Abstract
Background
A negative impact of premature birth on health in adulthood is well established. However, it is not clear whether healthy adults who were born prematurely but have similar physical activity levels compared to adults born at term have a reduced maximal aerobic exercise capacity (maximum oxygen consumption [VO2max]).
Objective
We aimed to determine the effect of premature birth on aerobic exercise capacity and lung function in otherwise healthy, physically active individuals.
Methods
A broad literature search was conducted in the PubMed database. Search terms included ‘preterm/premature birth’ and ‘aerobic exercise capacity’. Maximal oxygen consumption (mL/kg/min) was the main variable required for inclusion, and amongst those investigations forced expiratory volume in 1 s (FEV1, % predicted) was evaluated as a secondary parameter. For the systematic review, 29 eligible articles were identified. Importantly, for the meta-analysis, only studies which reported similar activity levels between healthy controls and the preterm group/s were included, resulting in 11 articles for the VO2max analysis (total n = 688, n = 333 preterm and n = 355 controls) and six articles for the FEV1 analysis (total n = 296, n = 147 preterm and n = 149 controls). Data were analysed using Review Manager ( Review Manager. RevMan version 5.4 software. The Cochrane Collaboration; 2020.).
Results
The systematic review highlighted the broad biological impact of premature birth. While the current literature tends to suggest that there may be a negative impact of premature birth on both VO2max and FEV1, several studies did not control for the potential influence of differing physical activity levels between study groups, thus justifying a focused meta-analysis of selected studies. Our meta-analysis strongly suggests that prematurely born humans who are otherwise healthy do have a reduced VO2max (mean difference: − 4.40 [95% confidence interval − 6.02, − 2.78] mL/kg/min, p < 0.00001, test for overall effect: Z = 5.32) and FEV1 (mean difference − 9.22 [95% confidence interval − 13.54, − 4.89] % predicted, p < 0.0001, test for overall effect: Z = 4.18) independent of physical activity levels.
Conclusions
Whilst the current literature contains mixed findings on the effects of premature birth on VO2max and FEV1, our focused meta-analysis suggests that even when physical activity levels are similar, there is a clear reduction in VO2max and FEV1 in adults born prematurely. Therefore, future studies should carefully investigate the underlying determinants of the reduced VO2max and FEV1 in humans born preterm, and develop strategies to improve their maximal aerobic capacity and lung function beyond physical activity interventions.
Similar content being viewed by others
Although premature birth is known to have negative effects in adult life, there is mixed evidence on the impact of premature birth on maximal aerobic exercise capacity. |
This systematic review indicates that the effects reported in previous studies may have been influenced by the level of physical activity. |
Our focused meta-analysis indicates that, when physical activity is accounted for, premature birth still has a negative impact on maximal aerobic exercise capacity. |
1 Introduction
Maximal aerobic exercise capacity is an important predictor of health, as reflected by the associations between maximal oxygen consumption (VO2max), an established indicator of cardiorespiratory fitness, and life expectancy [2, 3]. A number of factors can improve cardiorespiratory fitness [4], including regular exercise training. However, some studies have proposed that an individual’s maximal exercise capacity could be limited as a result of premature birth. Conversely, other studies have reported little or no impact of premature birth on VO2max, or indeed a positive effect [5,6,7].
While normal gestation period/birth term is noted at 40 weeks, individuals who are born prematurely are born at less than 37 weeks of gestation [8]. Preterm birth is sub-categorised further into; extremely preterm (less than 28 weeks gestation), very preterm (28–32 weeks), and moderate-to-late preterm (32–37 weeks) [9]. It is estimated that of those individuals born alive, 5–18% are born prematurely [9], which equates to roughly “15 million babies each year” [9]. The potentially deleterious effects of preterm birth on full organ development can impact the cardiovascular, pulmonary and respiratory systems [6, 10,11,12,13,14,15,16,17]. Therefore, aerobic exercise capacity can be limited by a reduced oxygen delivery because of cardiac dysfunction or an impaired oxygen uptake due to lower pulmonary development [12, 18,19,20,21,22,23,24,25], or both. Accordingly, pulmonary issues culminating specifically in lung and breathing difficulties in those born preterm have been cited as affecting their maximal aerobic exercise capacity. These issues are clinically expressed as broncho-pulmonary dysplasia (BPD), and evidence has been presented for BPD to cause a reduced maximal oxygen capacity in those born prematurely [26]. Those who are diagnosed with BPD are highly likely to receive supplemental oxygen treatment, and this combined with the potential for mechanical ventilation can cause lung function deficiencies categorised as BPD [6, 10, 27,28,29]. Although gas exchange efficiency may not be affected, it is probable that the work of breathing—and consequently whole-body oxygen consumption—may be altered [30]. Accordingly, adults who were born preterm with BPD are already more likely to have a reduced cardiorespiratory fitness [31, 32]. In contrast, there are numerous individuals born prematurely who do not have BPD, but whether they have a reduced exercise capacity is not clear. Although the majority of previous research implies that being born preterm has a negative impact on lung function and exercise capacity, there is sufficient alternative evidence to suggest that preterm birth may not be a clear factor for reduced VO2max. Furthermore, lung function and exercise capacity may also be influenced by differing physical activity levels between humans born preterm and humans born at term, perhaps explaining why the current literature reports mixed results.
