Abstract
Noninvasive disease monitoring and risk stratification by circulating tumor DNA (ctDNA) profiling has become a potential novel strategy for patient management in B-cell lymphoma. Emerging innovative therapeutic options and an unprecedented growth in our understanding of biological and molecular factors underlying lymphoma heterogeneity have fundamentally increased the need for precision-based tools facilitating personalized and accurate disease profiling and quantification. By capturing the entire mutational landscape of tumors, ctDNA assessment has some decisive advantages over conventional tissue biopsies, which usually target only one single tumor site. Due to its non- or minimal-invasive nature, serial and repeated ctDNA profiling provides a real-time picture of the genetic composition and facilitates quantification of tumor burden any time during the course of the disease. In this review, we present a comprehensive overview of technologies used for ctDNA detection and genotyping in B-cell lymphoma, focusing on pre-analytical and technical requirements, the advantages and limitations of various approaches, and highlight recent advances around improving sensitivity and suppressing technical errors. We broadly review potential applications of ctDNA in clinical practice and for translational research by describing how ctDNA might enhance lymphoma subtype classification, treatment response assessment, outcome prediction, and monitoring of measurable residual disease. We finally discuss how ctDNA could be implemented in prospective clinical trials as a novel surrogate endpoint and be utilized as a decision-making tool to guide lymphoma treatment in the future.
Similar content being viewed by others
Introduction
With the advent of precision medicine, our understanding and knowledge of B-cell lymphoma biology, molecular subtypes, and genetic landscapes have substantially increased over the last decade [1,2,3]. Similarly, major recent advances in basic and translational research have enhanced therapeutic options in lymphoma, including novel targeted agents, bispecific monoclonal antibodies, and cellular-based immunotherapies such as the chimeric antigen receptor T- (CAR T-) cell therapy [4]. As a result, identifying patient subgroups with high risk for treatment failure, predicting clinical outcomes early at diagnosis or during therapy, and optimizing patient selection for specific treatment strategies have moved to the core of modern translational lymphoma research and patient management [5].
Invasive tissue biopsies are the gold standard to obtain molecular information and to stratify lymphoma patients into genetic subgroups [3, 6]. However, such invasive procedures have several limitations. Surgical interventions carry procedural risks and often cannot be performed in patients with severe pre-existing health conditions or when tumor lesions are inaccessible. Furthermore, tissue biopsies do not fully capture spatial and temporal tumor heterogeneity, because only one single tumor site is usually sampled, and serial biopsies are not available in most cases [7,8,9,10,11,12]. Therefore, precise and accurate technologies that facilitate detection, quantification, and characterization of B-cell lymphomas in real-time are needed to overcome these limitations and to help succeed novel strategies of lymphoma precision medicine.
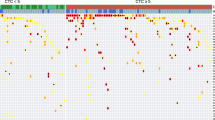
‘Liquid biopsy’ has emerged as an innovative approach to detect and characterize cancers non- or minimal-invasively through profiling of tumor-derived analytes in body fluids, most commonly blood but also cerebrospinal fluid (CSF), urine, ascites, pleural fluid, or saliva [13,14,15,16,17,18,19,20]. Circulating tumor DNA (ctDNA) in the blood plasma or CSF has become the most investigated analyte in B-cell lymphomas, as the majority of lymphoma patients do not present with circulating disease and therefore, circulating tumor cells (CTCs) are usually a less attractive target (Fig. 1) [21]. Circulating tumor DNA is shed from tumor deposits into circulation and represents a subset of the total cell-free DNA (cfDNA) pool released from cells undergoing apoptosis or necrosis [22]. Major advances in polymerase chain reaction- (PCR-) and next-generation sequencing- (NGS-) based technologies have led to improved detection of minimal ctDNA amounts in body fluids, facilitating ultrasensitive detection of minute residual tumor masses during or after therapy (measurable residual disease, MRD) for early identification of treatment failure and prediction of disease relapse in numerous cancer entities including lymphoma. As ctDNA reflects all types of tumor-specific genetic alterations including single nucleotide variants (SNVs), translocations, insertions/deletions (indels), and copy number variations (CNVs), it potentially allows comprehensive assessment of spatial tumor heterogeneity between different tumor lesions, classification of molecular subtypes, and the identification of temporal heterogeneity such as the emergence of resistance mutations over time [11, 15]. Both non- or minimal-invasive quantification of tumor burden and the characterization of tumor heterogeneity have potential clinical utility at various lymphoma milestones, with MRD monitoring during and after treatment being the most established application of ctDNA as of yet (Fig. 2) [5, 21, 23,24,25].
Cell-free DNA and circulating tumor DNA are released from malignant and non-malignant tissue into the blood stream and cerebrospinal fluid, where they can be accessed through blood draws and lumbar punctures. In lymphoma, ctDNA obtained from blood plasma or cerebrospinal fluid has been studied as a non- or minimal-invasive clinical biomarker. At the bottom, various aspects of cfDNA and ctDNA analyses in lymphoma patients are highlighted, including quantification of tumor burden and MRD monitoring during and after therapies, noninvasive tumor genotyping for lymphoma classification and characterization of tumor heterogeneity, and fragmentation patterns.
Profiling of ctDNA might be performed at various disease landmarks at diagnosis, during treatment, during surveillance, and at lymphoma progression to support decision-making by physicians or contribute novel insights to address innovative translational research questions. CNS central nervous system, MRD minimal residual disease.
In this review, we present an overview of current technologies used for ctDNA-based lymphoma quantification and profiling, illustrate advantages and limitations of the most commonly used liquid biopsy methods, discuss technical factors influencing their performance, and highlight recent advances to improve sensitivity and specificity. Furthermore, we highlight potential clinical applications and the perspectives for translational research of ctDNA analyses in various B-cell lymphoma entities at distinct clinical landmarks, and show how ctDNA could inform innovative clinical trials and guide personalized patient management in the near future.
Technical considerations for ctDNA detection and quantification
The utility of liquid biopsy technologies largely relies on adequate sensitivity and specificity to detect minute amounts of ctDNA in body fluids. Recent developments in molecular biology, high-throughput analytics, and bioinformatics have overcome major obstacles such as pre-analytical limitations, low recovery rates of cfDNA molecules or the high abundance of technical errors introduced during library preparation and the hybridization process, and substantially enhanced the technical performance of liquid biopsy methods [21, 24, 26].
Several pre-analytical factors need to be considered to ensure optimal sample collection and cfDNA processing in lymphoma patients. First, the detection limit of most liquid biopsy technologies heavily depends on the number of cfDNA molecules analyzed. Concentrations of cfDNA in lymphoma are highly variable, ranging from a median of ~6.5 ng/mL of plasma in indolent follicular lymphoma (FL) to ~650 ng/mL in primary mediastinal B-cell lymphomas (PMBCL), and are significantly associated with tumor stage [27, 28]. Thus, at least 10 mL of blood (≈4–6 mL blood plasma) are generally recommended to obtain a sufficient number of cfDNA molecules for subsequent analyses [24, 28, 29]. Second, when blood is collected in EDTA tubes, plasma should be isolated within 6 hours to avoid contamination of the plasma fraction with cellular DNA released from peripheral blood mononuclear cell (PBMC) lysis [29]. Cell-stabilizing tubes such as Streck® or PAXgene® tubes minimize the contamination effect, are stable at room temperature for approximately 7 days, and are preferred if tubes need to be shipped or stored for a longer time [30]. Finally, the presence of germline variants and clonal hematopoiesis of indeterminate potential (CHIP) could act as confounders and hamper accurate detection of somatic tumor-derived aberrations in ctDNA, particularly in the setting of tumor-agnostic noninvasive genotyping. Thus, paired sequencing of germline DNA (either from plasma-depleted whole blood, saliva, or buccal swabs) and leukocyte-derived DNA is recommended to subtract those errors from cfDNA analysis [29, 31,32,33,34].
