distinct demographic, anthropometric and PSG features. Further research with bigger sample size and additional parameters may pave the way for characterising distinct phenotypes and individualising OSA management.


Similar content being viewed by others
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
Zinchuk A, Yaggi HK (2020) Phenotypic subtypes of OSA: a challenge and opportunity for precision medicine. Chest 157(2):403–420. https://doi.org/10.1016/j.chest.2019.09.002
Trzepizur W, Blanchard M, Ganem T, Balusson F, Feuilloy M, Girault JM et al (2022) Sleep apnea-specific hypoxic burden, symptom subtypes, and risk of cardiovascular events and all-cause mortality. Am J Respir Crit Care Med 205(1):108–117. https://doi.org/10.1164/rccm.202105-1274OC
Kushida CA, Nichols DA, Holmes TH, Quan SF, Walsh JK, Gottlieb DJ et al (2012) Effects of continuous positive airway pressure on neurocognitive function in obstructive sleep apnea patients: the apnea positive pressure long-term efficacy study (APPLES). Sleep 35(12):1593–1602. https://doi.org/10.5665/sleep.2226
McEvoy RD, Antic NA, Heeley E, Luo Y, Ou Q, Zhang X et al (2016) CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med 375(10):919–931. https://doi.org/10.1056/NEJMoa1606599
Malhotra A, Mesarwi O, Pepin JL, Owens RL (2020) Endotypes and phenotypes in obstructive sleep apnea. Curr Opin Pulm Med 26(6):609–614. https://doi.org/10.1097/MCP.0000000000000724
Ye L, Pien GW, Ratcliffe SJ, Björnsdottir E, Arnardottir ES, Pack AI, Benediktsdottir B, Gislason T (2014) The different clinical faces of obstructive sleep apnoea: a cluster analysis. Eur Respir J 44(6):1600–1607. https://doi.org/10.1183/09031936.00032314
Mazzotti DR, Keenan BT, Lim DC, Gottlieb DJ, Kim J, Pack AI (2019) Symptom subtypes of obstructive sleep apnea predict incidence of cardiovascular outcomes. Am J Respir Crit Care Med 200(4):493–506. https://doi.org/10.1164/rccm.201808-1509OC
Joosten SA, Hamza K, Sands S, Turton A, Berger P, Hamilton G (2012) Phenotypes of patients with mild to moderate obstructive sleep apnoea as confirmed by cluster analysis. Respirology 17(1):99–107. https://doi.org/10.1111/j.1440-1843.2011.02037.x
Babbin SF, Velicer WF, Aloia MS, Kushida CA (2015) Identifying longitudinal patterns for individuals and subgroups: an example with adherence to treatment for obstructive sleep apnea. Multivariate Behav Res 50(1):91–108. https://doi.org/10.1080/00273171.2014.958211
Lyons MM, Bhatt NY, Pack AI, Magalang UJ (2020) Global burden of sleep-disordered breathing and its implications. Respirology 25(7):690–702. https://doi.org/10.1111/resp.13838
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ et al (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7(8):687–698. https://doi.org/10.1016/S2213-2600(19)30198-5
Berry RB, Albertario CL, Harding SM et al (2020) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Version 2.6. Darien, IL: American Academy of Sleep Medicine
World Health Organization. Regional Office for the Western Pacific. The Asia-Pacific perspective: redefining obesity and its treatment [Internet]. Sydney: Health Communications Australia; 2000 [cited 2022 Mar 21]. 55 p. Available from: https://apps.who.int/iris/handle/10665/206936
Joshi SR, Anjana RM, Deepa M, Pradeepa R, Bhansali A, Dhandania VK et al (2014) ICMR-INDIAB Collaborative Study Group Prevalence of dyslipidemia in urban and rural India: the ICMR-INDIAB study. PLoS One 9(5):e96808. https://doi.org/10.1371/journal.pone.0096808
World Health Organization. Waist circumference and waist-hip ratio: report of a WHO expert consultation, Geneva, 8–11 December 2008. 2011 [cited 2022 Mar 21]; Available from: https://apps.who.int/iris/handle/10665/44583