Improving the current understanding of the role of preterm birth on exercise capacity independent of physical activity levels will be of benefit to athletes, patients, medical practitioners and coaches. Therefore, this study aimed to carefully scrutinise the current literature (systematic review) and determine the effects of preterm birth on VO2max and forced expiratory lung volume in 1 s (FEV1) independent of prevailing physical activity levels (focused meta-analysis).
2 Methods
2.1 Literature Search
The literature search was conducted according to the Preferred Reporting Items for Systematic review and Meta-Analyses (PRISMA) 2020 guidelines [33]. NCBI was the primary database used for the literature search, with ResearchGate, Science Direct/Elsevier, TandF-Online, Springer Link and Google Scholar used as additional databases. The relevant literature was identified using different combinations of key search terms such as “premature birth”, “maximal aerobic exercise capacity” and “endurance running performance”. The literature search was conducted including the time period from January 2000 to August 2021.
2.2 Article Inclusion and Exclusion Criteria
Articles were eligible if they included both preterm and control groups within their studies. For the purpose of this systematic review and meta-analysis, and in accordance with the literature, we defined preterm individuals as those born at < 37 weeks gestation and an explicit documentation of not having been diagnosed with BPD. The control group was defined as those individuals born at ≥ 37 weeks gestation. The main parameter of interest was VO2max (mL/kg/min), indicative of maximal aerobic exercise capacity. To determine whether—in the same original investigations—lung function was also affected by preterm birth, we included FEV1 (% predicted) as a secondary parameter. Articles had to report VO2max, with FEV1 as a potential secondary parameter of interest to co-inform the outcome related to VO2max.
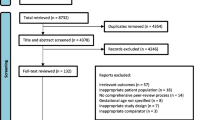
The results of the initial literature search revealed key themes that the majority of the current evidence could be categorised into: cardiovascular effects, pulmonary effects, respiratory effects and exercise/physical activity participation effects. Accordingly, these themes were added to the next phase of the literature search. This involved the addition of the themes into the initial search terms. This process was cyclical to ensure that a comprehensive literature search was conducted, and that selection bias remained as low as possible. The process is summarised in Fig. 1, and, following the preliminary screening of articles by one investigator (T.G.), the checking of the inclusion and exclusion criteria and of relevant data by both investigators, and the removal of duplicates, authors of two articles were contacted and asked for some of the data in different units. However, no response was received and hence the data could not be included within the review. Both investigators re-affirmed the included articles’ eligibility. In the end, 29 articles were included in the systematic review (see Table 1 and Fig. 1).
Flow diagram showing the literature selection process in accordance with the 2020 Preferred Reporting Items for Systematic review and Meta-Analyses (PRISMA) guidelines [33]. BPD broncho-pulmonary dysplasia, VO2max maximal oxygen consumption
Within the articles included in this review, the majority of the preterm participants were in the very preterm category (28–32 weeks), with a small number of the selected articles investigating moderate-to-late preterm (32–36 weeks) and an even smaller proportion of articles investigating individuals born extremely preterm (< 28 weeks). The age of assessment for the majority of articles ranged from 18 to 40 years. A small number of articles investigated children and adolescents aged 3–18 years, and a very small proportion of the included articles assessed the participants within a few days/weeks of birth.
