-
PDF
- Split View
-
Views
-
Cite
Cite
Ariadni Papadopoulou, Niraj S Kumar, Anne Vanhoestenberghe, Nader K Francis, Environmental sustainability in robotic and laparoscopic surgery: systematic review, British Journal of Surgery, Volume 109, Issue 10, October 2022, Pages 921–932, https://doi.org/10.1093/bjs/znac191
Close - Share Icon Share
Abstract
Minimally invasive surgical (MIS) techniques are considered the gold standard of surgical interventions, but they have a high environmental cost. With global temperatures rising and unmet surgical needs persisting, this review investigates the carbon and material footprint of MIS and summarizes strategies to make MIS greener.
The MEDLINE, Embase, and Web of Science databases were interrogated between 1974 and July 2021. The search strategy encompassed surgical setting, waste, carbon footprint, environmental sustainability, and MIS. Two investigators independently performed abstract/full-text reviews. An analysis of disability-adjusted life years (DALYs) averted per ton of carbon dioxide equivalents (CO2e) or waste produced was generated.
From the 2456 abstracts identified, 16 studies were selected reporting on 5203 MIS procedures. Greenhouse gas (GHG) emissions ranged from 6 kg to 814 kg CO2e per case. Carbon footprint hotspots included production of disposables and anaesthetics. The material footprint of MIS ranged from 0.25 kg to 14.3 kg per case. Waste-reduction strategies included repackaging disposables, limiting open and unused instruments, and educational interventions. Robotic procedures result in 43.5 per cent higher GHG emissions, 24 per cent higher waste production, fewer DALYs averted per ton of CO2, and less waste than laparoscopic alternatives.
The increased environmental impact of robotic surgery may not sufficiently offset the clinical benefit. Utilizing alternative surgical approaches, reusable equipment, repackaging, surgeon preference cards, and increasing staff awareness on open and unused equipment and desflurane avoidance can reduce GHG emissions and waste.
Introduction
Minimally invasive surgical (MIS) techniques have rapidly emerged in the last 30 years to become the preferred method for abdominal, thoracic, and urological procedures. The benefits of the minimally invasive approach have been well documented with regard to reduced postoperative pain, shorter hospital stay, improved cosmesis, and quicker return to normal function1–8. In combination with the rise in use of robotic surgery, laparoscopic surgery has led to a vast growth in caseload and the use of highly sophisticated technology and resources.
With the demand for surgery growing, especially in the developing world, global emissions and waste production arising from surgical intervention will only increase. The Lancet committee for surgery found that there is a need for 143 million more surgeries to reduce morbidity and mortality globally9. To fulfil this demand is to unleash unprecedented environmental consequences as a result of large-scale production of surgical infrastructure and equipment. Thus, the need for appropriate strategies to assess and minimize the environmental impact of surgery is of utmost priority for the future of healthcare provision services.
Sustainability in MIS has proven to be of great necessity in recent years, with an increased focus on minimizing the wastage and greenhouse gas (GHG) emissions associated with the provision of surgical care. A recent report showed that 4 to 5 per cent of carbon emissions in the UK arise from the National Health Service (NHS)10,11. Similar research in the USA found that 9 to 10 per cent of carbon emissions arise from healthcare12. Interestingly, the overall contribution of carbon emissions from MIS is yet to be fully elucidated or optimized. This study aimed to systematically review the MIS literature with the purpose of investigating the carbon footprint of MIS operations, the material footprint attributed to waste of MIS operations, and other environmental impacts of the MIS operating theatre.
Methods
Study design
This systematic review was conducted in accordance with the updated 2020 PRISMA guidelines and the Cochrane Handbook of Systematic Reviews of Interventions13–16.
Search strategy and selection criteria
The following databases were interrogated for relevant studies covering the time period between 1974 and July 2021: MEDLINE via Ovid, Embase via Ovid, and Web of Science. The Cochrane Database was searched to identify relevant systematic reviews. The databases were chosen as reputable sources and as they incorporate a wide range of biomedical and clinical medical reports. Web of Science was included to address basic science or recent technological innovations in green MIS.
We systematically searched the literature combining search terms specifying the surgical theatre setting; terms related to environmental sustainability; and terms narrowing our search to MIS. The following search strategy was used: (operation OR operating room* OR operating theater OR operating theatre OR surgical procedure) AND (sustainability OR ecolog* OR medical waste OR equipment reuse OR disposable equipment OR recycling OR climate change OR ‘life cycle assessment’ OR carbon footprint OR greenhouse gas*) AND (robotic surg* OR laparoscopic surg* OR minimally invasive surg* OR minimal access surgery OR MIS OR MAS). The search was further adjusted to include relevant medical subject heading terms and subject headings specific to MEDLINE and Embase. The detailed search strategy is provided in Appendix S1.
The studies identified following the primary search were assessed to determine their eligibility according to inclusion and exclusion criteria by two assessors (A.P. and N.S.K.). Subsequently, full-text articles were reviewed. To further decrease unidentified relevant studies, a manual search was conducted, and the reference lists of included studies was carefully examined.
Eligibility criteria
Full-text articles written in English addressing environmental sustainability in MIS and including original data were included. Life cycle assessments, observational and interventional studies were accepted.
Exclusion criteria
Case reports, conference abstracts, letters to the editor, opinion articles, reviews, and articles not written in English were excluded from this analysis. Studies including open and minimally invasive surgical cases where MIS findings were not reported separately were excluded. Cost-effectiveness studies that did not comment on the impact of their interventions on environmental sustainability were also excluded.
Data extraction and outcome measures
Data from included studies were systematically collected by A.P. and N.S.K. using a standardized Microsoft Excel 2010 template; any disagreement was resolved by discussion with the senior author (N.K.F.). Multiple data points were extracted. Baseline data included first author, publication year, study setting and country, study design, surgical specialty, type of MIS, patient sample size, and number of participating surgeons.
Data related to GHG emissions included number of GHGs considered, GHG emission types (1 to 3), GHG data type (direct, primary process activity, secondary process activity, secondary financial data), source of emission factors, and global warming potential (GWP). The main GHG-related outcomes were the average carbon dioxide (CO2) equivalents (CO2e) per case, percentage contribution of GHG sources to GHG emissions, and percentage reduction of total kg CO2e postintervention. Sources contributing to GHG emissions were categorized as ‘anaesthetics and pharmaceuticals’; ‘energy, including electricity’; ‘equipment’, ‘heating, ventilation, air conditioning’, ‘reusables’, ‘single-use materials and production’, ‘disposal and recycling’, and ‘water use and treatment’. Carbon hotspots, author recommendations, and assumptions were noted. For studies investigating carbon footprint, products and processes included in the measurement of GHG emissions were collected to identify commonly neglected components.
Carbon footprint is defined as the total amount of direct and indirect GHG emissions due to MIS, including CO2 and other GHG (methane, nitrous oxide, anaesthetic gases, etc.). The latter are converted to CO2e according to their global warming potential (amount of energy absorbed relative to the same mass of CO2). The material footprint includes the total weight of waste produced due to MIS, including material extraction and processing.
Regarding surgical waste, the following main outcomes were extracted: total weight of waste produced during the study period, weight of waste per case per included group, and percentage contribution of waste subcategories to total waste by weight. The waste classifications used were also documented. In studies including an intervention, extracted data included intervention design and time period, control used, number of cases pre- and postintervention, absolute and percentage change in amount of waste per case, total absolute and percentage change in waste, absolute and percentage change in cost of waste per case, total absolute and percentage change in waste cost, and relevant P values. Changes in peri- and intraoperative outcomes were also noted.
Life cycle assessments (LCAs) were included. A LCA is a methodology used to determine and quantify the environmental impacts of a product or service accounting for the materials and energy required during all the processes involved. It includes indicators such as GHG emissions and ozone depletion, and produces cumulative environmental impact information. Data points included LCA approach, guidelines used, functional unit (process evaluated by LCA), inventory boundaries (items or processes included in the LCA), life cycle impact assessment method, and software and databases used. The percentage contributions of different environmental impact sources (anaesthetics and pharmaceuticals; energy; reusables; single-use materials and production; disposal and recycling; and water use and treatment) to each of the 10 impact categories included on the Tool for Reduction and Assessment of Chemicals and Other Environmental Impacts (TRACI) were analyzed17.