There are numerous technologies available for ctDNA profiling that can be categorized into PCR-based methods (e.g., allele-specific oligonucleotide PCR [ASO-PCR] and digital droplet PCR [ddPCR]) and NGS-based approaches (Table 1). They can further be divided into those technologies allowing sensitive MRD detection and those that facilitate both MRD quantification and comprehensive assessment of mutational landscapes (i.e., genotyping). While PCR assays are cost effective, relatively easy to use, and have a short turnaround time, they can only target one single or a small number of recurrent somatic variants and are therefore not the preferred choice for broad noninvasive genotyping. Similar to other single-gene methods, sensitivities of PCR-based methods usually do not exceed allele frequencies (AF) of ~0.005%, because the cfDNA input is typically limited to a maximum of ~20,000 haploid genome equivalents (hGE) per blood draw (Table 1) [35]. Therefore, they are frequently used for MRD monitoring in lymphomas with highly recurrent chromosomal translocations such as t(14;18) in FL or t(11;14) in mantle cell lymphoma (MCL) (preferentially ASO-PCR), or with stereotypic mutations such as MYD88L265P in primary CNS lymphoma (PCNSL), waldenstrom macroglobulinemia (WM), or (MCD-, C5-) diffuse large B-cell lymphoma (DLBCL), and EZH2Y641N in FL or (EZB-, C3-) DLBCL [3, 6].
NGS-based technologies allow massive parallel sequencing of DNA molecules in a single flow cell [35]. Lymphomas are characterized by patient-specific clonal rearrangements of their immunoglobulin (Ig) V(D)J regions (=clonotypes), which can be identified in tumor tissue and monitored in cfDNA over time by NGS-based methods utilizing universal primer sets targeting the Ig heavy and light chains (IgHTS, clonoSEQ®) (Table 1). This assay, provided by Adaptive Biotechnologies, is FDA approved for MRD detection in patients with chronic lymphocytic leukemia (CLL), multiple myeloma (MM), and B-cell acute lymphoblastic leukemia (B-ALL) and has been utilized in most lymphomas for disease monitoring [36,37,38,39]. However, like other single-gene assays, IgHTS only captures one single genetic marker and its ctDNA detection limit is restricted to the number of cfDNA molecules analyzed (typically ~0.005%, see above, Table 1). Furthermore, due to high rates of somatic hypermutation (SHM) in germinal center lymphomas, in particular FL and DLBCL, IgHTS fails to detect clonal V(D)J-rearrangements in ~20% of patients, which limits its applicability in these lymphoma entities [35, 37, 38, 40].
Targeted amplicon-based or hybrid-capture NGS technologies have several dedicated advantages over single gene assays (Table 1). They target hundreds of lymphoma-specific genetic regions and enable the identification of the entire spectrum of genetic alterations (i.e., SNVs, indels, translocations, and CNVs) [12, 21, 26, 27, 41,42,43]. They typically utilize entity-specific sequencing panels that cover genetic regions known to be frequently mutated in lymphomas. Consequently, they do not require patient-specific optimization, are usually applicable to a broader population of patients, allow comprehensive genotyping from cfDNA and, through the identification of subclonal and low-frequency alterations, facilitate characterization of spatial and temporal tumor heterogeneity. Due to the ability to track multiple mutations per patient simultaneously and recent major advances in molecular biology and in silico strategies that suppress technical errors, sensitivity of targeted NGS-based approaches could be substantially improved. For example, Cancer Personalized Profiling by Deep Sequencing (CAPP-Seq) combines a unique barcoding strategy with a downstream bioinformatics algorithm that largely eliminates sequencing errors and stereotypic background (integrated digital error suppression, iDES), facilitating ctDNA detection down to an AF of ~0.002% [12, 26, 27, 42].
In situations with extremely low tumor burden, particularly during treatment and at the end of lymphoma therapy, current methods are still limited by suboptimal sensitivity [44,45,46]. Prior studies have used somatic mutations identified on both DNA strands to further decrease ctDNA detection limits (‘duplex sequencing’). This NGS-based strategy reduces sequencing errors by requiring two concordant events on both Watson and Crick strands for the detection of one SNV, achieving an analytical sensitivity of ~0.0002% [26, 47, 48]. Yet, the majority of recovered DNA molecules are single-stranded and only a minority contains both strands. Since maximal recovery of hGE is essential to liquid biopsy NGS approaches, this inefficacy substantially limits the applicability of duplex sequencing in the real-world setting (Table 1) [21, 26, 49]. To overcome this limitation, an innovative approach has been developed that further maximizes analytical sensitivity and reduces background error rates by tracking two or more variants (‘phased variants’) on the same strand of one single DNA molecule (‘PhasED-seq’, Phased Variant Enrichment and Detection Sequencing). This method offers extremely low error profiles while maintaining high genome recovery, thus facilitating ctDNA monitoring down to an analytical detection limit of ~0.00005% (i.e., 1 in 2,000,000, Table 1). PhasED-seq seems particularly useful in B-cell lymphoma, as mutations accumulate in stereotyped genetic regions caused by ongoing SHM and aberrant SHM through the activity of the enzyme activation-induced cytidine deaminase (AID) [49,50,51]. A similar strategy has been introduced recently by Meriranta et al., providing additional evidence that tracking of phased variants can significantly improve sensitivity of ctDNA detection in lymphoma patients [52].
Applications of ctDNA in lymphoma
Diagnostic tumor quantification by ctDNA and its prognostic value
The accurate reflection of tumor burden at diagnosis is a crucial characteristic of ctDNA as a noninvasive biomarker, because pretreatment disease burden is an established risk factor in various lymphoma entities and generally associated with worse outcomes. Numerous risk factors are a direct portrait of lymphoma burden such as the International Prognostic Index (IPI) in DLBCL, MCL, and FL [53,54,55], or total metabolic/radiographic tumor volume (TMTV/TRTV) from PET/CT scans or MRI [56]. Several research groups have investigated the relationship between pretreatment ctDNA concentrations and conventional markers of tumor burden and its role as a prognostic biomarker in B-cell lymphoma, as summarized in Table 2. In DLBCL, baseline ctDNA levels significantly correlate with IPI, TMTV as well as lactate dehydrogenase (LDH) concentrations and Ann Arbor stage [12, 27, 36, 39, 43, 52, 57, 58]. Importantly, this correlation can be directly translated into a prognostic effect, as pretreatment ctDNA concentrations have shown to be strongly predictive of clinical outcomes in univariate and multivariate analyses in patients receiving standard immunochemotherapy [12, 27, 52, 57, 58]. Furthermore, Frank et al. performed IgHTS on serial plasma samples from 69 patients with relapsed/refractory DLBCL (rrDLBCL) receiving anti-CD19 CAR T-cell therapy and demonstrated that pretreatment ctDNA levels significantly correlate with progression-free survival (PFS) and overall survival (OS) [39].
Similar results have been reported for other lymphomas. For example, both the amount of cfDNA and ctDNA concentrations at baseline assessed by targeted NGS-assays correlated with TMTV, stage, and clinical risk scores such as the International Prognostic Score (IPS) in HL patients [59,60,61]. Desch et al. used a targeted-capture HTS approach that covered 87 distinct genes to profile and quantify ctDNA in pediatric HL [62]. They found significant associations of ctDNA levels with TMTV and bulky disease, while ctDNA did not reflect disease stage in this cohort of patients [62]. In patients with MCL, ctDNA measured by IgHTS accurately mirrored radiographic tumor burden and ctDNA positivity assessed either by IgHTS or targeted-capture HTS was strongly predictive of clinical outcomes [25, 63, 64]. Lymphoma types with an indolent growth pattern such as FL or in lymphomas that are confined to the central nervous system (i.e., PCNSL or isolated secondary CNSL [iSCNSL]), ctDNA levels in blood plasma are substantially lower and ctDNA detection is more challenging [28, 65,66,67]. Here, the association between ctDNA levels and tumor burden or clinical outcomes is not fully established. For example, while previous studies failed to show any correlation in PCNSL [65, 66], Mutter et al. recently demonstrated that ctDNA mirrors MRI tumor volumes and predicts PFS and OS, both in log-rank and cox regression analyses, using PhasED-seq for ctDNA quantification [68]. In FL, three studies targeting either ctDNA clonotypes by IgHTS or assessing cfDNA concentrations by ddPCR revealed significant correlations with baseline TMTV and showed that higher ctDNA/cfDNA levels were associated with shorter PFS [38, 69, 70] (Table 2).
ctDNA-based response assessment during treatment
Treatment responses are highly variable in patients with B-cell lymphomas and accurate prediction of treatment failure or clinical outcomes would substantially improve personalized therapeutic strategies. While interim-PET/CT-guided prognostication and treatment has been implemented in standard clinical care of patients with HL [71], conventional methods for risk stratification and personalized treatment selection are limited in non-Hodgkin lymphomas. For example, the IPI, TMTV measured by PET/CT, or cell of origin (COO) subtypes have largely failed to demonstrate any utility for directing treatment in DLBCL [12, 72,73,74,75,76,77,78,79,80,81]. Therefore, ctDNA assessment at distinct time points during treatment and at the end of therapy might help overcome these limitations and improve patient risk stratification.
