Abstract
Men are more likely than women to die due to coronavirus disease 2019 (COVID-19). An open question is whether these sex differences reflect men’s generally poorer health and lower life expectancy compared to women of similar ages or if men face a unique COVID-19 disadvantage. Using age-specific data on COVID-19 mortality as well as cause-specific and all-cause mortality for 63 countries, we compared the sex difference in COVID-19 mortality to sex differences in all-cause mortality and mortality from other common causes of death to determine the magnitude of the excess male mortality disadvantage for COVID-19. We found that sex differences in the age-standardized COVID-19 mortality rate were substantially larger than for the age-standardized all-cause mortality rate and mortality rate for most other common causes of death. The excess male mortality disadvantage for COVID-19 was especially large in the oldest age groups. Our findings suggest that the causal pathways that link male sex to a higher mortality from a SARS-CoV-2 infection may be specific to SARS-CoV-2, rather than shared with the pathways responsible for the shorter life expectancy among men or sex differences for other common causes of death. Understanding these causal chains could assist in the development of therapeutics and preventive measures for COVID-19 and, possibly, other coronavirus diseases.
Similar content being viewed by others
Introduction
Males have a higher risk of death from coronavirus disease 2019 (COVID-19) than females [1,2,3,4,5,6]. This difference has been observed for both the case fatality rate (CFR; i.e., deaths among those diagnosed with a SARS-CoV-2 infection) and infection fatality rate (IFR; i.e., deaths among all those who were infected with SARS-CoV-2) [1]. This higher risk of death from COVID-19 in males has been highlighted both in the academic literature and the media [7,8,9].
Understanding why these disparities by sex exist has become an active area of research. However, given that the risk of death from COVID-19 is strongly related to age and other risk factors for all-cause mortality [6], and thus one’s expected remaining life expectancy [6], it is unclear whether the observed sex differences in the COVID-19 fatality rate are simply a reflection of men’s shorter life expectancy [10], which is at least in part due to their poorer health status at any given age. This study aimed to determine if sex differences in COVID-19 mortality are larger when compared to the all-cause mortality rate, mortality rates for other common causes of death, and—given SARS-CoV-2’s common respiratory manifestations—other respiratory causes of death, including respiratory infections. This information is important, as it begins to elucidate whether the higher COVID-19 mortality risk among males reflects the survival advantage among females compared to males, and is, thus, likely a result of the biological, behavioral, and social pathways that cause this survival advantage as opposed to causal pathways that are specific to COVID-19. Understanding these causal pathways could help in the development of therapeutics and preventive measures for COVID-19 and possibly other coronavirus diseases.
Methods
Data sources
COVID-19 mortality data
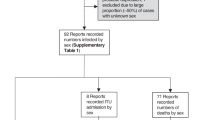
We extracted country-level data on COVID-19 deaths from the COVerAGE-DB database for countries for which age- and sex-disaggregated data were available with a reference date as near as possible to 9 February 2021 (as of 1 March 2022) and which had at least 50 recorded COVID-19 deaths as of this reference date [11]. We chose this cut-off date because coverage of COVID-19 vaccination, for which uptake likely differed by sex over time in different countries, was minimal in most countries until that date [12]. Age- and sex-disaggregated data were available for 63 countries: Afghanistan, Argentina, Australia, Austria, Belgium, Bosnia and Herzegovina, Brazil, Bulgaria, Cameroon, Canada, Chad, Chile, Colombia, Cuba, Czechia, Denmark, Dominican Republic, Ecuador, Eswatini, France, Germany, Greece, Honduras, Hungary, India, Iraq, Israel, Italy, Japan, Jordan, Kenya, Latvia, Lithuania, Malawi, Mexico, Moldova, Nepal, Netherlands, Nigeria, North Macedonia, Norway, Oman, Pakistan, Panama, Paraguay, Peru, Philippines, Portugal, Qatar, Romania, Slovakia, Slovenia, South Korea, Spain, Switzerland, Togo, Turkey, Ukraine, United Arab Emirates, United Kingdom, Uruguay, and the United States of America (USA). The disaggregation by age in COVerAGE-DB was by ten-year age groups.