From collected information on MIS and their waste output, a speculative analysis of disability-adjusted life years (DALYs) averted in 10 years postsurgery was generated per ton of CO2e or waste produced, supported by the methodology by Bhopal and Norheim18. Note that, owing to the lack of patient-specific data to provide information on patient indications and outcomes following surgery, DALYs were estimated using studies with similar cohorts19–22.
Quality assessment
The papers were independently evaluated by two assessors (A.P. and N.S.K.). Owing to the heterogeneity in study designs, quality assessment was examined using several metrics. LCAs were evaluated using modified criteria from Drew et al., based on Weidema’s Guidelines for Critical Review of LCAs,23,24 and pre-post non-controlled studies were assessed using the Cochrane Risk Of Bias In Non-Randomized Studies of Interventions (ROBINS-I) tool25. No standardized tool has been published to assess observational studies with environmental outcomes that are not classified as cohort, case–control, or cross-sectional. Hence, a non-standardized tool created by Rizan et al. was used26. Variations were discussed and resolved.
Results
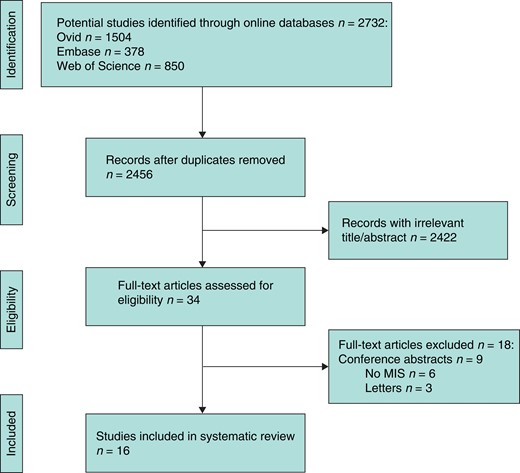
The titles and abstracts of 2456 unique citations were identified and 34 full-text papers were reviewed. After assessing for eligibility, 16 studies were included in the systematic review (Fig. 1): five LCAs27–31, four retrospective observational studies32–35, three pre-post non-controlled studies36–38, two prospective observational studies39,40, one observational study of undefined time frame41, and one model-based assessment that did not use LCA methodology42. The studies reported on a total of 5203 MIS procedures. Six studies27,28,31,32,34,41 included both laparoscopic and robotic procedures, while 10 focused on the laparoscopic approach29,30,33,35–40,42. Basic characteristics of the studies are available in Table 1 and quality assessment results can be viewed in Appendix S2. Methodology of outcome measurement, omission of scopes of GHG emission, lack of use of a carbon footprinting protocol, and non-assessment of parameter uncertainty were the most common parameters increasing risk of bias.
PRISMA flow diagram of included studies
MIS, minimally invasive surgery.
Characteristics of included studies
| Author, year . | Study setting, country . | Study design . | Surgical procedure (n) . | Focus and outcomes of study . |
|---|---|---|---|---|
| Adler et al. (2005)42 | Single general hospital, Germany | Model | Laparoscopic cholecystectomy (model assumes 255/year or 100/year over 5 years) | Reusable versus disposable instruments |
| Chasseigne et al. (2018)39 | Nîmes University Hospital, Nîmes, France | Prospective observational | Laparoscopic appendectomy, hernioplasty, cholecystectomy (n = 15) | Quantity and wastage reason of opened unused supplies |
| Graham et al. (2019)35 | American College of Surgeons case log, USA | Retrospective observational | Single incision paediatric endosurgery laparoscopic appendectomy (n = 246) | Waste of polymeric clips versus endoscopic staplers |
| Khor et al. (2020)40 | Single institution, Malaysia | Prospective observational | Phacoemulsification (n = 203) | Waste weight and composition reported |
| Ludwig et al. (2015)34 | Single tertiary care centre, USA | Retrospective observational | Robot-assisted laparoscopic radical prostatectomy (n = 1579) and robot-assisted partial nephrectomy (n = 313) | Robotic instrument exchange rate and lifetime estimation |
| Park et al. (2021)36 | Single institution, USA | Pre-post non-controlled | Laparoscopic paediatric surgery (n = 998) | Surgeons shown reports of their disposable utilization |
| Power et al. (2012)27 | Not specified, USA | LCA | Robotic and laparoscopic gastrointestinal, gynaecological, urological, miscellaneous | Quantifies CO2 emissions from MIS per year in USA |
| Rose et al. (2019)41 | Single military medical centre, USA | Observational | Laparoscopic and robotic general surgery (open cases excluded) (n = 30) | Waste and cost of opened and unused instruments |
| Ross et al. (2019)37 | Single acute care hospital, Canada | Pre-post non-controlled | Laparoscopic hysterectomy (n = 430) | Effect of cost-awareness campaign on disposable use |
| Takeuchi et al. (2005)38 | Single institution, Japan | Pre-post non-controlled | Laparoscopic gynaecological surgery (n = 20) | Waste and cost after repackaging disposables |
| Thiel et al. (2015)28 | Single institution teaching hospital, USA | LCA | Hysterectomy (n = 62): (a) abdominal versus (b) vaginal versus (c) laparoscopic versus (d) robotic | LCA of hysterectomy by surgical approach |
| Thiel et al. (2017)29 | Two tertiary care centres, India | LCA | Minimally invasive cataract phacoemulsification surgery | LCA and description of assembly line surgery |
| Thiel et al. (2018)30 | Single institution, university hospital, USA | LCA | Laparoscopic hysterectomy model interventions (a) anaesthesia, (b) surgical materials and equipment, (c) energy (n = 17) | Models the effect of interventions on carbon footprint of hysterectomy |
| Unger et al. (2017)31 | Single institution, USA | LCA | Four types of hysterectomy: abdominal, vaginal, robotic, laparoscopic | LCA of biopolymer versus plastic single-use medical devices |
| Woods et al. (2015)32 | Not specified, USA | Retrospective observational | Endometrial cancer staging (n = 150): (a) laparoscopy versus (b) laparotomy versus (c) robotic; O&G | Carbon footprint quantification by surgical approach |
| Yoshizawa et al. (2011)33 | Single institution, Japan | Retrospective observational | All laparoscopic procedures: GI, paediatric, gynaecological, urological surgery (n = 1157) | Extrapolating scope 1 CO2 emissions to total yearly scope 1 emissions in Japan |
| Author, year . | Study setting, country . | Study design . | Surgical procedure (n) . | Focus and outcomes of study . |
|---|---|---|---|---|
| Adler et al. (2005)42 | Single general hospital, Germany | Model | Laparoscopic cholecystectomy (model assumes 255/year or 100/year over 5 years) | Reusable versus disposable instruments |
| Chasseigne et al. (2018)39 | Nîmes University Hospital, Nîmes, France | Prospective observational | Laparoscopic appendectomy, hernioplasty, cholecystectomy (n = 15) | Quantity and wastage reason of opened unused supplies |
| Graham et al. (2019)35 | American College of Surgeons case log, USA | Retrospective observational | Single incision paediatric endosurgery laparoscopic appendectomy (n = 246) | Waste of polymeric clips versus endoscopic staplers |
| Khor et al. (2020)40 | Single institution, Malaysia | Prospective observational | Phacoemulsification (n = 203) | Waste weight and composition reported |
| Ludwig et al. (2015)34 | Single tertiary care centre, USA | Retrospective observational | Robot-assisted laparoscopic radical prostatectomy (n = 1579) and robot-assisted partial nephrectomy (n = 313) | Robotic instrument exchange rate and lifetime estimation |
| Park et al. (2021)36 | Single institution, USA | Pre-post non-controlled | Laparoscopic paediatric surgery (n = 998) | Surgeons shown reports of their disposable utilization |
| Power et al. (2012)27 | Not specified, USA | LCA | Robotic and laparoscopic gastrointestinal, gynaecological, urological, miscellaneous | Quantifies CO2 emissions from MIS per year in USA |
| Rose et al. (2019)41 | Single military medical centre, USA | Observational | Laparoscopic and robotic general surgery (open cases excluded) (n = 30) | Waste and cost of opened and unused instruments |
| Ross et al. (2019)37 | Single acute care hospital, Canada | Pre-post non-controlled | Laparoscopic hysterectomy (n = 430) | Effect of cost-awareness campaign on disposable use |
| Takeuchi et al. (2005)38 | Single institution, Japan | Pre-post non-controlled | Laparoscopic gynaecological surgery (n = 20) | Waste and cost after repackaging disposables |
| Thiel et al. (2015)28 | Single institution teaching hospital, USA | LCA | Hysterectomy (n = 62): (a) abdominal versus (b) vaginal versus (c) laparoscopic versus (d) robotic | LCA of hysterectomy by surgical approach |
| Thiel et al. (2017)29 | Two tertiary care centres, India | LCA | Minimally invasive cataract phacoemulsification surgery | LCA and description of assembly line surgery |
| Thiel et al. (2018)30 | Single institution, university hospital, USA | LCA | Laparoscopic hysterectomy model interventions (a) anaesthesia, (b) surgical materials and equipment, (c) energy (n = 17) | Models the effect of interventions on carbon footprint of hysterectomy |
| Unger et al. (2017)31 | Single institution, USA | LCA | Four types of hysterectomy: abdominal, vaginal, robotic, laparoscopic | LCA of biopolymer versus plastic single-use medical devices |
| Woods et al. (2015)32 | Not specified, USA | Retrospective observational | Endometrial cancer staging (n = 150): (a) laparoscopy versus (b) laparotomy versus (c) robotic; O&G | Carbon footprint quantification by surgical approach |
| Yoshizawa et al. (2011)33 | Single institution, Japan | Retrospective observational | All laparoscopic procedures: GI, paediatric, gynaecological, urological surgery (n = 1157) | Extrapolating scope 1 CO2 emissions to total yearly scope 1 emissions in Japan |
LCA, life cycle assessment; MIS, minimally invasive surgery; O&G, obstetrics and gynaecology; GI, gastrointestinal.
