Abstract
Summary
This study examined the effects of denosumab compared to bisphosphonates and vitamin D alone on muscle performance in patients with low BMD. While grip force improved in both the denosumab and bisphosphonate group, a superior increase in chair rising test force was observed in the denosumab group.
Introduction
The aim of this study was to investigate the effect of the anti-resorptive agent denosumab (Dmab) on upper and lower limb muscle performance compared to bisphosphonate (BP) treatment and vitamin D supplementation alone (i.e., basic therapy) in patients with low BMD.
Methods
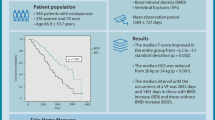
This retrospective, propensity score-matched (sex, age, BMI, follow-up time) cohort study included 150 osteopenic or osteoporotic patients receiving basic (n = 60), BP (n = 30) or Dmab (n = 60) therapy. All patients underwent a musculoskeletal assessment at baseline and follow-up, including DXA, laboratory bone metabolism parameters, grip force, and chair rising test mechanography. Mean annual percentage changes were calculated and compared between study groups.
Results
After a mean follow-up period of 17.6 ± 9.0 months, a significantly higher increase in grip force in both the Dmab (p < 0.001) and BP group (p = 0.001) compared to the vitamin D group was observed (vitamin D = − 6.1 ± 10.2%; BP = + 0.8 ± 8.2%; Dmab = + 5.1 ± 25.5%). The Dmab group showed a significantly higher increase in chair rising test force compared to the BP group (vitamin D = + 5.8 ± 12.7%; BP = + 0.9 ± 8.6%; Dmab = + 8.2 ± 14.4%; Dmab vs. BP p = 0.03). Neither the changes in BMD nor in bone metabolic parameters were associated with changes in muscle performance.
Conclusion
Dmab resulted in increased muscle strength in the upper and lower limbs, indicating systemic rather than site-specific effects as compared to BP. Based on these findings, Dmab might be favored over other osteoporosis treatments in patients with low BMD and poor muscle strength.
Similar content being viewed by others
Introduction
The demographic trend is shifting towards an aging society, with musculoskeletal disorders contributing significantly to the global burden of disease [1,2,3]. Age-related processes comprise musculoskeletal deterioration leading to quantitative and qualitative decline of both skeletal muscle and bone, defined by the terms sarcopenia and osteoporosis, respectively [4]. In line with the intrinsic coupling effects of muscle and bone tissue, the term osteosarcopenia has been proposed, mainly to improve identification of patients at high risk of fracture [5,6,7]. Both phenomena synergistically increase the risk of falls, fractures, frailty, and ultimately mortality with advancing age [8]. While numerous pharmacological agents have been approved for osteoporosis, sarcopenia is currently treated exclusively by lifestyle modification. The treatment of elderly patients with multifactorial and progressive osteosarcopenia primarily includes preventive measures, using the synergistic effects of adequate nutrition (i.e., calcium, vitamin D, creatine, and protein), physical exercise and balance training [9, 10].
The coupling between skeletal muscle and bone has long been considered to be primarily mechanical, but recent research suggests that muscle and bone tissues function as interacting secretory endocrine organs. By now, complex reciprocal interactions via myokines (e.g., myostatin [11], irisin [12]) and osteokines (e.g., osteocalcin [13], sclerostin[14]) have been discovered in the context of an existing muscle-bone crosstalk. In particular, the identification of the osteoprotegerin (OPG)/Receptor Activator of NF-κB Ligand (RANKL)/RANK pathway has been of major importance in this context [15]. RANK, the receptor for RANKL, is located on the surface of osteoclasts and their precursors, promotes osteoclast differentiation, function, and survival, and is antagonized by OPG, a competing soluble receptor. Pharmacological inhibition of RANK/RANKL signaling leads to impaired osteoclast precursor differentiation and impaired osteoclast function (i.e., bone resorption) [16]. Interestingly, RANK is also expressed in skeletal muscle and is involved in skeletal muscle function via the regulation of calcium storage [17]. In a mouse model of Duchenne muscular dystrophy, inhibition of RANKL was shown to reduce muscle fiber damage and to preserve muscle integrity [18].
