Abstract
Traditional disinfection methods against pathogens have numerous shortcomings, and inventive methods like cold plasma are required for virus inactivation. Here, an atmospheric pressure 13.56 MHz radio-frequency hollow cathode (RF–HC) cold plasma device has been used to build a cold plasma sterilization device, and its virucidal activity is assessed against P2 bacteriophage, a model surrogate for pathogenic viruses. The heart of this device contains a three-layered sterilization chamber which is a rectangular parallelopiped of 42 × 32 × 30 cm3. Optimization experiments were performed to make each corner of this chamber completely virus free after cold plasma treatment. This two-pronged study was conducted to establish the requirement of minimum vol. % H2O2 in minimum time for the complete elimination of phages inside this sterilization chamber even when plasma is not in the direct line of sight. In initial experiments, the effect of the direct plasma line of sight was seen as the top and bottom layers showing less phage killing as compared to the middle of the sterilization chamber. Complete sterilization of bacteriophage, in all the three layers inside the sterilization chamber, was achieved by plasma treatment with 6% H2O2 for 10 min in 80 watts of plasma operating power. It was also seen that 6% H2O2 mist alone is not sufficient to provide a high degree of sterilization, and normal water mist combined with cold plasma can provide a higher level of sterilization at each corner of the chamber.
Similar content being viewed by others
Introduction
Since the beginning of the twenty-first century, several pathogenic virus-related outbreaks (H1N1 flu, SARS, MERS, Covid-19 and Ebola) have caused significant mortality and morbidity, and catastrophic impacts on the lives and livelihoods across the globe [1]. Most of these diseases are infectious and spread mainly through air and surface transmission. Surface contagion can pose a high risk of transmission as the infectious virions can stay viable on various surfaces (e.g., plastic, metals, and cardboard) for several hours [2, 3]. Several traditional sterilization processes (sodium hypochlorite, soap water, steam, dry heat, alcohol, and UV) used for the surface decontamination have numerous shortcomings, and inventive methods are required for the virus inactivation [4, 5].
Recently, bacteriophages have been extensively used as surrogate organisms to study the virucidal effects of various physical methods as they are safe to use, exhibit structural characteristics equivalent to human and animal viruses and are easy to produce in large quantities [6, 7].
Cold plasma has emerged as an effective tool for various applications ranging from material science to the medical industry [8,9,10,11,12,13,14,15,16]. Earlier, cold plasmas were confined only within a vacuum chamber, but recent technological and scientific advances have facilitated cold plasma generation in ambience, devoid of vacuum chamber and pumping arrangements [17]. This progress has led to the development of several types of atmospheric pressure cold plasma sources and opened up a novel branch called plasma medicine where cold plasma can be used for therapeutic purposes like wound healing, cancer treatment and food sterilization [16, 18,19,20].
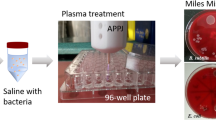
Recent work in our lab has shown that a 2.45 GHz microwave-based atmospheric pressure plasma jet (APPJ) and a hollow-cathode based atmospheric pressure cold plasma device (RF-HC) using 13.56 MHz frequency were both successful in pathogenic disinfection [21]. The comparative study also concluded that RF-HC has the advantage over APPJ in the terms of a larger area for sterilization. A later study showed that RF-HC device along with a nebulizer (for introducing water mist) in Argon plasma can effectively destroy Aeromonas hydrophila bacteriophage P2 at low operating power (70–90 watts) [22]. Systematic optical emission spectroscopy (OES) studies have shown that the plasma generated using this device emitted OH radical, reactive oxygen species, UV and other radicals which acted synergistically in cold plasma for pathogenic sterilization.
Based on these encouraging results, a ‘cold plasma sterilization device’ was built for the dry sterilization of varied articles, including documents and various personal belongings (purse, mobile, ornaments, food boxes, etc.). The device contains a sterilization chamber of 42 × 32 × 30 cm3, divided into 3 compartments, and the idea was to sterilize the articles placed within this chamber with the help of cold plasma. The details of the device are given in the subsequent section.