Characteristics of included studies
| Author, year . | Study setting, country . | Study design . | Surgical procedure (n) . | Focus and outcomes of study . |
|---|---|---|---|---|
| Adler et al. (2005)42 | Single general hospital, Germany | Model | Laparoscopic cholecystectomy (model assumes 255/year or 100/year over 5 years) | Reusable versus disposable instruments |
| Chasseigne et al. (2018)39 | Nîmes University Hospital, Nîmes, France | Prospective observational | Laparoscopic appendectomy, hernioplasty, cholecystectomy (n = 15) | Quantity and wastage reason of opened unused supplies |
| Graham et al. (2019)35 | American College of Surgeons case log, USA | Retrospective observational | Single incision paediatric endosurgery laparoscopic appendectomy (n = 246) | Waste of polymeric clips versus endoscopic staplers |
| Khor et al. (2020)40 | Single institution, Malaysia | Prospective observational | Phacoemulsification (n = 203) | Waste weight and composition reported |
| Ludwig et al. (2015)34 | Single tertiary care centre, USA | Retrospective observational | Robot-assisted laparoscopic radical prostatectomy (n = 1579) and robot-assisted partial nephrectomy (n = 313) | Robotic instrument exchange rate and lifetime estimation |
| Park et al. (2021)36 | Single institution, USA | Pre-post non-controlled | Laparoscopic paediatric surgery (n = 998) | Surgeons shown reports of their disposable utilization |
| Power et al. (2012)27 | Not specified, USA | LCA | Robotic and laparoscopic gastrointestinal, gynaecological, urological, miscellaneous | Quantifies CO2 emissions from MIS per year in USA |
| Rose et al. (2019)41 | Single military medical centre, USA | Observational | Laparoscopic and robotic general surgery (open cases excluded) (n = 30) | Waste and cost of opened and unused instruments |
| Ross et al. (2019)37 | Single acute care hospital, Canada | Pre-post non-controlled | Laparoscopic hysterectomy (n = 430) | Effect of cost-awareness campaign on disposable use |
| Takeuchi et al. (2005)38 | Single institution, Japan | Pre-post non-controlled | Laparoscopic gynaecological surgery (n = 20) | Waste and cost after repackaging disposables |
| Thiel et al. (2015)28 | Single institution teaching hospital, USA | LCA | Hysterectomy (n = 62): (a) abdominal versus (b) vaginal versus (c) laparoscopic versus (d) robotic | LCA of hysterectomy by surgical approach |
| Thiel et al. (2017)29 | Two tertiary care centres, India | LCA | Minimally invasive cataract phacoemulsification surgery | LCA and description of assembly line surgery |
| Thiel et al. (2018)30 | Single institution, university hospital, USA | LCA | Laparoscopic hysterectomy model interventions (a) anaesthesia, (b) surgical materials and equipment, (c) energy (n = 17) | Models the effect of interventions on carbon footprint of hysterectomy |
| Unger et al. (2017)31 | Single institution, USA | LCA | Four types of hysterectomy: abdominal, vaginal, robotic, laparoscopic | LCA of biopolymer versus plastic single-use medical devices |
| Woods et al. (2015)32 | Not specified, USA | Retrospective observational | Endometrial cancer staging (n = 150): (a) laparoscopy versus (b) laparotomy versus (c) robotic; O&G | Carbon footprint quantification by surgical approach |
| Yoshizawa et al. (2011)33 | Single institution, Japan | Retrospective observational | All laparoscopic procedures: GI, paediatric, gynaecological, urological surgery (n = 1157) | Extrapolating scope 1 CO2 emissions to total yearly scope 1 emissions in Japan |
| Author, year . | Study setting, country . | Study design . | Surgical procedure (n) . | Focus and outcomes of study . |
|---|---|---|---|---|
| Adler et al. (2005)42 | Single general hospital, Germany | Model | Laparoscopic cholecystectomy (model assumes 255/year or 100/year over 5 years) | Reusable versus disposable instruments |
| Chasseigne et al. (2018)39 | Nîmes University Hospital, Nîmes, France | Prospective observational | Laparoscopic appendectomy, hernioplasty, cholecystectomy (n = 15) | Quantity and wastage reason of opened unused supplies |
| Graham et al. (2019)35 | American College of Surgeons case log, USA | Retrospective observational | Single incision paediatric endosurgery laparoscopic appendectomy (n = 246) | Waste of polymeric clips versus endoscopic staplers |
| Khor et al. (2020)40 | Single institution, Malaysia | Prospective observational | Phacoemulsification (n = 203) | Waste weight and composition reported |
| Ludwig et al. (2015)34 | Single tertiary care centre, USA | Retrospective observational | Robot-assisted laparoscopic radical prostatectomy (n = 1579) and robot-assisted partial nephrectomy (n = 313) | Robotic instrument exchange rate and lifetime estimation |
| Park et al. (2021)36 | Single institution, USA | Pre-post non-controlled | Laparoscopic paediatric surgery (n = 998) | Surgeons shown reports of their disposable utilization |
| Power et al. (2012)27 | Not specified, USA | LCA | Robotic and laparoscopic gastrointestinal, gynaecological, urological, miscellaneous | Quantifies CO2 emissions from MIS per year in USA |
| Rose et al. (2019)41 | Single military medical centre, USA | Observational | Laparoscopic and robotic general surgery (open cases excluded) (n = 30) | Waste and cost of opened and unused instruments |
| Ross et al. (2019)37 | Single acute care hospital, Canada | Pre-post non-controlled | Laparoscopic hysterectomy (n = 430) | Effect of cost-awareness campaign on disposable use |
| Takeuchi et al. (2005)38 | Single institution, Japan | Pre-post non-controlled | Laparoscopic gynaecological surgery (n = 20) | Waste and cost after repackaging disposables |
| Thiel et al. (2015)28 | Single institution teaching hospital, USA | LCA | Hysterectomy (n = 62): (a) abdominal versus (b) vaginal versus (c) laparoscopic versus (d) robotic | LCA of hysterectomy by surgical approach |
| Thiel et al. (2017)29 | Two tertiary care centres, India | LCA | Minimally invasive cataract phacoemulsification surgery | LCA and description of assembly line surgery |
| Thiel et al. (2018)30 | Single institution, university hospital, USA | LCA | Laparoscopic hysterectomy model interventions (a) anaesthesia, (b) surgical materials and equipment, (c) energy (n = 17) | Models the effect of interventions on carbon footprint of hysterectomy |
| Unger et al. (2017)31 | Single institution, USA | LCA | Four types of hysterectomy: abdominal, vaginal, robotic, laparoscopic | LCA of biopolymer versus plastic single-use medical devices |
| Woods et al. (2015)32 | Not specified, USA | Retrospective observational | Endometrial cancer staging (n = 150): (a) laparoscopy versus (b) laparotomy versus (c) robotic; O&G | Carbon footprint quantification by surgical approach |
| Yoshizawa et al. (2011)33 | Single institution, Japan | Retrospective observational | All laparoscopic procedures: GI, paediatric, gynaecological, urological surgery (n = 1157) | Extrapolating scope 1 CO2 emissions to total yearly scope 1 emissions in Japan |
LCA, life cycle assessment; MIS, minimally invasive surgery; O&G, obstetrics and gynaecology; GI, gastrointestinal.