Concentrations of ctDNA usually change rapidly during lymphoma treatment. Quantitative response assessment of on-treatment ctDNA has shown to be highly prognostic in various lymphoma entities, as summarized in Table 3. In an early study by Roschewski et al., the authors observed that ctDNA negativity by IgHTS after two cycles of dose-adjusted EPOCH ± rituximab was associated with a favorable five-year PFS in patients with DLBCL [36]. Similarly, another study by Kurtz et al. defined two landmarks for the assessment of ‘molecular response’ during standard immunochemotherapy in DLBCL patients, utilizing serial ctDNA monitoring by CAPP-Seq: a 2-log reduction in ctDNA after 1 cycle of therapy (=early molecular response, EMR) and a 2.5-log reduction in ctDNA after 2 cycles of therapy (=major molecular response, MMR) [21, 27]. Patients achieving EMR and MMR had significantly superior event-free survival (EFS) and OS than patients without a 2- or 2.5-log ctDNA drop, both in frontline and salvage therapeutic settings [27]. However, EMR and MMR still misclassified certain patients at these fixed time points. Thus, the authors developed an approach integrating various prognostic factors measured before and during treatment (i.e., IPI, pretreatment ctDNA, COO, EMR, MMR, and interim PET/CT) into one single algorithm that updates the patient’s risk dynamically over time as more information becomes available (Continuous Individualized Risk Index, CIRI) [82]. This personalized method was applied to an independent validation cohort and outperformed conventional risk factors such as IPI, COO, interim PET/CT, and even EMR and MMR, for outcome prediction [82].
The value of ctDNA for risk assessment in DLBCL was further shown in other therapeutic settings. For example, CAR T-cell therapy has emerged as a novel strategy to treat B-cell lymphomas and has introduced new challenges for risk stratification and response assessment [25]. Two major recent studies evaluated the role of ctDNA in DLBCL patients who were treated with CAR T-cell therapy in more detail. Frank et al. used IgHTS to detect V(D)J clonotypes in the plasma of 72 relapsed/refractory (rr) DLBCL patients undergoing treatment with axicabtagene ciloleucel (axi-cel). They found that 70% of patients responding to CAR T-cell therapy had undetectable ctDNA 7 days after infusion, compared to 13% of progressing patients. At multiple time points after axi-cel infusion (days 21, 28, and 56), ctDNA positivity was predictive of clinical outcomes, both for PFS and OS [39]. In another study, Sworder et al. used CAPP-Seq to profile ctDNA at various landmarks before and after axi-cel therapy. They demonstrated that ctDNA levels were prognostic for PFS in univariate analyses both at diagnosis and at several time points after CAR T-cell infusion [83]. Similarly, Merryman et al. applied IgHTS to 141 patients with rrDLBCL undergoing autologous stem cell transplantation (autoSCT) and found that the identification of ctDNA in apheresis stem cell samples was predictive of PFS and OS [46]. Another study showed that an increase of ctDNA at day 15 of panobinostat treatment in rrDLBCL patients was significantly associated with treatment failure [84].
Beyond DLBCL, studies have demonstrated accurate risk assessment by ctDNA quantification during treatment in various lymphoma types. In PCNSL, ctDNA positivity assessed by PhasED-seq during curative-intent induction therapy strongly predicted clinical outcomes, both PFS and OS [85]. In HL, Spina et al. found that a 2-log reduction of ctDNA after 2 cycles of ABVD was associated with favorable PFS and OS [59]. One other study highlighted that both ctDNA positivity and levels of ctDNA assessed by targeted NGS correlated with PET/CT Deauville scores after 2 cycles of therapy [60]. In a large cohort of pediatric patients with HL, Desch et al. explored whether ctDNA detection during treatment correlated with radiographic response assessment by PET/CT. They found that ctDNA was not detectable in 43 patients (0/43) showing favorable PET results (i.e., qPET <3), while 5 out of 6 patients with unfavorable PET/CT (i.e., qPET >3) were ctDNA-positive [62]. In MCL, patients receiving dose-adjusted R-EPOCH plus bortezomib had favorable clinical outcomes when ctDNA was undetectable by IgHTS after 1 or 2 cycles of therapy or at the end of induction treatment [64]. Similarly, Smith et al. presented data on ctDNA evaluation after 3 cycles of bendamustine-based induction therapy (IgHTS) and observed shorter PFS in MCL patients with positive ctDNA [86] (Table 3).
ctDNA as a biomarker for MRD detection after therapy and during surveillance
After treatment, lymphomas are typically monitored by radiographic imaging, including CT scans or PET/CT. Yet, their utility is controversial due to suboptimal specificity, and serial scans are no longer recommended for routine lymphoma surveillance [87,88,89]. In contrast, ctDNA as a biomarker is usually more disease-specific and allows noninvasive and serial monitoring without radiation exposure. MRD monitoring and lymphoma surveillance after completion of therapy is certainly the most established application of ctDNA. Its prognostic value and the role of ctDNA for relapse prediction/detection have been explored in various publications (Table 4). Three independent studies demonstrated that serial monitoring of DLBCL patients in complete remission (CR) either by IgHTS or CAPP-Seq facilitates the detection of lymphoma recurrence in the vast majority of cases, with a ~3–6 month lead time prior to radiographic imaging [12, 36, 37]. However, Kumar et al. recently reported a moderate ctDNA detection rate of 56% at or before clinical relapse in a prospective multicenter trial assessing the performance of ctDNA monitoring after DLBCL frontline treatment, applying the single gene assay IgHTS [44]. In other therapeutic settings, Frank et al. recently showed robust detection of ctDNA either before or at radiographic relapse in 29 of 30 (94%) DLBCL patients with initial response to CAR T-cell therapy [39]. Merryman et al. demonstrated high ctDNA detection rates by IgHTS in relapsing patients following high-dose chemotherapy and autoSCT [46]. In MCL, IgHTS identified ctDNA during surveillance or at disease progression in 62% of patients, with a median lead time of 7.2 months [64].
Several other studies explored the prognostic value of ctDNA as a landmark after the end of treatment, a situation in which MRD detection is particularly challenging due to soberingly low amounts of ctDNA in blood plasma. In DLBCL, three studies reported favorable clinical outcomes in patients with undetectable ctDNA after completion of therapy using targeted-capture NGS-based technologies [12, 49, 52]. In MCL, Lakhotia et al. showed that ctDNA detection by IgHTS after induction therapy is associated with shorter PFS and OS [64] (Table 4).
Finally, the utility of MRD monitoring in FL through liquid biopsy technologies has been extensively investigated in a plethora of publications. However, data in FL mainly rely on the assessment of CTCs in peripheral blood (PB) and bone marrow (BM), not ctDNA or cfDNA. Therefore, these studies are not covered in this review and we encourage readers to consult other dedicated sources such as Pott et al. [90].
ctDNA for lymphoma diagnosis and noninvasive genotyping
Histopathological assessment of lymphoma tissue obtained from invasive surgical procedures is the gold standard for lymphoma diagnosis, characterization of genetic landscapes, and subtype classification. Yet, noninvasive genotyping by ctDNA profiling from body fluids might represent a complementary tool in certain situations in which tumor tissue is inaccessible or cannot be obtained repeatedly over the course of the disease. The current clinical relevance of noninvasive tumor genotyping by ctDNA is certainly lower than the utility of MRD monitoring and tumor quantification, which are closer to translation. However, noninvasive profiling of tumor genotypes could have important implications as a precision medicine tool in the future, but its potential for clinical translation will largely depend on the development of subtype-specific targeted therapies for treatment selection [91]. For example, FL and DLBCL patients carrying EZH2 mutations identified in lymphoma tissue or ctDNA show a better response to the EZH2 inhibitor tazemetostat than patients with wildtype EZH2 [92, 93]. Furthermore, the identification of co-existing mutations in MYD88 and CD79B might help identify DLBCL patients who are most likely to respond to the BTK inhibitor ibrutinib [94]. Similarly, mutations in MYD88, CCND1 or in genes involved in the NFκB pathway appear to be associated with resistance to ibrutinib in MCL [24, 95]. Here, noninvasive genotyping from ctDNA might help guiding treatment decisions in a subset of cases where tumor tissue is unavailable.
