Abstract
In this study, we developed green composites made of homogenized-bacterial cellulose, that is, gelatin containing different concentrations of mangosteen extract using tannin as a natural crosslinker. The films were fabricated using a fast and simple casting method. Scanning electron microscopy (SEM) micrographs showed uniform morphology. The water vapor permeability of the films ranged from 628 to 976 g/m2/day, which was comparable to commercial dressings. The fluid uptake ability ranged between 250 and 390%. All films in hydrated state were flexible, stable, and capable of bearing force. Furthermore, films containing the mangosteen extract had good stability, were well-embedded in the bacteria cellulose-based matrix, and could retain its bioactivity. The fabricated film exhibited good antibacterial property against S. aereus and E. coli upon direct contact according to the surface method test (JIS Z 2801), which become comparable to commercial tulle dressing. Films were nontoxic to human keratinocytes (HaCat) and human gingival fibroblasts (GF). Films exhibited anticancer properties against human oral cancer cells (CAL27). Bacterial cellulose pellicles were mechanically disintegrated into fibrils suspension and then reconstructed with the incorporation of gelatin and mangosteen extract. The novel biocomposites were created with improved antibacterial and anticancer properties. Our findings suggest that the biocomposites from bacterial cellulose, gelatin incorporated with mangosteen extract, could be an intriguing option for further research as the daily and single-use direct contact film for the treatment of skin wounds, gingivitis, periodontitis, and oral cancer.
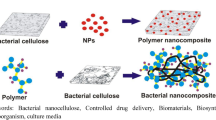
Graphical abstract

Similar content being viewed by others
Introduction
Bacterial cellulose (BC) is the cellulose produced by bacteria. Its molecular formula and polymeric structure are identical to the cellulose produced by plants. The absence of hemicelluloses, pectin, and lignin, reduces the effort of further purification (Ruan et al. 2016). BC has a gel-like fibril network, which possess high water-holding capacity, mechanical strength, and biocompatibility. A number of studies on BC-based composites have been reported as alternative biomaterials for biomedical approaches (Ullah et al. 2017; Bayir et al. 2019; Zhang et al. 2020a, b; Unal et al. 2021). Furthermore, BC is mostly used in hydrogel (never-dried state) form. Dehydration affects BC properties. It could lead to loss of dehydration and elasticity with intense shrinkage (Rebelo et al. 2018). This limits its application to meeting desirable properties. BC has been modified by different methods in situ and ex situ. However, these modifications are limited by the amounts, concentrations, and types of additives or reinforcement agents (Wang et al. 2011; Ma et al. 2014). Homogenization could turn BC into gel suspension form. This can be an alternative for producing BC-composites on the large scale through standard manufacturing and high-volume production. Furthermore, BC suspension is easy to combine with other additives, and the proportion of the film component could be accurately controlled (Azeredo et al. 2019). Shorten BC fibrils could also act as reinforcing agents and support matrix in the composites. Gelatin (G), a natural protein derived from the hydrolysis of native collagen, possesses many attractive properties, including biocompatibility, gel-forming ability, water solubility, and low antigenicity. It has been widely used in pharmaceutical and medical fields (Naskar et al. 2015; Yao et al. 2020). Gelatin is also suitable as a binder for biomaterials in soft tissue engineering (Kakkar et al. 2014). To improve gelatin stability for broader applications, it is necessary to stabilize it by crosslinking. Glutaraldehyde has been commonly used for gelatin crosslinking. However, it is toxic to humans (Gough et al. 2002; Takigawa and Endo 2006). Tannin (T) is an alternative natural crosslinker. It is derived from plants such as green tea leaves. Tannin is a phenolic compound. It has been documented for its interactions with proteins (Tavassoli-Kafrani et al. 2017; Zhang et al. 2010). Mangosteen (Garcinia mangostana) is a tropical tree native to Southeast Asian countries. It is widely grown in Thailand. The mangosteen extract (M) is a polyphenol, meaning it is insoluble in water. It has been well-documented in various in vitro and in vivo studies that mangosteen extract has substantial, antimicrobial, anti-inflammatory, anti-oxidant, and anticancer properties (Aisha et al. 2012; Scolamiero et al. 2018). Natural antimicrobial agents are safe to human health showing low adverse effects and drug resistance. Recent studies have reported on loading mangosteen extract into biopolymers. The mangosteen-loaded fibroin and poly(ethylenimine) nanoparticles were found as promising in ulcerative colitis treatment (Pham et al. 2020). Sustained release of mangosteen extract loaded in chitosan-carrageenan nanoparticles had the cytotoxicity against breast cancer cells (Wathoni et al. 2021). Phosphorylated collagen–mangosteen extract scaffolds showed potential in bone tissue engineering (Milan et al. 2021). To date, a facile, practical method is needed, and there are only few available reports on biocomposite obtained from BC incorporating mangosteen extract.
This work aimed to fabricate and characterize homogenized BC and gelatin composites containing mangosteen extract. The composites were fabricated via facile casting method, directly loading different concentrations of the extract and tannin crosslinking. The microstructure, Fourier transform infrared spectroscopy (FTIR), mechanical properties, fluid uptake ability, surface wettability, preliminary antimicrobial activity, and in vitro cell studies were evaluated to lay a foundation on tuning the properties of these hybrid biocomposites.
Materials and methods
Materials
BC hydrogel pellicles (size 1 cm × 1 cm × 1 cm) were supplied by the Institute of Research and Development of Food Product (Kasetsart University, Thailand). Gelatin (type A, 180 bloom) was purchased from Sigma-Aldrich, USA. Sorbitol was purchased from Ajax Finechem, Australia. Mangosteen ethanolic extract and tannin were purchased from the Specialty Natural Products Company, Thailand. All chemicals were used as received without further purification.
Preparation of bacterial cellulose-gelatin incorporating mangosteen extract films
To prepare BC slurry, BC pellicles were crushed thoroughly and homogenized using a blender (HR2096, Philips, China) at 1200 rpm for 5 min. The size of homogenized BC fibers was around 1–1.5 µm, with the average particle size of 1.25 µm (evaluated by using the laser particle size distribution analyzer, Mastersizer 3000, Malvern, UK).
BC slurry (~ 1% fiber content) was thoroughly mixed with the gelatin solution (15% w/w) at the weight ratio of 60:40 and sorbitol (2 g per 10 g of gelatin solution) for 1 h until the homogeneous mixture was formed. The different concentrations of mangosteen extract of 1%, 5%, and 10% w/w were added into the mixtures and were then gently stirred, and the tannin (10 mg per 1 g of gelatin solution) was added and stirred for 3 h. Homogeneous mixtures were poured into a polystyrene petridish 10 cm in diameter (50 g per plate) and air-dried at ambient temperature overnight. The bacterial cellulose/gelatin (BCG) films incorporating mangosteen extract films were then carefully peeled off and kept in the airtight container prior use. BCG-M0, BCG-M1, BCG-M5, and BCG-M10 represented BCG with a 0%, 1%, 5%, and 10% w/w concentration of mangosteen extract, respectively.