Carbon footprint of MIS
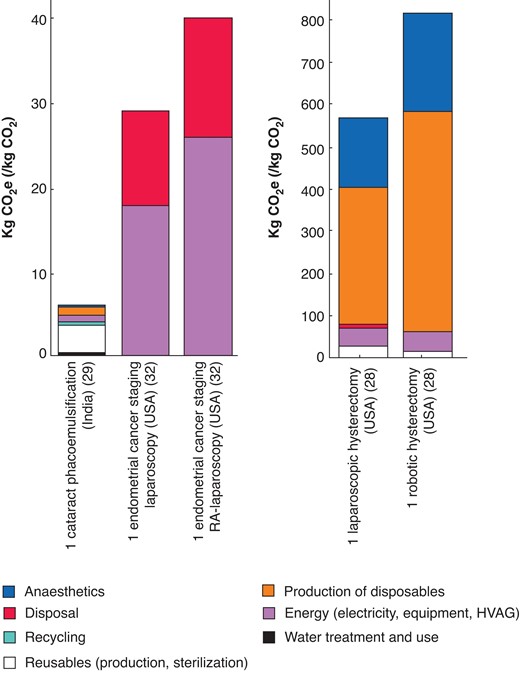
Six studies reported on the GHG emissions related to MIS procedures27–30,32,33. Three provided the carbon footprint of single MIS cases in kg of CO2e produced while showing the contribution of individual processes (Fig. 2)28,29,32. Cataract phacoemulsification in India had the lowest carbon footprint producing 6 kg CO2e per case29, while robotic hysterectomy in the USA had the highest GHG emissions at 814 kg CO2e28.
Carbon footprint of single minimally invasive surgical cases in included studies
CO2e, carbon dioxide equivalents.
Production of disposables and anaesthetics were the main contributors in high-emission minimally invasive hysterectomy accounting for 64 per cent and 28 per cent of GHG-related environmental impact by TRACI assessment, respectively28. In the lower-emitting endometrial cancer staging procedures energy and disposal appeared to be the main contributors to GHG emissions; however, anaesthetics and production of disposables were not investigated32. Production and sterilization of reusables was the largest contributor to phacoemulsification emissions, accounting for 57 per cent of environmental impacts despite only producing 3.42 kg CO2e per case29.
When comparing the carbon footprint of laparoscopic and robotic procedures, the latter were associated with increased emissions. Robotic hysterectomy had 43.5 per cent higher GHG emissions compared to laparoscopic hysterectomy in a study by Thiel et al.28 while Woods et al. reported a 38 per cent increase in kg CO2e produced during a robotically assisted endometrial cancer staging laparoscopy versus traditional laparoscopy32.
Evaluation of items and processes included in the carbon footprint calculation across the studies is shown in Appendix S3. The number of included items ranged from 20/37 over 9/12 processes evaluated in a study by Thiel et al.28 to only 1/37 items reported in a study by Yoshizawa et al.33 focusing on scope 1 emissions due to insufflation. Commonly neglected processes (reported in ≤ 2 studies) included surgical capital equipment manufacturing (n = 0), water use (n = 1), anaesthetic gas production and emission (n = 2), production and distribution of other drugs (n = 1), production of surgical supplies (n = 2), end of life of reusable supplies (n = 2), and end of life of other waste (n = 2).
Two of the included studies calculated the yearly CO2 emissions in their respective country setting due to MIS procedures. Power et al. estimated that 355 924 tonnes of CO2/year are released in the USA due to robotic and laparoscopic procedures in a LCA of MIS27. Yoshizawa et al. reported that 35 384 tonnes of CO2 were released in Japan in 2007 due to laparoscopic surgery, but this is a gross underestimation given only scope 1 emissions were included in the analysis33.
One LCA determined the theoretical effect of interventions on the carbon footprint of laparoscopic hysterectomy30. The anaesthetic interventions resulting in largest decrease in emissions were sevoflurane use only (27 per cent reduction) and propofol only (28 per cent reduction). In material interventions, minimal instrument hysterectomy (64 per cent reduction) and combined minimal material and maximum reuse (69 per cent reduction) resulted in the largest decrease in emissions, while recycling and reuse of linen and swabs only resulted in a 2 per cent decrease. Combination of occupancy sensors and low-carbon energy grid decreased emissions by 10 per cent. Combination of most successful measures from above resulted in 79 per cent reduction of GHG emissions30.
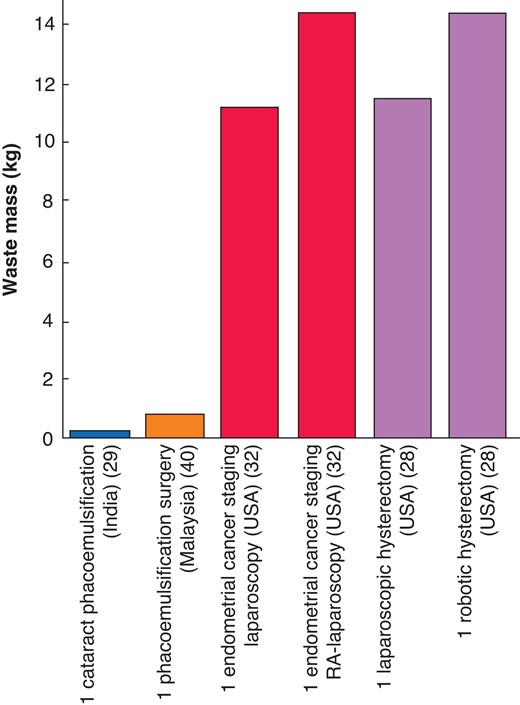
Material footprint of MIS
Of the 16 included studies, 11 addressed the material footprint of MIS operations28,29,32,35–42. Four studies reported the waste weight produced per case (Fig. 3)28,29,32,40. Similarly to the carbon footprint results, cataract phacoemulsification in India had the lowest material footprint, producing 0.25 kg per case29, while robotic hysterectomy and robotically assisted laparoscopy for endometrial cancer staging in the USA had the highest, with both procedures producing 14.3 kg per case28,32. Robotically assisted endometrial cancer staging laparoscopy produced significantly increased waste compared with traditional laparoscopy (14.3 versus 11.2; P < 0.01)32. Thiel et al. reported 24 per cent higher waste per case produced in robotic versus laparoscopic hysterectomy (14.3 versus 11.5); however, no significance testing was done28.
Material footprint of single minimally invasive surgical cases
RA, robotically-assisted.
Of the 11 studies, six provided waste classification data. Classification into general and medical waste was used in two studies28,40. The detailed waste classification systems used are provided in Appendix S4.