Regarding treatment effects, there is increasing evidence of potential beneficial effects on muscle strength by denosumab (Dmab), a RANKL inhibitor approved as a first line treatment of osteoporosis [19,20,21]. However, the power of previous studies was limited to small cohorts, impeding differentiation of specific effects. Therefore, the aim of this study was to investigate the effects of Dmab on muscle performance in patients with low BMD, to compare potential changes with a cohort of patients treated with vitamin D alone (i.e., basic therapy) and with bisphosphonates (BP), and to outline skeletal and metabolic factors that may mediate these effects.
Methods
Study design
Patients presenting to our outpatient clinic between January 2010 and June 2021 were retrospectively reviewed. Inclusion criteria comprised at least two available appointments, each documenting a continuous treatment regimen (basic, BP, Dmab), dual energy X-ray absorptiometry (DXA) measurements, muscle function assessments of hand grip force and chair rising test force and time as well as laboratory parameters of bone. Propensity score-matching was applied for the basic and the Dmab group regarding sex distribution, age, BMI and follow-up time, thus enabling comparability and eliminating possible selection bias. This way, n = 60 patients each were included in the Dmab and basic therapy group. Subsequently, a third group of BP-treated patients was also included and matched to the basic therapy and Dmab group, resulting in a cohort auf n = 30 patients (total n = 150). Patients with both pre-existing and newly initiated anti-resorptive medication were included. Vitamin D supplementation was provided in all patients prior to initiation of anti-resorptive treatment, which consisted of 1000–3000 IU daily or 20,000 IU weekly to normalize 25(OH)D3 levels (≥ 30 µg/L). The BP group consisted of patients treated with oral alendronate 70 mg weekly or i.v. ibandronate 3 mg every 3 months. Outcome variables were calculated as the annual percentage changes of DXA values, laboratory bone metabolism markers and muscle performance tests. Results are presented according to the STROBE guidelines for reporting observational studies [22].
DXA
Bone mineral density (BMD) was measured at the lumbar spine (L1–L4) and on both total hips using DXA (Lunar iDXA, GE Healthcare, Madison, WI, USA). T-scores expressing BMD standard deviations for young, sex-matched healthy adults were generated using the manufacturer’s software. DXA quality assurance was performed according to institutional standard operating procedures (SOPs) and through daily calibration scans with a specific phantom as recommended by the manufacturer.
Hand grip force
Hand grip force was measured during isotonic muscle contractions using a Leonardo Mechanograph® GF (Leonardo software version 4.4, Novotec Medical GmbH, Pforzheim, Germany). Patients were instructed to sit on a chair and place the examination arm flat on the thigh. Six measurements were taken, three with each arm, and the highest value of the six measurements was reported as hand grip force in kg.
Chair rising test
Chair rising test was performed using a ground reaction force platform (Leonardo Mechanograph® Ground Reaction Force Platform STD, Novotec Medical GmbH, Pforzheim, Germany) in conjunction with the supplied software (Leonardo v4.4, Novotec Medical GmbH, Pforzheim, Germany) [23]. Patients were instructed to sit on a bench (45 cm), place their feet shoulder-width apart on the platform and cross their arms over their bodies in front of their chests. From the seated position, patients were then asked to stand up and sit down again as quickly as possible for five repetitions. The time per stand-up cycle and the maximum stand-up force of both legs were calculated using the device.
Biochemical analysis
Serum laboratory parameters of bone metabolism including calcium, phosphate, alkaline phosphatase (ALP), bone-specific alkaline phosphatase (b-ALP), osteocalcin, parathyroid hormone (PTH) and 25-hydroxyvitamin D3 (25(OH)D3) as well as urinary deoxypyridinoline per creatinine (DPD/Crea) were measured at both baseline and follow-up.