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Knauert M, Naik S, Gillespie MB, Kryger M (2015) Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World J Otorhinolaryngol Head Neck Surg 1(1):17–27. https://doi.org/10.1016/j.wjorl.2015.08.001
Eckert DJ (2018) Phenotypic approaches to obstructive sleep apnoea – new pathways for targeted therapy. Sleep Med Rev 37:45–59. https://doi.org/10.1016/j.smrv.2016.12.003
Desai M, Oppenheimer J (2016) Elucidating asthma phenotypes and endotypes: progress towards personalized medicine. Ann Allergy Asthma Immunol 116(5):394–401. https://doi.org/10.1016/j.anai.2015.12.024
Brusselle GG, Koppelman GH (2022) Biologic therapies for severe asthma. N Engl J Med 386(2):157–171. https://doi.org/10.1056/NEJMra2032506
Bailly S, Destors M, Grillet Y, Richard P, Stach B, Vivodtzev I, Timsit JF, Lévy P, Tamisier R, Pépin JL (2016) Scientific council and investigators of the French national sleep apnea registry (OSFP) Obstructive sleep apnea: a cluster analysis at time of diagnosis. PLoS One 11(6):e0157318. https://doi.org/10.1371/journal.pone.0157318
Pien GW, Ye L, Keenan BT et al (2018) Changing faces of obstructive sleep apnea: treatment effects by cluster designation in the Icelandic Sleep Apnea Cohort. Sleep 1;41(3):zsx201. https://doi.org/10.1093/sleep/zsx201
Zinchuk AV, Jeon S, Koo BB, Yan X, Bravata DM, Qin L, Selim BJ, Strohl KP, Redeker NS, Concato J, Yaggi HK (2018) Polysomnographic phenotypes and their cardiovascular implications in obstructive sleep apnoea. Thorax 73(5):472–480. https://doi.org/10.1136/thoraxjnl-2017-210431
Azarbarzin A, Sands SA, Stone KL, Taranto-Montemurro L, Messineo L, Terrill PI, Ancoli-Israel S, Ensrud K, Purcell S, White DP, Redline S, Wellman A (2019) The hypoxic burden of sleep apnoea predicts cardiovascular disease-related mortality: the Osteoporotic Fractures in Men Study and the Sleep Heart Health Study. Eur Heart J 40(14):1149–1157. https://doi.org/10.1093/eurheartj/ehy624
Kitakata H, Kohno T, Fukuda K (2018) Sleep-disordered breathing in the elderly: is it distinct from that in the younger or middle-aged populations? J Thorac Dis 10(Suppl 9):S1102–S1107. https://doi.org/10.21037/jtd.2018.03.179
Joosten SA, O’Driscoll DM, Berger PJ, Hamilton GS (2014) Supine position related obstructive sleep apnea in adults: pathogenesis and treatment. Sleep Med Rev 18(1):7–17. https://doi.org/10.1016/j.smrv.2013.01.005
Kim KT, Cho YW, Kim DE, Hwang SH, Song ML, Motamedi GK (2016) Two subtypes of positional obstructive sleep apnea: supine-predominant and supine-isolated. Clin Neurophysiol 127(1):565–570. https://doi.org/10.1016/j.clinph.2015.06.009
Oksenberg A, Silverberg DS, Arons E, Radwan H (1997) Positional vs nonpositional obstructive sleep apnea patients: anthropomorphic, nocturnal polysomnographic, and multiple sleep latency test data. Chest 112(3):629–639. https://doi.org/10.1378/chest.112.3.629
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study has been approved by the Institutional Ethics Committee of St. John’s Medical College and Hospital, Bangalore, India (Protocol no. 138/2019). The study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All patients involved in the study have given informed consent prior to their inclusion in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Venkatnarayan, K., Krishnaswamy, U.M., Rajamuri, N.K.R. et al. Identifying phenotypes of obstructive sleep apnea using cluster analysis. Sleep Breath 27, 879–886 (2023). https://doi.org/10.1007/s11325-022-02683-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02683-2