The actual content of the mangostin, the major component of mangosteen extract in each film, was analyzed by spectrophotometry. Film samples (size 2 cm × 2 cm) were immersed in 20 ml of absolute ethanol under continuous shaking at 100 rpm at room temperature for 24 h. The supernatant was then collected, and the mangostin content was measured by spectrophotometer (Shimadzu UV-2550, Japan) at the wavelength of 320 nm (Pothitirat et al. 2009; Ahmad et al. 2013). The mangostin content was calculated from the standard curve of mangostin prepared at six known concentrations (n = 6) (Fig. S1). BCG-M0, BCG-M1, BCG-M5, and BCG-M10 containing mangostin at 0, 18.15 ± 0.27, 127.26 ± 0.36, and 237.47 ± 0.4 mg/cm3, respectively.
Morphology
The morphology of the surface and cross-section of the films were visualized using Scanning electron microscope (SEM; JSM-6610LV, JEOL, Japan) at an acceleration voltage of 10 kV. Samples were cryo-fractured by immersion in liquid nitrogen. For films in reswollen form, hydrated films were dehydrated in ethanol (ascending grade) and dried in a critical point dryer (Samdri 780-A, Tousimis, USA), where liquid carbon dioxide was used as a transitional medium. Samples were then mounted on the brass stub and sputtered with gold by sputter coater (Balzers-SCD 040, Balzers, Liechtenstein). Photographs were taken for morphology analysis.
Fourier transform infrared spectroscopy (FTIR)
The chemical structure of the films was analyzed by FTIR spectrometer (Spectrum One, PerkinElmer, USA). Samples were crushed and mixed with potassium bromide (KBr) into pellets and then characterized in the wavelength range of 400–4000 cm−1, at a resolution of 4 cm−1 for 50 scans.
Fluid uptake ability
The dry films 2 cm × 2 cm in size were weighed to find initial weight (W0). The films were then immersed in PBS for 6 and 24 h. The immersed films were then retrieved. Excess fluid on the film surface was blotted out by Kimwipes® paper, and the weight of samples were determined (Wt). The tests were done in triplicate. The fluid uptake ability was calculated as followed:
Water vapor transmission rate (WVTR)
The water vapor transmission rate (WVTR) of samples was determined by the water vapor permeability analyzer, PERMETRAN-W® model 398 (Mocon, USA) following ASTM E96 at 37 °C and 75% relative humidity. The samples were sealed to the open mount of test dish containing a desiccant, and the assembly was placed in a controlled atmosphere. The WVTR was determined as weight of the transmitted water vapor per surface area of the sample per 24 h.
Surface wettability
The water-contact-angle measurement was performed to evaluate the wettability of films. The contact angle of water droplets was measured using a contact angle analyzer OCA-20 (Dataphysics, Germany). Samples were then placed on the platform of the analyzer just below the needle, from which a 2-μL water droplet was dispensed from the micro needle, and the contact angle was measured in degrees using the SCA20 software. Measurements were done at least five different points for each sample.
Mechanical properties
Mechanical tests of dry and wet films were performed at room temperature. Samples were cut into strip (1 cm wide and 10 cm long). Tensile strength (TS), elongation at break (EB), and Young's modulus (YS) of the samples were measured according to ASTM D882 using an Universal Testing Machine (8872, INSTRON, USA). For wet test, the samples were pre-soaked in PBS for 24 h. Following the removal of excess PBS by Kimwipes® paper, the samples were tested. The data were reported as average values from at least six replicates.
Antibacterial testing
The antibacterial activity of fabricated films, as well as commercial tulle dressing, was assessed using the surface method according to Japanese International Standard, JIS Z 2801 (Kawakami et al. 2008). Films were tested against Staphylococcus aureus (S. aureus) ATCC 25,923 (representative Gram-positive bacteria) and Escherichia coli (E. coli) ATCC 25,922 (representative Gram-negative bacteria). Films were cut into 5 cm × 5 cm and placed on sterilized petridish. In brief, bacteria were suspended in nutrient broth medium. The bacteria suspension was dropped on the surface of each sample. The initial concentration of S. aureus and E. coli for each sample was 6.21 ± 0.04 and 6.02 ± 0.03 Log CFU/ml, respectively. Films were then subsequently incubated for 24 h at 37 °C. Following 24 h of incubation, the number of viable bacteria on surface samples were counted by the standard agar plate colony counting method. The images of agar plates were then taken. The experiments were done in triplicate.
Cell studies
Three different cells, human keratinocytes (HaCat), human gingival fibroblasts (GF), and oral cancer cells (CAL27, ATCC® CRL-2095™) were used for in vitro cell studies as a direct contact culture. HaCat cells were supplied from CLS-Cell lines services, Germany. GF cells were isolated from orthodontic teeth extracted from healthy young volunteers with an approval from the Ethics Committee of the Faculty of Dentistry, Chulalongkorn University, Thailand (study code: HREC-DCU 2012-079).
All cell types were cultured in Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% v/v Fetal Bovine Serum (FBS) and 1% of antibiotics in a humidified 37 °C incubator containing 5% (v/v) CO2. The sterilized films (16 mm in diameter) were placed in 24-well plates. Cell suspension was dropped onto each film with the cell-seeding density 5 × 104 cells per well and incubated at 37 °C in a humidified atmosphere composed of 5% CO2 for 24 h. Cells cultured on coverslips were served as control groups. The relative cell viability was evaluated by the MTT assay in accordance with ISO10993-5. Briefly, after 24 h of incubation, the medium was removed, and the MTT solution was added. Quantitative analysis of cell viability was assessed using the microplate reader (Multiskan, Thermo Scientific, USA) at the wavelength of 570 nm. The viability was normalized by the absorbance of each cell type cultured on coverslips for 24 h, which was expressed as 100% viability. All experiments were done in triplicate.
Cell morphology was observed using SEM. After 24 h of incubation, films were washed with PBS and fixed in 2.5% vol. fixative solution. They were dehydrated in serial dilutions of ethanol and dried in an automated Leica EM-CPD300 critical point dryer (Leica Microsystems, Austria). Samples were then sputter-coated with gold and observed under a JSM-5410 SEM (JEOL, Tokyo, Japan).
Statistical analysis
Quantitative data were presented as mean ± the standard deviation (SD) and obtained from at least three independent experiments. All data were analyzed using Minitab 17 software. Error bars represented SD. P values < 0.05 were considered statistically significant.
Results and discussions
Morphology
The morphology of the films was analyzed using SEM, and all films exhibited homogeneous morphology with no sign of phase separation or aggregation with a hint of roughness (Fig. 1). This inferred the good dispersion in the matrix. Gelatin could serve as a good binder to assist the dispersion of BC fibrils and mangosteen extract in the matrix, leading to homogeneous suspension. The homogeneous matrix of film surface without pores and cracks could also infer the structural integrity. SEM images of fracture cross-sectional of the films are illustrated in Fig. 2. Some dents were observed. BC fibrils were clearly observable in the BCG-M0 film. The dense structure of BCG-M1, BCG-M5, and BCG-M10 were visible. The film surface morphology in reswollen state was shown in Fig. 3. All films showed a uniform fibril network structure. This implied a good incorporation of mangosteen extract into the matrix. Significant macrostructural differences of film surface were not observed in this study.