Statistical analysis
Statistical analyses were performed using SPSS software version 27.0 (IBM Corp., Armonk, NY, USA). Quantitative characteristics are expressed as mean ± standard deviation (SD). The Kolmogorov–Smirnov test was applied to test normal distribution. To ensure comparability of the therapy groups, propensity score-matching was performed between the Dmab and the basic therapy group with respect to the parameters of sex, age, BMI, and follow-up time. Data were analyzed by analysis of variance (ANOVA) with post hoc analysis (Scheffé test). Paired t-tests were used to investigate the differences in mean laboratory values between the appointments at baseline and follow-up measurements. Correlation analyses were conducted using Pearson’s correlation to evaluate associations of changes in laboratory parameters, DXA measurements and changes in physical performance parameters. The significance level was set at p < 0.05.
Results
An overview of the baseline characteristics of the study population (n = 150 patients, 130 women, 20 men) is presented in Table 1. The study cohort consisted of postmenopausal women and men over 50 years of age who had DXA values in the range of osteoporosis or osteopenia. The mean follow-up period was 17.6 ± 9.0 months (minimum 8 months, maximum 59 months). Propensity score-matching ensured that the basic therapy group and the Dmab group did not differ in sex, age, BMI, and follow-up time (all p > 0.05). The BP group also did not differ in these parameters from both the basic therapy and Dmab group (all p > 0.05). Biochemical mean values of serum calcium, phosphate, 25(OH)D3 and DPD showed no significant differences between the treatment groups at baseline. Mean values of serum PTH (p = 0.038), ALP (p = 0.002), b-ALP (p = 0.006), and osteocalcin (p < 0.001) were different between the three groups. Post hoc analysis showed that these parameters were lower in the Dmab group compared to the basic group, whereas no differences were evident between the BP and the basic group. In all treatment groups, DXA measurements revealed low mean BMD values indicated by T-scores. While no significant differences existed in femoral BMD or T-score, spinal BMD but not T-score was slightly lower in the BP group (Table 1). Regarding muscle performance tests, mean hand grip force and CRT time/cycle were not significantly different in all treatment groups. Mean CRT force was slightly higher in the basic group compared to both anti-resorptive treatment groups (basic vs. BP: p = 0.002; basic vs. Dmab: p = 0.025).
At follow-up, 25(OH)D3 levels increased significantly in both the baseline group (p = 0.001) and the Dmab group (p < 0.001), whereas they remained constant in the BP group (Fig. 1A). The mean annual percentage changes in both femoral and spinal BMD were higher in the Dmab and BP group and were significantly higher compared to the basic group (mean femoral BMD in %change/year: basic = − 0.78% ± 2.12%; BP = + 0.68% ± 2.54%; Dmab = + 1.83% ± 2.66% and mean spinal BMD in %change/year: basic = − 0.04% ± 2.70%; BP = + 2.33% ± 4.79%; Dmab = + 3.30% ± 4.36%) (Fig. 1B, C).
Serum 25-hydroxyvitamin D3 (25(OH)D3) levels and annual percentage changes in DXA results comparing the three treatment groups (basic vs. bisphosphonates (BP) vs. denosumab (Dmab)). (A) Mean serum 25(OH)D3 values at baseline (BL) and follow-up (FU). (B) Comparison of mean annual percentage changes in femoral BMD (in %change/year). (C) Comparison of mean annual percentage changes in spinal BMD (in %change/year). P-values are indicated above the boxplots
The mean annual percentage change in hand grip force demonstrated an increase in both anti-resorptive treatment groups and a decrease in the basic group (mean hand grip force in %change/year: basic = − 6.05% ± 10.22%; BP = + 0.78% ± 8.23%; Dmab = + 5.14% ± 25.49%) (Fig. 2A). These changes were significantly higher in both the Dmab and BP groups compared to the basic group. The mean annual percentage change in CRT force was higher in the Dmab group compared to the BP group, with no significant differences between the other groups (mean CRT force in %change/year: basic = + 5.82 ± 12.74%; BP = + 0.95 ± 8.61%; Dmab = + 8.20 ± 14.38%) (Fig. 2B). The mean annual percentage changes in CRT time showed no differences between the three study groups. (Fig. 2C).