General mortality data
For the 63 countries for which sex- and age-disaggregated COVID-19 mortality data were available, we obtained age- and sex-disaggregated data on all-cause mortality and total population size from the Human Mortality Database (HMD) [13]. We extracted the latest available population and deaths count data for each country (as of 1 March 2022). Population and deaths count data were available for 32 countries from the HMD: Australia, Belgium, Canada, Chile, Croatia, Czechia, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Israel, Italy, Japan, Latvia, Lithuania, Luxembourg, Netherlands, Poland, Portugal, Slovakia, Slovenia, South Korea, Spain, Switzerland, Ukraine, United Kingdom, and USA. For countries not in the HMD, we obtained the standard projections of populations and deaths data for the 2015–2020 period from the 2019 revision of the United Nation’s World Population Prospects (WPP) [10]. Data on population size and deaths were available for one-year age groups in the HMD and for five-year age categories in the WPP. To be consistent with COVerAGE-DB, we aggregated data from both the HMD and WPP into ten-year age groups, and combined data for age groups older than 80 into one category (80 +).
Cause-specific mortality data
We also obtained the latest available mortality data for specific causes of deaths from the WHO mortality database for 50 out of our 63 countries [14]. The 13 countries for which cause-specific death data were not available were Afghanistan, Cameroon, Chad, Czechia, Eswatini, Georgia, India, Kenya, Malawi, Nepal, Nigeria, Pakistan, and Togo. Causes of death were classified according to the 10th revision of the International Classification of Diseases (ICD-10) [15]. We obtained data for the top six causes of death groups globally (according to the WHO mortality database [13]), which were circulatory diseases, cancer, chronic respiratory diseases, respiratory infections and tuberculosis, diabetes, and neurologic disorders. To compare COVID-19 mortality differences by sex with differences observed for other respiratory causes of deaths, we further categorized respiratory causes into six groups: acute upper respiratory infections, influenza, pneumonia, other acute lower respiratory infections, other diseases of the upper respiratory tract, and chronic lower respiratory diseases. The ICD-10 codes used to define the six major causes of mortality and the respiratory causes of death are presented in Table S2.
Statistical analyses
We calculated age-standardized mortality rates separately by country for men and women for COVID-19-specific, cause-specific, and all-cause mortality. Separately for men and women, we first estimated COVID-19, cause-specific, and all-cause mortality rates for each age group by dividing the total number of deaths due to each cause (or all deaths for all-cause) by the mid-year population in that age group. We then standardized each rate using the overall age distribution of each country so that sex differences in mortality were not skewed by sex differences in the age distribution within countries.
Rate ratios for the sex differences in COVID-19 mortality were calculated for each country by dividing the age-standardized COVID-19-specific mortality rate in men by the age-standardized COVID-19-specific mortality rate in women. Similarly, sex differences in all-cause mortality were examined using the rate ratios obtained by dividing the age-standardized all-cause mortality rate in men by the age-standardized all-cause mortality rate in women. We calculated excess mortality disadvantage—the difference between the male-to-female mortality rate ratio from COVID-19 and that from all causes—by dividing the two ratios. We also present the relative difference in these rate ratios of mortality by age group (0–39, 40–49, 50–59, 60–69, 70–79, and 80 + years), major causes of mortality (circulatory diseases, cancer, chronic respiratory diseases, respiratory infections and tuberculosis, diabetes, and neurologic disorders), and common respiratory causes of death.