Fourier transform infrared spectroscopy (FTIR)
The functional groups of the fabricated films were characterized through FTIR. FTIR spectra are presented in Fig. 4. In the case of pure BC, the broad adsorption bands at 3392 cm−1 were designated to the stretching frequency of the –OH group, as well as to the intramolecular and intermolecular hydrogen bonds (Andrade et al. 2019). The band around 2900 cm−1 represented C–H stretching and –CH2 asymmetric stretching vibrations (Andrade et al. 2019; Xiaorui et al. 2022). The band at 1647 cm−1 indicated the H–O–H bending of the absorbed water (Wahid et al. 2019). The band at 1061 cm−1 was a result of the presence of C–O–C stretching vibrations (Barud et al. 2011; Xiaorui et al. 2022). The band around 890 cm−1 represented typical β-1, 4-glycosidic linkages (Quan et al. 2020). The mains bands observed for gelatin were the partially overlapped stretching vibrations of O–H and N–H groups (3408 cm−1); amide I bands originated from C=O stretching vibration coupled to N–H vibration (1643 cm−1); amide II bands arose from the N–H bending vibrations, coupled to C–N stretching vibrations (1535 cm−1); the peak of amide III was attributed to vibration in the plane of C-N and N–H groups of bound amides (Muyonga et al. 2004; Sharahi et al. 2021; Min et al. 2022). Tannin displayed characteristic common bands. The broad adsorption band at 3408 cm−1 for O–H stretching vibration, 1710 cm−1 for C=O stretching, 1615 cm−1 for aromatic ring stretch vibrations, and 1200 cm−1 for C–O bond stretching vibration (Falcão et al. 2013). FTIR spectra of mangosteen extract showed main adsorption peaks of O–H stretching (3370 cm−1), C–H asymmetric stretching vibration (2923 cm−1), stretching vibration of unconjugated carbonyl (C=O) groups (1736 cm−1), and C–O stretching (1108 cm−1) (Aminah et al. 2014; Lee et al. 2016; Rohman et al. 2020; Zhang et al. 2020a, b). BC and gelatin bonded together and formed BC-gelatin composites via physical intermolecular hydrogen bonds (Ye et al. 2019). Cellulose, tannin, and plasticizer formed intermolecular hydrogen bonds (Zhou et al. 2016).
For BCG-M0, BCG-M1, BCG-M5, and BCG-M10, we observed the main characteristics peaks of both BC and gelatin. The saccharide structure caused the peaks in the range between 896 and 1060 cm−1 (Murali et al. 2019). The composites showed protein specific N–H bending (Unal et al. 2021). The single broad adsorption bands of hydrogen-bonded O–H stretching vibration were at around 3352–3412 cm−1 (Unal et al. 2021). Compared to pure BC, C–O–C stretching vibration peaks of each composite were slightly shifted toward the lower wavenumber (1059–1060 cm−1). Furthermore, the bands at 1200 and 1710 cm−1 of tannin and at 1736 cm−1 of mangosteen extract were not clearly noticeable in all fabricated films. These could attribute to strong hydrogen bonding among parental components. These also implied the formation of complexes. Proteins were bonded and formed complexes with polysaccharide and polyphenols (Taheri et al. 2020). The plausible explanations of polyphenols-protein complexes could be the interactions between phenolic and amino groups of protein chains. Simultaneously, hydrogen bonding between hydrophobic sites of proteins such as pyrrolidine rings assisted in the stabilization of complexes (Ghahri et al. 2017; Jordan et al. 2018). Findings reported that tannin could form strong hydrogen bonds with proteins (Lu et al. 2020). C–H stretching bands of mangosteen extract were observed along with the slight shifting in wavenumber (2926–2932 cm−1) in all mangosteen extract-loaded films. This confirmed the presence of mangosteen extract in composites. It was proposed that the interaction between protein and mangosteen extract attributed to hydrogen bonds and hydrophobic interactions (Zhou et al. 2021). The intensity of the bands depended on the concentration of mangosteen extract, which was caused by intermolecular hydrogen bonds formed between the hydroxyl groups of polyphenols and hydroxyl/amino groups (Valdés et al. 2019; Zhang et al. 2020a, b). This confirmed the presence of mangosteen extract in the composite films. Small shifts and intensity changes were noticed, which could be due to some modifications leading to small variations of rotation and vibration frequencies via hydrogen bonds. Furthermore, hydrophobic interaction was established between the hydrophobic groups of polyphenols and the NH2 groups of gelatin (Hoque et al. 2010). The functional groups of cellulose and polyphenols could also act as hydrogen donors promoting the formation of hydrogen bonds between the individual fibers (Nagarajan et al. 2015). Various studies were also reported for the biopolymers loaded with phenolic compounds. They proposed the intermolecular interaction (hydrogen bonds and electrostatic interactions) within the film matrix (Correa-Pacheco et al. 2019; Yong et al. 2020). It was also proposed that interactions between biopolymers and tannin under ambient temperature were hydrogen and electrostatic bonds (Aadil et al. 2016; Liu et al. 2017).
Fluid uptake ability
Fluid uptake ability was in the range of 250–390% (Fig. 5). The film without mangosteen extract showed the fluid uptake ability at around 390% following 24 h of PBS immersion (simulate clinical conditions), while those incorporating mangosteen extract had a lower percentage of fluid uptake ability. The addition of mangosteen extract reduced the fluid uptake ability in a concentration-dependent manner attributable to hydrophobic property of tannin and mangosteen extract. The less fluid absorption was due to strong interactions among polyphenol-rich compounds and biopolymer chains. These interactions would reduce the film water affinity (Chang-Bravo et al. 2014). Following fluid absorption capacity tests, all films could maintain their integrities throughout the immersion period. Fluid uptake ability is one of the important aspects for wound care. The moisture balance is essential to promote healing. Effective wound dressings are supposed to maintain moisture at the wound site while removing exudates. In a study of absorption capacity of a super absorbent dressing, the absorption capacity was in the range of 50–220% (Cutting and Westgate 2012). The fluid uptake ability was found between 250 and 390%, comparable with those of the commercial dressings.
Water vapor transmission rate (WVTR)
The WVTR in this work was in the range of 628–976 g/m2/day (Fig. 6). The WVTR values tended to decrease with the increasing mangosteen extract concentration. This finding was similar to previous studies (Bodini et al. 2013; De Araújo et al. 2015). This was because the hydrophobic property of polyphenols could form interactions within film matrix and reduce hygroscopicity of the films. The addition of polyphenols lowered the void space within the film matrix that permits water vapor to pass. Dressings in biomedical application are supposed to maintain moist environment, allowing moisture vapor and atmospheric gases exchange between wounded tissues and surroundings. Dressings also protect the wound from bacteria or viruses, keep the wound comfortable, and help the healing process. The high WVTR could dehydrate wound, whereas the low WVTR could cause the wound exudate accumulation. The WVTR of intact human skin ranged between 240 and 1920 g/m2/day, whereas the uncover wound could be in the order of 4800 g/m2/day (Nangia et al. 1989). The WVTR of commercial hydrocolloid dressing and films were in the range of 394–1000 g/m2/day (Wu et al. 1995; Wlaschin et al. 2019). It has been reported that the wound sites dressed with the moderate WVTR dressings (600–900 g/m2/day) healed faster in rat model studies (Yusof et al. 2003; Ahi et al. 2019). The WVTR values in this study were in compliance with the previous reports.