Annual percentage changes of upper and lower limb muscle performance comparing the three treatment groups (basic vs. bisphosphonates (BP) vs. denosumab (Dmab)). (A) Mean annual percentage changes in hand grip force (GF in %change/year). (B) Mean annual percentage changes in chair rising test (CRT) force in %change/year. (C) Mean annual percentage changes in CRT time in %change/year. P-values are indicated above the boxplots
To identify possible influencing factors of altered muscle performance, the annual percentage changes in hand grip force and CRT force were correlated with the annual percentage changes in femoral and spinal BMD as well as the annual percentage changes in various bone metabolism markers. No significant correlations between the annual percentage changes in hand grip force/CRT force and femoral/spinal BMD could be detected (Fig. 3A, B), which also accounted for the individual treatment groups (Supplementary Fig. 1A–F). We also correlated the annual percentage changes in hand grip force and CRT force with bone metabolism markers, finding only one significant negative correlation between the annual percentage change in calcium levels and the annual percentage change in CRT force (r = -0.243; p = 0.006) (Fig. 3C–F, Supplementary Fig. 2).
Associations between mean annual percentage changes in muscle performance measures and DXA/laboratory results for the entire study cohort. (A) Correlation between mean annual percentage changes in chair rising test (CRT) force/grip force (GF) and femoral BMD. (B) Correlation between mean annual percentage changes in chair rising test (CRT) force/grip force (GF) and spinal BMD. (C) Correlation between mean annual percentage changes in chair rising test (CRT) force/grip force (GF) and serum calcium. (D) Correlation between mean annual percentage changes in chair rising test (CRT) force/grip force (GF) and vitamin D (25(OH)D3). (E) Correlation between mean annual percentage changes in chair rising test (CRT) force/grip force (GF) and bone-specific alkaline phosphatase (b-ALP). (F) Correlation between mean annual percentage changes in chair rising test (CRT) force/grip force (GF) and urinary deoxypyridinoline per creatinine (DPD/Crea). Linear correlation analysis was performed in all panels. Bold indicates statistical significance (p < 0.05)
Discussion
In addition to the established benefits of RANKL inhibition on bone mass and fracture risk in the context of osteoporosis treatment, there is emerging evidence of its beneficial effects on skeletal muscle. Mechanistic aspects of RANKL inhibition and skeletal muscle function have previously been demonstrated in osteoporotic mice, in which improved muscle performance was revealed following OPG and Dmab treatment [19]. However, detailed data in patients in larger cohorts with differentiation of site-specific effects and influencing factors were hitherto not available. Therefore, the aim of our study was to investigate the effect of Dmab on upper and lower extremity muscle performance in elderly patients with low BMD in comparison to BP and basic therapy. We demonstrated in a cohort of 150 patients with low BMD that Dmab results in increased muscle strength in the upper and lower limbs, indicating systemic rather than site-specific effects as compared to BP. This improvement in muscle performance did not appear to be associated with changes in bone mass or laboratory markers of bone metabolism.
To date, few animal and human studies have examined the relationship between Dmab and muscle function. Bonnet et al. showed improvement in muscle function associated with increased muscle mass and decreased antimyogenic and inflammatory gene expression in mice as well as improved grip force in postmenopausal women treated with Dmab (n = 18) [19]. Phu et al. compared strength, balance, and physical performance in elderly patients receiving anti-resorptive therapy during a six-month observation period and found a significant increase in multidirectional mobility and a significant decrease in fear of falling with Dmab (n = 51) versus zoledronic acid (n = 28) [24]. Further clinical results confirmed the positive effects of both Dmab (n = 15) and BP (n = 25) on skeletal muscle mass and function in elderly patients with hip fractures, with no significant differences between treatment groups [25]. More recently, Miedany et al. demonstrated a significantly lowered fall risk associated with improvement in physical performance and muscle strength under Dmab compared to BP treatment [21]. Importantly, Dmab discontinuation resulted in worsening of fall risk and muscle performance measures, supporting the hypothesis that Dmab affects bone and muscle tissue reciprocally, even concerning pharmacotherapeutic rebound effects. Finally, a pooled analysis from five studies including postmenopausal women, men with osteoporosis as well as breast and prostate cancer patients, detected a significant decrease in falls compared to placebo, indicating a possible benefit on muscle strength and balance [26]. These collective data provide increasing evidence of potential beneficial effects of anti-resorptive agents on general muscle strength, but studies have largely been limited to small cohorts or are limited to observational aspects of fall risk.