A basic requirement of tumor-agnostic noninvasive genotyping is that liquid biopsy robustly mirrors tumor mutational patterns. Numerous studies have shown that the concordance between tissue-based and ctDNA-based genotyping is usually greater than 70%, even if the tumor cell content is exceptionally low like in HL (0.1–3%) [12, 41, 57, 59,60,61,62]. In general, mutation detection rates from tumors are higher than from plasma specimens due to the larger tumor content. However, mutations present in plasma but not in tumor tissue are frequently observed, indicating that ctDNA profiling can capture variants that are missed by single-site tumor biopsies (i.e., spatial heterogeneity) [12, 41, 57, 59]. For example, plasma genotyping by targeted NGS identified mutations in CARD11 and PIM1 genes in a patient diagnosed with FL that were not detected in a diagnostic inguinal lymph node biopsy. Yet, these mutations were shared between plasma and the patient’s transformed FL biopsy of a retroperitoneal mass 9 months later at disease progression, indicating that both indolent and aggressive clones were already present before histological transformation (HT) [12]. Other publications demonstrated simultaneous capturing of two EZH2-mutated clones in plasma by ddPCR that originate from two distinct tumor locations of a patient with FL, or the occurrence of XPO1 mutations in 29% of HL patients who did not show any XPO1 aberrations in tumor biopsies [96, 97]. Camus et al. provide additional evidence that genetic profiling from ctDNA in HL patients could have some decisive advantages over tumor genotyping due to low tumor cell content in this disease. They found that 52% of all mutations detected in 42 HL patients at diagnosis were exclusively present in plasma but not in corresponding tumor specimens [61].
Tumor biopsies can be particularly challenging in patients with central nervous system lymphoma (CNSL). Here, stereotactic serial biopsies are the gold standard to obtain brain tumor material for subsequent histopathological evaluation. However, invasive neurosurgical biopsies can be inconclusive or delayed due to concurrent steroid treatment and carry procedural risks, especially in patients with deep brainlesions [98,99,100,101,102]. Therefore, non- or minimal-invasive ctDNA profiling from plasma or CSF seems desirable in this group of patients, especially because flow cytometry and cytopathology from CSF are insensitive and require large sample volumes [103]. Several studies demonstrated moderate to high detection rates of ctDNA in CSF or plasma of PCNSL patients by utilizing either PCR-based methods for MYD88L265P detection or broader NGS-based technologies, suggesting that a subset of patients with suspected brain lymphoma might be able to forego invasive surgical procedures [20, 68, 104,105,106,107,108,109,110]. Another major clinical challenge is the occurrence of CNS relapses in DLBCL patients and the inability to detect occult CNS involvement by conventional CSF flow cytometry and cytopathology. Olszewski et al. were able to detect ctDNA in CSF by IgHTS in 8 out of 19 (42%) DLBCL patients with high risk of CNS involvement but no overt CNS disease. Importantly, no patients with negative ctDNA but 29% with detectable ctDNA developed CNS relapse one year after DLBCL diagnosis [111].
Intravascular large B-cell lymphoma (IVLBCL) is another rare DLBCL subtype characterized by lymphoma cells infiltrating blood vessels but no obvious tumor mass, making conventional diagnosis by imaging or tissue biopsies extremely challenging [5, 24, 112]. Interestingly, variant allele frequencies and the number of identified mutations seem to be higher in ctDNA compared to biopsy-derived DNA in this disease [113]. Shimada et al. applied whole exome sequencing (WES) to comprehensively profile ctDNA in 18 IVLBCL patients. They found an enrichment of mutations associated with ABC-DLBCL (i.e., mutations in MYD88 and CD79B) and frequent rearrangements involving programmed cell death ligands 1 and 2 (PD-L1/PD-L2) [114].
ctDNA for assessment of tumor heterogeneity
In DLBCL, mutational landscapes are highly heterogenous and allow classification of patients into subgroups that have significant implications for clinical outcomes [3, 6]. DLBCL tumors can further be classified according to their transcriptionally distinct B-cell differentiation state (COO: germinal center B cell-like (GCB) and activated B cell-like (ABC) DLBCL [1, 115,116,117,118]. Technologies used to evaluate COO from tumor tissue such as the gold standard gene-expression profiling (GEP) or immunohistochemistry algorithms are either unavailable in clinical routine or limited due to suboptimal classification performance [2]. Previous reports have shown that noninvasive classification of DLBCL tumors according to their COO phenotypes is feasible, either based on the mutational landscape of ctDNA or fragmentation patterns of cfDNA [12, 119]. The latter approach uses promotor fragmentation entropy and targeted deep sequencing of transcription start sites to infer expression of genes of interest and classify histological and molecular subtypes in DLBCL [119, 120].
The mutational landscapes of relapsed lymphomas are often substantially different from diagnostic tumor specimens [8, 121]. While serial tissue biopsies at lymphoma relapse are often not performed, ctDNA genotyping might add important information on molecular tumor heterogeneity over time. Indeed, three previous studies demonstrated clonal divergence between the diagnostic tumor specimen and plasma ctDNA at lymphoma relapse in DLBCL, FL, and HL patients using targeted-capture NGS [12, 41, 59]. Interestingly, while genomic divergence was relatively moderate in rrDLBCL and FL, the greatest molecular distance was observed in FL patients undergoing histological transformation (tFL), reflecting the biological shift from an indolent to an aggressive behavior [12]. Histological transformation of indolent lymphoma entities to aggressive lymphomas occurs at a rate of 2–3% per year and is associated with an unfavorable prognosis [122, 123]. Tumor biopsies at transformation are often not performed or fail to detect the transformed tumor site [25, 124]. By incorporating the magnitude of the genomic distance and the amount of ctDNA in plasma within a mathematical model, HT could be predicted noninvasively by CAPP-Seq prior to clinical detection with high sensitivity and specificity [12, 28].
In many cases, the emergence of novel subclones over time reflects a process of clonal selection under treatment pressure, especially with targeted agents. Various studies revealed that molecular mechanisms of resistance in lymphoma can be captured noninvasively by ctDNA profiling. For example, Agarwal et al. demonstrated robust detection of emerging resistance alterations in blood plasma of MCL patients receiving ibrutinib plus venetoclax within a phase II clinical trial, using a targeted amplicon-based NGS sequencing panel (42 genes) and low-coverage WGS. Among these acquired genetic events were the loss of chromosome 9p21.1-p23.4 and mutations in components of the SWI-SNF chromatin-remodeling complex [63, 125]. Other studies in DLBCL demonstrated the emergence of resistance mutations by serial ctDNA genotyping using targeted NGS panels, including novel BTKC481S resistance mutations in patients receiving ibrutinib monotherapy. [12, 41, 52, 126]. Most recently, Sworder et al. observed the emergence of mutations in CD19, PAX5, and TP53 following DLBCL relapse after CAR T-cell therapy, representing candidate resistance mechanisms to this novel therapeutic approach [83]. Finally, Spina et al. systematically explored mutational evolution patterns in serial ctDNA samples from 13 HL patients with lymphoma relapse following ABVD frontline therapy or salvage treatment. While they found that ancestral mutations mostly persist over time, all cases demonstrated clonal shifts with novel mutations detected in plasma at lymphoma recurrence such as PIM1, IRF8, or TNFAIP3 [59].
Future directions and conclusions
Circulating tumor DNA has emerged as an attractive biomarker in B-cell lymphomas with various potential clinical applications. Yet, there are multiple aspects and dimensions of ctDNA analyses, each of which revealing different facets of a patient’s lymphoma. The value of ctDNA for tumor quantification, MRD monitoring, and risk stratification has been extensively explored over recent years, in part due to tremendous advances of innovative technologies that facilitate ultrasensitive ctDNA detection. Thus, this application can be considered closest to translation, with prospective clinical trials warranted to investigate whether early ctDNA profiling on-treatment or MRD monitoring during surveillance in lymphoma lead to improved outcomes and toxicity profiles. For example, patients who show insufficient molecular response based on ctDNA quantification could benefit from alternative therapeutic strategies, ideally at a time point where disease burden is lowest to increase the efficacy of salvage regimens or novel strategies such as CAR T-cell therapy [127,128,129]. On the other hand, patients with favorable ctDNA responses might do just as well with reduced cycles of chemotherapy or less toxic agents. In general, ctDNA has the potential to serve as a novel surrogate endpoint to help accelerate and improve clinical trial designs and drug development.
Other aspects of ctDNA in lymphoma such as noninvasive tumor genotyping, characterizing tumor heterogeneity or fragmentation patterns are more exploratory but are increasingly relevant for addressing important translational research questions and could be leveraged to overcome limitations of tissue biopsies. For example, serial assessment of ctDNA could enhance our understanding of molecular factors underlying clonal evolution and treatment resistance in lymphoma, particularly in lymphoma types where tumors are largely inaccessible such as CNS lymphomas. Noninvasive detection of resistance mechanisms might also facilitate treatment modifications right before patients undergo clinically overt lymphoma progression. Furthermore, cfDNA fragmentation patterns or methylation features could have potential utility for lymphoma classification and characterizing molecular and histological subtypes, augmenting standard pathological procedures.
