Abstract
Summary
The association between socioeconomic status (SES) and bone mineral density (BMD) in men remains controversial. We showed that SES was positively associated with BMD in American men. Confounding factors like race/ethnicity and age could affect the association.
Introduction
Based on the data from the National Health and Nutrition Examination Survey (NHANES), 2011–2020, this article aims to investigate the association of SES (poverty income ratio (PIR) and education level) with the BMD in American men.
Methods
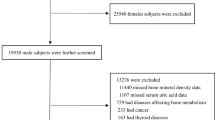
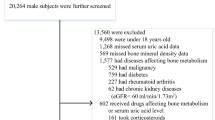
We evaluated the association of SES with BMD in 4446 men aged ≥ 20 years (mean age, 41.0 ± 13.4 years) from the NHANES 2011–2020. BMD was measured by dual-energy X-ray absorptiometry (DXA) at the lumbar spine. We used multivariate linear regression models to examine the relationship between SES and total spine BMD, adjusted for a large range of confounding factors.
Results
Compared with other PIR quarters, individuals in the highest quarter of PIR were more likely to be older and white and had fewer smoking or drinking behaviors. After adjusting for race/ethnicity, age, drinking and smoking behavior, body mass index (BMI), total protein, serum calcium, serum uric acid, cholesterol, serum phosphorus, and blood urea nitrogen, PIR was positively correlated with total spine BMD (β = 0.004 95% CI: 0.001–0.007, P = 0.006). Individuals with the highest degree (college degree or above) had a 0.057 g/cm2 greater BMD than that of the lowest degree (less than 9th grade) (β = 0.057 95% CI: 0.037–0.077, P < 0.001).
Conclusions
Our study indicates that SES was positively associated with the lumbar BMD among American men. Clinicians, healthcare providers, and policymakers should consider the unequal SES of men when implementing osteoporosis prevention and treatment strategies.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available in the supplementary material of this article.
Code availability
Not applicable.
References
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Hernlund E, Svedbom A, Ivergård M, et al. (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136
Reginster JY, Burlet N (2006) Osteoporosis: a still increasing prevalence. Bone 38:S4-9
Mustapha A, Ssekasanvu J, Chen I et al (2022) Hypertension and socioeconomic status in south central Uganda: a population-based cohort study. Glob Heart 17:3
Hawkins Carranza F, Corbatón-Anchuelo A, Bermejo Pareja F et al (2022) Incidence of type 2 diabetes in the elderly in Central Spain: association with socioeconomic status, educational level, and other risk factors. Prim Care Diabetes 16(2):279–286
Valentin G, Ravn MB, Jensen EK et al (2021) Socio-economic inequalities in fragility fracture incidence: a systematic review and meta-analysis of 61 observational studies. Osteoporos Int 32:2433–2448
Valentin G, Pedersen SE, Christensen R et al (2020) Socio-economic inequalities in fragility fracture outcomes: a systematic review and meta-analysis of prognostic observational studies. Osteoporos Int 31:31–42
Brennan SL, Winzenberg TM, Pasco JA, Wluka AE, Dobbins AG, Jones G (2013) Social disadvantage, bone mineral density and vertebral wedge deformities in the Tasmanian older adult cohort. Osteoporos Int 24:1909–1916
Hsieh CH, Wang CY, McCubbin M, Zhang S, Inouye J (2008) Factors influencing osteoporosis preventive behaviours: testing a path model. J Adv Nurs 62:336–345
Hernandez-Rauda R, Martinez-Garcia S (2004) Osteoporosis-related life habits and knowledge about osteoporosis among women in El Salvador: a cross-sectional study. BMC Musculoskelet Disord 5:29
Song SY, Kim Y, Park H, Kim YJ, Kang W, Kim EY (2017) Effect of parity on bone mineral density: a systematic review and meta-analysis. Bone 101:70–76
Lins Vieira NF, da Silva Nascimento J, do Nascimento CQ, Barros Neto JA, Oliveira Dos Santo ACS (2021) Association between bone mineral density and nutritional status, body composition and bone metabolism in older adults. J Nutr Health Aging 25:71–76
Wang MC, Dixon LB (2006) Socioeconomic influences on bone health in postmenopausal women: findings from NHANES III, 1988–1994. Osteoporos Int 17:91–98
Du Y, Zhao LJ, Xu Q, Wu KH, Deng HW (2017) Socioeconomic status and bone mineral density in adults by race/ethnicity and gender: the Louisiana osteoporosis study. Osteoporos Int 28:1699–1709
Elliot JR, Gilchrist NL, Wells JE (1996) The effect of socioeconomic status on bone density in a male Caucasian population. Bone 18:371–373