2.3 Meta-analysis: Selection Criteria Data Analysis
For the meta-analysis, additional inclusion and exclusion criteria were predefined to reduce the number of confounding factors and advance our knowledge beyond the mere summary of the current literature. Specifically, the included articles were required to report either only VO2max or both VO2max and FEV1 in the units of mL/kg/min and % predicted, respectively. In the original articles, VO2max needed to be obtained via a treadmill, cycle ergometer or a shuttle run test. The FEV1 data were collected using either a Vmax 22 spirometer or pneumotachograph. Articles were only included for the meta-analysis if they included both male and female participants. Importantly, whilst regular exercise was not an inclusion criterion, an indication of similar exercise participation between the study groups was necessary to avoid the confounding influence of different exercise participation. Therefore, original studies were required to have conducted a survey using a physical activity questionnaire, and studies were only included if (1) there was a quantified report of physical activity in both study groups and (2) there was no significant difference in physical activity between the two relevant study groups. Both investigators screened the remaining articles for inclusion in the meta-analysis, matching the data provided with the eligibility criteria. As a result, a total of 11 articles were eligible that reported VO2max, and of those, a total of six articles reported FEV1. For these articles, mean and standard deviation for VO2max and for FEV1, along with the sample size of both the preterm and the control group within each article were extracted and collated in an Excel spreadsheet [34]. Across the 11 articles included in the meta-analysis of VO2max, a total of 688 participants were included, with a split of 333 born preterm, and 355 in the control group born at term. Across the six articles included in the meta-analysis of FEV1, a total of 296 participants were included, with 147 born preterm and 149 controls born at term.
Data were treated as continuous variables, and for each parameter a random-effects analysis was performed in Review Manager (RevMan, version 5.4) [1]. The analysis included weighting, alongside a heterogeneity score and the overall effect. Results are reported as the mean difference with 95% confidence intervals (see Figs. 2 and 3).
Forest plot for maximal oxygen consumption (VO2max). Adults born preterm had a significantly lower VO2max than those born at term. Importantly, following removal of original studies that did not report physical activity levels in the study groups six out of 11 studies still had a non-significant difference. However, the overall effect of all 11 studies reveals that adults born preterm had a significantly lower VO2max. Total 95% confidence interval (CI) − 4.40 (− 6.02, − 2.78), heterogeneity: Tau2 = 2.36; Chi2 = 14.99, df = 10 (p = 0.13); I2 = 33%, test for overall effect: Z = 5.32 (p < 0.00001). IV inverse variance
Forest plot for forced expiratory volume in 1 s (FEV1). In the selected studies, those born preterm had a consistently lower FEV1. Total 95% confidence interval (CI) − 9.22 (− 13.54, − 4.89), heterogeneity: Tau2 = 13.54; Chi2 = 9.83, df = 5 (p = 0.08); I2 = 49%, test for overall effect: Z = 4.18 (p < 0.0001). IV inverse variance
3 Results
3.1 Systematic Review
Following the review of the 29 articles, and a categorisation of the outcomes into effects related to maximal aerobic capacity (based upon VO2max) and to lung function (based upon FEV1), the main trends were noted (see Table 1). There, it can be noted that the majority of previously completed original studies indicated that prematurity may have a negative effect on both VO2max and FEV1. However, several studies also reported no significant impact of preterm birth on VO2max, and one article suggested a positive effect. Conversely, more consistent evidence appears to exist for FEV1, with 76% (13 out of 17) of the studies that report FEV1 findings concluding that preterm birth was associated with a lower FEV1 compared with healthy controls.
3.2 Meta-analysis
Data are shown in Figs. 2 and 3. When analysed for those studies that reported similar physical activity levels between the study groups, our meta-analysis indicated that adults born preterm had a significantly lower VO2max compared with those born preterm without BPD and similar activity levels (mean difference − 4.40 [95% CI − 6.02, − 2.78] mL/kg/min, p < 0.00001, test for overall effect: Z = 5.32). Similarly, FEV1 was significantly lower in humans born preterm without BPD and similar activity levels (mean difference: − 9.22 [95% CI − 13.54, − 4.89] % predicted, p < 0.0001, test for overall effect: Z = 4.18).
4 Discussion
In relation to the main objective, this study found that both VO2max and FEV1 are significantly reduced in young adults born prematurely. Importantly, these results are based upon comparisons between individuals with similar physical activity levels. Thus, the present study extends the previous knowledge and highlights the need to understand the precise origins and mechanisms that lead to the reduced aerobic capacity, and potential interventions to counter the negative effect, as discussed in more detail below.
4.1 Reduced Maximal Aerobic Exercise Capacity: A Problem of O2 Delivery, Ventilation or Local O2 Uptake?
In general, the factors that influence VO2max are numerous, as investigations in patients with heart failure have highlighted [35, 36]. Given the different time course of organ developments during foetal gestation [37], it is possible that a reduced VO2max may be caused by (1) an underdeveloped heart and reduced cardiac function, resulting in lower O2 delivery, (2) underdeveloped lungs and a reduced ventilatory capacity, or (3) disruption of normal mitochondrial function, thereby affecting the local O2 uptake to metabolically active tissues. In relation to reduced cardiac function, Hirose et al. [13] reported a negative effect of prematurity on diastolic filling of the left ventricle, likely caused by an immature myocardium [14, 38, 39]. Similarly, data from Crispi et al. [38] and McKay et al. [40] indicate that the impaired early filling was accompanied by a reduced cardiac output, suggesting that the heart of prematurely born humans likely provides a reduced blood supply to working muscles during exercise, which would impair aerobic exercise capacity [41, 42]. Whether the reduced stroke volume previously reported is simply an effect of the smaller left ventricle because of reduced filling [43, 44] (and thus indicating more of a systemic influence of the circulating blood volume instead of impaired heart muscle function itself), or whether there is an intrinsic impairment in myocardial contraction and/or relaxation remains to be determined.