However, the lack of standardization and harmonization of liquid biopsy technologies between laboratories currently hamper the broad implementation of ctDNA profiling across countries and in multicenter clinical trials. Yet, several initiatives were launched to define standards for pre-analytical handling, panel design, assay performance, and bioinformatics, including the ‘ctDNA working group meeting at the ASH Annual Meeting’ and the ‘15-ICML workshop on ctDNA’ in 2019 [29].
Ultimately, with the combination of recent major technical advances allowing the detection of vanishing amounts of ctDNA and novel machine learning approaches that facilitate intelligent implementation of the various dimensions of ctDNA as an analyte, we envision the prospective evaluation of the clinical value of ctDNA for lymphoma genotyping, risk stratification, and MRD monitoring in the near future.
References
Alizadeh AA, Eisen MB, Davis RE, Ma C, Lossos IS, Rosenwald A, et al. Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature. 2000;403:503–11.
Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103:275–82.
Schmitz R, Wright GW, Huang DW, Johnson CA, Phelan JD, Wang JQ, et al. Genetics and pathogenesis of diffuse large B-cell lymphoma. N Engl J Med. 2018;378:1396–407.
Cheson BD, Nowakowski G, Salles G. Diffuse large B-cell lymphoma: new targets and novel therapies. Blood Cancer J. 2021;11:68.
Poynton E, Okosun J. Liquid biopsy in lymphoma: Is it primed for clinical translation? eJHaem. 2021;2:3.
Chapuy B, Stewart C, Dunford AJ, Kim J, Kamburov A, Redd RA, et al. Molecular subtypes of diffuse large B cell lymphoma are associated with distinct pathogenic mechanisms and outcomes. Nat Med. 2018;24:679–90.
Kridel R, Chan FC, Mottok A, Boyle M, Farinha P, Tan K, et al. Histological transformation and progression in follicular lymphoma: a Clonal Evolution Study. PLoS Med. 2016;13:e1002197.
Green MR, Kihira S, Liu CL, Nair RV, Salari R, Gentles AJ, et al. Mutations in early follicular lymphoma progenitors are associated with suppressed antigen presentation. Proc Natl Acad Sci USA. 2015;112:E1116–25.
Wu C, de Miranda NF, Chen L, Wasik AM, Mansouri L, Jurczak W, et al. Genetic heterogeneity in primary and relapsed mantle cell lymphomas: Impact of recurrent CARD11 mutations. Oncotarget. 2016;7:38180–90.
Melchardt T, Hufnagl C, Weinstock DM, Kopp N, Neureiter D, Tränkenschuh W, et al. Clonal evolution in relapsed and refractory diffuse large B-cell lymphoma is characterized by high dynamics of subclones. Oncotarget. 2016;7:51494–502.
Scherer F. Capturing tumor heterogeneity and clonal evolution by circulating tumor DNA profiling. Recent Results Cancer Res. 2020;215:213–30.
Scherer F, Kurtz DM, Newman AM, Stehr H, Craig AF, Esfahani MS, et al. Distinct biological subtypes and patterns of genome evolution in lymphoma revealed by circulating tumor DNA. Sci Transl Med. 2016;8:364ra155.
Dudley JC, Schroers-Martin J, Lazzareschi DV, Shi WY, Chen SB, Esfahani MS, et al. Detection and surveillance of bladder cancer using urine tumor DNA. Cancer Discov. 2019;9:500–9.
Nuzzo PV, Berchuck JE, Korthauer K, Spisak S, Nassar AH, Abou Alaiwi S, et al. Detection of renal cell carcinoma using plasma and urine cell-free DNA methylomes. Nat Med. 2020;26:1041–3.
Wehrle J, Philipp U, Jolic M, Follo M, Hussung S, Waldeck S, et al. Personalized treatment selection and disease monitoring using circulating tumor DNA profiling in real-world cancer patient management. Diagnostics. 2020;10:550.
Smith CG, Moser T, Mouliere F, Field-Rayner J, Eldridge M, Riediger AL, et al. Comprehensive characterization of cell-free tumor DNA in plasma and urine of patients with renal tumors. Genome Med. 2020;12:23.
Eckmann JD, Ebner DW, Kisiel JB. Multi-target stool DNA testing for colorectal cancer screening: emerging learning on real-world performance. Curr Treat Options Gastroenterol. 2020;18:109–119.
Wang Y, Springer S, Mulvey CL, Silliman N, Schaefer J, Sausen M, et al. Detection of somatic mutations and HPV in the saliva and plasma of patients with head and neck squamous cell carcinomas. Sci Transl Med. 2015;7:293ra104.
Baburaj G, Damerla RR, Udupa KS, Parida P, Munisamy M, Kolesar J, et al. Liquid biopsy approaches for pleural effusion in lung cancer patients. Mol Biol Rep. 2020;47:8179–87.
Baraniskin A, Schroers R. Liquid biopsy and other non-invasive diagnostic measures in PCNSL. Cancers. 2021;13.
Cirillo M, Craig AFM, Borchmann S, Kurtz DM. Liquid biopsy in lymphoma: molecular methods and clinical applications. Cancer Treat Rev. 2020;91:102106.
Wan JCM, Massie C, Garcia-Corbacho J, Mouliere F, Brenton JD, Caldas C, et al. Liquid biopsies come of age: towards implementation of circulating tumour DNA. Nat Rev Cancer. 2017;17:223–38.
Melani C, Wilson WH, Roschewski M. Liquid biopsy in non-Hodgkin’s lymphoma. Hematol Oncol. 2019;37 Suppl 1:70–4.
Huet S, Salles G. Potential of circulating tumor DNA for the management of patients with lymphoma. JCO Oncol Pract. 2020;16:561–8.
Lakhotia R, Roschewski M. Circulating tumour DNA in B-cell lymphomas: current state and future prospects. Br J Haematol. 2021;193:867–81.
Newman AM, Lovejoy AF, Klass DM, Kurtz DM, Chabon JJ, Scherer F, et al. Integrated digital error suppression for improved detection of circulating tumor DNA. Nat Biotechnol. 2016;34:547–55.
Kurtz DM, Scherer F, Jin MC, Soo J, Craig AFM, Esfahani MS, et al. Circulating tumor DNA measurements as early outcome predictors in diffuse large B-cell lymphoma. J Clin Oncol. 2018;36:2845–53.
Schroers-Martin JG, Kurtz DM, Soo J, Jin M, Scherer F, Craig A, et al. Determinants of circulating tumor DNA levels across lymphoma histologic subtypes. Blood. 2017;130:4018.
Rossi D, Kurtz DM, Roschewski M, Cavalli F, Zucca E, Wilson WH. The development of liquid biopsy for research and clinical practice in lymphomas: report of the 15-ICML workshop on ctDNA. Hematol Oncol. 2020;38:34–7.
Parackal S, Zou D, Day R, Black M, Guilford P. Comparison of Roche cell-free DNA collection tubes. Pract Lab Med. 2019;16:e00125.
Razavi P, Li BT, Brown DN, Jung B, Hubbell E, Shen R, et al. High-intensity sequencing reveals the sources of plasma circulating cell-free DNA variants. Nat Med. 2019;25:1928–37.
Chabon JJ, Hamilton EG, Kurtz DM, Esfahani MS, Moding EJ, Stehr H, et al. Integrating genomic features for non-invasive early lung cancer detection. Nature. 2020;580:245–51.
Genovese G, Kähler AK, Handsaker RE, Lindberg J, Rose SA, Bakhoum SF, et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N Engl J Med. 2014;371:2477–87.
Jaiswal S, Fontanillas P, Flannick J, Manning A, Grauman PV, Mar BG, et al. Age-related clonal hematopoiesis associated with adverse outcomes. N Engl J Med. 2014;371:2488–98.
Scherer F, Kurtz DM, Diehn M, Alizadeh AA. High-throughput sequencing for noninvasive disease detection in hematologic malignancies. Blood. 2017;130:440–52.
Roschewski M, Dunleavy K, Pittaluga S, Moorhead M, Pepin F, Kong K, et al. Circulating tumour DNA and CT monitoring in patients with untreated diffuse large B-cell lymphoma: a correlative biomarker study. Lancet Oncol. 2015;16:541–9.
