Abstract
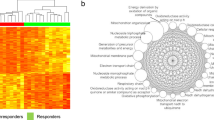
Gemtuzumab ozogamicin (GO) is an anti-CD33 monoclonal antibody linked to calicheamicin, a DNA damaging agent, and is a well-established therapeutic for treating acute myeloid leukemia (AML). In this study, we used LASSO regression modeling to develop a 10-gene DNA damage response gene expression score (CalDDR-GEx10) predictive of clinical outcome in pediatric AML patients treated with treatment regimen containing GO from the AAML03P1 and AAML0531 trials (ADE + GO arm, N = 301). When treated with ADE + GO, patients with a high CalDDR-GEx10 score had lower complete remission rates (62.8% vs. 85.5%, P = 1.7 7 * 10−5) and worse event-free survival (28.7% vs. 56.5% P = 4.08 * 10−8) compared to those with a low CalDDR-GEx10 score. However, the CalDDR-GEx10 score was not associated with clinical outcome in patients treated with standard chemotherapy alone (ADE, N = 242), implying the specificity of the CalDDR-GEx10 score to calicheamicin-induced DNA damage response. In multivariable models adjusted for risk group, FLT3-status, white blood cell count, and age, the CalDDR-GEx10 score remained a significant predictor of outcome in patients treated with ADE + GO. Our findings present a potential tool that can specifically assess response to calicheamicin-induced DNA damage preemptively via assessing diagnostic leukemic cell gene expression and guide clinical decisions related to treatment using GO.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The transcriptomic and clinical data used in this study were obtained from the TARGET database (https://target-data.nci.nih.gov/Public/AML/mRNA-seq), however, data are only publicly available for N = 128 treated with ADE + GO and N = 175 patients treated with ADE alone. Other controlled data used in this study were obtained and used with permission from the Children’s Oncology Group.
References
Döhner H, Weisdorf DJ, Bloomfield CD. Acute myeloid leukemia. N Engl J Med. 2015;373:1136–1152.
Sievers EL, Appelbaum FR, Spielberger RT, Forman SJ, Flowers D, Smith FO, et al. Selective ablation of acute myeloid leukemia using antibody-targeted chemotherapy: a phase I study of an anti-CD33 calicheamicin immunoconjugate. Blood. 1999;93:3678–84.
Hamann PR, Hinman LM, Hollander I, Beyer CF, Lindh D, Holcomb R, et al. Gemtuzumab ozogamicin, a potent and selective anti-CD33 antibody—calicheamicin conjugate for treatment of acute myeloid leukemia. Bioconjug Chem. 2002;13:47–58.
Jen EY, Ko C-W, Lee JE, Del Valle PL, Aydanian A, Jewell C, et al. FDA Approval: Gemtuzumab ozogamicin for the treatment of adults with newly-diagnosed CD33-positive acute myeloid leukemia. Clin Cancer Res. 2018. https://doi.org/10.1158/1078-0432.CCR-17-3179.
Norsworthy KJ, Ko C, Lee JE, Liu J, John CS, Przepiorka D, et al. FDA approval summary: Mylotarg for treatment of patients with relapsed or refractory CD33‐positive acute myeloid leukemia. Oncologist. 2018. https://doi.org/10.1634/theoncologist.2017-0604.
Gbadamosi M, Meshinchi S, Lamba JK Gemtuzumab ozogamicin for treatment of newly diagnosed CD33-positive acute myeloid leukemia. Future Oncol. 2018; 14. https://doi.org/10.2217/fon-2018-0325.
Pollard JA, Alonzo TA, Loken M, Gerbing RB, Ho PA, Bernstein ID, et al. Correlation of CD33 expression level with disease characteristics and response to gemtuzumab ozogamicin containing chemotherapy in childhood AML. Blood. 2012;119:3705–3711.
Pollard JA, Loken M, Gerbing RB, Raimondi SC, Hirsch BA, Aplenc R, et al. CD33 expression and its association with gemtuzumab ozogamicin response: results from the randomized phase III children’s oncology group trial AAML0531. J Clin Oncol. 2016;34:747–755.
Lamba JK, Chauhan L, Shin M, Loken MR, Pollard JA, Wang YC, et al. CD33 splicing polymorphism determines gemtuzumab ozogamicin response in de novo acute myeloid leukemia: Report from randomized phase III children’s oncology group trial AAML0531. J Clin Oncol. 2017;35:674–2682.
Chauhan L, Shin M, Wang Y-C, Loken M, Pollard J, Aplenc R, et al. CD33_PGx6_Score predicts gemtuzumab ozogamicin response in childhood acute myeloid leukemia: a report from the Children’s Oncology Group. JCO Precis Oncol. 2019:3;1–15.
Rafiee R, Chauhan L, Alonzo TA, Wang YC, Elmasry A, Loken MR, et al. ABCB1 SNP predicts outcome in patients with acute myeloid leukemia treated with Gemtuzumab ozogamicin: a report from Children’s Oncology Group AAML0531 trial. Blood Cancer J. 2019; 9. https://doi.org/10.1038/s41408-019-0211-y.
Zein N, Sinha A, McGahren W, Ellestad G. Calicheamicin yI: an antitumor antibiotic that cleaves double-stranded DNA site specifically. Science. 1988;240:198–201.