Another potential influence on the output of the heart could be blood pressure. Bennet et al. [45] and Crispi et al. [38] have suggested that prematurity impairs the adequate response to drops in blood pressure. This could be an issue during exercise, when the reduction in arterial resistance should assist the heart in providing a greater stroke volume, and hence the cardiac output. If there was indeed a problem with an increase in cardiac output during exercise that was disproportionate to the reduction in vascular resistance, an involvement of the heart muscle itself, and not (just) peripheral circulatory complications, becomes likely. Equally, the aforementioned reduction in diastolic function could indicate an intrinsic problem with the heart muscle itself; and not only with the left side of the heart but also the right side [46]. This could be caused secondary to a reduced systolic function, or independently. The interdependence between the different organ systems is particularly evident during the whole-body effort of exercise. However, there are also indications that different organ systems may be involved to different extents in humans born preterm. For example, some studies have reported a lower aerobic capacity despite similar pulmonary function [12]. Haraldsdottir et al. [12] and Goss et al. [46] suggested that this may be linked to the lower cardiac index at 50% and 100% of maximal workload. However, without additional cardiac measurements, for example myocardial strain and twist, these data do not indicate whether there is a reduction in intrinsic cardiac muscle function, or whether the problem lies more in the peripheral circulation.
An interesting aspect raised by Horsberg Eriksen et al. [14] is the diagnostic potential of exercise tests in adults born prematurely. In their study, Horsberg Eriksen et al. [14] reported a similar myocardial function at rest but a slightly lower function during exercise. These data highlight two important points. First, they indicate that the heart may indeed be affected, but only in a stressed state, such as during exercise, when an increased whole-body energetic demand must be covered. Second, exercise tests may be able to discriminate between individuals at risk that cannot be detected just at rest. This fits with the previous suggestion of using exercise tests to stress the heart of pregnant women to determine the progression of their pregnancy [47]. We now speculate that, perhaps, this may even extend to a prediction of premature birth and subsequent health of the baby as it develops into adulthood. Considering the well-known generation-spanning effect of some maternal biology, this hypothesis may not be as bold as it may initially sound.
Perhaps less surprising is our finding of a reduced lung function, as represented by FEV1. However, we purposefully excluded any studies with patients who had been diagnosed with BPD. Therefore, there appear to be limitations in lung function that may not be strictly linked to structural underdevelopments or damage of alveolar tissue caused by premature birth. Indeed, Farrell et al. [48] have suggested that a lower pulmonary gas exchange efficiency caused by higher pulmonary resistance was only present in a minority of individuals. Therefore, it could be that the reduced FEV1 confirmed in our study may reflect an increased work of breathing, which in turn has been associated with alterations in whole-body metabolism [30]. Similarly, Laurie et al. [20] proposed that an increased pulmonary resistance can increase pulmonary artery pressure as a natural response to exercise, which could cause pulmonary hypertension in premature individuals. Greater resistance implies a reduced volume of oxygen per time may transit through the lungs, which is supported by a low PaO2 and a high A-aDO2 during exercise under normoxic conditions at a high intensity, thus contributing to the reduced aerobic capacity [42]. As Laurie et al. [20] suggested, prematurely arrested lung development is a factor that can cause difficulty in responding to blood pressure changes [45] and can be accompanied by pulmonary hypertension secondary to reduced lung sizes, closed blood vessels and congestion of amniotic fluid that is harder to displace [17, 49]. Considering that exercise disproportionately increases pulmonary pressures and, therefore, stress on the right ventricle, premature birth may further exacerbate this effect during physical effort. Consequently, the circulatory issues may not only impact venous return during exercise, but also the transfer of blood to the left ventricle. Halvorsen et al. [11] additionally found an increased sensitivity to respiratory conditions, including asthma and bronchial hyperresponsiveness that contributed to a reduced FEV1. As these respiratory conditions can cause airway inflammation and subsequently a restriction in VO2, they too may contribute to the lower VO2max and FEV1 observed in our study.