Three pre-post non-controlled studies with interventions to decrease waste production were included36–38. Park et al. introduced personal report cards for surgeons with disposable supply utilization and supply cost per case, resulting in significant disposable supply cost reduction of 42.6 per cent (P < 0.001) due to reduced disposable use36. Ross et al. implemented a cost-awareness campaign that decreased disposable supply cost in laparoscopic hysterectomy by 12 per cent37. Takeuchi et al. sanctioned the repackaging of disposable instruments into packs of essential items customized to laparoscopic gynaecological surgery at their institution, resulting in a waste reduction of 400 g per case or 280 kg per year38.
Three observational studies proposed readily applicable interventions for waste reduction in the MIS theatre. In a retrospective study, Graham et al. compared endoscopic staplers used during paediatric laparoscopic appendectomy with polymeric clips placed with non-disposable laparoscopic appliers and found polymeric clips to result in a 99 per cent decrease in waste production and a projected reduction of 289 kg of waste annually35. Two studies addressed the contribution of opened but unused supplies to waste. In a case series by Rose et al., opened but unused supplies accounted for up to 27 per cent of items and $4528.1841. More complex robotic operations had the highest cost of wasted supplies ($379)41. Chasseigne et al. also reported that up to 20.1 per cent of surgical supply cost was attributed to open, unused items with anticipation of surgeons’ needs (27 per cent), aseptic errors (17 per cent), and comfort (22 per cent) being the most common causes of wastage39. Applied and proposed interventions for waste management are summarized in Table 2.
Summary of applied and proposed interventions for waste management in minimally invasive surgery
| Author (year) . | Surgical intervention/specialty . | Intervention . | Time period . | Change in waste mass (%) . | Change in cost per case . | Long-term change in cost . |
|---|---|---|---|---|---|---|
| Chasseigne et al. (2018)39 | Laparoscopic appendectomy, hernioplasty, cholecystectomy | Proposed decreasing opened and unused waste by price transparency reports per instrument and case | July–August 2015 | NS | Laparoscopic appendectomy: €23.1; hernioplasty: €6.4; cholecystectomy: €4.4 | €210.9 |
| Graham et al. (2019)35 | Laparoscopic appendectomy | Proposed switch of endoscopic staplers to polymeric clips placed with non-disposable laparoscopic appliers | 2011–2017 | 0.965 kg (−99%) | $286–$333 per case | NS |
| Park et al. (2021) 36 | Laparoscopic paediatric surgery | Individual monthly and quarterly surgeon report cards with supply cost per case and disposable supply utilization, meetings to reflect on instrument use | 2017–2019 | NS | $190 (−42.6%) (P < 0.001) | $71 035 for the first year $38 875 for the next 6 months (P = 0.012) |
| Rose et al. (2019)41 | Laparoscopic hysterectomy | Proposed updating surgeons’ instrument preference cards and training staff to decrease opened and unused waste, increase instrument knowledge and avoid distractions | September 2018–February 2019 | 27% of waste items were opened unused and could be eliminated | NS | $4528.18 Predicted savings |
| Ross et al. (2019)37 | Laparoscopic hysterectomy | Cost-awareness campaign: educational meetings on cost, full day skills lab, posters and demonstrations | 2016–2017 | NS | $116 (−12%) | $7798 across 67 cases |
| Takeuchi et al. (2005)38 | Laparoscopic gynaecological surgery | Repackaging of disposable instruments into customized packs of 28 essential items (external packaging manufacturer) | NS | 400 g Predicted 280 kg reduction per year | NS | $1792 savings per year |
| Author (year) . | Surgical intervention/specialty . | Intervention . | Time period . | Change in waste mass (%) . | Change in cost per case . | Long-term change in cost . |
|---|---|---|---|---|---|---|
| Chasseigne et al. (2018)39 | Laparoscopic appendectomy, hernioplasty, cholecystectomy | Proposed decreasing opened and unused waste by price transparency reports per instrument and case | July–August 2015 | NS | Laparoscopic appendectomy: €23.1; hernioplasty: €6.4; cholecystectomy: €4.4 | €210.9 |
| Graham et al. (2019)35 | Laparoscopic appendectomy | Proposed switch of endoscopic staplers to polymeric clips placed with non-disposable laparoscopic appliers | 2011–2017 | 0.965 kg (−99%) | $286–$333 per case | NS |
| Park et al. (2021) 36 | Laparoscopic paediatric surgery | Individual monthly and quarterly surgeon report cards with supply cost per case and disposable supply utilization, meetings to reflect on instrument use | 2017–2019 | NS | $190 (−42.6%) (P < 0.001) | $71 035 for the first year $38 875 for the next 6 months (P = 0.012) |
| Rose et al. (2019)41 | Laparoscopic hysterectomy | Proposed updating surgeons’ instrument preference cards and training staff to decrease opened and unused waste, increase instrument knowledge and avoid distractions | September 2018–February 2019 | 27% of waste items were opened unused and could be eliminated | NS | $4528.18 Predicted savings |
| Ross et al. (2019)37 | Laparoscopic hysterectomy | Cost-awareness campaign: educational meetings on cost, full day skills lab, posters and demonstrations | 2016–2017 | NS | $116 (−12%) | $7798 across 67 cases |
| Takeuchi et al. (2005)38 | Laparoscopic gynaecological surgery | Repackaging of disposable instruments into customized packs of 28 essential items (external packaging manufacturer) | NS | 400 g Predicted 280 kg reduction per year | NS | $1792 savings per year |
NS, not specified.
Summary of applied and proposed interventions for waste management in minimally invasive surgery
| Author (year) . | Surgical intervention/specialty . | Intervention . | Time period . | Change in waste mass (%) . | Change in cost per case . | Long-term change in cost . |
|---|---|---|---|---|---|---|
| Chasseigne et al. (2018)39 | Laparoscopic appendectomy, hernioplasty, cholecystectomy | Proposed decreasing opened and unused waste by price transparency reports per instrument and case | July–August 2015 | NS | Laparoscopic appendectomy: €23.1; hernioplasty: €6.4; cholecystectomy: €4.4 | €210.9 |
| Graham et al. (2019)35 | Laparoscopic appendectomy | Proposed switch of endoscopic staplers to polymeric clips placed with non-disposable laparoscopic appliers | 2011–2017 | 0.965 kg (−99%) | $286–$333 per case | NS |
| Park et al. (2021) 36 | Laparoscopic paediatric surgery | Individual monthly and quarterly surgeon report cards with supply cost per case and disposable supply utilization, meetings to reflect on instrument use | 2017–2019 | NS | $190 (−42.6%) (P < 0.001) | $71 035 for the first year $38 875 for the next 6 months (P = 0.012) |
| Rose et al. (2019)41 | Laparoscopic hysterectomy | Proposed updating surgeons’ instrument preference cards and training staff to decrease opened and unused waste, increase instrument knowledge and avoid distractions | September 2018–February 2019 | 27% of waste items were opened unused and could be eliminated | NS | $4528.18 Predicted savings |
| Ross et al. (2019)37 | Laparoscopic hysterectomy | Cost-awareness campaign: educational meetings on cost, full day skills lab, posters and demonstrations | 2016–2017 | NS | $116 (−12%) | $7798 across 67 cases |
| Takeuchi et al. (2005)38 | Laparoscopic gynaecological surgery | Repackaging of disposable instruments into customized packs of 28 essential items (external packaging manufacturer) | NS | 400 g Predicted 280 kg reduction per year | NS | $1792 savings per year |
| Author (year) . | Surgical intervention/specialty . | Intervention . | Time period . | Change in waste mass (%) . | Change in cost per case . | Long-term change in cost . |
|---|---|---|---|---|---|---|
| Chasseigne et al. (2018)39 | Laparoscopic appendectomy, hernioplasty, cholecystectomy | Proposed decreasing opened and unused waste by price transparency reports per instrument and case | July–August 2015 | NS | Laparoscopic appendectomy: €23.1; hernioplasty: €6.4; cholecystectomy: €4.4 | €210.9 |
| Graham et al. (2019)35 | Laparoscopic appendectomy | Proposed switch of endoscopic staplers to polymeric clips placed with non-disposable laparoscopic appliers | 2011–2017 | 0.965 kg (−99%) | $286–$333 per case | NS |
| Park et al. (2021) 36 | Laparoscopic paediatric surgery | Individual monthly and quarterly surgeon report cards with supply cost per case and disposable supply utilization, meetings to reflect on instrument use | 2017–2019 | NS | $190 (−42.6%) (P < 0.001) | $71 035 for the first year $38 875 for the next 6 months (P = 0.012) |
| Rose et al. (2019)41 | Laparoscopic hysterectomy | Proposed updating surgeons’ instrument preference cards and training staff to decrease opened and unused waste, increase instrument knowledge and avoid distractions | September 2018–February 2019 | 27% of waste items were opened unused and could be eliminated | NS | $4528.18 Predicted savings |
| Ross et al. (2019)37 | Laparoscopic hysterectomy | Cost-awareness campaign: educational meetings on cost, full day skills lab, posters and demonstrations | 2016–2017 | NS | $116 (−12%) | $7798 across 67 cases |
| Takeuchi et al. (2005)38 | Laparoscopic gynaecological surgery | Repackaging of disposable instruments into customized packs of 28 essential items (external packaging manufacturer) | NS | 400 g Predicted 280 kg reduction per year | NS | $1792 savings per year |
NS, not specified.