Kurtz DM, Green MR, Bratman SV, Scherer F, Liu CL, Kunder CA, et al. Noninvasive monitoring of diffuse large B-cell lymphoma by immunoglobulin high-throughput sequencing. Blood. 2015;125:3679–87.
Sarkozy C, Huet S, Carlton VE, Fabiani B, Delmer A, Jardin F, et al. The prognostic value of clonal heterogeneity and quantitative assessment of plasma circulating clonal IG-VDJ sequences at diagnosis in patients with follicular lymphoma. Oncotarget. 2017;8:8765–74.
Frank MJ, Hossain NM, Bukhari A, Dean E, Spiegel JY, Claire GK, et al. Monitoring of circulating tumor DNA improves early relapse detection after axicabtagene ciloleucel infusion in large B-Cell lymphoma: results of a prospective multi-institutional trial. J Clin Oncol. 2021;39:27.
Pott C, Sehn LH, Belada D, Gribben J, Hoster E, Kahl B, et al. MRD response in relapsed/refractory FL after obinutuzumab plus bendamustine or bendamustine alone in the GADOLIN trial. Leukemia. 2020;34:522–32.
Rossi D, Diop F, Spaccarotella E, Monti S, Zanni M, Rasi S, et al. Diffuse large B-cell lymphoma genotyping on the liquid biopsy. Blood. 2017;129:1947–57.
Newman AM, Bratman SV, To J, Wynne JF, Eclov NC, Modlin LA, et al. An ultrasensitive method for quantitating circulating tumor DNA with broad patient coverage. Nat Med. 2014;20:548–54.
Bohers E, Viailly PJ, Becker S, Marchand V, Ruminy P, Maingonnat C, et al. Non-invasive monitoring of diffuse large B-cell lymphoma by cell-free DNA high-throughput targeted sequencing: analysis of a prospective cohort Blood Cancer J. 2018;8:74.
Kumar A, Westin J, Schuster SJ, Nowakowski GS, Lossos IS, Batlevi CL, et al. Interim analysis from a prospective multicenter study of next-generation sequencing minimal residual disease assessment and CT monitoring for surveillance after frontline treatment in diffuse large B-cell lymphoma. Blood. 2020:136–S1.
Kurtz DM, Chabon JJ, Soo J, Co Ting Keh L, Alig S, Schultz A, et al. Phased variants improve DLBCL minimal residual disease detection at the end of therapy. Hematol Oncol. 2021;39:1537–1547.
Merryman RW, Redd RA, Taranto E, Ahmed G, Jeter E, McHugh KM, et al. Prognostic value of circulating tumor DNA (ctDNA) in autologous stem cell graft and post-transplant plasma samples among patients with diffuse large B-cell lymphoma. Blood. 2020;136:22–23.
Schmitt MW, Kennedy SR, Salk JJ, Fox EJ, Hiatt JB, Loeb LA. Detection of ultra-rare mutations by next-generation sequencing. Proc Natl Acad Sci USA. 2012;109:14508–13.
Kennedy SR, Schmitt MW, Fox EJ, Kohrn BF, Salk JJ, Ahn EH, et al. Detecting ultralow-frequency mutations by duplex sequencing. Nat Protoc. 2014;9:2586–606.
Kurtz DM, Soo J, Co Ting Keh L, Alig S, Chabon JJ, Sworder BJ, et al. Enhanced detection of minimal residual disease by targeted sequencing of phased variants in circulating tumor DNA. Nat Biotechnol. 2021;39:1537–1547.
Pasqualucci L, Neumeister P, Goossens T, Nanjangud G, Chaganti RS, Küppers R, et al. Hypermutation of multiple proto-oncogenes in B-cell diffuse large-cell lymphomas. Nature. 2001;412:341–6.
Scherer F, Navarrete MA, Bertinetti-Lapatki C, Boehm J, Schmitt-Graeff A, Veelken H. Isotype-switched follicular lymphoma displays dissociation between activation-induced cytidine deaminase expression and somatic hypermutation. Leuk Lymphoma. 2016;57:151–60.
Meriranta L, Alkodsi A, Pasanen A, Lepistö M, Mapar P, Blaker YN, et al. Molecular features encoded in the ctDNA reveal heterogeneity and predict outcome in high-risk aggressive B-cell lymphoma. Blood. 2022;139:1863–77.
Project IN-HsLPF. A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med. 1993;329:987–94.
Hoster E, Dreyling M, Klapper W, Gisselbrecht C, van Hoof A, Kluin-Nelemans HC, et al. A new prognostic index (MIPI) for patients with advanced-stage mantle cell lymphoma. Blood. 2008;111:558–65.
Solal-Céligny P, Roy P, Colombat P, White J, Armitage JO, Arranz-Saez R, et al. Follicular lymphoma international prognostic index. Blood. 2004;104:1258–65.
Sasanelli M, Meignan M, Haioun C, Berriolo-Riedinger A, Casasnovas RO, Biggi A, et al. Pretherapy metabolic tumour volume is an independent predictor of outcome in patients with diffuse large B-cell lymphoma. Eur J Nucl Med Mol Imaging. 2014;41:2017–22.
Rivas-Delgado A, Nadeu F, Enjuanes A, Casanueva-Eliceiry S, Mozas P, Magnano L, et al. Mutational landscape and tumor burden assessed by cell-free DNA in diffuse large B-cell lymphoma in a population-based study. Clin Cancer Res. 2021;27:513–21.
Alig S, Macaulay CW, Kurtz DM, Dührsen U, Hüttmann A, Schmitz C, et al. Short diagnosis-to-treatment interval is associated with higher circulating tumor DNA levels in diffuse large B-cell lymphoma. J Clin Oncol. 2021;39:2605–16.
Spina V, Bruscaggin A, Cuccaro A, Martini M, Di Trani M, Forestieri G, et al. Circulating tumor DNA reveals genetics, clonal evolution, and residual disease in classical Hodgkin lymphoma. Blood. 2018;131:2413–25.
Sobesky S, Mammadova L, Cirillo M, Drees E, Mattlener J, Dörr H, et al. Exhaustive circulating tumor DNA sequencing reveals the genomic landscape of Hodgkin lymphoma and facilitates ultrasensitive detection of minimal residual disease. 2021. https://www.medrxiv.org/content/10.1101/2021.03.16.21253679v1.
Camus V, Viennot M, Lequesne J, Viailly PJ, Bohers E, Bessi L, et al. Targeted genotyping of circulating tumor DNA for classical Hodgkin lymphoma monitoring: a prospective study. Haematologica. 2021;106:154–62.
Desch AK, Hartung K, Botzen A, Brobeil A, Rummel M, Kurch L, et al. Genotyping circulating tumor DNA of pediatric Hodgkin lymphoma. Leukemia. 2020;34:151–66.
Agarwal R, Chan YC, Tam CS, Hunter T, Vassiliadis D, Teh CE, et al. Dynamic molecular monitoring reveals that SWI-SNF mutations mediate resistance to ibrutinib plus venetoclax in mantle cell lymphoma. Nat Med. 2019;25:119–29.
Lakhotia R, Melani C, Dunleavy K, Pittaluga S, Saba NS, Lindenberg L, et al. Circulating tumor DNA predicts therapeutic outcome in mantle cell lymphoma. Blood Adv. 2022;6:2667–2680.
Fontanilles M, Marguet F, Bohers É, Viailly PJ, Dubois S, Bertrand P, et al. Non-invasive detection of somatic mutations using next-generation sequencing in primary central nervous system lymphoma. Oncotarget. 2017;8:48157–68.
Hattori K, Sakata-Yanagimoto M, Suehara Y, Yokoyama Y, Kato T, Kurita N, et al. Clinical significance of disease-specific MYD88 mutations in circulating DNA in primary central nervous system lymphoma. Cancer Sci. 2018;109:225–30.
Hickmann AK, Frick M, Hadaschik D, Battke F, Bittl M, Ganslandt O, et al. Molecular tumor analysis and liquid biopsy: a feasibility investigation analyzing circulating tumor DNA in patients with central nervous system lymphomas. BMC Cancer. 2019;19:192.
Mutter JA, Alig S, Lauer EM, Esfahani MS, Mitschke J, Kurtz DM, et al. Profiling of circulating tumor DNA for noninvasive disease detection, risk stratification, and MRD monitoring in patients with CNS lymphoma. Blood. 2021;138:6.