Lastly, instead of using age standardization, we calculated remaining life expectancy-adjusted mortality rates for men and women. The rationale for this robustness check is that remaining life expectancy may be a better measure of biological age than calendar age, since men and women at similar chronological ages often have different remaining life expectancies. To estimate remaining life expectancy-adjusted rates, we first obtained data on remaining life expectancy by age from the HMD and WPP. Specifically, for the latest year (in HMD) and period (in the WPP) for which data were available as of 09 February 2021, we obtained the remaining life expectancy at each single year of age separately for each country and sex. We then created 5-year groups for remaining life expectancy (0–4, 5–9, 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–50, and 50 + years) and matched these to each age by sex and country (e.g., for each age in the mortality data, we noted which remaining life expectancy group this age belonged to). Lastly, we estimated standardized mortality rates, where rather than set a common age-distribution for men and women, we instead set a common distribution of individuals across remaining life expectancy groups. This results in a standardized rate that has the interpretation of “what would the mortality rates for men and women be if they had the same population distribution of years of life expectancy remaining?”. All analyses were implemented in R version 4.1.2 [16].
We estimated confidence intervals around each of the ratios following the procedures recommended by Flanders [17] and Breslow and Day [18]. To do this, we first used the Delta method to estimate the standard error of each ratio. To construct confidence intervals, we used the observation that the natural log of rate ratios, rather than the ratios themselves, are approximately normally distributed and estimated the confidence interval first on the ln scale as log(estimates) ± 1.96(Standard error) and then exponentiated these bounds to convert them back to the ratio scale [18].
Data and materials availability
All the data used in the study are publicly available. COVID-19 mortality data are available from the COVerAGE-DB (https://osf.io/mpwjq/). Data on population size by age and sex are available from the HMD (www.mortality.org) and the United Nation’s WPP (https://www.who.int/healthinfo/mortality_data/en/). All statistical code to reproduce our analyses is available publicly at https://osf.io/d54ws/.
Results
Age- and sex-disaggregated data on COVID-19 deaths were available for 63 countries (Table 1). Chad, Cuba, and Togo had less than 100 recorded deaths from COVID-19. The number of deaths by sex for each of the six major groups of causes of deaths examined in this analysis are shown in Table S1.
Sex differences in COVID-19 compared to all-cause mortality
Figure 1 presents the age-standardized male-to-female rate ratios of mortality from COVID-19 and all causes. Point estimates greater than one in Fig. 1 indicate that men had a higher rate of death than women. The same information but depicted as a scatterplot and as the relative difference in the rate ratio are shown in Figs. S1 and S2, respectively. We found that in most countries, the male disadvantage for COVID-19 mortality was substantially larger than their all-cause mortality disadvantage. This result was robust to standardization by remaining life expectancy (Fig. S3).
Rate ratios for the sex differences in COVID-19 and all-cause mortality were calculated for each country by dividing the age-standardized mortality rate in males by the age-standardized mortality rate in females. Horizontal lines depict 95% confidence intervals.
Sex differences in COVID-19 compared to all-cause mortality by age group
We found the largest excess male disadvantage in COVID-19 mortality for the group aged 80 years and older (Fig. 2). Among younger age groups, especially those aged less than 50 years, the direction and magnitude of the difference between the male COVID-19 disadvantage and the male disadvantage for all-cause mortality varied greatly by country. These patterns were similar when using remaining-life expectancy-adjusted rates.
The relative difference in the rate ratio was calculated by dividing (separately among each age group shown) the male-to-female rate ratio for the COVID-19-specific mortality rate by the male-to-female rate ratio for the all-cause mortality rate. Horizontal lines depict 95% confidence intervals.
Sex differences in COVID-19 compared to other major causes of mortality
Comparing the male disadvantage for COVID-19 to their disadvantage in mortality from several major causes of mortality (circulatory diseases, cancer, chronic respiratory diseases, respiratory infections and tuberculosis, diabetes, and neurologic disorders), we found that in most countries the relative sex differences for COVID-19 were larger than for each of the other common causes of death (Figs. 3 and S4). However, this was not true for chronic respiratory conditions for which countries were spread approximately equally across the vertical dashed line drawn at one, which indicates that the relative sex difference for COVID-19 mortality was approximately the same as for chronic respiratory diseases. Implementing the same analysis as in Fig. 3 for each common respiratory cause of death (the ICD-10 codes used for categorization are shown in Table S2) revealed that the similar male disadvantage in mortality for chronic respiratory conditions as for COVID-19 is largely driven by a high male disadvantage in mortality from bronchitis and emphysema (the most common condition grouped under “chronic lower respiratory diseases”; Fig. S5).