The lifetime of robotic instruments was investigated by Ludwig et al.34. Monopolar curved scissors were identified as the instrument with highest exchange rate (12.4 per cent of cases) during robot-assisted laparoscopic radical prostatectomy and partial nephrectomy, and may have fewer than 10 lives, contributing to waste in robotic procedures.
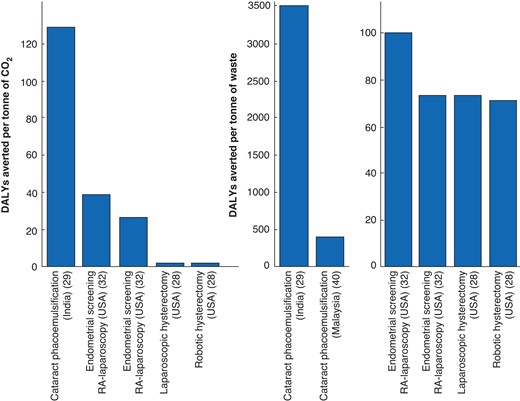
Disability-adjusted life years averted per tonne of CO2/waste
As expected, analysis of DALYs averted showed that surgeries with low carbon and material footprints corresponded to higher DALYs averted per tonne of CO2 or waste produced. Phacoemulsification had the highest DALYs averted per tonne of CO2 and per tonne of waste produced, equalling 125 DALYs per tonne CO2 and 3420 DALYs per tonne of waste29. Robotically assisted hysterectomy had the lowest benefit, with two DALYs averted per tonne CO2 and 72 DALYs per tonne of waste28. Both for endometrial cancer screening and hysterectomy, robotic approaches were associated with lower DALYs averted per tonne of CO2 and waste, with the largest difference being associated with endometrial cancer staging (Fig. 4). Detailed methodology and results of DALYs averted analysis are provided in Appendix S5.
Disability-adjusted life years (DALYs) averted per tonne of carbon dioxide equivalents (CO2e) and per tonne of waste produced from minimally invasive surgery
RA, robotically-assisted.
Other environmental impact outcomes
Two LCAs considered other environmental impacts of phacoemulsification and minimally invasive hysterectomy28,29. The percentage contribution of different processes to environmental outcomes are provided in Table 3. The main contributors to ozone depletion are production of disposables (64 to 97 per cent) and anaesthetics (3 to 23 per cent) in both publications. Regarding hysterectomy in the USA, the production of disposables is the main contributor to acidification (76 to 84 per cent); carcinogens (80 to 87 per cent); non-carcinogens (68 to 71 per cent); respiratory effects (87 to 92 per cent); ecotoxicity (78 to 83 per cent); cumulative energy demand (86 to 91 per cent); and eutrophication (46 to 52 per cent followed by disposal)28. Eutrophication occurs in water bodies due to an increase in nitrates and phosphates from pesticide runoff and industrial waste leading to decreased oxygen levels and loss of biodiversity. Disposables production (33 to 41 per cent) and energy use (42 to 43 per cent) were the main contributors to smog formation28. In all categories, energy use and reusables were the next most important contributors. The impacts of laparoscopic hysterectomy were 9 to 37 per cent lower than those of robotic hysterectomy across all outcomes28. Disposable production was the main contributor in ozone depletion due to phacoemulsification in India as well29. However, it was the production and processing of reusables that mainly contributed to smog (55 per cent), acidification (61 per cent), eutrophication (50 per cent), carcinogens (44 per cent), non-carcinogens (33 per cent), respiratory effects (76 per cent), ecotoxicity (48 per cent), and cumulative energy demand (36 per cent) in that setting29.
| . | Anaesthetics and drugs (%) . | Energy (electricity, equipment, HVAG) (%) . | Reusables (sterilization, allocation, production) (%) . | Disposable and recycled materials production (%) . | Disposal (%) . | Recycling (%) . | Water treatment and use (%)* . |
|---|---|---|---|---|---|---|---|
| Ozone depletion | 3–23 | 0–2 | 0–8 | 64–97 | 0 | 0–1 | 1 |
| Greenhouse gases | 4–29 | 6–21 | 2–57 | 14–64 | 0–1 | 0–4 | 4 |
| Smog | 0–5 | 23–43 | 17–55 | 10–41 | 0–1 | 1–3 | 4 |
| Acidification | 0–3 | 11–20 | 5–61 | 10–84 | 0–2 | 0–2 | 4 |
| Eutrophication | 0–1 | 2–13 | 3–50 | 7–52 | 0–43 | 0–1 | 28 |
| Carcinogens | 0–1 | 2–12 | 9–44 | 25–87 | 1 | 1–2 | 14 |
| Non-carcinogens | 0–2 | 9–11 | 8–33 | 9–71 | 0–10 | 0–1 | 48 |
| Respiratory effects | 0 | 6–20 | 2–76 | 3–92 | 0 | 0 | 1 |
| Ecotoxicity | 0 | 6–12 | 6–48 | 22–83 | 5 | 0.5–2 | 16 |
| Cumulative energy demand | 0–4 | 9.5–12 | 2–36 | 23–91 | 0–1 | 0.5–10 | 4 |
| . | Anaesthetics and drugs (%) . | Energy (electricity, equipment, HVAG) (%) . | Reusables (sterilization, allocation, production) (%) . | Disposable and recycled materials production (%) . | Disposal (%) . | Recycling (%) . | Water treatment and use (%)* . |
|---|---|---|---|---|---|---|---|
| Ozone depletion | 3–23 | 0–2 | 0–8 | 64–97 | 0 | 0–1 | 1 |
| Greenhouse gases | 4–29 | 6–21 | 2–57 | 14–64 | 0–1 | 0–4 | 4 |
| Smog | 0–5 | 23–43 | 17–55 | 10–41 | 0–1 | 1–3 | 4 |
| Acidification | 0–3 | 11–20 | 5–61 | 10–84 | 0–2 | 0–2 | 4 |
| Eutrophication | 0–1 | 2–13 | 3–50 | 7–52 | 0–43 | 0–1 | 28 |
| Carcinogens | 0–1 | 2–12 | 9–44 | 25–87 | 1 | 1–2 | 14 |
| Non-carcinogens | 0–2 | 9–11 | 8–33 | 9–71 | 0–10 | 0–1 | 48 |
| Respiratory effects | 0 | 6–20 | 2–76 | 3–92 | 0 | 0 | 1 |
| Ecotoxicity | 0 | 6–12 | 6–48 | 22–83 | 5 | 0.5–2 | 16 |
| Cumulative energy demand | 0–4 | 9.5–12 | 2–36 | 23–91 | 0–1 | 0.5–10 | 4 |
Only presented in one publication by Thiel et al. (2017)29.