The reduced aerobic capacity in adults born prematurely could theoretically also be linked to a lower O2 uptake at the level of the tissues. Specifically, mitochondrial density and function may play a role, in particular during exercise. Studies have postulated that impaired alveolar and cerebral white matter development in infants born prematurely may be linked to mitochondrial dysfunction [50], and that adults born preterm may have a (paradoxically) increased mitochondrial O2 consumption [51]. As similarly increased O2 consumption has been reported in diabetic patients, these data indicate a negative metabolic development that could be associated with an increased risk of disease. However, an important modifier that has been explored less in relation to the points discussed so far is lifestyle, in particular exercise training. Ruf et al. [21] found that those who adopted a more sedentary lifestyle involving less moderate vigorous exercise exhibited a decreased VO2, and thus exercise capacity. Lovering et al. [32] demonstrated that those born preterm exercised at lower peak workloads than their peers, typically eliciting a reduced exercise capacity. Similarly, Vrijlandt et al. [52] illustrated that lactate threshold and maximum heart rate appeared lower for those born preterm. Yet their VO2max, rate of perceived exertion and breathing rate were no different to their peers. This further consolidates the notion that careful differentiation is required between the lifestyle of individuals when evaluating the independent effects of premature birth. For these reasons, this meta-analysis presents an important step forward as it shows the effects independent of one major modifier, i.e. physical activity. Consequently, future studies should always determine the physical activity levels and attempt to understand the underlying causes of a reduced aerobic capacity, which may impact human health and performance.
5 Limitations
Despite the greatest efforts to generate a precise account of the effects of preterm birth on maximal aerobic exercise capacity, some limitations were unavoidable. First, it has to be acknowledged that there was not sufficient information available to determine the potential influence of perinatal oxygen administration or different glucocorticoid treatments on adult exercise capacity. In the future, prospective studies examining this influence will be of great value and may explain some of the variability in the current data. Second, we were not able to determine the role of different extents of prematurity, which may also explain some of the variability observed. Third, any systematic review and meta-analysis carries the potential to be influenced by publication bias. In our investigation, the number of studies below and above the mean difference for VO2max was five and six, respectively. The visual inspection of the forest plot did not show any obvious publication bias. Of course, future studies with larger numbers of publications may be needed to fully exclude the possibility of publication bias. For FEV1, there were too few studies to confidently evaluate the possibility of publication bias. Finally, we do not know whether there may be a difference in female and male individuals born prematurely, which is an area of great interest for future studies.
6 Conclusions
Through the means of a systematic review and a focused meta-analysis, this study reveals that human adults born preterm have a reduced VO2max and FEV1 independent of physical activity levels. Consequently, in adults born preterm, exercise interventions may result in a lower benefit compared with adults born at term, and additional therapeutic interventions or higher exercise intensities/volumes may be required.
Change history
09 September 2023
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1007/s40279-023-01935-9
References
Review Manager. RevMan version 5.4 software. The Cochrane Collaboration; 2020. Download and installation RevMan 5 | Cochrane Training.
Strasser B, Burtscher M. Survival of the fittest: VO2max, a key predictor of longevity?’. Front Biosci (Landmark Ed). 2018;23:1505–16. https://doi.org/10.2741/4657.
Harber M, Kaminsky L, Arena R, Blair S, Franklin B, Myers J, et al. Impact of cardiorespiratory fitness on all-cause and disease-specific mortality: advances since 2009. Prog Cardiovasc Dis. 2017;60(1):11–20. https://doi.org/10.1016/j.pcad.2017.03.001.
Foster C. VO2 max and training indices as determinants of competitive running performance. J Sports Sci. 1983;1:13–22. https://doi.org/10.1080/02640418308729657.
Moura-Dos-Santos M, Wellington-Barros J, Brito-Almeida M, Manhães-de-Castro R, Maia J, Góis LC. Permanent deficits in handgrip strength and running speed performance in low-birth-weight children. Am J Hum Biol. 2013;25(1):58–62. https://doi.org/10.1002/ajhb.22341.
Narang I, Bush A, Rosenthal M. Gas transfer and pulmonary blood flow at rest and during exercise in adults 21 years after preterm birth. Am J Respir Crit Care Med. 2009;180(4):339–45. https://doi.org/10.1164/rccm.200809-1523OC.
Vollsæter M, Clemm HH, Satrell E, Eide GE, Røksund OD, Markestad T, et al. Adult respiratory outcomes of extreme preterm birth: a regional cohort study. Ann Am Thorac Soc. 2015;12(3):313–22. https://doi.org/10.1513/annalsats.201406-285oc.