In the present work, we have studied the efficacy of this ‘cold plasma sterilization device’ towards decimating the bacteriophage and thereby decontaminating the surfaces as a function of H2O2 concentration, exposure time and phage position. The idea used here is to achieve complete sterilization in each corner of the device in minimum time and minimum H2O2 requirement.
Experimental and Device Information
Phage Lysate Preparation
P2 phage, a bacteriophage (virus) of A. hydrophila CECT 839T (Type culture), was isolated from the sewage treatment plant. It belongs to the Podoviridae family of order Caudovirales. P2 phage was propagated using A. hydrophila CECT 839 T as the host. Figure 1 shows the TEM image of P2 phage. Both the cases of positive and negative stainings are seen in the image. Phage lysate was prepared according to the previously described protocol by Bonilla et al. [23] with minor modifications. One ml of overnight grown A. hydrophila CECT 839T culture was added to 25 ml Tryptic Soya Broth (TSB), (containing 1 mM CaCl2 and 1 mM MgCl2) and kept at 30 °C, 150 rpm on a shaker. At 0.3 O.D. (3 × 108 cells/ml), 500 μl of the P2 lysate (1 × 109 pfu (plaques forming unit)/ml) was added to A. hydrophila CECT 839 T culture and incubated at 30 °C for 30 min without shaking the mixture. The culture was grown at 30 °C with vigorous shaking, 220 rpm for 3–4 h till lysis (visible aggregated cell debris) occurred. A TSB flask (containing 1 mM CaCl2 and 1 mM MgCl2) of no-phage control (only A. hydrophila culture) was also incubated under similar conditions for comparing turbidity with the lysed culture. 0.2% v/v chloroform was added to the lysed bacterial broth followed by shaking-incubation for 10 min. The lysed bacterial broth was centrifuged at 10,000 rpm for 20 min at 4 °C, followed by the addition of 0.1% chloroform to the supernatant and stored at 4 °C. Preparation of the phage lysate was confirmed by spot inoculating 5 μl of lysate on previously spread A. hydrophila CECT 839T culture on TSA plate.
Phage Enumeration
This phage lysate was used to determine the phage titer (PFU/ml) using soft agar overlay method [24] with minor modifications. Filtered phage lysate was serially diluted in SM buffer (100 mM NaCl, 8 mM MgSO4, 50 mM Tris–Cl, pH 7.5). For each serial dilution, 100 µl phage lysate was mixed with 100 µl of log phase A. hydrophila CECT 839T (~ 108 cells/ml) culture followed by incubation at 30 °C for 10 min to facilitate phage adsorption. The mixture was added to 4 ml of molten soft (0.4%) agar and overlaid on TSA + 1 mM CaCl2 plates. Plaques were counted after overnight incubation of plates at 30 °C, and the phage titer was determined in terms of plaque forming unit (PFU/ml).
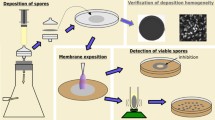
Assessment of Virucidal Efficiency of the Sterilization Chamber
Virucidal efficiency of the sterilization chamber was evaluated by exposing A. hydrophila bacteriophage P2 to different cold plasma treatments w.r.t. position of phage sample, exposure time and H2O2 concentration. Hundred microliters of P2 phage suspension with known concentration (~ 107 pfu/ml, plaque forming unit, pfu) in SM buffer (100 mM NaCl, 8 mM MgSO4, 50 mM Tris–Cl, pH 7.5) was spotted on pre-sterile paper discs and kept at different positions in the sterilization chamber. These phage-inoculated discs were exposed to different combinations of cold plasma, H2O2 and time. Phage-inoculated discs, not exposed to cold plasma or H2O2, were kept in the sterilization chamber for 10 min and they were used as control samples for assessing the virucidal efficiency. Phages from the control and treated discs were extracted by suspending and vortexing these discs in 10 ml SM buffer for 3 min. Extracted lysates were tenfold serially diluted in SM buffer. Viability of bacteriophage was assessed by spotting 10 µl of appropriately diluted phage suspension on previously spread A. hydrophila CECT 839T (host) bacterial lawn on TSA + 1 mM CaCl2 plates. The plates were observed for plaques (clear zone of lysis by bacteriophage) formation after incubation for 24 h.
RF-Hollow Cathode Plasma & Sterilization Device
The plasma device used in this case is a hollow cathode (H-C) based whose principle is detailed elsewhere [21, 22] but discussed in brief for its completeness. Here, two electrodes are kept at equal potential and their inter-electrode distance is less than the electron-neutral collision mean free path. Here, this condition is achieved by making a spiral groove inside the live electrode with ~ 280 μm width. Plasma is generated inside this groove by connecting it to a 13.56 MHz power supply. The ground electrode is a brass disc with 3 mm punctuated holes. Figure 2a shows a schematic of the live and ground electrode to give an idea about the RF-HC device. Figure 2b shows the 3-D schematic of the complete device. Figure 2c shows a photograph of the device with Argon plasma. Argon was used as the gas for plasma generation as it is a noble gas and cheap to use. Figure 2d shows the photograph of the temperature measurement of the ground electrode with a commercial IR thermometer with plasma showing temperature of 46.9 °C. One should also remember that plasmas are not black bodies and using an IR temperature monitor will not measure plasma temperature. Measurement of ground electrode temperature was done to make sure that plasma aided process remains the solitary reason for inactivation of microorganisms and not the high temperature, as it is well known that exposure to high temperature inactivates and kills the microorganisms. All the microorganisms for these experiments were kept at least 7 cm away from the ground electrode at room temperature.
Actual photograph of the device with important components marked is shown in the Fig. 3a. In the schematic, it is shown that the complete device is fabricated in different rows. The top row contains a 13.56 MHz, 300 watts RF power supply. This supply is connected to the RF-HC cold plasma device in the 2nd row to supply the required energy for the plasma generation. In this row, RF-HC cold plasma device is kept at the centre and the aforesaid sterilization chamber, divided into three compartments, is placed just in front of the cold plasma. One can arrange different articles like documents, personal belongings (keys, ornaments and purses) in these racks for sterilization. These racks made the entire volume of the chamber more usable. A commercial nebulizer is kept at the bottom of the 2nd row in such a way that mist produced by this nebulizer will interact with plasma to create OH radicals and important reactive oxygen and nitrogen species (ROS & RNS), aiding in the sterilization process. The detailed drawing of the sterilization chamber with dimensions are shown in Fig. 3c. The 3rd row of Fig. 3a contains a door that was used to refill the nebulizer water when needed and a rotameter to supply Argon gas at a fixed flow rate of 20 LPM. The electronic control of the entire device is placed in the 4th row where electric mains, switches for start, reset is placed along with a buzzer and timer. The buzzer is supposed to go off when timer completes a sterilization cycle. The 5th row contains the reservoir tank and matching network. The tank circulates tap water in a closed loop to cool the plasma device and the matching network helps in dynamic impedance matching at 13.56 MHz frequency. All these rows are placed within a commercial 19-inch experimental rack to house the complete device. Figure 3b shows the photograph of the device housed inside the experimental rack.
Figure 4 shows the experimental arrangement inside different racks for plasma treatment of P2 phage. Bacteriophage was kept at four corners of each rack as depicted in the figure. The corner spot was chosen as the benchmark for sterilization as they would be at different distances from the plasma line of sight and deemed to be difficult for radicals to reach for the sterilization. Each corner was given a number and the numbering was done clockwise for each row. The sides with numbers 1,2; 5,6; 9,10 are closer to the plasma device while the opposite sides with numbers 3,4; 7,8; 11,12 are facing the door of the sterilization chamber. Several experiments were conducted using this number system as detailed in the next section. Argon plasma was ignited at 80 watts of input power for each experiment.