Delfau-Larue MH, van der Gucht A, Dupuis J, Jais JP, Nel I, Beldi-Ferchiou A, et al. Total metabolic tumor volume, circulating tumor cells, cell-free DNA: distinct prognostic value in follicular lymphoma. Blood Adv. 2018;2:807–16.
Distler A, Lakhotia R, Phelan JD, Pittaluga S, Melani C, Muppidi JR, et al. A prospective study of clonal evolution in follicular lymphoma: circulating tumor DNA correlates with overall tumor burden and fluctuates over time without therapy. Blood. 2021;138:1328.
Trotman J, Barrington SF. The role of PET in first-line treatment of Hodgkin lymphoma. Lancet Haematol. 2021;8:e67–e79.
Casasnovas RO, Ysebaert L, Thieblemont C, Bachy E, Feugier P, Delmer A, et al. FDG-PET-driven consolidation strategy in diffuse large B-cell lymphoma: final results of a randomized phase 2 study. Blood. 2017;130:1315–26.
Chiappella A, Martelli M, Angelucci E, Brusamolino E, Evangelista A, Carella AM, et al. Rituximab-dose-dense chemotherapy with or without high-dose chemotherapy plus autologous stem-cell transplantation in high-risk diffuse large B-cell lymphoma (DLCL04): final results of a multicentre, open-label, randomised, controlled, phase 3 study. Lancet Oncol. 2017;18:1076–88.
Dührsen U, Müller S, Hertenstein B, Thomssen H, Kotzerke J, Mesters R, et al. Positron emission tomography-guided therapy of aggressive non-Hodgkin lymphomas (PETAL): a multicenter, randomized phase III trial. J Clin Oncol. 2018;36:2024–34.
Hertzberg M, Gandhi MK, Trotman J, Butcher B, Taper J, Johnston A, et al. Early treatment intensification with R-ICE and 90Y-ibritumomab tiuxetan (Zevalin)-BEAM stem cell transplantation in patients with high-risk diffuse large B-cell lymphoma patients and positive interim PET after 4 cycles of R-CHOP-14. Haematologica. 2017;102:356–63.
Leonard JP, Kolibaba KS, Reeves JA, Tulpule A, Flinn IW, Kolevska T, et al. Randomized Phase II study of R-CHOP with or without bortezomib in previously untreated patients with non-germinal center B-cell-like diffuse large B-cell lymphoma. J Clin Oncol. 2017;35:3538–46.
Moskowitz CH, Schöder H, Teruya-Feldstein J, Sima C, Iasonos A, Portlock CS, et al. Risk-adapted dose-dense immunochemotherapy determined by interim FDG-PET in advanced-stage diffuse large B-Cell lymphoma. J Clin Oncol. 2010;28:1896–903.
Nowakowski GS, Chiappella A, Gascoyne RD, Scott DW, Zhang Q, Jurczak W, et al. ROBUST: a phase III study of lenalidomide plus R-CHOP versus placebo plus R-CHOP in previously untreated patients with ABC-type diffuse large B-cell lymphoma. J Clin Oncol. 2021;39:1317–28.
Stiff PJ, Unger JM, Cook JR, Constine LS, Couban S, Stewart DA, et al. Autologous transplantation as consolidation for aggressive non-Hodgkin’s lymphoma. N. Engl J Med. 2013;369:1681–90.
Swinnen LJ, Li H, Quon A, Gascoyne R, Hong F, Ranheim EA, et al. Response-adapted therapy for aggressive non-Hodgkin’s lymphomas based on early [18F] FDG-PET scanning: ECOG-ACRIN Cancer Research Group study (E3404). Br J Haematol. 2015;170:56–65.
Younes A, Sehn LH, Johnson P, Zinzani PL, Hong X, Zhu J, et al. Randomized phase III trial of ibrutinib and rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone in non-germinal center B-cell diffuse large B-cell lymphoma. J Clin Oncol. 2019;37:1285–95.
Kurtz DM, Esfahani MS, Scherer F, Soo J, Jin MC, Liu CL, et al. Dynamic risk profiling using serial tumor biomarkers for personalized outcome prediction. Cell. 2019;178:699–713 e19.
Sworder B, Kurtz DM, Alig S, Frank MJ, Macauley CW, Garofalo A, et al. Determinants of resistance to engineered T-cell therapies targeting CD19 in lymphoma. Hematol Oncol. 2021;39.
Assouline SE, Nielsen TH, Yu S, Alcaide M, Chong L, MacDonald D, et al. Phase 2 study of panobinostat with or without rituximab in relapsed diffuse large B-cell lymphoma. Blood. 2016;128:185–94.
Mutter JA, Alig S, Lauer EM, Esfahani MS, Mitschke J, Kurtz DM, et al. Noninvasive detection, classification, and risk stratification of primary CNS lymphomas by ctDNA profiling. Hematol Oncol. 2021;39.
Smith M, Jegede O, Parekh S, Hanson CA, Martin P, Till BG, et al. Minimal Residual Disease (MRD) assessment in the ECOG1411 randomized phase 2 trial of front-line bendamustine-rituximab (BR)-based induction followed by rituximab (R) ± lenalidomide (L) consolidation for mantle cell lymphoma (MCL). Blood. 2019;134:751.
Moskowitz CH. Interim PET-CT in the management of diffuse large B-cell lymphoma. Hematol Am Soc Hematol Educ Program. 2012;2012:397–401.
Thompson CA, Ghesquieres H, Maurer MJ, Cerhan JR, Biron P, Ansell SM, et al. Utility of routine post-therapy surveillance imaging in diffuse large B-cell lymphoma. J Clin Oncol. 2014;32:3506–12.
Huntington SF, Svoboda J, Doshi JA. Cost-effectiveness analysis of routine surveillance imaging of patients with diffuse large B-cell lymphoma in first remission. J Clin Oncol. 2015;33:1467–74.
Pott C, Wellnitz D, Ladetto M. Minimal residual disease in follicular lymphoma. Ann Lymphoma. 2021;5:32.
Kurtz DM. The many facets of liquid biopsies in lymphoma. Blood. 2022;139:1780–1.
Daigle S, McDonald AA, Morschhauser F, Salles G, Ribrag V, McKay P, et al. Discovery of candidate predictors of response to tazemetostat in diffuse large B-cell lymphoma and follicular lymphoma using NGS technology on ctDNA samples collected pre-treatment. Blood. 2017;130:4013.
Morschhauser F, Tilly H, Chaidos A, McKay P, Phillips T, Assouline S, et al. Tazemetostat for patients with relapsed or refractory follicular lymphoma: an open-label, single-arm, multicentre, phase 2 trial. Lancet Oncol. 2020;21:1433–42.
Wilson WH, Young RM, Schmitz R, Yang Y, Pittaluga S, Wright G, et al. Targeting B cell receptor signaling with ibrutinib in diffuse large B cell lymphoma. Nat Med. 2015;21:922–6.
Hershkovitz-Rokah O, Pulver D, Lenz G, Shpilberg O. Ibrutinib resistance in mantle cell lymphoma: clinical, molecular and treatment aspects. Br J Haematol. 2018;181:306–19.
Nagy Á, Bátai B, Balogh A, Illés S, Mikala G, Nagy N, et al. Quantitative analysis and monitoring of EZH2 Mutations Using Liquid Biopsy in Follicular Lymphoma. Genes. 2020;11:785.
Camus V, Stamatoullas A, Mareschal S, Viailly PJ, Sarafan-Vasseur N, Bohers E, et al. Detection and prognostic value of recurrent exportin 1 mutations in tumor and cell-free circulating DNA of patients with classical Hodgkin lymphoma. Haematologica. 2016;101:1094–101.
Manoj N, Arivazhagan A, Bhat DI, Arvinda HR, Mahadevan A, Santosh V, et al. Stereotactic biopsy of brainstem lesions: Techniques, efficacy, safety, and disease variation between adults and children:a single institutional series and review. J Neurosci Rural Pract. 2014;5:32–9.
Ferreira MP, Ferreira NP, Pereira Filho AEA, Pereira Filho GEA, Franciscatto AC. Stereotactic computed tomography-guided brain biopsy: diagnostic yield based on a series of 170 patients. Surg Neurol. 2006;65 Suppl 1:S1:27–1:32.
Malone H, Yang J, Hershman DL, Wright JD, Bruce JN, Neugut AI. Complications Following Stereotactic Needle Biopsy of Intracranial Tumors. World Neurosurg. 2015;84:1084–9.
Jain D, Sharma MC, Sarkar C, Deb P, Gupta D, Mahapatra AK. Correlation of diagnostic yield of stereotactic brain biopsy with number of biopsy bits and site of the lesion. Brain Tumor Pathol. 2006;23:71–5.