World Health Organization. Newborn health: preterm babies. 2015. https://www.who.int/news-room/q-a-detail/what-is-a-preterm-baby. Accessed 8 Nov 2020.
World Health Organization. Preterm birth. 2018. https://www.who.int/en/news-room/fact-sheets/detail/preterm-birth. Accessed 8 Nov 2020.
Gallacher DJ, Hart K, Kotecha S. Common respiratory conditions of the newborn. Breathe. 2016;12:30–42. https://doi.org/10.1183/20734735.000716.
Halvorsen T, Skadberg B, Eide G, Røksund O, Carlsen K, Bakke P. Pulmonary outcome in adolescents of extreme preterm birth: a regional cohort study. Acta Paediatr. 2004;93:1294–300. https://doi.org/10.1111/j.1651-2227.2004.tb02926.x.
Haraldsdottir K, Watson A, Pegelow D, Palta M, Tetri L, Levin T, et al. Blunted cardiac output response to exercise in adolescents born preterm. Eur J Appl Physiol. 2020;120(11):2547–54. https://doi.org/10.1007/s00421-020-04480-9.
Hirose A, Khoo N, Aziz K, Al-Rajaa N, van den Boom J, Savard W, et al. Evolution of left ventricular function in the preterm infant. J Am Soc Echocardiogr. 2015;28(3):302–8. https://doi.org/10.1016/j.echo.2014.10.017.
Horsberg Eriksen B, Nestaas E, Hole T, Liestøl K, Støylen A, Fugelseth D. Myocardial function in term and preterm infants. Influence of heart size, gestational age and postnatal maturation. Early Hum Dev. 2014;90(7):359–64. https://doi.org/10.1016/j.earlhumdev.2014.04.010.
Huckstep O, Williamson W, Telles F, Burchert H, Bertagnolli M, Herdman C, et al. Physiological stress elicits impaired left ventricular function in preterm-born adults. J Am Coll Cardiol. 2018;71(12):1347–56. https://doi.org/10.1016/j.jacc.2018.01.046.
Näsänen-Gilmore P, Sipola-Leppänen M, Tikanmäki M, Matinolli H, Eriksson J, Järvelin M, et al. Lung function in adults born preterm. PLoS ONE. 2018;13(10):0205979. https://doi.org/10.1371/journal.pone.0205979.
O’Connor M, Cornfield D, Austin E. Pulmonary hypertension in the premature infant. Curr Opin Pediatr. 2016;28(3):324–30. https://doi.org/10.1097/MOP.0000000000000355.
Duke JW, Lewandowski AJ, Abman SH, Lovering AT. Physiological aspects of cardiopulmonary dysanapsis on exercise in adults born preterm. J Physiol. 2022;600:463–82. https://doi.org/10.1113/JP281848.
Gibson A, Doyle L. Respiratory outcomes for the tiniest or most immature infants. Semin Fetal Neonatal Med. 2014;19(2):105–11. https://doi.org/10.1016/j.siny.2013.10.006.
Laurie S, Elliott J, Beasley K, Mangum T, Goodman R, Duke J, et al. Exaggerated increase in pulmonary artery pressure during exercise in adults born preterm. Am J Respir Crit Care Med. 2018;197(6):821–3. https://doi.org/10.1164/rccm.201704-0740LE.
Ruf K, Thomas W, Brunner M, Speer C, Hebestreit H. Diverging effects of premature birth and bronchopulmonary dysplasia on exercise capacity and physical activity: a case control study. Respir Res. 2019;20(1):260. https://doi.org/10.1186/s12931-019-1238-0.
Smith LJ, van Asperen PP, McKay KO, Selvadurai H, Fitzgerald DA. Reduced exercise capacity in children born very preterm. J Am Acad Pediatr. 2008;122(2):e287–93. https://doi.org/10.1542/peds.2007-3657.
Svedenkrans J, Henckel E, Kowalski J, Norman M, Bohlin K. Long-term impact of preterm birth on exercise capacity in healthy young men: a national population-based cohort study. PLoS ONE. 2013;8(12): e80869. https://doi.org/10.1371/journal.pone.0080869.
O’Dea C, Logie K, Wilson A, Pillow J, Murray C, Banton G, et al. Lung abnormalities do not influence aerobic capacity in school children born preterm. Eur J Appl Physiol. 2021;121(2):489–98. https://doi.org/10.1007/s00421-020-04530-2.
Caskey S, Gough A, Rowan S, Gillespie S, Clarke J, Riley M, et al. Structural and functional lung impairment in adult survivors of bronchopulmonary dysplasia. Ann Am Thorac Soc. 2016;13(8):1262–70. https://doi.org/10.1513/AnnalsATS.201509-578OC.