To further investigate the potential beneficial effect of denosumab on muscle performance, we here assessed upper and lower limb muscle performance in 150 osteopenic or osteoporotic patients receiving basic therapy, bisphosphonates, or denosumab. In general, the results of our study are consistent with the literature. Interestingly however, both Dmab and BP were associated with improved hand grip force. Dmab additionally resulted in a significant increase in CRT force compared to BP, implying a systemic effect on both upper and lower limbs. Specifically, the positive effect of Dmab on CRT force (i.e., lower limb muscle performance) may explain the decreased risk of falls reported in previous studies [26]. As a potential confounding factor, 25(OH)D3 levels increased in the basic and Dmab group at follow-up, whereas they remained constant in the BP group. In this context, it is important to note that two meta-analyses revealed a modest positive effect of vitamin D supplementation on global muscle strength [27] and a positive effect on lower limb muscle strength alone [28]. Nonetheless, we could not find an association between the changes of 25(OH)D3 and muscle strength.
We additionally examined the relationship between changes in muscle performance and changes in BMD and laboratory markers of bone metabolism to further investigate possible influencing factors. We did not find associations regarding changes in femoral or spinal BMD, 25(OH)D3, or bone remodeling parameters. Notably, while a potential impact of excessive bone resorption on muscle function was previously discussed [29], a negative association between serum bone resorption marker C-terminal telopeptide (CTX) and lower limb muscle strength has been reported [30]. Here, we evaluated treatment-related changes rather than cross-sectional data, which could explain these potentially conflicting results. Furthermore, we assessed urinary DPD instead of serum CTX. The relevance of the detected negative linear association between changes in serum calcium levels and CRT force remains questionable, but it is possible that lower serum calcium as a result of the anti-resorptive treatment may affect muscle function. While neither marked hypo- nor hypercalcemia were observed in our patients, both conditions are associated with loss of muscle function (muscle tetany and muscle atony, respectively) [31].
There are limitations of our study that need to be mentioned. The retrospective and observational study design exposes potential weaknesses regarding comparability of treatment groups, as denosumab is generally used in patients at higher risk of fracture. Propensity score-matching was one way to minimize this source of error. In addition, some of the patients were already on anti-resorptive treatment prior to the baseline assessment, which may mask the validity on possible time-specific effects. Finally, the small sample must be acknowledged as a clear limitation of our study. Nonetheless, our results may provide further motivation to investigate the effect of RANKL inhibition by denosumab on muscle performance by means of randomized-controlled trials. Of note, there are other examples in musculoskeletal research in which randomized controlled trials have confirmed the results of smaller observational studies related to repurposing of bone-specific drugs, including the finding that bisphosphonates are effective for painful bone marrow lesions [32, 33].
In conclusion, our results suggest that Dmab has a superior effect on muscle strength compared to BP, likely not directly related to its effects on the skeleton. Therefore, Dmab might be preferred in patients with osteosarcopenia to improve muscle performance and to limit fall risk. Prospective studies are now needed to validate our results. Further investigation of muscle-bone crosstalk and, in particular, the OPG/RANKL/RANK pathway is needed to elucidate how Dmab affects skeletal muscle tissue.