Surface wettability
Film wettability can be described by contact angle between liquid and film surface. In this study, water contact angles were in the range between 49° and 69° (Fig. 7.) The water contact angle appeared to slightly increase along with the concentration of mangosteen extract. The addition of hydrophobic mangosteen extract could reduce the hydrophilicity of films. Various studies reported that the sufficient contact angle for mucoadhesive patches were in the range between 45° and 65°, showing that films could specifically bind or adhere to mucus (Rojewska et al. 2019; Stie et al. 2020). Within these ranges of contact angles, fluid could provide an adequate spread and the vacuum was formed between material and surface. Surface wettability is known to allow protein adherence, cell attachment, and cell proliferation. The appropriate water contact-angle range for cell adhesion and wound-healing processes is 40°–70°, which is considered as moderate hydrophilic (Unnithan et al. 2015). The water contact-angle values achieved in this study are in compliance with the aforementioned requirements.
Mechanical properties
The mechanical properties of dry and hydrated films are shown in Fig. 8A–F. TS and EB of dry films are in the range of 130–179 MPa, 2.6–4.2%, respectively, inferring that the addition of mangosteen extract could slightly reduce mechanical properties in a concentration-dependent manner. Polyphenols could form strong intermolecular interactions among biopolymer chains. This could restrict the orientation of the matrix during film formation. The dispersed polyphenol compounds could lead discontinuities within the matrix, leading to the reduction of film resistance (Chang-Bravo et al. 2014; Valdés et al. 2019). Mechanical properties of films in the hydrated state are practically important in clinical use. Thus, for hydrated films, TS, EB and YS were in the range between 1.8 and 2.5 MPa, 46.7–50.2% and 3.6–5.7 MPa, respectively. Hydrated films were found to be more flexible compared to those of dry films. It was proposed that water was able to behave as plasticizers, clusters of water molecules filled voids in the biopolymeric matrix, resulting in the increase of the ductility (Olivas et al. 2008; Jost et al. 2014; Wu et al. 2014). TS inferred the ability of films to bear forces without damage during fabrication and handling. EB referred to how much films could be stretched before rupture. The optimum TS range for wound dressing and skin cell culture is 0.8–18 MPa (Elsner et al. 2010; Gomes et al. 2015; Yu et al. 2016). EB in the range of 40%–60% was reported to be a sufficient flexibility and accelerated wound-healing processes in rat model (Zaman et al. 2011; Kumar et al. 2013; Qu et al. 2018; Goncalves et al. 2020). TS and EB values in this work were found to match the aforementioned range. The YS of human skin appeared in the range of 4.6–20 MPa (Genevro et al. 2019). YS values in this work were also comparable to human skin and buccal mucosa (Silver et al. 2001; Chen et al. 2015; Choi et al. 2020).
Antibacterial testing
For antibacterial activity testing, the fabricated films were studied, and commercial tulle dressing (Sofra-tulle®) was used as a control. The number of living bacterial cells was counted after 24 h of incubation (Fig. 9A). Disk diffusion is the method based on the release of antimicrobial substances from the films into agar, resulting in a microbial inhibition zone around the films. In this study, inhibition zones were not observed for all fabricated films for both bacteria (data not shown). Similar findings have been reported by other studies for protein films incorporating plant polyphenols (Salgado et al. 2012; Musso et al. 2017, 2019). For this reason, the mangosteen extract may be restrained within the films. In addition, it was previously reported that nanocellulose served as diffusion barrier and retard the release of polyphenols from cellulose-based films (Bajpai et al. 2015). The mangosteen extract has poor solubility in water, and it barely dissolves in water-based mediums. It was slightly released from the films and hardly diffusable in the agar due to the interactions between polyphenols and biopolymer chains within the matrix. The antibacterial tests were also assessed according to JIS Z 2801 standard, which is a quantitative antimicrobial test to measure the growth that may occur after materials are inoculated by bacteria. The bacterial counts on the surface of BCG-M5 and BCG-M10 were comparable to available tulle dressing. In this study, the mangosteen extract-loaded films had a greater inhibition effect against Gram-positive bacteria (S. aureus) than against Gram-negative ones (E. coli) after 24 h of contact (Fig. 9B). These results were in agreement with previous findings that mangosteen extract was more effective against Gram-positive strains (Zhang et al. 2020a, b; Jamila et al. 2021). This was due to the differences in the cell wall structure, cell physiology, and metabolism between Gram-positive and Gram-negative strains. Furthermore, several proposed mechanisms of how mangosteen extract react to bacteria were reported. The plausible explanations for the non-leaching films in this study were that the mangosteen extract could bind to the receptors of the bacteria cell walls, disrupting integrity of the bacterial cell wall leading to cell death (Koh et al. 2013; Nguyen et al. 2014). The fabricated films could suppress bacterial growth upon direct contact. They could be considered passive antibacterial biomaterials as they inhibit bacteria growth without antibacterial agent leaching. This type of material could be locally applied directly at the target site. It may only affect the microbial infection site but did not affect beneficial bacteria or any other surrounding healthy tissues. This would minimize the undesirable effects of antibacterial agents. These non-leaching composites would not turn into infectious agent reservoir as direct contact proceeds. Further studies should clarify the mode of action of these non-leaching films.
Cell studies
In vitro cell study was a preliminary assessment that could indicate the potential for clinical application. Cell viability of the films was accessed following the direct contact method of ISO10993-5. Cells cultured on coverslips were used for the reference. The percentages of cell viability of HaCat, GF, and CAL27 cells are presented in Fig. 10.
According to ISO10993-5 standard, the viability percentages of HaCat and GF cells over a period of 24 h were > 70%, indicating film non-cytotoxicity. This inferred that all fabricated films were cytocompatible with healthy human cells. For CAL27 cells, it was found that the number of cells dropped over the time course of 24 h culture period in a mangosteen extract content-dependent manner. The apparent decrease in CAL27, oral cancer cell lines, was observed. SEM micrographs of HaCat, GF, and CAL27 are presented in Fig. 11.
Hacat and GF cells grew well on all composite films. Cells elongated, spread out, and maintained their typical characteristics shape over the culture period. It was noticed that the incorporation of mangosteen extract might induce some changes in the cellular morphology. Distinct morphological alterations and deformation of CAL27 cells were observed on mangosteen-loaded films. CAL27 exhibited the loss of adhesion and cellular retraction. Since the mangosteen extract was barely leached out, the mode of action would be from the interaction between cell surface molecules. Recent studies reported that the mangosteen extract could bind to tumor-necrosis-factor-related apoptosis-inducing ligand (TRAIL), which is involved in oral cancer cells apoptosis and cell cycle arrest (Kumazaki et al. 2015; Fukuda et al. 2017; De Looff et al. 2019). These receptors are expressed on the cancer cell surface but not on the normal cell surface (Wang et al. 2003; Dai et al. 2015). Furthermore, the mangosteen extract is also capable of inducing apoptosis, suppressing the expression of oncogenes and transcription factors, inducing epithelial-mesenchymal transition (EMT) in cancer cells. The mangosteen extract could bind with the Wingless-related integration site (Wnt) and interfere the Wnt/β-catenin signaling pathway, leading to cancer cells apoptosis (Yoo et al. 2011; Lei et al. 2014; Xu et al. 2014; Verma et al. 2016; Yang et al. 2021). Further studies should clarify the actual mode of action of films incorporating the mangosteen extract on cancer cells.