| . | Anaesthetics and drugs (%) . | Energy (electricity, equipment, HVAG) (%) . | Reusables (sterilization, allocation, production) (%) . | Disposable and recycled materials production (%) . | Disposal (%) . | Recycling (%) . | Water treatment and use (%)* . |
|---|---|---|---|---|---|---|---|
| Ozone depletion | 3–23 | 0–2 | 0–8 | 64–97 | 0 | 0–1 | 1 |
| Greenhouse gases | 4–29 | 6–21 | 2–57 | 14–64 | 0–1 | 0–4 | 4 |
| Smog | 0–5 | 23–43 | 17–55 | 10–41 | 0–1 | 1–3 | 4 |
| Acidification | 0–3 | 11–20 | 5–61 | 10–84 | 0–2 | 0–2 | 4 |
| Eutrophication | 0–1 | 2–13 | 3–50 | 7–52 | 0–43 | 0–1 | 28 |
| Carcinogens | 0–1 | 2–12 | 9–44 | 25–87 | 1 | 1–2 | 14 |
| Non-carcinogens | 0–2 | 9–11 | 8–33 | 9–71 | 0–10 | 0–1 | 48 |
| Respiratory effects | 0 | 6–20 | 2–76 | 3–92 | 0 | 0 | 1 |
| Ecotoxicity | 0 | 6–12 | 6–48 | 22–83 | 5 | 0.5–2 | 16 |
| Cumulative energy demand | 0–4 | 9.5–12 | 2–36 | 23–91 | 0–1 | 0.5–10 | 4 |
| . | Anaesthetics and drugs (%) . | Energy (electricity, equipment, HVAG) (%) . | Reusables (sterilization, allocation, production) (%) . | Disposable and recycled materials production (%) . | Disposal (%) . | Recycling (%) . | Water treatment and use (%)* . |
|---|---|---|---|---|---|---|---|
| Ozone depletion | 3–23 | 0–2 | 0–8 | 64–97 | 0 | 0–1 | 1 |
| Greenhouse gases | 4–29 | 6–21 | 2–57 | 14–64 | 0–1 | 0–4 | 4 |
| Smog | 0–5 | 23–43 | 17–55 | 10–41 | 0–1 | 1–3 | 4 |
| Acidification | 0–3 | 11–20 | 5–61 | 10–84 | 0–2 | 0–2 | 4 |
| Eutrophication | 0–1 | 2–13 | 3–50 | 7–52 | 0–43 | 0–1 | 28 |
| Carcinogens | 0–1 | 2–12 | 9–44 | 25–87 | 1 | 1–2 | 14 |
| Non-carcinogens | 0–2 | 9–11 | 8–33 | 9–71 | 0–10 | 0–1 | 48 |
| Respiratory effects | 0 | 6–20 | 2–76 | 3–92 | 0 | 0 | 1 |
| Ecotoxicity | 0 | 6–12 | 6–48 | 22–83 | 5 | 0.5–2 | 16 |
| Cumulative energy demand | 0–4 | 9.5–12 | 2–36 | 23–91 | 0–1 | 0.5–10 | 4 |
Only presented in one publication by Thiel et al. (2017)29.
A LCA by Unger et al. showed that substitution of petroleum-based plastic for single-use medical devices with biopolymers decreases human health impacts, acidification, and cumulative energy demand, but increases smog and ozone depletion-related impacts of minimally invasive hysterectomy by approximately 900 per cent and 125 per cent, respectively, due to agricultural processes including the fermentation of biopolymer polylactide and biopolymer transport (Fig. 5)31.
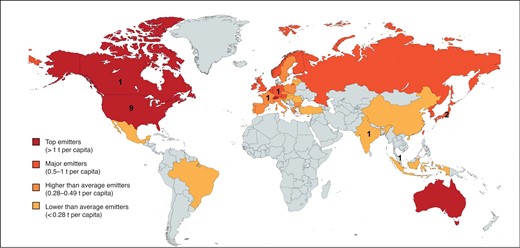
World chart demonstrating the number of included publications per country against the national healthcare-generated emissions in carbon dioxide equivalents emissions (tCO2e) per capita43
Discussion
This systematic review is dedicated to sustainable MIS. The evidence gathered showed that there is limited high-level evidence on the environmental impact of MIS, heterogeneity in study design, and data recording, hindering robust analysis. The majority of studies were conducted in the USA, one of the top healthcare-related CO2 emitters per capita. Unfortunately, only two of four top-emitter countries and one of 15 major emitters43 conducted studies relevant to the environmental impact of MIS, demonstrating the need for further research. The UK has committed to making its NHS net zero in carbon by 2040, the first national strategy to do so, inspiring 14 others to follow suit at the COP26 meeting in 202144. Given a growing movement towards sustainability, it is of outmost importance that evidence is available to best facilitate and evidence strategies towards this.
This review demonstrates that a single robotic surgical case can produce up to 814 kg CO2e, which is equivalent to the GHG emissions produced by driving a gasoline-powered car for 3658 km or the emissions corresponding to a single passenger flying from London to Rome 2.6 times26,45–47. The major contributors to the carbon footprint of MIS varied according to the type of operation and setting. Major carbon footprint hotspots to target included the production of disposables and anaesthetics, followed by energy use and disposal. Only one study examined interventions in the form of a LCA model. Minimal material and maximum reuse of equipment during hysterectomy resulted in a 69 per cent reduction to GHG emissions. Use of sevoflurane or propofol resulted in up to 60 per cent reduced GHG emissions versus desflurane use, a finding consistent with previous studies, including open surgical operations48,49. These results reflect similar carbon hotspots to those identified by Rizan et al. in a systematic review that proposed increased use of reusables and environmentally conscious electricity use with occupancy sensors and renewable energy sources26.
Three27,32,33 of six studies27–29,32,40,42 accounted for less than half of the processes of GHG emission considered in this study based on the Greenhouse Gas Protocol50. With evidence that is not rooted in said protocol and fails to account for various processes of GHG generation and emission, adequate identification of hotspot processes can prove challenging. We recommend that researchers of GHG emissions of MIS refer to the protocol or Appendix S3 as a guide to aid study design and boundaries, as well as reporting on future MIS sustainability studies. Inclusion of multiple GHG and scope 1 to 3 emissions is important and direct, primary process activity data should be considered where possible.
The material footprint of MIS in this study varied from 0.25 kg to 14.3 kg per case. The global average waste production per capita per day equals 0.74 kg but can be as low as 0.11 kg in developing nations. The upper range of waste produced during one MIS case equals that produced by a person during 19 days as a global average or during 130 days in developing countries51. Strategies proven to reduce waste production include replacing endoscopic staplers with a higher production footprint with polymeric clips and educational interventions, including workshops, and multidisciplinary team meetings and report cards to inform surgeons on the waste production of their cases and how to reduce the use of disposables. The repackaging of equipment into institution-specific packs of essential disposable supplies is another successful strategy. The packs should be designed according to ‘design for environment’ principles, including minimizing material used (design for dematerialization) and suitability for reuse or recycling (design for end of life)52,53. LCA and clinical input should be incorporated with regular updates to exclude rarely used equipment reflecting changes in practice. Lifetimes of robotic instruments such as monopolar scissors should be extended, while other instruments can outlive recommended uses and should be changed only when indicated.
Waste classification and segregation differ worldwide. Four of 11 studies did not include waste classification36–38,41 and only two reported material composition of waste by weight28,42. We recommend researchers use the WHO medical waste classification to standardize reporting. The material composition of waste could then be calculated for individual used items and extrapolated where possible to identify materials with a high environmental impact.