References
Smith E, Hoy DG, Cross M, Vos T, Naghavi M, Buchbinder R, Woolf AD, March L (2014) The global burden of other musculoskeletal disorders: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis 73:1462–1469
Sanchez-Riera L, Carnahan E, Vos T, Veerman L, Norman R, Lim SS, Hoy D, Smith E, Wilson N, Nolla JM, Chen JS, Macara M, Kamalaraj N, Li Y, Kok C, Santos-Hernandez C, March L (2014) The global burden attributable to low bone mineral density. Ann Rheum Dis 73:1635–1645
Beaudart C, Rizzoli R, Bruyere O, Reginster JY, Biver E (2014) Sarcopenia: burden and challenges for public health. Arch Public Health 72:45
Girgis CM (2015) Integrated therapies for osteoporosis and sarcopenia: from signaling pathways to clinical trials. Calcif Tissue Int 96:243–255
Binkley N, Buehring B (2009) Beyond FRAX: it’s time to consider “sarco-osteopenia.” J Clin Densitom 12:413–416
Clynes MA, Gregson CL, Bruyere O, Cooper C, Dennison EM (2021) Osteosarcopenia: where osteoporosis and sarcopenia collide. Rheumatology (Oxford) 60:529–537
Teng Z, Zhu Y, Teng Y, Long Q, Hao Q, Yu X, Yang L, Lv Y, Liu J, Zeng Y, Lu S (2021) The analysis of osteosarcopenia as a risk factor for fractures, mortality, and falls. Osteoporos Int 32:2173–2183
Frisoli A Jr, Chaves PH, Ingham SJM, Fried LP (2011) Severe osteopenia and osteoporosis, sarcopenia, and frailty status in community-dwelling older women: results from the Women’s Health and Aging Study (WHAS) II. Bone 48:952–957
Raisz LG (2005) Pathogenesis of osteoporosis: concepts, conflicts, and prospects. J Clin Invest 115:3318–3325
Kirk B, Zanker J, Duque G (2020) Osteosarcopenia: epidemiology, diagnosis, and treatment-facts and numbers. J Cachexia Sarcopenia Muscle 11:609–618
Dankbar B, Fennen M, Brunert D, Hayer S, Frank S, Wehmeyer C, Beckmann D, Paruzel P, Bertrand J, Redlich K (2015) Myostatin is a direct regulator of osteoclast differentiation and its inhibition reduces inflammatory joint destruction in mice. Nat Med 21:1085–1090
Colaianni G, Cuscito C, Mongelli T, Pignataro P, Buccoliero C, Liu P, Lu P, Sartini L, Di Comite M, Mori G, Di Benedetto A, Brunetti G, Yuen T, Sun L, Reseland JE, Colucci S, New MI, Zaidi M, Cinti S, Grano M (2015) The myokine irisin increases cortical bone mass. Proc Natl Acad Sci U S A 112:12157–12162
Mera P, Laue K, Wei J, Berger JM, Karsenty G (2016) Osteocalcin is necessary and sufficient to maintain muscle mass in older mice. Mol Metab 5:1042–1047
Huang J, Romero-Suarez S, Lara N, Mo C, Kaja S, Brotto L, Dallas SL, Johnson ML, Jahn K, Bonewald LF, Brotto M (2017) Crosstalk between MLO-Y4 osteocytes and C2C12 muscle cells is mediated by the Wnt/beta-catenin pathway. JBMR plus 1:86–100
He C, He W, Hou J, Chen K, Huang M, Yang M, Luo X, Li C (2020) Bone and muscle crosstalk in aging. Front Cell Dev Biol 8:585644
Lacey DL, Boyle WJ, Simonet WS, Kostenuik PJ, Dougall WC, Sullivan JK, San Martin J, Dansey R (2012) Bench to bedside: elucidation of the OPG-RANK-RANKL pathway and the development of denosumab. Nat Rev Drug Discov 11:401–419
Dufresne SS, Dumont NA, Boulanger-Piette A, Fajardo VA, Gamu D, Kake-Guena S-A, David RO, Bouchard P, Lavergne É, Penninger JM (2016) Muscle RANK is a key regulator of Ca2+ storage, SERCA activity, and function of fast-twitch skeletal muscles. Am J Physiol Cell Physiol 310:C663–C672
Hamoudi D, Marcadet L, Piette Boulanger A, Yagita H, Bouredji Z, Argaw A, Frenette J (2019) An anti-RANKL treatment reduces muscle inflammation and dysfunction and strengthens bone in dystrophic mice. Hum Mol Genet 28:3101–3112
Bonnet N, Bourgoin L, Biver E, Douni E, Ferrari S (2019) RANKL inhibition improves muscle strength and insulin sensitivity and restores bone mass. J Clin Invest 129:3214–3223
Phu S, Bani Hassan E, Vogrin S, Kirk B, Duque G (2019) Effect of denosumab on falls, muscle strength, and function in community-dwelling older adults. J Am Geriatr Soc 67:2660–2661