Conclusions
This work proposed a fast, simple, eco-friendly, and cost-effective way to fabricate a multifunctional biocomposite. Direct incorporation of the mangosteen extract into the BCG film matrix and crosslinking with tannin did not require any special scientific equipment. Furthermore, the fabrication also did not require using harsh conditions such as high temperature or harsh chemicals. The mangosteen extract was well-embedded in the matrix and could preserve their useful bioactivities. The fabricated films were capable of suppressing the bacteria colonization. Films demonstrated the antibacterial activity against E. coli (Gram-negative) and S. aureus (Gram-positive) upon direct contact according to Japanese International Standard (JISZ2801) compared with the commercial control. Furthermore, antibacterial property of the films was particularly good against S. aureus. In addition, films showed anticancer property against oral cancer cells but were still cytocompatible with human keratinocytes and GF. This suggested that these multifunctional biocomposites could represent an intriguing option for the treatment of skin wounds, gingivitis, periodontitis, and oral cancer.
References
Aadil K, Barapatre A, Jha H (2016) Synthesis and characterization of Acacia lignin-gelatin film for its possible application in food packaging. Bioresour Bioprocess 3:220. https://doi.org/10.1186/s40643-016-0103-y
Ahi ZB, Renkler NZ, Seker MG, Tuzlakoglu K (2019) Biodegradable polymer films with a natural antibacterial extract as novel periodontal barrier membranes. Int J Biomater 2019:1–7. https://doi.org/10.1155/2019/7932470
Ahmad M, Yamin BM, Lazim AM (2013) A study on dispersion and characterisation of α-mangostin loaded pH sensitive microgel systems. Chem Central J 7(1):85. https://doi.org/10.1186/1752-153x-7-85
Aisha AF, Abu-Salah KM, Ismail Z, Majid AMSA (2012) In vitro and in vivo anti-colon cancer effects of Garcinia mangostana xanthones extract. BMC Compl Altern Med 12(1):104. https://doi.org/10.1186/1472-6882-12-104
Aminah LN, Leong ST, Ho CY, Wong YS, Kairulazam CK (2014) Characterization of Garcinia Mangostana Linn. seeds as potential feedstocks for biodiesel production. Int J Eng Technol 6(2):146–150. https://doi.org/10.7763/ijet.2014.v6.684
Andrade FK, Morais JPS, Muniz CR, Nascimento JHOD, Vieira RS, Gama FMP, Rosa MF (2019) Stable microfluidized bacterial cellulose suspension. Cellulose 26(10):5851–5864. https://doi.org/10.1007/s10570-019-02512-y
Azeredo HMC, Barud H, Farinas CS, Vasconcellos VM, Claro AM (2019) Bacterial cellulose as a raw material for food and food packaging applications. Front Sustain Food Syst 2019:3. https://doi.org/10.3389/fsufs.2019.00007
Bajpai S, Chand N, Ahuja S (2015) Investigation of curcumin release from chitosan/cellulose micro crystals (CMC) antimicrobial films. Int J Biol Macromol 79:440–448. https://doi.org/10.1016/j.ijbiomac.2015.05.012
Barud HS, Souza JL, Santos DB, Crespi MS, Ribeiro C, Messaddeq Y, Ribeiro S (2011) Bacterial cellulose/poly(3-hydroxybutyrate) composite membranes. Carbohydr Polym 83(3):1279–1284. https://doi.org/10.1016/j.carbpol.2010.09.049
Bayir E, Bilgi E, Hames EE, Sendemir A (2019) Production of hydroxyapatite–bacterial cellulose composite scaffolds with enhanced pore diameters for bone tissue engineering applications. Cellulose 26(18):9803–9817. https://doi.org/10.1007/s10570-019-02763-9
Bodini R, Sobral P, Favaro-Trindade C, Carvalho R (2013) Properties of gelatin-based films with added ethanol- propolis extract. LWT 51(1):104–110. https://doi.org/10.1016/j.lwt.2012.10.013
Chang-Bravo L, López-Córdoba A, Martino M (2014) Biopolymeric matrices made of carrageenan and corn starch for the antioxidant extracts delivery of Cuban red propolis and yerba mate. React Func Polym 85:11–19. https://doi.org/10.1016/j.reactfunctpolym.2014.09.025
Chen J, Ahmad R, Li W, Swain M, Li Q (2015) Biomechanics of oral mucosa. J R Soc Interface 12(109):20150325. https://doi.org/10.1098/rsif.2015.0325
Choi JJE, Zwirner J, Ramani RS, Ma S, Hussaini HM, Waddell JN, Hammer N (2020) Mechanical properties of human oral mucosa tissues are site dependent: a combined biomechanical, histological and ultrastructural approach. Clin Exp Dent Res 6(6):602–611. https://doi.org/10.1002/cre2.305
Correa-Pacheco ZN, Bautista-Baños S, Ramos-García MDL, Martínez-González MDC, Hernández-Romano J (2019) Physicochemical characterization and antimicrobial activity of edible propolis-chitosan nanoparticle films. Prog Org Coat 137:105326. https://doi.org/10.1016/j.porgcoat.2019.105326
Cutting KF, Westgate SJ (2012) Super-absorbent dressings: How do they perform in vitro? Br J Nurs 21(20):S14–S19
Dai X, Zhang J, Arfuso F, Chinnathambi A, Zayed EM, Alharbi SA, Kumar AP, Ahn KS, Sethi G (2015) Targeting TNF-related apoptosis-inducing ligand (TRAIL) receptor by natural products as a potential therapeutic approach for cancer therapy. Exp Biol Med 240(6):760–773. https://doi.org/10.1177/1535370215579167
De Araújo GKP, De Souza SJ, Da Silva MV, Yamashita F, Gonçalves OH, Leimann FV, Shirai MA (2015) Physical, antimicrobial and antioxidant properties of starch-based film containing ethanolic propolis extract. Int J Food Sci Technol 50(9):2080–2087. https://doi.org/10.1111/ijfs.12869
De Looff M, De Jong S, Kruyt FAE (2019) Multiple interactions between cancer cells and the tumor microenvironment modulate TRAIL signaling: implications for TRAIL receptor targeted therapy. Front Immunol 10:1530. https://doi.org/10.3389/fimmu.2019.01530
Elsner JJ, Zilberman M (2010) Novel antibiotic-eluting wound dressings: an in vitro study and engineering aspects in the dressing’s design. J Tissue Viability 19(2):54–66. https://doi.org/10.1016/j.jtv.2009.11.001
Falcão L, Araújo MEM (2013) Tannins characterization in historic leathers by complementary analytical techniques ATR-FTIR, UV-Vis and chemical tests. J Cult Heritage 14(6):499–508
Fukuda M, Sakashita H, Hayashi H, Shiono J, Miyake G, Komine Y, Taira F (2017) Synergism between α-mangostin and TRAIL induces apoptosis in squamous cell carcinoma of the oral cavity through the mitochondrial pathway. Oncol Rep. https://doi.org/10.3892/or.2017.6030