Discussion
Across 63 countries, the size of the male COVID-19 mortality disadvantage tends to be substantially larger than the general male mortality disadvantage and the male disadvantage in several major causes of death. Thus, the higher probability of succumbing to a SARS-CoV-2 infection among men compared to women does not appear to be fully explained by the fact that across ages men generally have poorer health and a lower remaining life expectancy. This observation suggests that the causal pathways that link male sex to a shorter life expectancy may not fully explain the unusually high male disadvantage in COVID-19 mortality. Our findings, therefore, lend support to hypotheses that posit that the causal pathways that link male sex to a higher mortality from a SARS-CoV-2 infection may be specific to SARS-CoV-2 rather than shared with the pathways responsible for the shorter life expectancy among men than women or the causal pathways for sex differences for other common causes of death.
We do find that the male COVID-19 mortality disadvantage is similar to the size of the male disadvantage in mortality from chronic respiratory diseases. This might suggest that the sex differences in COVID-19 mortality exist due to a causal pathway that is shared by both COVID-19 and chronic respiratory disease. However, our analysis shows that the high male disadvantage for chronic respiratory disease is driven by a stark male mortality disadvantage for bronchitis and emphysema, which in turn is likely explained by the higher prevalence of smoking (especially in the past) among men than women [19,20,21]. Although smoking could be a part of the causal pathway that explains the male mortality disadvantage for COVID-19, it likely is not the main pathway because smoking has been found to not be as strong a risk factor for the combined outcome of SARS-CoV-2 infection and COVID-19 mortality as some other common risk factors, such as diabetes and obesity [6, 22].
There are several other potential reasons for the higher COVID-19 mortality rate among men. Some studies cite a higher rate of comorbidities, such as diabetes and heart disease, as the reason for the higher COVID-19 fatality rate among men [4, 20, 23,24,25]. While we cannot directly test this hypothesis, we find that across countries the male COVID-19 mortality disadvantage is substantially larger than their disadvantage for circulatory diseases and diabetes. This suggests that differences in cardiovascular comorbidities may not be a driving factor behind the sex differences in COVID-19 mortality. Other studies suggest that biological factors may explain these disparities. For example, men have a higher expression of the angiotensin-converting enzyme 2 receptor, which is used by SARS-CoV-2 to enter the host cell [3, 26, 27]. Other possible biological factors relate to immunological differences between males and females [28,29,30,31]. Ultimately, a combination of biological, behavioral, and social pathways may be responsible for the high male disadvantage in COVID-19 mortality. Elucidating these causal chains is an important research area given that it may assist in the development of therapeutics and preventive measures for COVID-19 and future outbreaks of coronavirus diseases.
This study has several limitations. First and foremost, this study can only provide suggestive evidence as to whether or not the causal pathways underlying the male disadvantage for COVID-19 mortality are shared with those underlying the all-cause mortality disadvantage for men. Second, our mortality rate calculations for COVID-19 use the total population (by sex) as the denominator. Thus, the assumption underlying the validity of our calculation is that there are no substantial differences in the probability of being infected with SARS-CoV-2 between males and females. To date, evidence from seroprevalence studies suggests that this assumption is reasonable [32, 33]. An alternative approach is to use the number of identified cases of SARS-CoV-2 infections as the denominator (i.e., calculating the case fatality rate). This approach, however, assumes that the degree of underdetection of SARS-CoV-2 infections is the same among men as among women. This assumption would, for example, be violated if males are more likely to develop symptoms from a SARS-CoV-2 infection than females and are, therefore, more likely to seek out a COVID-19 test, or if men have better access to testing than women. Although both choices for the denominator (total population or number of cases) rely on untestable assumptions, our analyses in which we use the number of cases instead of the total population as denominator found that the choice of denominator does not substantially change our conclusions.