Miedany YE, Gaafary ME, Toth M, Hegazi MO, Aroussy NE, Hassan W, Almedany S, Nasr A, Bahlas S, Galal S (2021) Is there a potential dual effect of denosumab for treatment of osteoporosis and sarcopenia? Clin Rheumatol 40:4225–4232
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 12:1495–1499
Rupp T, Butscheidt S, Jahn K, Simon MJ, Mussawy H, Oheim R, Barvencik F, Amling M, Rolvien T (2018) Low physical performance determined by chair rising test muscle mechanography is associated with prevalent fragility fractures. Arch Osteoporos 13:71
Rossini A, Frigerio S, Dozio E, Trevisan R, Perseghin G, Corbetta S (2020) Effect of denosumab on glucose homeostasis in postmenopausal women with breast cancer treated with aromatase inhibitors: a pilot study. Int J Endocrinol 2020:1809150
Pizzonia M, Casabella A, Natali M, Petrocchi L, Carmisciano L, Nencioni A, Molfetta L, Giannotti C, Bianchi G, Giusti A, Santolini F, Monacelli F (2021) Osteosarcopenia in very old age adults after hip fracture: a real-world therapeutic standpoint. Front Med (Lausanne) 8:612506
Chotiyarnwong P, McCloskey E, Eastell R, McClung MR, Gielen E, Gostage J, McDermott M, Chines A, Huang S, Cummings SR (2020) A pooled analysis of fall incidence from placebo-controlled trials of denosumab. J Bone Miner Res 35:1014–1021
Beaudart C, Buckinx F, Rabenda V, Gillain S, Cavalier E, Slomian J, Petermans J, Reginster JY, Bruyere O (2014) The effects of vitamin D on skeletal muscle strength, muscle mass, and muscle power: a systematic review and meta-analysis of randomized controlled trials. J Clin Endocrinol Metab 99:4336–4345
Zhang L, Quan M, Cao ZB (2019) Effect of vitamin D supplementation on upper and lower limb muscle strength and muscle power in athletes: a meta-analysis. PLoS ONE 14:e0215826
Trivedi T, Guise TA (2022) Systemic effects of abnormal bone resorption on muscle, metabolism, and cognition. Bone 154:116245
Kirk B, Lieu N, Vogrin S, Sales M, Pasco JA, Duque G (2022) Serum levels of C-terminal telopeptide (CTX) are associated with muscle function in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. https://doi.org/10.1093/gerona/glac008
Kasperk C (2017) Hypercalcemic crisis and hypocalcemic tetany. Internist (Berl) 58:1029–1036
Bartl C, Imhoff A, Bartl R (2012) Treatment of bone marrow edema syndrome with intravenous ibandronate. Arch Orthop Trauma Surg 132:1781–1788
Seefried L, Genest F, Baumann J, Heidemeier A, Meffert R, Jakob F (2022) Efficacy of zoledronic acid in the treatment of nonmalignant painful bone marrow lesions: a triple-blind, randomized, placebo-controlled phase III clinical trial (ZoMARS). J Bone Miner Res 37:420–427
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Study design: T Rolvien. Study conduct: EVV, T Rupp, RO, FB, MA and T Rolvien. Data analysis: EVV, T Rupp and AS. Drafting Manuscript: EVV, T Rupp and T Rolvien. Revising Manuscript: All authors. EVV, T Rupp and T Rolvien take responsibility for the integrity of the data analysis.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval for this retrospective study was obtained from the local ethics committee. The study reports according to the STROBE guidelines for reporting observational studies. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Tobias Rupp, Emil von Vopelius, André Strahl, Florian Barvencik, Michael Amling and Tim Rolvien declare that they have no conflict of interest. Ralf Oheim has served as a speaker and advisory board member for Kyowa Kirin, Inozyme and UCB and has received an institutional research grant from Kyowa Kirin and UCB.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Rupp, T., von Vopelius, E., Strahl, A. et al. Beneficial effects of denosumab on muscle performance in patients with low BMD: a retrospective, propensity score-matched study. Osteoporos Int 33, 2177–2184 (2022). https://doi.org/10.1007/s00198-022-06470-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06470-3