Genevro GM, Neto RJG, Paulo LDA, Lopes P, de Moraes MA, Beppu MM (2019) Glucomannan asymmetric membranes for wound dressing. J Mater Res 34(4):481–489. https://doi.org/10.1557/jmr.2018.463
Ghahri S, Mohebby B, Pizzi A, Mirshokraie A, Mansouri HR (2017) Improving Water resistance of soy-based adhesive by vegetable Tannin. J Polym Environ 26(5):1881–1890. https://doi.org/10.1007/s10924-017-1090-6
Gomes S, Rodrigues G, Martins G, Roberto M, Mafra M, Henriques C, Silva J (2015) In vitro and in vivo evaluation of electrospun nanofibers of PCL, chitosan and gelatin: a comparative study. Mater Sci Eng C 46:348–358. https://doi.org/10.1016/j.msec.2014.10.051
Gonçalves MM, Carneiro J, Justus B, Espinoza JT, Budel JM, Farago PV, de Paula JP (2020) Preparation and characterization of a novel antimicrobial film dressing for wound healing application. Braz J Pharm Sci. https://doi.org/10.1590/s2175-97902020000118784
Gough JE, Scotchford CA, Downes S (2002) Cytotoxicity of glutaraldehyde crosslinked collagen/poly(vinyl alcohol) films is by the mechanism of apoptosis. J Biomed Mater Res 61(1):121–130. https://doi.org/10.1002/jbm.10145
Hoque S, Benjakul S, Prodpran T (2010) Properties of film from cuttlefish (Sepia pharaonis) skin gelatin incorporated with cinnamon, clove and star anise extracts. Food Hydrocoll 25(5):1085–1097. https://doi.org/10.1016/j.foodhyd.2010.10.005
Jamila N, Khan N, Bibi N, Waqas M, Khan SN, Atlas A, Amin F, Khan F, Saba M (2021) Hg(II) sensing, catalytic, antioxidant, antimicrobial, and anticancer potential of Garcinia mangostana and α-mangostin mediated silver nanoparticles. Chemosphere 272:129794. https://doi.org/10.1016/j.chemosphere.2021.129794
Jordan LG, Booth BW (2018) HER2+ breast cancer cells undergo apoptosis upon exposure to tannic acid released from remodeled cross-linked collagen type I. J Biomed Mater Res Part A 106(1):26–32. https://doi.org/10.1002/jbm.a.36205
Jost V, Kobsik K, Schmid M, Noller K (2014) Influence of plasticiser on the barrier, mechanical and grease resistance properties of alginate cast films. Carbohydr Polym 110:309–319. https://doi.org/10.1016/j.carbpol.2014.03.096
Kakkar P, Verma S, Manjubala I, Madhan B (2014) Development of keratin–chitosan–gelatin composite scaffold for soft tissue engineering. Mater Sci Eng C 45:343–347. https://doi.org/10.1016/j.msec.2014.09.021
Kawakami H, Yoshida K, Nishida Y, Kikuchi Y, Sato Y (2008) Antibacterial properties of metallic elements for alloying evaluated with application of JIS Z 2801:2000. ISIJ Int 48(9):1299–1304. https://doi.org/10.2355/isijinternational.48.1299
Koh J-J, Qiu S, Zou H, Lakshminarayanan R, Li J, Zhou X, Tang C, Saraswathi P, Verma C, Tan DT, Tan AL, Liu S (1828) Beuerman RW (2013) Rapid bactericidal action of alpha-mangostin against MRSA as an outcome of membrane targeting. Biochimica Et Biophysica Acta (BBA) Biomembr 2:834–844. https://doi.org/10.1016/j.bbamem.2012.09.004
Kumar PS, Raj NM, Praveen G, Chennazhi KP, Nair SV, Jayakumar R (2013) In vitro and in vivo evaluation of microporous chitosan hydrogel/nanofibrin composite bandage for skin tissue regeneration. Tissue Eng Part A 19(3–4):380–392. https://doi.org/10.1089/ten.tea.2012.0376
Kumazaki M, Shinohara H, Taniguchi K, Ueda H, Nishi M, Ryo A, Akao Y (2015) Understanding of tolerance in TRAIL-induced apoptosis and cancelation of its machinery by α-mangostin, a xanthone derivative. Oncotarget 6(28):25828–25842
Lee KX, Shameli K, Miyake M, Kuwano N, Khairudin NBBA, Mohamad SEB, Yew YP (2016) Green synthesis of gold nanoparticles using aqueous extract of garcinia mangostana fruit peels. J Nanomater 2016:1–7. https://doi.org/10.1155/2016/8489094
Lei J, Huo X, Duan W, Xu Q, Li R, Ma J, Li X, Han L, Li W, Sun H, Wu E, Ma Q (2014) α-Mangostin inhibits hypoxia-driven ROS-induced PSC activation and pancreatic cancer cell invasion. Cancer Lett 347(1):129–138. https://doi.org/10.1016/j.canlet.2014.02.003
Liu C, Zhang Y, Li X, Luo J, Gao Q, Li J (2017) A high-performance bio-adhesive derived from soy protein isolate and condensed tannins. RSC Adv 7:21226–21233. https://doi.org/10.1039/c7ra01210a
Lu R, Zhang X, Cheng X, Zhang Y, Zan X, Zhang L (2020) Medical applications based on supramolecular self-assembled materials from tannic acid. Front Chem 8:583484. https://doi.org/10.3389/fchem.2020.583484
Ma T, Zhao QQ, Ji KH, Zeng B, Li GQ (2014) Homogeneous and porous modified bacterial cellulose achieved by in situ modification with low amounts of carboxymethyl cellulose. Cellulose 21(4):2637–2646. https://doi.org/10.1007/s10570-014-0316-1
Milan E, Rodrigues M, Martins V, Plepis A, Fuhrmann-Lieker T, Horn M (2021) Mineralization of phosphorylated fish skin collagen/mangosteen scaffolds as potential materials for bone tissue regeneration. Molecules 26(10):2899. https://doi.org/10.3390/molecules26102899
Min S, Ezati P, Rhim J-W (2022) Gelatin-based packaging material incorporated with potato skins carbon dots as functional filler. Ind Crops Prod 181:114820. https://doi.org/10.1016/j.indcrop.2022.114820
Murali S, Kumar S, Koh J, Seena S, Singh P, Ramalho A, Sobral AJFN (2019) Bio-based chitosan/gelatin/Ag@ZnO bionanocomposites: synthesis and mechanical and antibacterial properties. Cellulose 26(9):5347–5361. https://doi.org/10.1007/s10570-019-02457-2
Musso YS, Salgado PR, Mauri AN (2017) Smart edible films based on gelatin and curcumin. Food Hydrocoll 66:8–15. https://doi.org/10.1016/j.foodhyd.2016.11.007
Musso YS, Salgado PR, Mauri AN (2019) Smart gelatin films prepared using red cabbage (Brassica oleracea L.) extracts as solvent. Food Hydrocoll 89:674–681. https://doi.org/10.1016/j.foodhyd.2018.11.036
Muyonga J, Cole C, Duodu K (2004) Fourier transform infrared (FTIR) spectroscopic study of acid soluble collagen and gelatin from skins and bones of young and adult Nile perch (Lates niloticus). Food Chem 86(3):325–332. https://doi.org/10.1016/j.foodchem.2003.09.038
Nagarajan M, Benjakul S, Prodpran T, Songtipya P (2015) Properties and characteristics of nanocomposite films from tilapia skin gelatin incorporated with ethanolic extract from coconut husk. J Food Sci Technol 52(12):7669–7682. https://doi.org/10.1007/s13197-015-1905-1
Nangia A, Hung C (1989) Design of a new hydrocolloid dressing. Burn 15(6):385–388. https://doi.org/10.1016/0305-4179(89)90104-6