Edwards M, Kotecha S, Lowe J, Watkins W, Henderson A, Kotecha S. Effect of preterm birth on exercise capacity: a systematic review and meta-analysis. Pediatr Pulmonol. 2015;50(3):293–301. https://doi.org/10.1002/ppul.23117.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723. https://doi.org/10.1164/ajrccm.163.7.2011060.
Vrijlandt EJ, Gerritsen J, Boezen HM, Grevink RG, Duiverman EJ. Lung function and exercise capacity in young adults born prematurely. Am J Respir Crit Care Med. 2006;173(8):890–6. https://doi.org/10.1164/rccm.200507-1140oc.
Robič Pikel T, Starc G, Strel J, Kovač M, Babnik J, Golja P. Impact of prematurity on exercise capacity and agility of children and youth aged 8 to 18. Early Hum Dev. 2017;110:39–45. https://doi.org/10.1016/j.earlhumdev.2017.04.015.
Sheel A, Dominelli P. Breathing during exercise: there is no such thing as a free lunch. Exp Physiol. 2019;104(9):1333–4. https://doi.org/10.1113/EP087922.
Duke J, Elliott J, Laurie S, Beasley K, Mangum T, Hawn J, et al. Pulmonary gas exchange efficiency during exercise breathing normoxic and hypoxic gas in adults born very preterm with low diffusion capacity. J Appl Physiol. 2014;117(5):473–81. https://doi.org/10.1152/japplphysiol.00307.2014.
Lovering A, Laurie S, Elliott J, Beasley K, Yang X, Gust C, et al. Normal pulmonary gas exchange efficiency and absence of exercise-induced arterial hypoxemia in adults with bronchopulmonary dysplasia. J Appl Physiol. 2013;115(7):1050–6. https://doi.org/10.1152/japplphysiol.00592.2013.
Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(29):71. https://doi.org/10.1136/bmj.n71.
Microsoft Office Professional Plus (2016). Version 2107.
Houstis NE, Eisman AS, Pappagianopoulos PP, Wooster L, Bailey CS, Wagner PD, et al. Exercise intolerance in heart failure with preserved ejection fraction: diagnosing and ranking its causes using personalized O2 pathway analysis. Circulation. 2018;137(2):148–61. https://doi.org/10.1161/circulationaha.117.029058.
Dhakal BP, Malhotra R, Murphy RM, Pappagianopoulos PP, Baggish AL, Weiner RB, et al. Mechanisms of exercise intolerance in heart failure with preserved ejection fraction: the role of abnormal peripheral oxygen extraction. Circ Heart Fail. 2015;8(2):286–94. https://doi.org/10.1161/CIRCHEARTFAILURE.114.001825.
Rueda-Clausen CF, Morton JS, Davidge ST. The early origins of cardiovascular health and disease: who, when, and how. Semin Reprod Med. 2011;29(3):197–210. https://doi.org/10.1055/s-0031-1275520.
Crispi F, Rodríguez-López M, Bernardino G, Sepúlveda-Martínez Á, Prat-González S, Pajuelo C, et al. Exercise capacity in young adults born small for gestational age. JAMA Cardiol. 2021;6(11):1308–16. https://doi.org/10.1001/jamacardio.2021.2537.
Huckstep O, Burchert H, Williamson W, Telles F, Tan C, Bertagnolli M, et al. Impaired myocardial reserve underlies reduced exercise capacity and heart rate recovery in preterm-born young adults. Eur Heart J Cardiovasc Image. 2021;22(5):572–80. https://doi.org/10.1093/ehjci/jeaa060.
McKay L, Goss K, Haraldsdottir K, Beshish A, Barton G, Palta M, et al. Decreased ventricular size and mass mediate the reduced exercise capacity in adolescents and adults born premature. Early Hum Dev. 2021;160: 105426. https://doi.org/10.1016/j.earlhumdev.2021.105426.
Daniels J, Foster C, Yarbrough R. Changes in VO2 max and running performance with training. Eur J Appl Physiol Occup Physiol. 1978;39(4):249–54. https://doi.org/10.1007/BF00421448.
Jones A, Kirby B, Clark I, Rice H, Fulkerson E, Wylie L, et al. Physiological demands of running at 2-hour marathon race pace. J Appl Physiol. 2020;130(2):369–79. https://doi.org/10.1152/japplphysiol.00647.2020.
Klabunde RE. Cardiovascular physiology concepts. 3rd ed. Philadelphia, USA: Wolters Kluwer; 2021.