Robotic procedures were linked with up to 43.5 per cent higher GHG emissions and up to 24 per cent higher waste weight than their laparoscopic alternatives. a discrepancy largely attributed to the production of disposables (Fig. 2). Wood et al. reported plastic, cotton, and paper as the main municipal solid waste contributing to minimally invasive hysterectomy waste, which can be tackled using the reduce, reuse, and recycle approaches54. However, complex materials, including robotic arms and disposable instruments, caused the majority of environmental impacts in robotic hysterectomy, accounting for 93 per cent of global warming potential, 100 per cent of ozone depletion, and 86.3 per cent of energy demand54. This agrees with the findings of Thiel et al., which found the production of disposables to be the main contributor to multiple environmental impacts of robotic hysterectomy28. A systematic review by Drew et al.24 demonstrated that disposable equipment was associated with higher environmental impacts than reusable equivalents across all impact categories, making the adoption of reusables a valid intervention. Re-manufactured single-use medical devices can decrease complex waste in robotic surgery if used. Remanufacturing involves sterilization, quality control, certification, and repackaging of single-use medical devices by a manufacturer, followed by device redistribution conforming to national guidelines55. The carbon footprint of medical devices should be considered in the designing stages or investigated by the hospital in the context of sustainable procurement, which results in the purchasing of products with the least adverse effect on the environment56–58.
Reserving robotic operations for the most suitable patients and adopting the laparoscopic approach where possible could reduce the environmental impact of MIS. There was a fourfold increase in the number of robotic operations in England between 2013 and 2018, and the numbers continue to rise59. However, this rapid uptake is not associated with equivalent measures to investigate and or reduce the carbon footprint of MIS in the UK. From our analysis, we note that robotic surgery has a lower DALYs averted per tonne of CO2e as the increase in environmental impact may not be sufficiently offset by a clinical benefit. This raises the question of whether healthcare systems should prioritize sustainability outcomes or patient outcomes. For example, the DALYs averted per tonne of waste produced are only slightly higher in laparoscopic hysterectomy versus the robotic approach (73 versus 71) because they are balanced by better robotic outcomes. However, when comparing laparoscopic and robotically assisted endometrial cancer screening, the laparoscopic approach has lower waste mass produced and higher DALYs averted per operation, leading to a larger discrepancy in DALYs averted per tonne of waste (100 versus 73). Hence, this methodology can quantify the benefit from surgery and the environmental impact, focusing attempts for sustainable interventions where they are needed.
The limitations of this review include that the composition of waste was not reported in most studies, making the identification of waste hotspots challenging. Additionally, we used a non-standardized quality assessment tool26 for the seven observational studies included, as the outcome was environmental and not related to the patients or the interventions. There are currently no standardized tools that address this study design. We also note that none of the studies included provided high-quality randomized controlled trial data, and most of the studies had limited sample sizes or were reporting results from a single centre, limiting the quality of evidence. Additionally, the relatively high risk of bias found among the studies may have affected the reliability and precision of the outcome measures. Specifically, factors that may compromise internal validity and accuracy of CO2e measurements include not accounting for all carbon-emitting processes, limited available life cycle inventory data tailored to the medical sector and lacking geographically and institutionally relevant data. Similarly, indirect waste of MIS through material extraction and processing was not accounted for in any of the studies. The external validity of GHG emissions may be hindered by differences in inventory boundaries of LCA and operative setup variations across different cases, surgeons, and medical centres. Discrepancies in waste segregation and management also reduce the reproducibility of waste outcomes. Moving forward, these challenges may be addressed as LCA practices become standardized. The present studies represent only a few countries contributing to the global carbon footprint of healthcare as there were limited reports and only publications written in English were included. Therefore, some processes contributing to the carbon and material footprints may be ignored. However, to our knowledge, this is the first review to focus on sustainability in MIS and incorporate both carbon and material footprint of the techniques discussed.
More LCAs of MIS are needed to assess multiple environmental impacts beyond carbon and material footprint. LCAs of individual procedures in different specialties are required to identify the most effective environmental interventions and to expand the range of surgeries being optimized within the hospital setting to facilitate implementation of efficient processes aimed towards sustainability.
Three-tiered minimally invasive surgery sustainability recommendations
Surgical equipment manufacturing
Factor the carbon footprint of surgical equipment into the manufacturing process and maximize reprocessing potential of disposable medical devices.
Provide accurate robotic instrument life information, update it regularly, and conduct research on extending instrument life.
Research alternative materials to substitute petroleum-based plastic in disposables, including tackling the agriculture-related negative environmental impacts of biopolymers.
Surgical equipment procurement (hospital management)
Practice sustainable procurement in the business phase of capital acquisition, including factoring robotic instrument life into the robotic interphase selection.
Favour reusable equipment use and assess carbon footprint of single-use MIS devices prior to purchasing.
Consider purchasing remanufactured single-use devices abiding by national regulations.
Operation planning and theatre clinical team
Careful selection of robotic cases and consider their impact on sustainability of green operating room.
Substitute disposables with reusable surgical equipment, where possible.
Consider repackaging into hospital and operation-specific minimal material operation packs.
Update surgeon preference cards and train theatre stuff to increase awareness of the environmental burden of opened but unused equipment.
Favour sevoflurane or propofol-induced anaesthesia over desflurane use.
Use occupancy sensors and low-carbon energy grid from renewable energy providers.
Conclusion
Current MIS practice contributes to GHG emissions through the production of disposables, anaesthetic gases, energy use and disposal. Carbon and waste hotspots differ by operation and setting, with higher GHG emissions, waste, and other environmental impacts attributed to robotic techniques, specifically the production of disposables. Further collaborative efforts are required, focusing on standardized LCAs of operations and surgical equipment to identify effective interventions that will improve the environmental sustainability of MIS. These will subsequently need to be implemented at scale to improve clinical outcomes and work towards net zero wastage.
Funding
This research received a grant by the funding body University College London under the UCL Connected Learning Internships Scheme, project ID: 35. The funding body, University College London, did not have a role in study design, collection, analysis, and interpretation of data, writing of the report, and the decision to submit the paper for publication
Acknowledgements
A.P. was responsible for generating the study idea, designed the analysis and methods. A.P. and N.K. reviewed the literature. A.P. and N.K. did the analysis. A.P. wrote the first draft of the manuscript, which benefited from contributions by all authors. A.V. and N.F. participated in the analysis, edited the manuscript and provided scientific guidance. We would like to thank the Sustainability Task Force at University College London for supporting this project.
Disclosure. The authors declare no conflict of interest.
Supplementary material
Supplementary material is available at BJS online.
Data Availability
Data are available in the paper and appendix. Additional data are available via the corresponding author on request.
References
Resources for further reading
Greening the Operating Room Checklist, Practice Greenhealth:https://practicegreenhealth.org/tools-and-resources/greening-or-checklist https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwj_kPPl5-j1AhXbQkEAHQUvAqEQFnoECAwQAQ&url=https%3A%2F%2Fpracticegreenhealth.org%2Fsites%2Fdefault%2Ffiles%2Fupload-files%2Fgor_checklist_r5_web.pdf&usg=AOvVaw1IKLyrADR6preLVSrrB4UH
Forum for discussion on improving the environmental sustainability of operating theatres: https://networks.sustainablehealthcare.org.uk/network/sustainable-operating-theatres
Care pathways carbon footprint calculator, Sustainable Healthcare Coalition: https://shcpathways.org/full-calculator/
The anaesthetic impact calculator, Royal College of Anaesthetists: https://rcoa.ac.uk/about-college/strategy-vision/environment-sustainability/anaesthetic-impact-calculator
Minimally invasive surgery: a sustainable growth opportunity: https://www.mackayshields.com/insights-landing/956-minimally-invasive-surgery-a-sustainable-growth-opportunity
Green theatre: https://publishing.rcseng.ac.uk/doi/full/10.1308/rcsbull.2019.272
Using surgical sustainability principles to improve planetary health and optimize surgical services following the COVID-19 pandemic: https://publishing.rcseng.ac.uk/doi/full/10.1308/rcsbull.2020.148
Surgery and the NHS Carbon Footprint: https://publishing.rcseng.ac.uk/doi/pdf/10.1308/rcsbull.2020.152
NHS Supply Chain, minimally invasive surgery: https://www.supplychain.nhs.uk/product-information/contract-launch-brief/minimally-invasive-surgery/
A standardized method for estimating the carbon footprint of disposable minimally invasive surgical devices: https://journals.lww.com/aosopen/Fulltext/2021/09000/A_Standardized_Method_for_Estimating_the_Carbon.22.aspx
Delivering a Net Zero National Health Service: https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf