Abstract
The spike protein of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the major antigen stimulating the host’s protective immune response. Here we assessed the efficacy of therapeutic monoclonal antibodies (mAbs) against Omicron variant (B.1.1.529) sublineage BA.1 variants in Syrian hamsters. Of the FDA-approved therapeutic mAbs tested (that is, REGN10987/REGN10933, COV2-2196/COV2-2130 and S309), only COV2-2196/COV2-2130 efficiently inhibited BA.1 replication in the lungs of hamsters, and this effect was diminished against a BA.1.1 variant possessing the S-R346K substitution. In addition, treatment of BA.1-infected hamsters with molnupiravir (a SARS-CoV-2 RNA-dependent RNA polymerase inhibitor) or S-217622 (a SARS-CoV-2 protease inhibitor) strongly reduced virus replication in the lungs. These findings suggest that the use of therapeutic mAbs in Omicron-infected patients should be carefully considered due to mutations that affect efficacy, and demonstrate that the antiviral compounds molnupiravir and S-217622 are effective against Omicron BA.1 variants.
Similar content being viewed by others
Main
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is responsible for coronavirus disease 2019 (COVID-19), continues to spread around the world and has caused 6.1 million deaths so far. The Omicron variant (B.1.1.529) of SARS-CoV-2 was detected in November 2021 in South Africa and has spread rapidly around the world. Omicron variants have been classified into six different sublineages: BA.1, BA.1.1, BA.2, BA.3, BA.4 and BA.5. The original Omicron lineage, BA.1, rapidly became the prevailing variant circulating in many countries. A notable feature of the BA.1 variant is that it contains more than 30 amino acid substitutions in its spike (S) protein, which induces the immune responses of the host, specifically the production of neutralizing antibodies1. Importantly, 15 of these substitutions are in the receptor-binding domain (RBD) of the S protein, which is the major target for monoclonal antibody (mAb)-based therapy, raising concerns of decreased effectiveness of current therapeutic monoclonal antibodies (mAbs) for COVID-19 against this variant.
Recent studies using in vitro neutralization assays have demonstrated that the BA.1 variants show reduced sensitivity to some monoclonal and polyclonal antibodies relative to past isolates or other SARS-CoV-2 variants2,3,4,5,6. However, the in vivo efficacy of mAbs against the BA.1 variant is unknown. Here we assessed the efficacy of U.S. Food and Drug Administration (FDA)-approved therapeutic mAbs against BA.1 variants in Syrian hamsters, a well-established animal model for SARS-CoV-2 research7,8,9. In addition, using this model, we evaluated the therapeutic efficacy of small-molecule antiviral agents for COVID-19 against these variants.
Results
Therapeutic effects of mAbs on BA.1 variants
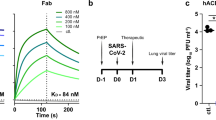
As of April 2022, the FDA has issued Emergency Use Authorizations (EUAs) to permit the emergency use of four different mAbs as therapeutic agents for the treatment and/or prevention of COVID-19 in adult and paediatric patients: REGEN-COV, a combination of imdevimab (REGN10987) and casirivimab (REGN10933); Xevudy, which is sotrovimab (VIR-7831); Evusheld (AZD7442), a combination of tixagevimab (COV2-2196 or AZD8955) and cilgavimab (COV2-2130 or AZD1061); and bebtelovimab (LY-CoV1404). We tested REGN10987/REGN10933, S309 (which is the precursor of sotrovimab) and COV2-2196/COV2-2130 for their therapeutic efficacy against BA.1. Sotrovimab for clinical use has been engineered with two amino acid mutations (M428L/N434S) in the fragment crystallizable (Fc) region, which extend the half-life of antibodies in vivo10. Both the COV2-2196 and COV2-2130 mAbs for clinical use contain the M252Y/S254T/T256E and L234F/L235E/P331S mutations in their Fc regions, which increase the half-life of antibodies and reduce the effector functions of antibodies, respectively11,12,13. All of the mAbs used in this study were synthesized according to publicly available sequences without any modifications (see Methods)14. The reactivity of all five mAbs was validated using enzyme-linked immunosorbent assay (ELISA) plates coated with recombinant S protein derived from the reference strain Wuhan/Hu-1/2019 and from a representative Omicron variant, and by neutralization assays; the results were consistent with previously published data4,6,14. We treated five hamsters with a single dose of the REGN10987/REGN10933 or COV2-2196/COV2-2130 combination (2.5 mg kg−1 each), or S309 as monotherapy (5 mg kg−1) by intraperitoneal injection on Day 1 after intranasal inoculation with 103 plaque-forming units (p.f.u.) of CoV-2/UT-HP095-1N/Human/2020/Tokyo (D614G; HP095) or hCoV-19/Japan/NC928-2N/2021 (Omicron BA.1; NC928) (Fig. 1a). A human mAb specific to the haemagglutinin of influenza B virus was injected intraperitoneally to five hamsters on Day 1 post-infection as a control. The animals were killed, and nasal turbinate and lung samples were collected for virus titrations on Day 4 post-infection. Sera were also collected at this timepoint and tested in an ELISA for RBD-specific IgG antibodies to confirm successful antibody transfer. Hamsters with low levels of ELISA titre (≤640) were excluded from further analysis.
a, Schematic diagram of the experimental workflow for assessing the therapeutic effects of monoclonal antibodies. b–d, Syrian hamsters were intranasally inoculated with 103 p.f.u. of D614G (HP095) (b), BA.1 (NC928) (c) or BA.1.1 (NC929) (d). On Day 1 post-infection of D614G (HP095) or BA.1 (NC928), the hamsters were intraperitoneally injected with a single dose of the REGN10987/REGN10933 or COV2-2196/COV2-2130 combination (2.5 mg kg−1 each), or S309 as monotherapy (5 mg kg−1). On Day 1 post-infection with BA.1.1 (NC929), the hamsters were intraperitoneally injected with a single dose of COV2-2130 as monotherapy (5 mg kg−1) or with the COV2-2196/COV2-2130 combination (2.5 mg kg−1 each). As a control, a human monoclonal antibody (1430E3/9) against the haemagglutinin of influenza B virus was injected. Hamsters were euthanized on Day 4 post-infection for virus titration. Sera were also collected at this timepoint, and titres of RBD-specific IgG antibodies in the sera were determined using ELISA plates coated with recombinant RBD derived from the S protein of Wuhan/Hu-1/2019 (GenBank accession no. MN908947). Top panels; ELISA titres and virus titres in animals treated with monoclonal antibodies. Red to blue shading represents the degree (high to low) of each titre in the animals. Bottom panels; bar graphs of virus titres in the respiratory organs of animals whose antibodies were successfully transferred. The endpoint titre is defined as the reciprocal of the highest dilution with an OD450 cut-off value ≥0.1. Antibody-transferred hamsters with low ELISA titres (≤640) (Nos. 1, 6, 48, and 49 denoted in red) were excluded from this analysis. The detection limit for virus titres was 1.7 log10(p.f.u. g−1). Vertical bars show the mean ± s.e.m. Points indicate data from individual hamsters (b, S309 and REGN10987/REGN10933, n = 4; d, COV2-2196/COV2-2130, n = 3; other groups in b–d, n = 5). The lower limit of detection is indicated by the horizontal dotted line. To compare the lung titres of the different groups in the BA.1 (NC928)-infected hamsters, we used a Kruskal-Wallis test followed by Dunn’s multiple comparisons test. To compare the nasal turbinate and lung titres of the different groups in the D614G (HP095) or BA.1.1 (NC929)-infected hamsters and the nasal turbinate titres of the different groups in the BA.1 (NC928)-infected hamsters, we used a one-way ANOVA followed by Dunnett’s multiple comparisons test. P < 0.05 was considered statistically significant.
For the D614G (HP095)-infected groups, treatment with REGN10987/REGN10933 or COV2-2196/COV2-2130 resulted in a significant reduction in virus titres in both the nasal turbinates (mean reduction in viral titre, 2.9 and 3.2 log10(p.f.u. g−1), respectively) and lungs (mean reduction in viral titre, 2.9 and 2.4 log10(p.f.u. g−1), respectively) compared with control mAb-treated animals (Fig. 1b). These results are consistent with those of previous studies in which the combinations of REGN10987/REGN10933 or COV2-2196/COV2-2130 were shown to have therapeutic activity against infection with early (USA-WA1/2020) or variant (USA-WA1/2020 N501Y/D614G) SARS-CoV-2 strains in rhesus macaques, hamsters and mice15,16,17. Virus titres in the lungs of animals treated with S309 were significantly lower than those in the organs of animals treated with the control mAb (mean reduction in viral titre, 1.5 log10(p.f.u. g−1)). In contrast, no differences in viral titres in the nasal turbinates were observed between the animals that were treated with this mAb and those treated with the control mAb. Thus, S309 showed less therapeutic effect against infection with D614G (HP095) compared with the other mAbs. For the BA.1 (NC928)-infected groups, neither S309 nor REGN10987/REGN10933 influenced the virus titres in the nasal turbinates or the lungs of the animals (Fig. 1c). However, COV2-2196/COV2-2130 significantly reduced the virus titres in the lungs of the animals (mean reduction in viral titre, 2.7 log10(p.f.u. g−1)), whereas the virus titres in their nasal turbinates were not affected by this treatment. Previous studies have shown that mutations at amino acid position 346 of the RBD affect the binding of class 3 mAbs such as COV2-213018,19,20,21. Next, we examined the neutralization activities of mAbs against an Omicron BA.1.1 (that is, hCoV-19/Japan/NC929-1N/2021; NC929; BA.1.1 is a subvariant of BA.1 possessing the R346K mutation in the S protein). A live-virus focus reduction neutralization assay revealed that BA.1.1 was neutralized by S309, REGN10933, COV2-2196, COV2-2130 or the combination of COV2-2196 and COV2-2130 to varying degrees (Supplementary Table 1), similar to our previous findings with Omicron BA.1 (NC928)14. However, unlike our previous results with BA.1 (NC928), COV2-2130 showed extremely high 50% focus reduction neutralization titre (FRNT50) values against BA.1.1 (NC929, 13,558.20 ng ml−1), suggesting that this therapeutic mAb may not be effective against BA.1.1 variants encoding the S-R346K mutation. We therefore asked whether the COV2-2196/COV2-2130 combination or COV2-2130 as monotherapy could inhibit the replication of BA.1.1 (NC929) in the respiratory tract of hamsters. We found that neither COV2-2130 nor COV2-2196/COV2-2130 had an effect on the virus titres in the nasal turbinates or the lungs of the animals (Fig. 1d). Taken together, these results indicate that the COV2-2196/COV2-2130 combination can restrict viral replication in the lungs of animals infected with BA.1 bearing S-346R even if the mAbs are administrated after the infection has occurred. In contrast, the COV2-2196/COV2-2130 combination may not be effective against BA.1.1 harbouring the S-R346K mutation.
Therapeutic effects of antivirals on BA.1 variants
Molnupiravir (an inhibitor of the RNA-dependent RNA polymerase of SARS-CoV-2) was approved by the FDA for the treatment of adult patients with COVID-19 on 23 December 2021. S-217622, an inhibitor of the main protease (also called 3CLpro) of SARS-CoV-2, is currently in clinical trials. We previously showed that the susceptibility of BA.1 (NC928) to molnupiravir was comparable to that of an early SARS-CoV-2 strain (NC002) and other variants of concern14. In this study, we confirmed that the BA.1 variant and the early (SARS-CoV-2/UT-NC002-1T/Human/2020/Tokyo) strains have similar sensitivities to S-217622 in vitro (Supplementary Table 2).
After establishing the in vitro sensitivity of the BA.1 variants to antiviral compounds, we assessed their therapeutic efficiencies in hamsters infected with the BA.1 (NC928). The dosage of molnupiravir for hamsters was determined on the basis of previous studies to evaluate the effect of molnupiravir against SARS-CoV-2 in the mouse model22. For S-217622, first we evaluated its pharmacokinetic (PK) parameters in hamsters. In hamsters administered S-217622 at 60 mg kg−1, the plasma concentration of S-217622 reached the maximum at 1.88 h and then declined with a half-life (t1/2,z) value of 3.43 h. The maximum concentration (Cmax), area under the concentration–time curve (AUC)0–24h and AUC0-inf values at 60 mg kg−1 were 128 µM, 937 µM h and 945 µM h, respectively (Extended Data Fig. 1 and Supplementary Table 3). These PK parameters indicate that the plasma concentration of S-217622 would be expected to be 15.6 µM at 12 h after dosing at 60 mg kg−1, which is higher than the 50% effective concentration (EC50; 1.73 µM) (Supplementary Table 2); therefore, we determined that we would administer S-217622 at a dosage of 60 mg kg−1 per 12 h. Hamsters intranasally infected with 103 p.f.u. of virus were treated by oral gavage twice daily (at 12 h intervals) for 1, 2 or 3 d with 500 mg kg−1 per 12 h (1,000 mg kg−1 d−1) molnupiravir or with 60 mg kg−1 per 12 h (120 mg kg−1 d−1) S-217622, beginning at 24 h post-infection (Fig. 2a). On Days 2, 3 or 4 post-infection, the animals were killed, and nasal turbinates and lungs were collected for virus titration. Although no differences in the virus titres in the nasal turbinates were found between the animals that were treated with molnupiravir and those treated with methylcellulose (control) on Days 3 and 4 post-infection, treatment with this compound led to a significant 7.3-fold reduction in virus titres in the nasal turbinates on Day 2 post-infection (Fig. 2b). Treatment with S-217622 resulted in significant 18.3 and 9.9-fold reductions in virus titres in the nasal turbinates on Days 2 and 4 post-infection, respectively. Moreover, both compounds dramatically reduced lung virus titres; no virus was recovered from the lungs of all four animals treated with molnupiravir at any timepoint post-infection, from the lungs of all four animals treated with S-217622 on Days 2 and 3 post-infection, or from the lungs of 3 of the 4 animals treated with S-217622 on Day 4 post-infection.
a, Schematic diagram of the experimental workflow for assessing the therapeutic effects of antiviral compounds. b, Syrian hamsters were intranasally inoculated with 103 p.f.u. of BA.1 (NC928). At 24 h post-infection (hpi), hamsters were treated with 500 mg kg−1 molnupiravir orally twice daily for 3 d or 60 mg kg−1 S-217622 orally twice daily for 3 d. Methylcellulose served as a control for oral treatment. Hamsters were euthanized on Days 2, 3 and 4 post-infection for virus titration. Vertical bars show the mean ± s.e.m. Points indicate data from individual hamsters (n = 4 per group). c, Schematic diagram of the experimental workflow for investigating the emergence of resistant variants. d,e, Four Syrian hamsters were intranasally inoculated with 103 p.f.u. of BA.1 (NC928). CPA was administered intraperitoneally to hamsters on Days −3, 1, 5 and 9 relative to infection. At 24 hpi, hamsters were treated with 500 mg kg−1 molnupiravir orally twice daily for 5 d or 60 mg kg−1 S-217622 orally twice daily for 5 d. Methylcellulose served as a control for oral treatment. d, Hamsters were euthanized on Days 7 and 14 post-infection for virus titration. Vertical bars show the mean ± s.e.m. Points indicate data from individual hamsters (n = 4 per group). e, Drug susceptibility of viruses. Viruses were isolated from the lungs of immunosuppressed animals treated with molnupiravir, S-217622 or the vehicle control on Days 7 and 14 post-infection. EC50 values of molnupiravir or S-217622 were determined using the Spearman–Karber formula on the basis of the appearance of visually detectable CPE in quadruplicate experiments. EIDD-1931 is the active form of molnupiravir. -, not applicable. Red to blue shading represents the degree (high to low) of each titre in the animals. In b and d, the lower limit of detection is indicated by horizontal dashed lines. To compare the lung and nasal turbinate titres of the different groups in the BA.1 (NC928)-infected hamsters, we used a Kruskal-Wallis test followed by Dunn’s multiple comparisons test, and a one-way ANOVA followed by Dunnett’s multiple comparisons test, respectively. P < 0.05 was considered statistically significant.
Prolonged replication of influenza viruses in drug recipients is associated with an increased risk of emergence of antiviral drug resistance23,24,25. Therefore, we asked whether treatment with these compounds in immunosuppressed hosts with prolonged viral shedding could result in the emergence of resistant variants. To generate an immunocompromised model, cyclophosphamide (CPA) was administered intraperitoneally to hamsters on Days −3, 1, 5 and 9 relative to infection as described previously26 (Fig. 2c). On Day 7 post-infection, virus titres were low in the nasal turbinates and lungs of untreated hamsters (Fig. 2d). In contrast, high levels of infection were sustained in the respiratory tract of the CPA-treated animals on Days 7 and 14 post-infection, indicating that immunosuppressive treatment with CPA lead to prolonged viral shedding. Both molnupiravir and S-217622 efficiently inhibited virus replication in the lungs of the immunosuppressed animals on Day 7 post-infection (mean reduction in viral titre, 4.2 and 3.4 log10(p.f.u. g−1), respectively) (Fig. 2d). These compounds also reduced the levels of infectious virus in the lungs on Day 14 post-infection, although the difference compared with the vehicle control group was not statistically significant. However, neither molnupiravir nor S-217622 affected the virus titres in the nasal turbinates of the animals on Days 7 and 14 post-infection. These results suggest that viral clearance cannot be achieved in immunocompromised hosts by the short-term use of these antiviral compounds. We determined the in vitro EC50 of molnupiravir and S-217622 against viruses isolated from the lungs of immunosuppressed animals treated with each compound or the vehicle control on Days 7 and 14 post-infection. The susceptibilities of isolates recovered from the drug-treated animals to each compound were comparable to those from control vehicle-treated animals (Fig. 2e). Deep sequencing analysis revealed that viruses isolated from the lungs of the molnupiravir-treated animal (#19) on Day 14 post-infection did not possess any mutations in the RNA-dependent RNA polymerase compared with the sequence from the samples from the control animal (#15) (Supplementary Table 4). No mutation was detected in the main protease of viruses recovered from the lungs of the S-217622-treated animals (#10 and #22) on Day 7 or Day 14 post-infection. The number of mutations detected in viruses isolated from the lungs of the molnupiravir-treated animal (#19) was greater than that from the control animal (#15) or S-217622-treated animals (#10 and #22).This finding is consistent with the mechanism of action of molnupiravir being a mutagen, leading to ‘error catastrophe’ during viral replication27. Together, these observations suggest that under the conditions tested, the emergence of resistant variants in immunosuppressed hamsters treated with molnupiravir or S-217622 appears to be limited.
Collectively, our observations suggest that the two antiviral compounds tested here considerably restrict Omicron BA.1 variant replication in the lower respiratory tract. In addition, animals treated with S-217622 had a significant reduction in virus titres in their upper respiratory tract.
Discussion
The emergence of SARS-CoV-2 Omicron variants carrying a large number of mutations in the RBD of the S protein has raised concern that these variants may limit the therapeutic usefulness of mAbs. In this study, we observed that the mAb combination COV2-2196/COV2-2130 efficiently suppressed the replication of an Omicron BA.1 variant lacking the S-R346K mutation in the lungs of hamsters when these mAbs were administrated 1 d post-infection, but was not effective against an Omicron BA.1.1 variant with the S-R346K mutation. Our results are consistent with those of previous studies in which mutations at position 346 of the RBD were found to confer immune escape from class 3 neutralizing mAbs such as COV2-213018,19,20.
Recent studies using in vitro neutralization assays have shown that sotrovimab and its parental form (S309) neutralize the Omicron variants4,6,14. In addition, prophylactic administration of hamster IgG2a S309 has been shown to prevent or significantly diminish the replication of SARS-CoV-2 in hamsters28. However, in this study, we observed that the therapeutic administration of this mAb had no effect on the virus titres in the respiratory tracts of hamsters infected with the BA.1 (NC928) variant. This lack of therapeutic efficacy against the BA.1 (NC928) variant may be due to the lower antibody-binding activities detected in animals at the time of virus titration (3 d after antibody administration) in S309-treated animals compared with COV2-2196/COV2-2130-treated animals (Fig. 1). Another study has shown that Fc effector functions enhance the therapeutic activity of neutralizing mAbs against SARS-CoV-2 infections in hamsters29. Because the S309 tested in this study originated from a human, its Fc receptor might not be optimal to recruit effector functions in hamsters. Further investigations are required to determine whether the replication of the BA.1 variants is efficiently inhibited by S309 possessing Fc domains modified to match the target host Fc receptors.
We observed that Omicron BA.1 variants replicated less efficiently in the lungs of infected hamsters (Fig. 2b), consistent with our previous study30. A recent study has shown that Omicron variants replicate to lower titres than Delta variants in lower airway organoids and Calu-3 lung cells31, although Omicron and Delta variants replicate with similar efficiency in human nasal epithelial cultures. Human protein transmembrane protease serine 2 (TMPRSS2)31, which is expressed at high levels in human and hamster lung32,33, activates the S protein of SARS-CoV-2 and the S protein of Omicron variants has been shown to inefficiently use TMPRSS2. Therefore, the reduced TMPRSS2 usage of the Omicron S protein may affect the replication of Omicron variants in the lungs of humans and hamsters.
Our study has several potential limitations: (1) Although hamsters are one of the most susceptible animals to SARS-CoV-2 among those tested, including mice and non-human primates, the Omicron BA.1 variants are attenuated in hamsters especially in the lungs. It is not known whether the Omicron variants in humans are as attenuated as in hamsters. The difference (if any) in the replication of the Omicron variants in humans and hamsters may affect the effectiveness of the mAbs and antiviral compounds; (2) We did not see efficacy with some of the mAbs or mAb cocktails. Because it is difficult to administer a large volume of antibodies intravenously to hamsters, we administered them intraperitonially. However, in humans, they are administered intravenously. The route of administration may affect the efficacy of antibodies; (3) The mAbs generated in this study are not identical to the mAbs in clinical use because amino acid substitutions have been introduced into clinical mAbs to enhance their half-lives and reduce their effector functions and this difference may have led to the lower efficacy in the hamster model; and (4) The mAbs tested in this study have the human IgG1 Fc region. Because the Fcγ receptors of humans and hamsters are different, inefficient Fc-mediated effector functions elicited by interactions with Fcγ receptors may have affected the efficacy in hamsters.
In conclusion, our data show that the two small-molecule antiviral agents molnupiravir and S-217622 may have therapeutic value against Omicron BA.1 variants of SARS-CoV-2. Our data also suggest that the mAb combination COV2-2196/COV2-2130 may be an effective treatment option against Omicron BA.1 variants that lack the S-R346K mutation. Importantly, however, this mAb combination may not provide effective treatment against Omicron BA.1.1 variants harbouring the S-R346K mutation. The use of therapeutic mAbs in patients infected with Omicron variants should be carefully considered.
Methods
Cells
VeroE6/TMPRSS2 (JCRB 1819) cells34,35 were propagated in the presence of 1 mg ml−1 geneticin (G418; Invivogen) and 5 μg ml−1 plasmocin prophylactic (Invivogen) in Dulbecco’s modified Eagle’s medium (DMEM) containing 10% fetal calf serum and antibiotics, and maintained at 37 °C with 5% CO2. Chinese hamster ovary (CHO) cells were maintained in DMEM containing 10% fetal calf serum and antibiotics at 37 °C with 5% CO2. Expi293 cells (Thermo Fisher) were maintained in Expi293 expression medium (Thermo Fisher) at 37 °C under 8% CO2. The cells were regularly tested for mycoplasma contamination using PCR, and confirmed to be mycoplasma-free.
Viruses
hCoV-19/Japan/NC928-2N/2021 (Omicron BA.1; NC928)14, hCoV-19/Japan/NC929-1N/2021(Omicron BA.1.1; NC929), SARS-CoV-2/UT-NC002-1T/Human/2020/Tokyo (NC002)7 and SARS-CoV-2/UT-HP095-1N/Human/2020/Tokyo (D614G; HP095)35 were propagated in VeroE6/TMPRSS2 cells in VP-SFM (Thermo Fisher). All experiments with SARS-CoV-2 were performed in enhanced biosafety level 3 containment laboratories at the University of Tokyo, which are approved for such use by the Ministry of Agriculture, Forestry and Fisheries, Japan.
Antibodies
Amino acid sequences for the variable region of the heavy and light chains of the following human monoclonal antibodies against the S protein were used for gene synthesis: clones tixagevimab (COV2-2196/AZD8895; GenBank accession numbers QLI33947 and QLI33948), casirivimab (REGN10933; PDB accession numbers 6XDG_B and 6XDG_D), cilgavimab (COV2-2130/AZD1061; GenBank accession numbers QKY76296 and QKY75909), imdevimab (REGN10987; PDB accession numbers 6XDG_A and 6XDG_A) and S309 (PDB accession numbers 6WS6_A and 6WS6_F). An artificial signal sequence and the constant gamma heavy (IgG1, UniProtKB/Swiss-Prot accession number P01857) and kappa (UniProtKB/Swiss-Prot accession number P01834) or lambda (UniProtKB/Swiss-Prot accession number P0DOY2) light chain coding sequences were added before and after each variable region. Codon usage was optimized for expression in CHO cells. The synthesized genes were cloned into a plasmid for protein expression and transfected into CHO cells. Cell culture media were collected after incubation for 10–14 d at 37 °C. A human monoclonal antibody (1430E3/9) against the haemagglutinin of influenza B virus36 was previously cloned into the expression vector Mammalian Power Express System (TOYOBO) and was transiently expressed by Expi293 cells. Monoclonal antibodies were purified by using MabSelect SuRe LX (Cytiva) or a protein A column. Purity was confirmed by SDS–PAGE and/or HPLC before use. The reactivities of these antibodies against SARS-CoV-2, including the Alpha, Beta, Delta, Gamma and Omicron variants, have been tested previously14.
Antiviral compounds
Molnupiravir (EIDD-2801) was purchased from MedChemExpress. S-217622 was kindly provided by Shionogi Co., Ltd. All compounds were dissolved in 0.5% methylcellulose before use in in vivo experiments.
Pharmacokinetics studies in Syrian hamsters
Male Syrian hamsters (5 weeks) were purchased from Japan SLC. The dosing vehicle was 0.5% (w/v) methylcellulose (400 cP). The compound was orally administered at 60 mg kg−1 (n = 4) under non-fasted conditions. Blood samples (0.1 ml) were collected with disposable syringes containing anticoagulants (EDTA 2K and heparin) at 0.5, 1, 2, 4, 8 and 24 h after dosing. Blood samples were centrifuged (1,800 × g, 4 °C, 10 min) to obtain plasma samples, which were transferred to tubes and stored in a freezer until analysed. Plasma concentrations were determined using a liquid chromatography–tandem mass spectrometry (LC–MS/MS) system following protein precipitation with acetonitrile (MeCN). The LC–MS/MS system, equipped with a positive electrospray ionization (ESI) surface, consisted of an API5000 tandem mass spectrometer (AB SCIEX) and a Nexera ultra high-performance liquid chromatograph system (Shimadzu). The multiple reaction monitoring mode was selected and monitored the precursor ion (m/z 532.347) and product ion (m/z 145.042). The cone voltage and collision energy were set to 90 V and 55 V, respectively. The column YMC-Triart C18 (3 µm, 2.1 mm Inner Diameter (I.D.) × 50 mm, YMC) was used and column temperature was maintained at 40 °C for chromatographic separation of analytes. The mobile phases were 0.1% (v/v) formic acid in distilled water (mobile phase A) and MeCN (mobile phase B). The flow rate was 0.75 ml min−1. The gradient condition was 30-65-95-95-30 (% of mobile phase B concentration)/0-0.9-0.91-1.1-1.11-1.5 (min). Pharmacokinetic parameters of S-217622 in plasma were calculated by using WinNonlin (Ver. 8.3, Certara, L.P.) on the basis of a non-compartment analysis with uniform weighting. The concentration of S-217622 at 12 h after single oral administration of S-217622 was simulated using a non-parametric analysis from the mean plasma concentration data after single oral administration of S-217622 at 60 mg kg−1.
Evaluation of therapeutic efficacy of mAbs and antiviral compounds in Syrian hamsters
Five- to six-week-old male Syrian hamsters (Japan SLC) were used in this study. For the evaluation of mAb efficacy in hamsters, under isoflurane anaesthesia, five hamsters per group were inoculated intranasally with 103 p.f.u. (in 30 μl) of HP095, BA.1 (NC928) or BA.1.1 (NC929). On Day 1 post-infection, the hamsters were injected intraperitoneally with 1 ml of a mAb preparation (5 mg kg−1). The animals were euthanized on Day 4 post-infection, and the virus titres in the nasal turbinates and lungs were determined using plaque assays on VeroE6/TMPRSS2 cells.
For the evaluation of antiviral compound efficacy in hamsters, under isoflurane anaesthesia, four hamsters per group were inoculated intranasally with 103 p.f.u. (in 30 μl) of BA.1 (NC928). At 24 h after inoculation, hamsters were treated with the following antiviral compounds: (1) molnupiravir, 500 mg kg−1 (in 1 ml) administered orally twice daily; (2) S-217622, 60 mg kg−1 (in 1 ml) administered orally twice daily; or (3) methylcellulose (1 ml) as a control for oral treatment. The animals were euthanized on Day 2, 3 or 4 post-infection, and the virus titres in the nasal turbinates and lungs were determined using plaque assays on VeroE6/TMPRSS2 cells.
For the evaluation of the emergence of antiviral-resistant virus in hamsters, CPA was administered intraperitoneally to hamsters on Day −3 (140 mg kg−1), 1 (100 mg kg−1), 5 (100 mg kg−1) and 9 (100 mg kg−1) relative to infection. Under isoflurane anaesthesia, four hamsters per group were inoculated intranasally with 103 p.f.u. (in 30 μl) of BA.1 (NC928) on Day 0. At 24 h after inoculation, the hamsters were treated with the following antiviral compounds for 5 d: (1) molnupiravir, 500 mg kg−1 (in 1 ml) administered orally twice daily; (2) S-217622, 60 mg kg−1 (in 1 ml) administered orally twice daily; or (3) methylcellulose (1 ml) as a control for oral treatment. The animals were euthanized on Day 7 or 14 post-infection, and the virus titres in the nasal turbinates and lungs were determined using plaque assays on VeroE6/TMPRSS2 cells. Viruses were also isolated from lung homogenates for EC50 determination and viral genome analysis.
All experiments with hamsters were performed in accordance with the Science Council of Japan’s Guidelines for Proper Conduct of Animal Experiments and the guidelines set by the Institutional Animal Care committee. The protocols were approved by the Animal Experiment Committee of the Institute of Medical Science, the University of Tokyo (approval number PA19-75).
ELISA
ELISA was performed as previously reported37. Briefly, 96-well Maxisorp microplates (Nunc) were incubated with the recombinant RBD of the S protein or HexaPro prefusion-stabilized versions of the S ectodomain (S6pro)38 (prototype virus or omicron variant) (50 μl per well at 2 μg ml−1), or with PBS at 4 °C overnight and were then incubated with 5% skim milk in PBS containing 0.05% Tween-20 (PBS-T) for 1 h at room temperature. The microplates were reacted for 1 h at room temperature with hamster serum samples (initially diluted 40-fold) or monoclonal antibodies (1 µg ml−1) in PBS-T containing 5% skim milk and subsequently serially 2-fold diluted, followed by peroxidase-conjugated goat anti-human IgG, Fcγ fragment-specific antibody (Jackson Immuno-Research) for 1 h at room temperature. Then, 1-Step Ultra TMB-Blotting solution (Thermo Fisher) was added to each well, followed by incubation for 3 min at room temperature. The reaction was stopped by the addition of 2 M H2SO4 and the optical density at 450 nm (OD450) was immediately measured. The average OD450 values of two PBS wells were subtracted from the average OD450 values of the two RBD or S6pro wells for background correction. A subtracted OD450 value of 0.1 or more was regarded as positive; the minimum dilution to give a positive result was used as the ELISA titre (for hamster serum) or the minimum concentration to bind S protein (for monoclonal antibodies).
FRNT
Neutralization activities of SARS-CoV-2 were determined using a focus reduction neutralization assay as previously described14,39. Serial dilutions of monoclonal antibodies (starting concentration, 50,000 ng ml−1) were mixed with 1,000 focus-forming units of virus per well and incubated for 1 h at 37 °C. The antibody–virus mixture was inoculated on VeroE6/TMPRSS2 cells in 96-well plates in duplicate and incubated for 1 h at 37 °C. An equal volume of 1.2% Avicel RC-581 (DuPont Nutrition) in culture medium was added to each well. The cells were incubated for 24 h at 37 °C and then fixed with formalin. After the formalin was removed, the cells were immunostained with a mouse monoclonal antibody against SARS-CoV-1/2 nucleoprotein (clone 1C7C7, Sigma-Aldrich), followed by a horseradish peroxidase-labelled goat anti-mouse immunoglobulin (SeraCare Life Sciences). The infected cells were stained with TrueBlue Substrate (SeraCare Life Sciences) and then washed with distilled water. After cell drying, the focus numbers were quantified using an ImmunoSpot S6 Analyzer, ImmunoCapture software and BioSpot software (Cellular Technology). The results are expressed as FRNT50 values, which were calculated using GraphPad Prism software.
Determination of EC50 values
VeroE6/TMPRSS2 cells were seeded in 96-well plates 1 d before infection and incubated at a multiplicity of infection of 0.01 with SARS-CoV-2 at 37 °C for 1 h. The inocula were then replaced with MEM containing 5% fetal calf serum and serially diluted EIDD-1931 (the active form of molnupiravir) or S-217622, and the cells were incubated at 37 °C with 5% CO2 for 3 d to observe cytopathic effects (CPE). The EC50 was determined using the Spearman–Karber formula40 on the basis of the appearance of visually detectable CPE in quadruplicate experiments.
Whole-genome sequencing
Viral RNA was extracted using a QIAamp viral RNA mini kit (QIAGEN). The whole genome of SARS-CoV-2 was amplified using a modified ARTIC network protocol as described previously41. Briefly, viral complementary DNA was synthesized from the extracted RNA using a LunarScript RT SuperMix kit (New England BioLabs). The DNA was amplified by performing a multiplexed PCR in two pools using the ARTIC-N1 primers v5 and the Q5 Hot Start DNA polymerase (New England BioLabs). The DNA libraries for Illumina NGS were prepared from pooled amplicons using a QIAseq FX DNA library kit (QIAGEN) and were then analysed using the iSeq 100 System (Illumina). To determine the sequence of hCoV-19/Japan/NC929-1N/2021 (Omicron; NC929), the reads were assembled using the CLC Genomics Workbench (version 21, Qiagen), with the Wuhan/Hu-1/2019 sequence (GenBank accession no. MN908947) as a reference. The sequence of NC929 was deposited in the Global Initiative on Sharing All Influenza Data (GISAID) database with accession ID: EPI_ISL_7890636. For the analysis of the viral genomes isolated from the lungs of hamsters treated with antiviral compounds, the reads were assembled using the CLC Genomics Workbench (version 22, Qiagen), with the NC928 sequence (GISAID accession no. EPI_ISL_7507055) as a reference. Amino acid mutations detected at a frequency of ≥10% are listed.
Statistical analysis
GraphPad Prism software was used to analyse all data. We compared virus titres in hamster organs with the control using a one-way analysis of variance (ANOVA) followed by Dunnett’s multiple comparisons test, or the Kruskal-Wallis test followed by Dunn’s test with multiple comparisons. Differences between groups were considered significant for P < 0.05.
Reagent availability
All reagents described in this paper are available through Material Transfer Agreements.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All data supporting the findings of this study are available in the paper. There are no restrictions in obtaining access to the primary data. The sequence of hCoV-19/Japan/NC929-1N/2021 (Omicron BA.1.1; NC929) was deposited in the Global Initiative on Sharing All Influenza Data (GISAID) database with accession ID: EPI_ISL_7890636. Source data are provided with this paper.
Code availability
No code was used in the course of the data acquisition or analysis.
References
Walls, A. C. et al. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell 181, 281–292.e6 (2020).
Planas, D. et al. Considerable escape of SARS-CoV-2 Omicron to antibody neutralization. Nature https://doi.org/10.1038/s41586-021-04389-z (2022).
Cameroni, E. et al. Broadly neutralizing antibodies overcome SARS-CoV-2 Omicron antigenic shift. Nature https://doi.org/10.1038/s41586-021-04386-2 (2022).
Cao, Y. et al. Omicron escapes the majority of existing SARS-CoV-2 neutralizing antibodies. Nature https://doi.org/10.1038/s41586-021-04385-3 (2022).
Carreño, J. M. et al. Activity of convalescent and vaccine serum against SARS-CoV-2 Omicron. Nature https://doi.org/10.1038/s41586-022-04399-5 (2022).
Liu, L. et al. Striking antibody evasion manifested by the omicron variant of SARS-CoV-2. Nature https://doi.org/10.1038/s41586-021-04388-0 (2022).
Imai, M. et al. Syrian hamsters as a small animal model for SARS-CoV-2 infection and countermeasure development. Proc. Natl Acad. Sci. USA 117, 16587–16595 (2020).
Sia, S. F. et al. Pathogenesis and transmission of SARS-CoV-2 in golden hamsters. Nature 583, 834–838 (2020).
Chan, J. F. et al. Simulation of the clinical and pathological manifestations of coronavirus disease 2019 (COVID-19) in a golden Syrian hamster model: implications for disease pathogenesis and transmissibility. Clin. Infect. Dis. 71, 2428–2446 (2020).
Zalevsky, J. et al. Enhanced antibody half-life improves in vivo activity. Nat. Biotechnol. 28, 157–159 (2010).
Dall’Acqua, W. F. et al. Increasing the affinity of a human IgG1 for the neonatal Fc receptor: biological consequences. J. Immunol. 169, 5171–5180 (2002).
Oganesyan, V., Gao, C., Shirinian, L., Wu, H. & Dall’Acqua, W. F. Structural characterization of a human Fc fragment engineered for lack of effector functions. Acta Crystallogr. D 64, 700–704 (2008).
Corti, D., Purcell, L. A., Snell, G. & Veesler, D. Tackling COVID-19 with neutralizing monoclonal antibodies. Cell 184, 3086–3108 (2021).
Takashita, E. et al. Efficacy of antibodies and antivirals against a SARS-CoV-2 Omicron variant. N. Engl. J. Med. 386, 995–998 (2022).
Baum, A. et al. Antibody cocktail to SARS-CoV-2 spike protein prevents rapid mutational escape seen with individual antibodies. Science 369, 1014–1018 (2020).
Zost, S. J. et al. Potently neutralizing and protective human antibodies against SARS-CoV-2. Nature 584, 443–449 (2020).
Chen, R. E. et al. In vivo monoclonal antibody efficacy against SARS-CoV-2 variant strains. Nature 596, 103–108 (2021).
Barnes, C. O. et al. SARS-CoV-2 neutralizing antibody structures inform therapeutic strategies. Nature 588, 682–687 (2020).
Dong, J. et al. Genetic and structural basis for SARS-CoV-2 variant neutralization by a two-antibody cocktail. Nat. Microbiol. 6, 1233–1244 (2021).
Greaney, A. J. et al. Mapping mutations to the SARS-CoV-2 RBD that escape binding by different classes of antibodies. Nat. Commun. 12, 4196 (2021).
Garcia-Beltran, W. F. et al. mRNA-based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. Cell https://doi.org/10.1016/j.cell.2021.12.033 (2022).
Wahl, A. et al. SARS-CoV-2 infection is effectively treated and prevented by EIDD-2801. Nature 591, 451–457 (2021).
Bowden, R. A. Respiratory virus infections after marrow transplant: the Fred Hutchinson Cancer Research Center experience. Am. J. Med 102, 27–30 (1997).
Englund, J. A. et al. Common emergence of amantadine- and rimantadine-resistant influenza A viruses in symptomatic immunocompromised adults. Clin. Infect. Dis. 26, 1418–1424 (1998).
Ison, M. G., Gubareva, L. V., Atmar, R. L., Treanor, J. & Hayden, F. G. Recovery of drug-resistant influenza virus from immunocompromised patients: a case series. J. Infect. Dis. 193, 760–764 (2006).
Brocato, R. L. et al. Protective efficacy of a SARS-CoV-2 DNA vaccine in wild-type and immunosuppressed Syrian hamsters. NPJ Vaccines 6, 16 (2021).
Kabinger, F. et al. Mechanism of molnupiravir-induced SARS-CoV-2 mutagenesis. Nat. Struct. Mol. Biol. 28, 740–746 (2021).
Lempp, F. A. et al. Lectins enhance SARS-CoV-2 infection and influence neutralizing antibodies. Nature 598, 342–347 (2021).
Winkler, E. S. et al. Human neutralizing antibodies against SARS-CoV-2 require intact Fc effector functions for optimal therapeutic protection. Cell 184, 1804–1820.e16 (2021).
Halfmann, P. J. et al. SARS-CoV-2 Omicron virus causes attenuated disease in mice and hamsters. Nature 603, 687–692 (2022).
Meng, B. et al. Altered TMPRSS2 usage by SARS-CoV-2 Omicron impacts infectivity and fusogenicity. Nature 603, 706–714 (2022).
Ferren, M. et al. Hamster organotypic modeling of SARS-CoV-2 lung and brainstem infection. Nat. Commun. 12, 5809 (2021).
Tomris, I. et al. Distinct spatial arrangements of ACE2 and TMPRSS2 expression in Syrian hamster lung lobes dictates SARS-CoV-2 infection patterns. PLoS Pathog. 18, e1010340 (2022).
Matsuyama, S. et al. Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells. Proc. Natl Acad. Sci. USA 117, 7001–7003 (2020).
Imai, M. et al. Characterization of a new SARS-CoV-2 variant that emerged in Brazil. Proc. Natl Acad. Sci. USA https://doi.org/10.1073/pnas.2106535118 (2021).
Yasuhara, A. et al. Antigenic drift originating from changes to the lateral surface of the neuraminidase head of influenza A virus. Nat. Microbiol. 4, 1024–1034 (2019).
Yamayoshi, S. et al. Antibody titers against SARS-CoV-2 decline, but do not disappear for several months. EClinicalMedicine 32, 100734 (2021).
Hsieh, C. L. et al. Structure-based design of prefusion-stabilized SARS-CoV-2 spikes. Science 369, 1501–1505 (2020).
Vanderheiden, A. et al. Development of a rapid focus reduction neutralization test assay for measuring SARS-CoV-2 neutralizing antibodies. Curr. Protoc. Immunol. 131, e116 (2020).
Ramakrishnan, M. A. Determination of 50% endpoint titer using a simple formula. World J. Virol. 5, 85–86 (2016).
Uraki, R. et al. Characterization and antiviral susceptibility of SARS-CoV-2 Omicron/BA.2. Nature https://doi.org/10.1038/s41586-022-04856-1 (2022).
Acknowledgements
We thank Shionogi Co., Ltd. for providing S-217622 and its pharmacokinetic data in hamsters; S. Watson for scientific editing; and K. Yokota for technical assistance. This work was supported by a Research Program on Emerging and Re-emerging Infectious Diseases (JP20fk0108412, JP21fk0108615 and JP20fk0108472), a Project Promoting Support for Drug Discovery (JP20nk0101632), the Japan Program for Infectious Diseases Research and Infrastructure (JP22wm0125002) from the Japan Agency for Medical Research and Development, the National Institutes of Allergy and Infectious Diseases Center for Research on Influenza Pathogenesis (HHSN272201400008C), and the Center for Research on Influenza Pathogenesis and Transmission (CRIPT) (75N93021C00014).
Author information
Authors and Affiliations
Contributions
R.U., M.K. and M. Imai performed the in vivo experiments. M.K., S.Y., M. Ito, E.T., M.U., Y.F., A.Y., K.I.-H. and Y.S.-T. performed the in vitro experiments. S.Y. and S.F. performed deep sequencing analysis and interpretation. R.U., M.K., M. Imai, S.Y., S.W., H.H. and Y.K. obtained funding, conceived the study and supervised the research. R.U., M. Imai and Y.K. wrote the initial draft, with all other authors providing editorial comments.
Corresponding author
Ethics declarations
Competing interests
Y.K. has received unrelated funding support from Daiichi Sankyo Pharmaceutical, Toyama Chemical, Tauns Laboratories, Inc., Shionogi & Co. LTD, Otsuka Pharmaceutical, KM Biologics, Kyoritsu Seiyaku, Shinya Corporation and Fuji Rebio. All other authors declare no competing interests.
Peer review
Peer review information
Nature Microbiology thanks Robert Garry, Stanley Perlman and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Plasma concentration profile of S-217622 after single oral administration to hamsters at 60 mg/kg.
S-217622 was orally administered to Syrian hamsters at 60 mg/kg under non-fasted conditions. Blood samples (0.1 mL) were collected at 0.5, 1, 2, 4, 8, and 24 h after dosing and the plasma concentrations of S-217622 were determined. Data are expressed as the mean ± SD (n = 4/group).
Supplementary information
Supplementary Tables 1–4
Supplementary Table 1. Efficacy of monoclonal antibodies against SARS-CoV-2 Omicron BA1.1 variant in vitro. Supplementary Table 2. Virus sensitivity to S-217622 in vitro. Supplementary Table 3. Pharmacokinetic parameters of S-217622 in plasma after single oral administration to hamsters at 60 mg kg−1. Supplementary Table 4. Sequence changes in viruses isolated from the lungs of immunosuppressed hamsters after treatment with antiviral compounds.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 1
Statistical source data.
Rights and permissions
About this article
Cite this article
Uraki, R., Kiso, M., Imai, M. et al. Therapeutic efficacy of monoclonal antibodies and antivirals against SARS-CoV-2 Omicron BA.1 in Syrian hamsters. Nat Microbiol 7, 1252–1258 (2022). https://doi.org/10.1038/s41564-022-01170-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-022-01170-4