Singh Y. Evolution of the left ventricular function in preterm infants: long-term significance. Kardiol Pol. 2019;77(4):417–8. https://doi.org/10.33963/kp.14808.
Bennet L, Booth L, Drury P, Quaedackers J, Gunn A. Preterm neonatal cardiovascular instability: does understanding the foetus help evaluate the newborn? Clin Exp Pharmacol Physiol. 2012;39(11):965–72. https://doi.org/10.1111/j.1440-1681.2012.05744.x.
Goss K, Beshish A, Barton G, Haraldsdottir K, Levin T, Tetri L, et al. Early pulmonary vascular disease in young adults born preterm. Am J Respir Crit Care Med. 2018;198(12):1549–58. https://doi.org/10.1164/rccm.201710-2016OC.
Meah V, Cockcroft J, Stöhr EJ. Maternal cardiac twist pre pregnancy: potential as a novel marker of pre-eclampsia. Fetal Matern Med Rev. 2013;24(4):7. https://doi.org/10.1017/S0965539513000156.
Farrell ET, Bates ML, Pegelow DF, Palta M, Eickhoff JC, O’Brien MJ, et al. Pulmonary gas exchange and exercise capacity in adults born preterm. Ann Am Thorac Soc. 2015;12(8):1130–7. https://doi.org/10.1513/AnnalsATS.201410-470OC.
Farrow K, Steinhorn R. Pulmonary hypertension in premature infants: sharpening the tools of detection. Am J Respir Crit Care Med. 2015;191(1):12–4. https://doi.org/10.1164/rccm.201411-2112ED.
Ten VS. Mitochondrial dysfunction in alveolar and white matter developmental failure in premature infants’. Pediatr Res. 2017;81(2):286–92. https://doi.org/10.1038/pr.2016.216.
Kumari S, Barton GP, Goss KN. Increased mitochondrial oxygen consumption in adult survivors of preterm birth. Pediatr Res. 2021;90(6):1147–52. https://doi.org/10.1038/s41390-021-01387-9.
Vrijlandt E, Reijneveld S, Aris-Meijer J, Bos A. Respiratory health in adolescents born moderately-late preterm in a community-based cohort. J Pediatr. 2018;203:429–36. https://doi.org/10.1016/j.jpeds.2018.07.083.
Kajantie E, Strang-Karlsson S, Hovi P, Räikkönen K, Pesonen A, Heinonen K, et al. Adults born at very low birth weight exercise less than their peers born at term. J Pediatr. 2010;157(4):610-6.e1. https://doi.org/10.1016/j.jpeds.2010.04.002.
Lowe J, Cousins M, Kotecha SJ, Kotecha S. Physical activity outcomes following preterm birth. Paediatr Respir Rev. 2017;22:76–82. https://doi.org/10.1016/j.prrv.2016.08.012.
Rogers M, Fay T, Whitfield M, Tomlinson J, Grunau R. Aerobic capacity, strength, flexibility, and activity level in unimpaired extremely low birth weight (<=800 g) survivors at 17 years of age compared with term-born control subjects. Pediatrics. 2005;116(1):e58-65. https://doi.org/10.1542/peds.2004-1603.
Haraldsdottir K, Watson A, Beshish A, Pegelow D, Palta M, Tetri L, et al. Heart rate recovery after maximal exercise is impaired in healthy young adults born preterm. Eur J Appl Physiol. 2019;119(4):857–66. https://doi.org/10.1007/s00421-019-04075-z.
Acknowledgements
We sincerely thank the reviewers for their excellent suggestions and the constructive approach to the peer-review process. Several aspects of the manuscript, in particular the important points mentioned in the limitations section but also the addition of some articles that we originally missed, have improved because of their thoughtful and helpful comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by Projekt DEAL. No relevant sources of funding were used to assist in the preparation of this article.
Conflicts of interest/competing interests
Thomas Gostelow and Eric J. Stöhr declare that they do not have any conflicts of interest in relation to this work.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The data underlying this report will be made available to third parties upon reasonable request.
Code availability
Not applicable.
Author contributions
TG conceived the research, performed the initial literature research and wrote the manuscript. EJS reviewed the appropriateness of the extracted data and verified the inclusion of relevant articles, supervised the analysis and critically reviewed the manuscript. Both authors read and approved the final manuscript.
Additional information
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1007/s40279-023-01935-9"
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gostelow, T., Stöhr, E.J. RETRACTED ARTICLE: The Effect of Preterm Birth on Maximal Aerobic Exercise Capacity and Lung Function in Healthy Adults: A Systematic Review and Meta-analysis. Sports Med 52, 2627–2635 (2022). https://doi.org/10.1007/s40279-022-01710-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-022-01710-2