This study indicates that the causal pathways that link male sex to a higher mortality from a SARS-CoV-2 infection may not be shared with the causal pathways for sex differences in all-cause mortality or other common causes of death. Instead, our analysis suggests that the male mortality disadvantage from COVID-19 may be due to sex-specific pathways of SARS-CoV-2 infections. Understanding these SARS-CoV-2-specific pathways could help with the design and development of both preventive measures and therapeutics for COVID-19 and potentially other coronavirus diseases.
References
Blackburn J, Yiannoutsos CT, Carroll AE, Halverson PK, Menachemi N. Infection fatality ratios for COVID-19 among noninstitutionalized persons 12 and older: results of a random-sample prevalence study. Ann Intern Med. 2020. https://doi.org/10.7326/M20-5352.
Boerner L. COVID-19 is probably more deadly to men than women, but scientists still aren’t sure why [Internet]. 2020. https://cen.acs.org/biological-chemistry/infectious-disease/COVID-19-probably-deadly-men/98/i29. Accessed 1 Nov 2020
Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R, Klein SL. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ. 2020;11(1):1–13.
Jin J-M, Bai P, He W, Wu F, Liu X-F, Han D-M, et al. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health. 2020. https://doi.org/10.3389/fpubh.2020.00152/full.
Pradhan A, Olssen P-E. Sex differences in severity and mortality from COVID-19: are males more vulnerable? Biol Sex Differ. 2020;11(1):53.
Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–6.
Alkhouli M, Nanjundappa A, Annie F, Bates MC, Bhatt DL. Sex Differences in case fatality rate of COVID-19: insights from a Multinational Registry. Mayo Clin Proc. 2020;95(8):1613–20.
Bendix A, Secon H. More men die from coronavirus than women—here’s why that might be—Business Insider [Internet]. 2020. https://www.businessinsider.com/why-more-men-die-from-coronavirus-than-women-2020-3. Accessed 19 Nov 2020
Lord D. Coronavirus fact check: Are more men than women dying from COVID-19? [Internet]. 2020. https://www.kiro7.com/news/trending/coronavirus-fact-check-are-more-men-than-women-dying-covid-19/JMMCO3I4NBD3XPNHQFEACXVILQ/. Accessed 19 Nov 2020
World Population Prospects—Population Division—United Nations [Internet]. [cited 2021 Jan 12]. Available from: https://population.un.org/wpp/
Riffe, Tim, Enrique Acosta, and the COVerAGE-DB team. Data Resource Profile: COVerAGE-DB: a global demographic database of COVID-19 cases and deaths. Int J Epidemiol 2021;50(2):390–390.
Ritchie H, Mathieu E, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina E, et al. Coronavirus pandemic (COVID-19). Our World Data 2020 Mar 5. https://ourworldindata.org/covid-vaccinations. Accessed 9 Feb 2022
University of California, Berkeley, Max Planck Institute for Demographic Research. Human Mortality Database [Internet]. Available from: www.mortality.org
World Health Organization. WHO Mortality Database [Internet]. 2019. Available from: https://www.who.int/data/data-collection-tools/who-mortality-database
National Center for Health Statistics. ICD-ICD-10-International Classification of Diseases, Tenth Revision [Internet]. 2020 [cited 2021 Feb 11]. https://www.cdc.gov/nchs/icd/icd10.htm
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2021.
Flanders WD. Approximate variance formulas for standardized rate ratios. J Chronic Dis. 1984;37(6):449–53.
Breslow NE, Day NE. Statistical methods in cancer research Volume II—The design and analysis of cohort studies. IARC Sci Publ. 1987;82:1–406.