Naskar D, Kundu SC, James NR (2015) Fabrication of cationized gelatin nanofibers by electrospinning for tissue regeneration. RSC Adv 5(109):89521–89530. https://doi.org/10.1039/C5RA10384C
Nguyen PTM, Falsetta ML, Hwang G, Gonzalez-Begne M, Koo H (2014) α-Mangostin disrupts the development of Streptococcus mutans Biofilms and Facilitates Its Mechanical Removal. PLoS ONE 9(10):e111312. https://doi.org/10.1371/journal.pone.0111312
Olivas GI, Barbosa-Cánovas GV (2008) Alginate-calcium films: Water vapor permeability and mechanical properties as affected by plasticizer and relative humidity. LWT 41(2):359–366. https://doi.org/10.1016/j.lwt.2007.02.015
Pham DT, Tetyczka C, Hartl S, Absenger-Novak M, Fröhlich E, Tiyaboonchai W, Roblegg E (2020) Comprehensive investigations of fibroin and poly(ethylenimine) functionalized fibroin nanoparticles for ulcerative colitis treatment. J Drug Deliv Sci Technol 57:101484. https://doi.org/10.1016/j.jddst.2019.101484
Pothitirat W, Chomnawang MT, Supabphol R, Gritsanapan W (2009) Comparison of bioactive compounds content, free radical scavenging and anti-acne inducing bacteria activities of extracts from the mangosteen fruit rind at two stages of maturity. Fitoterapia 80(7):442–447. https://doi.org/10.1016/j.fitote.2009.06.005
Qu J, Zhao X, Liang Y, Zhang T, Ma PX, Guo B (2018) Antibacterial adhesive injectable hydrogels with rapid self-healing, extensibility and compressibility as wound dressing for joints skin wound healing. Biomaterials 183:185–199. https://doi.org/10.1016/j.biomaterials.2018.08.044
Quan VM, Li B, Sukyai P (2020) Bacterial cellulose modification using static magnetic field. Cellulose 27(10):5581–5596. https://doi.org/10.1007/s10570-020-03159-w
Rebelo AR, Archer AJ, Chen X, Liu C, Yang G, Liu Y (2018) Dehydration of bacterial cellulose and the water content effects on its viscoelastic and electrochemical properties. Sci Technol Adv Mater 19(1):203–211. https://doi.org/10.1080/14686996.2018.1430981
Rohman A, Arifah FH, Irnawati AG, Muchtaridi M (2020) The application of FTIR spectroscopy and chemometrics for classification of Mangosteen extract and its correlation with alpha-mangostin. J Appl Pharm Sci 10(4):149–154. https://doi.org/10.7324/japs.2020.104019
Rojewska M, Bartkowiak A, Milanowski B, Prochaska K, Lulek J (2019) Physicochemical and release studies of new mucoadhesive fluconazole delivery systems. Coll Surf a: Physicochem Eng Asp 566:11–20. https://doi.org/10.1016/j.colsurfa.2018.12.058
Ruan C, Zhu Y, Zhou X, Abidi N, Hu Y, Catchmark JM (2016) Effect of cellulose crystallinity on bacterial cellulose assembly. Cellulose 23(6):3417–3427. https://doi.org/10.1007/s10570-016-1065-0
Salgado PR, López-Caballero ME, Gómez-Guillén MC, Mauri AN, Montero MP (2012) Exploration of the antioxidant and antimicrobial capacity of two sunflower protein concentrate films with naturally present phenolic compounds. Food Hydrocoll 29(2):374–381. https://doi.org/10.1016/j.foodhyd.2012.03.006
Scolamiero G, Pazzini C, Bonafè F, Guarnieri C, Muscari C (2018) Effects of α-mangostin on viability, growth and cohesion of multicellular spheroids derived from human breast cancer cell lines. Int J Med Sci 15(1):23–30. https://doi.org/10.7150/ijms.22002
Sharahi M, Hivechi A, Bahrami SH, Hemmatinejad N, Milan PB (2021) Co-electrospinning of lignocellulosic nanoparticles synthesized from walnut shells with poly(caprolactone) and gelatin for tissue engineering applications. Cellulose 28(8):4943–4957. https://doi.org/10.1007/s10570-021-03709-w
Silver FH, Freeman JW, Devore D (2001) Viscoelastic properties of human skin and processed dermis. Ski Res Technol 7(1):18–23. https://doi.org/10.1034/j.1600-0846.2001.007001018.x
Stie MB, Gätke JR, Wan F, Chronakis IS, Jacobsen J, Nielsen HM (2020) Swelling of mucoadhesive electrospun chitosan/polyethylene oxide nanofibers facilitates adhesion to the sublingual mucosa. Carbohydr Polym 242:116428. https://doi.org/10.1016/j.carbpol.2020.116428
Taheri P, Jahanmardi R, Koosha M, Abdi S (2020) Physical, mechanical and wound healing properties of chitosan/gelatin blend films containing tannic acid and/or bacterial nanocellulose. Int J Biol Macromol 154:421–432. https://doi.org/10.1016/j.ijbiomac.2020.03.114
Takigawa T, Endo Y (2006) Effects of glutaraldehyde exposure on human health. J Occup Health 48(2):75–87. https://doi.org/10.1539/joh.48.75
Tavassoli-Kafrani E, Goli SAH, Fathi M (2017) Fabrication and characterization of electrospun gelatin nanofibers crosslinked with oxidized phenolic compounds. Int J Biol Macromol 103:1062–1068. https://doi.org/10.1016/j.ijbiomac.2017.05.152
Ullah H, Badshah M, Mäkilä E, Salonen J, Shahbazi M-A, Santos HA, Khan T (2017) Fabrication, characterization and evaluation of bacterial cellulose-based capsule shells for oral drug delivery. Cellulose 24(3):1445–1454. https://doi.org/10.1007/s10570-017-1202-4
Unal S, Arslan S, Yilmaz BK, Oktar FN, Sengil AZ, Gunduz O (2021) Production and characterization of bacterial cellulose scaffold and its modification with hyaluronic acid and gelatin for glioblastoma cell culture. Cellulose 28(1):117–132. https://doi.org/10.1007/s10570-020-03528-5
Unnithan AR, Sasikala ARK, Murugesan P, Gurusamy M, Wu D, Park CH, Kim CS (2015) Electrospun polyurethane-dextran nanofiber mats loaded with Estradiol for post-menopausal wound dressing. Int J Biol Macromol 77:1–8. https://doi.org/10.1016/j.ijbiomac.2015.02.044
Valdés A, García AV, Martínez-Abad A, Vilaplana F, Jimenez A, Garrigós M (2019) Gelatin-based antimicrobial films incorporating pomegranate (Punica granatum L.) seed juice by-product. Molecules 25(1):166. https://doi.org/10.3390/molecules25010166
Verma RK, Yu W, Shrivastava A, Shankar S, Srivastava RK (2016) α-Mangostin-encapsulated PLGA nanoparticles inhibit pancreatic carcinogenesis by targeting cancer stem cells in human, and transgenic (KrasG12D, and KrasG12D/tp53R270H) mice. Sci Rep 6(1):32743. https://doi.org/10.1038/srep32743
Wahid F, Bai H, Wang F-P, Xie Y-Y, Zhang Y-W, Chu L-Q, Jia S-R, Zhong C (2019) Facile synthesis of bacterial cellulose and polyethyleneimine based hybrid hydrogels for antibacterial applications. Cellulose 27(1):369–383. https://doi.org/10.1007/s10570-019-02806-1
Wang S, El-Deiry WS (2003) TRAIL and apoptosis induction by TNF-family death receptors. Oncogene 22(53):8628–8633. https://doi.org/10.1038/sj.onc.1207232
Wang J, Wan Y, Han J, Lei X, Yan T, Gao C (2011) Nanocomposite prepared by immobilising gelatin and hydroxyapatite on bacterial cellulose nanofibres. Micro Nano Lett 6(3):133–136. https://doi.org/10.1049/mnl.2010.0209
Wathoni N, Meylina L, Rusdin A, Mohammed A, Tirtamie D, Herdiana Y, Motoyama K, Panatarani C, Joni I, Lesmana R, Muchtaridi M (2021) The potential cytotoxic activity enhancement of α-mangostin in Chitosan-Kappa carrageenan-loaded nanoparticle against MCF-7 cell line. Polymers 13(11):1681. https://doi.org/10.3390/polym13111681
Wlaschin KF, Ninkovic J, Griesgraber GW, Atan SC, Young AJ, Pereira JM, Solberg MJ, Smith G, Parks PJ, McNulty AK, Langer-Anderson DL (2019) The impact of first-aid dressing design on healing of porcine partial thickness wounds. Wound Repair Regen 27(6):622–633. https://doi.org/10.1111/wrr.12747
Wu P, Fisher A, Foo P, Queen D, Gaylor J (1995) In vitro assessment of water vapour transmission of synthetic wound dressings. Biomaterials 16(3):171–175. https://doi.org/10.1016/0142-9612(95)92114-l
Wu T, Farnood R, O’kelly K, Chen B. (2014) Mechanical behavior of transparent nanofibrillar cellulose-chitosan nanocomposite films in dry and wet conditions. J Mech Behav Biomed Mater 32:279–286. https://doi.org/10.1016/j.jmbbm.2014.01.014
Xiaorui K, Cong Z, Pin X, Zhanwen D, Zhijiang C (2022) Copper ion-imprinted bacterial cellulose for selectively removing heavy metal ions from aqueous solution. Cellulose 2022:1–19. https://doi.org/10.1007/s10570-022-04519-4
Xu Q, Ma J, Lei J, Duan W, Sheng L, Chen X, Hu A, Wang Z, Wu Z, Wu E, Ma Q, Li X (2014) α-Mangostin suppresses the viability and epithelial-mesenchymal transition of pancreatic cancer cells by downregulating the PI3K/Akt pathway. BioMed Res Int 2014:1–12. https://doi.org/10.1155/2014/546353
Yang S, Zhou F, Dong Y, Ren F (2021) α-mangostin induces apoptosis in human osteosarcoma cells through ROS-mediated endoplasmic reticulum stress via the WNT pathway. Cell Transpl. https://doi.org/10.1177/09636897211035080
Yao M, Li J, Zhang J, Ma S, Wang L, Gao F, Guan F (2020) Dual-enzymatically cross-linked gelatin hydrogel enhances neural differentiation of human umbilical cord mesenchymal stem cells and functional recovery in experimental murine spinal cord injury. J Mater Chem B 9(2):440–452. https://doi.org/10.1039/d0tb02033h
Ye S, Jiang L, Su C, Zhu Z, Wen Y, Shao W (2019) Development of gelatin/bacterial cellulose composite sponges as potential natural wound dressings. Int J Biol Macromol 133:148–155. https://doi.org/10.1016/j.ijbiomac.2019.04.095
Yong H, Liu J (2020) Recent advances in the preparation, physical and functional properties, and applications of anthocyanins-based active and intelligent packaging films. Food Packag Shelf Life 26:100550. https://doi.org/10.1016/j.fpsl.2020.100550
Yoo J-H, Kang K, Jho EH, Chin Y-W, Kim J, Nho CW (2011) α- and γ-Mangostin inhibit the proliferation of colon cancer cells via β-catenin gene regulation in Wnt/cGMP signalling. Food Chem 129(4):1559–1566. https://doi.org/10.1016/j.foodchem.2011.06.007
Yu B, Kang S-Y, Akthakul A, Ramadurai N, Pilkenton M, Patel A, Nashat A, Anderson DG, Sakamoto FH, Gilchrest BA, Anderson RR, Langer RS (2016) An elastic second skin. Nat Mater 15(8):911–918. https://doi.org/10.1038/nmat4635
Yusof NLBM, Wee A, Lim LY, Khor E (2003) Flexible chitin films as potential wound-dressing materials: wound model studies. J Biomed Mater Res A 66A(2):224–232. https://doi.org/10.1002/jbm.a.10545
Zaman HU, Islam J, Khan MA, Khan RA (2011) Physico-mechanical properties of wound dressing material and its biomedical application. J Mech Behav Biomed Mater 4(7):1369–1375. https://doi.org/10.1016/j.jmbbm.2011.05.007
Zhang X, Do MD, Casey P, Sulistio A, Qiao GG, Lundin L, Lillford P, Kosaraju S (2010) Chemical modification of gelatin by a natural phenolic cross-linker, Tannic Acid. J Agric Food Chem 58(11):6809–6815. https://doi.org/10.1021/jf1004226
Zhang C, Cao J, Zhao S, Luo H, Yang Z, Gama M, Zhang Q, Su D, Wan Y (2020a) Biocompatibility evaluation of bacterial cellulose as a scaffold material for tissue-engineered corneal stroma. Cellulose 27(5):2775–2784. https://doi.org/10.1007/s10570-020-02979-0
Zhang X, Liu J, Yong H, Qin Y, Liu J, Jin C (2020b) Development of antioxidant and antimicrobial packaging films based on chitosan and mangosteen (Garcinia mangostana L.) rind powder. Int J Biol Macromol 145:1129–1139. https://doi.org/10.1016/j.ijbiomac.2019.10.038
Zhou B, Hu X, Zhu J, Wang Z, Wang X, Wang M (2016) Release properties of tannic acid from hydrogen bond driven antioxidative cellulose nanofibrous films. Int J Biol Macromol 91:68–74. https://doi.org/10.1016/j.ijbiomac.2016.05.084
Zhou X, Dai Q, Huang X, Qin Z (2021) Preparation and characterizations of antibacterial-antioxidant film from soy protein isolate incorporated with mangosteen peel extract. E-Polymers 21(1):575–589. https://doi.org/10.1515/epoly-2021-0058
Acknowledgments
This research project is supported by the Second Century Fund (C2F), Chulalongkorn University, National Research Council of Thailand (NRCT) N42A650201 and Thailand Science Research and Innovation Fund Chulalongkorn University (CU_FRB65_bcg (37)_216_62_01).
Funding
This research project is supported by the Second Century Fund (C2F), Chulalongkorn University, National Research Council of Thailand (NRCT) N42A650201 and Thailand Science Research and Innovation Fund Chulalongkorn University (CU_FRB65_bcg (37)_216_62_01).
Author information
Authors and Affiliations
Contributions
Conceptualization, methodology, validation, investigation, formal analysis, resources and data curation: NC, MO and MP, validation: SS, writing, reviewing and editing: NC, MO and MP, supervision: MO and HU, project administration: MO and HU, funding acquisition: MO and HU.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chiaoprakobkij, N., Seetabhawang, S., Okhawilai, M. et al. Multifunctional bacterial cellulose-gelatin containing mangosteen extract films with improved antibacterial and anticancer properties. Cellulose 29, 6811–6830 (2022). https://doi.org/10.1007/s10570-022-04685-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10570-022-04685-5