Myong JP, Kim HR, Choi SE, Koo JW (2012) The effect of socioeconomic position on bone health among Koreans by gender and menopausal status. Calcif Tissue Int 90:488–495
Nabipour I, Cumming R, Handelsman DJ et al (2011) Socioeconomic status and bone health in community-dwelling older men: the CHAMP study. Osteoporos Int 22:1343–1353
Araujo AB, Yang M, Suarez EA et al (2014) Racial/ethnic and socioeconomic differences in bone loss among men. J Bone Miner Res 29:2552–2560
Loucks EB, Rehkopf DH, Thurston RC, Kawachi I (2007) Socioeconomic disparities in metabolic syndrome differ by gender: evidence from NHANES III. Ann Epidemiol 17:19–26
Suresh S, Sabanayagam C, Shankar A (2011) Socioeconomic status, self-rated health, and mortality in a multiethnic sample of US adults. J Epidemiol 21:337–345
Lane NE (2006) Epidemiology, etiology, and diagnosis of osteoporosis. Am J Obstet Gynecol 194:S3-11
Akkus Z, Camdeviren H, Celik F, Gur A, Nas K (2005) Determination of osteoporosis risk factors using a multiple logistic regression model in postmenopausal Turkish women. Saudi Med J 26:1351–1359
Gur A, Sarac AJ, Nas K, Cevik R (2004) The relationship between educational level and bone mineral density in postmenopausal women. BMC Fam Pract 5:18
Guadalupe-Grau A, Fuentes T, Guerra B, Calbet JA (2009) Exercise and bone mass in adults. Sports Med 39:439–468
Brennan SL, Henry MJ, Wluka AE, Nicholson GC, Kotowicz MA, Pasco JA (2010) Socioeconomic status and bone mineral density in a population-based sample of men. Bone 46:993–999
del Rio BL, RomeraBaures M, Pavia Segura J et al (1992) Bone mineral density in two different socio-economic population groups. Bone Miner 18:159–168
Xu X, Liu L, Sharma M, Zhao Y (2015) Smoking-related knowledge, attitudes, behaviors, smoking cessation idea and education level among young adult male smokers in Chongqing, China. Int J Environ Res Public Health 12:2135–2149
Mullen PD, Simons-Morton DG, Ramírez G, Frankowski RF, Green LW, Mains DA (1997) A meta-analysis of trials evaluating patient education and counseling for three groups of preventive health behaviors. Patient Educ Couns 32:157–173
Macgregor CB, Meerkin JD, Alley SJ, Vandelanotte C, Reaburn PJ (2018) Osteoporosis and low bone mineral density (osteopenia) in rural and remote Queensland. Aust J Rural Health 26:369–374
Wastesson JW, RingbäckWeitoft G, Parker MG, Johnell K (2013) Educational level and use of osteoporosis drugs in elderly men and women: a Swedish nationwide register-based study. Osteoporos Int 24:433–442
Arabi A, Nabulsi M, Maalouf J et al (2004) Bone mineral density by age, gender, pubertal stages, and socioeconomic status in healthy Lebanese children and adolescents. Bone 35:1169–1179
Crandall CJ, Merkin SS, Seeman TE, Greendale GA, Binkley N, Karlamangla AS (2012) Socioeconomic status over the life-course and adult bone mineral density: the Midlife in the U.S. Study. Bone 51:107–13
Crandall CJ, Miller-Martinez D, Greendale GA, Binkley N, Seeman TE, Karlamangla AS (2012) Socioeconomic status, race, and bone turnover in the Midlife in the US Study. Osteoporos Int 23:1503–1512
Nam HS, Shin MH, Zmuda JM et al (2010) Race/ethnic differences in bone mineral densities in older men. Osteoporos Int 21:2115–2123
Conradie M, Conradie MM, Kidd M, Hough S (2014) Bone density in black and white South African women: contribution of ethnicity, body weight and lifestyle. Arch Osteoporos 9:193
Ho SC, Chen YM, Woo JL (2005) Educational level and osteoporosis risk in postmenopausal Chinese women. Am J Epidemiol 161:680–690
Allali F, Rostom S, Bennani L, Abouqal R, Hajjaj-Hassouni N (2010) Educational level and osteoporosis risk in postmenopausal Moroccan women: a classification tree analysis. Clin Rheumatol 29:1269–1275
Yu CX, Zhang XZ, Zhang K, Tang Z (2015) A cross-sectional study for estimation of associations between education level and osteoporosis in a Chinese men sample. BMC Musculoskelet Disord 16:382
Acknowledgements
We acknowledge the data from the National Health and Nutrition Examination Survey (NHANES).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the ethics review board of the National Center for Health Statistics.
Consent to participate
Written consent was obtained from each participant.
Consent for publication
Not applicable.
Conflict of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xiao, PL., Fuerwa, C., Hsu, CJ. et al. Socioeconomic status influences on bone mineral density in American men: findings from NHANES 2011–2020. Osteoporos Int 33, 2347–2355 (2022). https://doi.org/10.1007/s00198-022-06498-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06498-5