Ritchie H. Who smokes more, men or women? [Internet]. Our World in Data. https://ourworldindata.org/who-smokes-more-men-or-women. Accessed 20 Jan 2021
Capuano A, Rossi F, Paolisso G. Covid-19 kills more men than women: an overview of possible reasons. Front Cardiovasc Med. 2020. https://doi.org/10.3389/fcvm.2020.00131/full.
World Health Organization. Smoking and COVID-19 [Internet]. 2020 [cited 2020 Nov 19]. Available from: https://www.who.int/news-room/commentaries/detail/smoking-and-covid-19
Westreich D, Edwards JK, Tennant PWG, Murray EJ, van Smeden M. Choice of outcome in COVID-19 studies and implications for policy: mortality and fatality. Am J Epidemiol. 2022;191(2):282–6.
Guarino B. Why the coronavirus is killing more men than women. Washington Post [Internet]. https://www.washingtonpost.com/science/2020/10/17/coronavirus-men-immune-system/. Accessed 19 Nov 2020
Holman N, Knighton P, Kar P, O’Keefe J, Curley M, Weaver A, et al. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2020;8(10):823–33.
Lancet T. The gendered dimensions of COVID-19. Lancet Lond Engl. 2020;395(10231):1168.
Behl T, Kaur I, Bungau S, Kumar A, Uddin MS, Kumar C, et al. The dual impact of ACE2 in COVID-19 and ironical actions in geriatrics and pediatrics with possible therapeutic solutions. Life Sci. 2020;257:118075.
Ni W, Yang X, Yang D, Bao J, Li R, Xiao Y, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 2020;24(1):1–10.
Cunningham A. COVID-19 kills more men than women. The immune system may be why [Internet]. Science News. 2020. https://www.sciencenews.org/article/coronavirus-covid-19-kills-more-men-than-women-why-immune-system. Accessed 19 Nov 2020
Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–38.
Geggel L. Why are more men dying from COVID-19?|Live Science [Internet]. https://www.livescience.com/why-covid-19-more-severe-men.html. Accessed 19 Nov 2020
Chakravarty D, Nair SS, Hammouda N, Ratnani P, Gharib Y, Wagaskar V, et al. Sex differences in SARS-CoV-2 infection rates and the potential link to prostate cancer. Commun Biol. 2020;3(1):1–12.
Anand S, Montez-Rath M, Han J, Bozeman J, Kerschmann R, Beyer P, et al. Prevalence of SARS-CoV-2 antibodies in a large nationwide sample of patients on dialysis in the USA: a cross-sectional study. Lancet. 2020;396(10259):1335–44.
Ng OT, Marimuthu K, Koh V, Pang J, Linn KZ, Sun J, et al. SARS-CoV-2 seroprevalence and transmission risk factors among high-risk close contacts: a retrospective cohort study. Lancet Infect Dis. 2020;21(3):333–43. https://doi.org/10.1016/S1473-3099(20)30833-1.
Funding
Pascal Geldsetzer is a Chan Zuckerberg Biohub investigator. Nikkil Sudharsanan was supported by the Alexander von Humboldt Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
PG: conceptualization, methodology, writing—original draft preparation; TM: methodology, data analysis, writing—reviewing and editing; NJ: methodology, writing—original draft preparation; TR: conceptualization, methodology, data analysis. Writing—reviewing and editing; AR: methodology, writing—reviewing and editing; NS: conceptualization, methodology, writing—reviewing and editing.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study received a determination of not-human subjects research from the institutional review board of the Heidelberg University Hospital.
Consent to participate
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Geldsetzer, P., Mukama, T., Jawad, N.K. et al. Sex differences in the mortality rate for coronavirus disease 2019 compared to other causes of death: an analysis of population-wide data from 63 countries. Eur J Epidemiol 37, 797–806 (2022). https://doi.org/10.1007/s10654-022-00866-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-022-00866-5