During experiment, 80 watts of RF power was used to ignite Argon. Figure 5 shows a typical optical emission spectrum (OES) of the plasma generated in the system. For this measurement, the tip of the optical fibre of OES was placed at the centre of the middle rack of the sterilization chamber. Major atomic lines and molecular bands are identified in the spectrum. The spectrum shows the presence of Ar I lines as expected. Apart from these, O I atomic lines are also detected near 777 nm. Among molecular bands, a strong presence of OH band between 306–310 nm and N2 second positive system (SPS) at 336 nm are detected easily. In the UV-C region of the spectrum Kaplan bands of N2, γ and δ bands of NO and \({\mathrm{O}}_{2}^{-}\) superoxide bands are spotted aiding the germicidal capabilities of the device.
Results and Discussion
Table 1 shows the results obtained from the experiments to test the virucidal ability of the sterilization chamber on A. hydrophila bacteriophage. Bacteriophages having a higher count (> 100 pfu/ml] in the spotted region will form a zone of confluent clearing instead of forming individual plaques. A zone of lysis by bacteriophage in the spotted region against bacterial growth indicates that the virus is viable. All the experiments conducted inside the sterilization chamber are divided into 6 sets as detailed in Table 1. In Table 1, the nebulizer mixer is indicated in each case through H2O2 concentration, where 0 means that the nebulizer is switched on but no H2O2 is mixed in water; while %H2O2 is mentioned in the other cases. The first set (not undergoing any treatment) was designated as the control set and had phage count of 6.73 ± 0.18 log PFU/ml. The second set of experiments was conducted, at four corners of each rack, with only tap water in the nebulizer (Fig. 4). The results showed that 10 min of cold plasma exposure with water mist is successful in the partial eradication of the virus from 106 pfu/ml to 104 pfu/ml in the top and bottom racks, and 103 pfu/ml in the middle rack. This shows ~ 99% reduction in the top and bottom racks, and ~ 99.9% in the middle rack. Previously, it was shown that virucidal ROS and UV can be generated in plasma through water mist from a commercial nebulizer in front of RF-HC plasma; however, set 2 shows that the eradication is not complete in this case [21]. It was also observed that the virucidal effect is more prominent in the middle rack as compared to the other two racks. This is understandable considering the geometry of the sterilization chamber (Fig. 3a) where the middle rack faces the majority of the plasma area. Subsequently, it was thought to add a low concentration of H2O2 to boost the virucidal effect of the plasma.
Set 3 of plasma exposure was conducted with 1% H2O2 solution for 10 min but similar results were obtained as in set 2 indicating no significant changes in virucidal effect with 1% H2O2 solution as compared to the 0% H2O2. In the next set of experiment (set 4), H2O2 content was increased from 1 to 6%. Here, it should be mentioned that Occupation Safety and Health Act (OSHA) of the USA, sets the limit for legal airborne permissible exposure limit (PEL) of H2O2 as 1 PPM averaged over an 8-h work shift [25] and thus, emission of H2O2 was measured by a commercial H2O2 detector (D 16–2 Portasens III, P/N 00–1042). For 6% H2O2 solution, maximum emission measured was 0.5 ppm near the central region of the middle rack inside the sterilization chamber. No H2O2 emission was recorded in the detector after the closure of the chamber door. Set 4 experiment was conducted to test whether H2O2 mist with its known germicidal effect is sufficient to eradicate the phage from all the four corners of all racks. In this case, plasma was not switched on and treatment with H2O2 mist, sent through a nebulizer, was conducted for 10 min. On comparing experimental results from sets 2 & 4, one can observe that the virucidal effect is one order of magnitude better with set 2 (0% H2O2 + cold plasma combination) showing plaque survival of 103 to 104 pfu/ml as compared to set 4 (only 6% H2O2 mist exposure) which showed plaque survival as 103 to 105 pfu/ml. In both these cases, it can be seen from the results of each set that there is a drop in the virucidal activity when the phage affected region is farther from the line of sight of the plasma. The virucidal effect in set 4 (only with 6% H2O2) is not uniform in all three racks and tends to provide better sterilization in the central rack when compared to the top and bottom racks. Comparing set 2 (only plasma and 0% H2O2) and 4, one can see that the level of sterilization is approximately the same in the central rack in both cases but set 2 provides better sterilization for the top and bottom racks. The result shows that 6% H2O2 mist (set 4) alone is not sufficient to eliminate phage from all the three racks and some other method may be required in increasing its performance. Set 5 shows the experimental scheme where a combination of 6% H2O2 mist and RF-HC cold plasma treatment for 5 min showed the highest degree of virucidal effect (~ 99.99% reduction) as compared to all the previous sets. Moreover, eradication was uniform across all corners of all the racks. However, the complete eradication of phage was still not achieved. Therefore, in the next set (set 6) of experiment, plasma treatment was increased to 10 min. This combination treatment resulted in the complete eradication of phages (no plaque observed) from all three racks. These 6 sets of experiments prove that for complete eradication of phage from each corner of each rack of the 42 × 32 × 30 cm3 sterilization chamber, one should use 6% H2O2 solution in the nebulizer and subsequent cold plasma treatment must be conducted for 10 min.
Figure 6 shows representative photographs of the plates, for each set of treatments, observed for plaque (clear zone of lysis by bacteriophage) formation after incubation for 24 h. Representative photographs have been given separately for different serially-diluted combinations for each set of experiments. The dilution marker has been pasted on each photograph with dilution ranging from 100, 10–1, 10–2, 10–3 and 10–4. It is to be mentioned that 10–1 to 10–4 dilutions were used for the control set; whereas, 100 to 10–2 were used for the treated sets. For each set, result of the middle layer is only shown for ease of comparison. These photographs corroborated with the results shown in Table 1.
Conclusion
Atmospheric pressure RF-HC cold plasma device has been used here to fabricate a cold plasma sterilization device. The heart of this device contains a three-layered sterilization chamber where the virucidal efficacy of cold plasma has been checked against P2 bacteriophage. Comprehensive testing has been done so that each corner of the sterilization chamber away from the direct line of sight of plasma can also become virus free. In experiment sets 2 to 5, the top and bottom layers showed less phage killing as compared to the middle layer due to the effect of a direct plasma line of sight. It was seen that 6% H2O2 mist alone is not sufficient to provide a high degree of sterilization and normal water mist combined with cold plasma can provide a higher level of sterilization at each corner of the chamber. Complete sterilization of bacteriophage in all the three layers inside the ‘sterilization chamber’ can be observed by combination treatment of 6% H2O2 and cold plasma for 10 min with 80 watts of plasma operating power.
References
Jocelyne P, Guy B (2021) Pandemics throughout history. Front Microbiol. https://doi.org/10.3389/fmicb.2020.631736
Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, LloydSmith JO, de Wit E, Munster VJ (2020) Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 382:1564
Bhardwaj R, Agrawal A (2020) Likelihood of survival of coronavirus in a respiratory droplet deposited on a solid surface. Phys Fluids 32:061704
Guettari M, Aferni AE (2021)Coronavirus Disinfection Physical Methods. In: Fighting the COVID-19 Pandemic. London, United Kingdom: IntechOpen, 2021 [Online]. Available: https://www.intechopen.com/chapters/77771https://doi.org/10.5772/intechopen.99091
Mohammadi MA, Ahangari H, Khajavi MZ, Yousefi M, Scholtz V, Hosseini SM (2021) Inactivation of viruses using nonthermal plasma in viral suspensions and foodstuff: A short review of recent studies. J Food Saf 41(5):e12919. https://doi.org/10.1111/jfs.12919
Barros J, Ferraz MP, Monteiro FJ (2021) Bacteriophage Phi 6 as Surrogate and Human-Harmless Viruses to Study Anti-SARS-CoV-2 Approaches. COVID-19 Pand Case Stud Opinions 2(1):175–177
Franke G, Knobling B, Brill FH, Becker B, Klupp EM, Belmar Campos C, Pfefferle S, Lütgehetmann M, Knobloch JK (2021) An automated room disinfection system using ozone is highly active against surrogates for SARS-CoV-2. J Hosp Infect 112:108–113
Grill A (1994) Cold plasma in materials fabrication, vol 151, IEEE Press, New York
Pankaj SK, Keener KM (2017) Cold plasma: background, applications and current trends. Curr Opin Food Sci 16:49–52
Barve SA, Chopade SS, Kar R, Chand N, Deo MN, Biswas A, Sinha S (2017) SiOx containing diamond like carbon coatings: effect of substrate bias during deposition. Diam Relat Mater 71:63–72
Laroussi M (2015) Low-temperature plasma jet for biomedical applications: a review. IEEE Trans Plasma Sci 43(3):703–712
Bunz O, Mese K, Zhang W, Piwowarczyk A, Ehrhardt A (2018) Effect of cold atmospheric plasma (CAP) on human adenoviruses is adenovirus type-dependent. PloS one, 13(10)
Arndt S, Unger P, Berneburg M, Bosserhoff AK, Karrer S (2018) Cold atmosphericplasma(CAP)activates angiogenesis-relatedmoleculesin skin keratinocytes, fibroblasts and endothelial cells and improves wound angiogenesis in an autocrine and paracrine mode. J Dermatol Sci 89(2):181–190
Ranjan R, Krishnamraju PV, Shankar T, Gowd S (2017) Nonthermal plasma in dentistry: an update. J Int Soc Prevent Commun Dentist 7(3):71
Lin L, Wang L, Liu Y, Xu C, Tu Y, Zhou J (2018) Non-thermal plasma inhibits tumor growth and proliferation and enhances the sensitivity to radiation in vitro and in vivo. Oncol Rep 40(6):3405–3415
Laroussi M, Kong MG, Morfill G (eds) (2012) Plasma medicine: applications of low-temperature gas plasmas in medicine and biology. Cambridge University Press, Cambridge
Schutze A, Jeong JY, Babayan SE, Park J, Selwyn GS, Hicks RF (1998) The atmospheric-pressure plasma jet: a review and comparison to other plasma sources. IEEE Trans Plasma Sci 26(6):1685–1694
Misra NN, Schlüter O, Cullen PJ (eds) (2016) Cold plasma in food and agriculture: Fundamentals and applications. Academic Press, Cambridge
Keidar M, Shashurin A, Volotskova O, Ann Stepp M, Srinivasan P, Sandler A, Trink B (2013) Cold atmospheric plasma in cancer therapy. Phys Plasmas 20(5):057101
Watson GA, Jacofsky MC, Jacofsky DJ (2013) U.S. Patent Application No. 13/620,214
Bute A, Nagar KR, Chand N, Bhale D, Shashidhar R, Patil DS, Narayana-Rao AVSS, Maiti N (2021) Effect of water vapor on the virucidal behavior of rf-hollow cathode cold plasma: a study by optical emission spectroscopy. IEEE Trans Plasma Sci 49:2774–2784
Kar R, Chand N, Bute A, Maiti N, Narayan Rao AVSS, Nagar V, Shashidhar R, Patil DS, Ghosh SK, Sharma A (2020) Cold plasma: clean technology to destroy pathogenic micro-organisms. Trans Indian Natl Acad Eng, 5, 327–331 (2020).
Bonilla N, Rojas MI, Netto Flores Cruz G, Hung SH, Rohwer F, Barr JJ (2016) Phage on tap-a quick and efficient protocol for the preparation of bacteriophage laboratory stocks. PeerJ 4:e2261
Sanders ER (2012) Aseptic laboratory techniques: plating methods. J Vis Exp 63:e3064
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
V. Nagar and R. Kar these auhtors have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Nagar, V., Kar, R., Pansare-Godambe, L. et al. Evaluation of Virucidal Efficacy of Cold Plasma on Bacteriophage Inside a Three-Layered Sterilization Chamber. Plasma Chem Plasma Process 42, 1115–1126 (2022). https://doi.org/10.1007/s11090-022-10269-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11090-022-10269-9