Dedon PC, Salzberg AA, Xu J. Exclusive production of bistranded DNA damage by calicheamicin. Biochemistry. 1993;32:3617–3622.
Elmroth K, Nygren J, Mårtensson S, Ismail IH, Hammarsten O. Cleavage of cellular DNA by calicheamicin gamma1. DNA Repair. 2003;2:363–374.
Dedon PC, Goldberg IH. Free-radical mechanisms involved in the formation of sequence-dependent bistranded DNA lesions by the antitumor antibiotics bleomycin, neocarzinostatin, and calicheamicin. Chem Res Toxicol. 1992;5:311–332.
Pannunzio NR, Watanabe G, Lieber MR. Nonhomologous DNA end-joining for repair of DNA double-strand breaks. J Biol Chem. 2018;293:10512–10523.
Lieber MR. The mechanism of double-strand DNA break repair by the nonhomologous DNA end-joining pathway. Annu Rev Biochem. 2010;79:181–211.
Shibata A, Jeggo PA. DNA double-strand break repair in a cellular context. Clin Oncol. 2014;26:243–249.
Amico D, Barbui AM, Erba E, Rambaldi A, Introna M. Differential response of human acute myeloid leukemia cells to gemtuzumab ozogamicin in vitro: role of Chk1 and Chk2 phosphorylation and caspase 3. Blood. 2003;101:4589–4597.
Rosen DB, Harrington KH, Cordeiro JA, Leung LY, Putta S, Lacayo N, et al. AKT signaling as a novel factor associated with in vitro resistance of human AML to gemtuzumab ozogamicin. PLoS One. 2013;8:e53518.
Carr MI, Zimmermann A, Chiu L-Y, Zenke FT, Blaukat A, Vassilev LT. DNA-PK inhibitor, M3814, as a new combination partner of mylotarg in the treatment of acute myeloid leukemia. Front Oncol. 2020;10:127.
Godwin CD, Bates OM, Jean SR, Laszlo GS, Garling EE, Beddoe ME, et al. Anti-apoptotic BCL-2 family proteins confer resistance to calicheamicin-based antibody-drug conjugate therapy of acute leukemia. Leuk Lymphoma. 2020;61:2990–2994.
Papageorgiou I, Loken MR, Brodersen LE, Gbadamosi M, Uy GL, Meshinchi S, et al. CCGG deletion (rs201074739) in CD33 results in premature termination codon and complete loss of CD33 expression: another key variant with potential impact on response to CD33-directed agents. Leuk Lymphoma. 2019;60. https://doi.org/10.1080/10428194.2019.1569232.
Xu Q, He S, Yu L. Clinical benefits and safety of gemtuzumab ozogamicin in treating acute myeloid leukemia in various subgroups: an updated systematic review, meta-analysis, and network meta-analysis. Front Immunol. 2021;12. https://www.frontiersin.org/article/10.3389/fimmu.2021.683595.
Cooper TM, Franklin J, Gerbing RB, Alonzo TA, Hurwitz C, Raimondi SC, et al. AAML03P1, a pilot study of the safety of gemtuzumab ozogamicin in combination with chemotherapy for newly diagnosed childhood acute myeloid leukemia: a report from the Children’s Oncology Group. Cancer. 2012;118:761–769.
Gamis AS, Alonzo TA, Meshinchi S, Sung L, Gerbing RB, Raimondi SC, et al. Gemtuzumab ozogamicin in children and adolescents with de novo acute myeloid leukemia improves event-free survival by reducing relapse risk: Results from the randomized phase III children’s oncology group Trial AAML0531. J Clin Oncol. 2014;32:3021–3032.
Elsayed AH, Rafiee R, Cao X, Raimondi S, Downing JR, Ribeiro R, et al. A six-gene leukemic stem cell score identifies high risk pediatric acute myeloid leukemia. Leukemia. 2020;34:735–745.
Therneau TM, Atkinson EJ, Foundation M. An introduction to recursive partitioning using the RPART routines (Long). 2022:1–52.
Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and regression trees. Routledge, 2017.
Acknowledgements
This work was supported by the NIH (R21CA155524), The Leukemia Lymphoma Society (6610-20), The St Baldrick’s Foundation, University of Florida Health Cancer Center, and College of Pharmacy, University of Florida. NIH awards U10CA180899, U10CA180886, U10CA98413, and U10CA098543 supported the clinical trial.
Author information
Authors and Affiliations
Contributions
Study concept and design: JKL and MOG; Acquisition of clinical data: RR, TAD, AG, SM, and BAH; Data generation, analysis, and interpretations: MOG, VS, RR, AHE, OO, NN, ADJ, YW, AD, TAD, SM, and JKL; Manuscript writing and preparation: MOG and JKL; Revision and review of manuscript: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Gbadamosi, M.O., Shastri, V.M., Elsayed, A.H. et al. A ten-gene DNA-damage response pathway gene expression signature predicts gemtuzumab ozogamicin response in pediatric AML patients treated on COGAAML0531 and AAML03P1 trials. Leukemia 36, 2022–2031 (2022). https://doi.org/10.1038/s41375-022-01622-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41375-022-01622-0