Önder E, Arıkök AT, Önder S, Han Ü, Sorar M, Kertmen H, et al. Corticosteroid pre-treated primary CNS lymphoma: a detailed analysis of stereotactic biopsy findings and consideration of interobserver variability. Int J Clin Exp Pathol. 2015;8:7798–808.
Pittman M, Treese S, Chen L, Frater JL, Nguyen TT, Hassan A, et al. Utility of flow cytometry of cerebrospinal fluid as a screening tool in the diagnosis of central nervous system lymphoma. Arch Pathol Lab Med. 2013;137:1610–8.
Watanabe J, Natsumeda M, Kanemaru Y, Okada M, Oishi M, Kakita A, et al. Comparison of circulating tumor DNA between body fluids in patients with primary central nervous system lymphoma. Leuk Lymphoma. 2019;60:3587–9.
Bobillo S, Crespo M, Escudero L, Mayor R, Raheja P, Carpio C, et al. Cell free circulating tumor DNA in cerebrospinal fluid detects and monitors central nervous system involvement of B-cell lymphomas. Haematologica. 2021;106:513–21.
Hiemcke-Jiwa LS, Minnema MC, Radersma-van Loon JH, Jiwa NM, de Boer M, Leguit RJ. et al. The use of droplet digital PCR in liquid biopsies:a highly sensitive technique for MYD88 p.(L265P) detection in cerebrospinal fluid. Hematol Oncol. 2018;36:429–35.
Hiemcke-Jiwa LS, Leguit RJ, Snijders TJ, Bromberg JEC, Nierkens S, Jiwa NM, et al. MYD88 p.(L265P) detection on cell-free DNA in liquid biopsies of patients with primary central nervous system lymphoma. Br J Haematol. 2019;185:974–7.
Grommes C, Tang SS, Wolfe J, Kaley TJ, Daras M, Pentsova EI, et al. Phase 1b trial of an ibrutinib-based combination therapy in recurrent/refractory CNS lymphoma. Blood. 2019;133:436–45.
Gupta M, Burns E, Georgantas NZ, Thierauf J, Nayyar N, Gordon A, et al. A rapid genotyping panel for detection of primary central nervous system lymphoma. Blood. 2021;138:382–386.
Ferreri AJM, Calimeri T, Lopedote P, Francaviglia I, Daverio R, Iacona C, et al. MYD88 L265P mutation and interleukin-10 detection in cerebrospinal fluid are highly specific discriminating markers in patients with primary central nervous system lymphoma: results from a prospective study. Br J Haematol. 2021;193:497–505.
Olszewski AJ, Chorzalska AD, Petersen M, Ollila TA, Zayac A, Kurt H, et al. Detection of clonotypic DNA in the cerebrospinal fluid as a marker of central nervous system invasion in lymphoma. Blood Adv. 2021;5:5525–35.
Ponzoni M, Ferreri AJ, Campo E, Facchetti F, Mazzucchelli L, Yoshino T, et al. Definition, diagnosis, and management of intravascular large B-cell lymphoma: proposals and perspectives from an international consensus meeting. J Clin Oncol. 2007;25:3168–73.
Suehara Y, Sakata-Yanagimoto M, Hattori K, Nanmoku T, Itoh T, Kaji D, et al. Liquid biopsy for the identification of intravascular large B-cell lymphoma. Haematologica. 2018;103:e241–e4.
Shimada K, Yoshida K, Suzuki Y, Iriyama C, Inoue Y, Sanada M, et al. Frequent genetic alterations in immune checkpoint-related genes in intravascular large B-cell lymphoma. Blood. 2021;137:1491–502.
Lenz G, Wright G, Dave SS, Xiao W, Powell J, Zhao H, et al. Stromal gene signatures in large-B-cell lymphomas. N Engl J Med. 2008;359:2313–23.
Rosenwald A, Wright G, Chan WC, Connors JM, Campo E, Fisher RI, et al. The use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. N Engl J Med. 2002;346:1937–47.
Scott DW, Wright GW, Williams PM, Lih CJ, Walsh W, Jaffe ES, et al. Determining cell-of-origin subtypes of diffuse large B-cell lymphoma using gene expression in formalin-fixed paraffin-embedded tissue. Blood. 2014;123:1214–7.
Salles G, de Jong D, Xie W, Rosenwald A, Chhanabhai M, Gaulard P, et al. Prognostic significance of immunohistochemical biomarkers in diffuse large B-cell lymphoma: a study from the Lunenburg Lymphoma Biomarker Consortium. Blood. 2011;117:7070–8.
Esfahani MS, Hamilton EG, Mehrmohamadi M, Nabet BY, Alig SK, King DA, et al. Inferring gene expression from cell-free DNA fragmentation profiles. Nat Biotechnol. 2022;40:585–97.
Clyde D. Using cell-free DNA to infer gene expression. Nat Rev Genet. 2022;23:323.
Rushton CK, Arthur SE, Alcaide M, Cheung M, Jiang A, Coyle KM, et al. Genetic and evolutionary patterns of treatment resistance in relapsed B-cell lymphoma. Blood Adv. 2020;4:2886–98.
Kridel R, Sehn LH, Gascoyne RD. Pathogenesis of follicular lymphoma. J Clin Investig. 2012;122:3424–31.
Montoto S, Fitzgibbon J. Transformation of indolent B-cell lymphomas. J Clin Oncol. 2011;29:1827–34.
Pasqualucci L, Khiabanian H, Fangazio M, Vasishtha M, Messina M, Holmes AB, et al. Genetics of follicular lymphoma transformation. Cell Rep. 2014;6:130–40.
Tam CS, Anderson MA, Pott C, Agarwal R, Handunnetti S, Hicks RJ, et al. Ibrutinib plus venetoclax for the treatment of mantle-cell lymphoma. N Engl J Med. 2018;378:1211–23.
Scherer F, Kurtz DM, Newman AM, Craig AFM, Stehr H, Zhou L, et al. Noninvasive detection of ibrutinib resistance in non-Hodgkin lymphoma using cell-free DNA. Blood. 2016;128:1752.
Locke FL, Miklos DB, Jacobson CA, Perales MA, Kersten MJ, Oluwole OO, et al. Axicabtagene ciloleucel as second-line therapy for large B-Cell lymphoma. N Engl J Med. 2022;386:640–54.
Hamlin PA, Zelenetz AD, Kewalramani T, Qin J, Satagopan JM, Verbel D, et al. Age-adjusted International Prognostic Index predicts autologous stem cell transplantation outcome for patients with relapsed or primary refractory diffuse large B-cell lymphoma. Blood. 2003;102:1989–96.
Park JH, Rivière I, Gonen M, Wang X, Sénéchal B, Curran KJ, et al. Long-term follow-up of CD19 CAR therapy in acute lymphoblastic leukemia. N Engl J Med. 2018;378:449–59.
Acknowledgements
We thank Janina Kress for assistance with the graphic design of the figures.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
EML analyzed the data, designed the work that led to the submission, interpreted the results, helped drafting the manuscript, and approved the final version. JM analyzed the data, designed the work that led to the submission, interpreted the results, helped drafting the manuscript, and approved the final version. FS supervised the work, analyzed the data, designed the work that led to the submission, interpreted the results, and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
EML: No competing financial interests in relation to the work. JM: No competing financial interests in relation to the work. FS: No competing financial interests in relation to the work. Receives research funding from Else Kröner Fresenius-Stiftung (Grant No. 2018_A38), Deutsche Forschungsgemeinschaft (DFG, Grant No. SCHE 1870/3-1), Fördergesellschaft Forschung Tumorbiologie, Zentrum für Personalisierte Medizin, Deutsches Konsortium für Translationale Krebsforschung, Biothera-Stiftung, Forschungskommission Freiburg, and Roche Sequencing Solutions. Supported by the Deutsche Gesellschaft für Innere Medizin Clinician Scientist Program.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lauer, E.M., Mutter, J. & Scherer, F. Circulating tumor DNA in B-cell lymphoma: technical advances, clinical applications, and perspectives for translational research. Leukemia 36, 2151–2164 (2022). https://doi.org/10.1038/s41375-022-01618-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-022-01618-w
This article is cited by
-
Utility of Measurable Residual Disease (MRD) Assessment in Mantle Cell Lymphoma
Current Treatment Options in Oncology (2023)
-
Clinical implications of circulating tumor DNA in predicting the outcome of diffuse large B cell lymphoma patients receiving first-line therapy
BMC Medicine (2022)