Abstract
Background and Objective
Muscle injuries are one of the main daily problems in sports medicine, football in particular. However, we do not have a reliable means to predict the outcome, i.e. return to play from severe injury. The aim of the present study was to evaluate the capability of the MLG-R classification system to grade hamstring muscle injuries by severity, offer a prognosis for the return to play, and identify injuries with a higher risk of re-injury. Furthermore, we aimed to assess the consistency of our proposed system by investigating its intra-observer and inter-observer reliability.
Methods
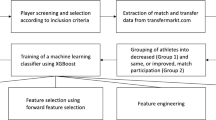
All male professional football players from FC Barcelona, senior A and B and the two U-19 teams, with injuries that occurred between February 2010 and February 2020 were reviewed. Only players with a clinical presentation of a hamstring muscle injury, with complete clinic information and magnetic resonance images, were included. Three different statistical and machine learning approaches (linear regression, random forest, and eXtreme Gradient Boosting) were used to assess the importance of each factor of the MLG-R classification system in determining the return to play, as well as to offer a prediction of the expected return to play. We used the Cohen’s kappa and the intra-class correlation coefficient to assess the intra-observer and inter-observer reliability.
Results
Between 2010 and 2020, 76 hamstring injuries corresponding to 42 different players were identified, of which 50 (65.8%) were grade 3r, 54 (71.1%) affected the biceps femoris long head, and 33 of the 76 (43.4%) were located at the proximal myotendinous junction. The mean return to play for grades 2, 3, and 3r injuries were 14.3, 12.4, and 37 days, respectively. Injuries affecting the proximal myotendinous junction had a mean return to play of 31.7 days while those affecting the distal part of the myotendinous junction had a mean return to play of 23.9 days. The analysis of the grade 3r biceps femoris long head injuries located at the free tendon showed a median return to play time of 56 days while the injuries located at the central tendon had a shorter return to play of 24 days (p = 0.038). The statistical analysis showed an excellent predictive power of the MLG-R classification system with a mean absolute error of 9.8 days and an R-squared of 0.48. The most important factors to determine the return to play were if the injury was at the free tendon of the biceps femoris long head or if it was a grade 3r injury. For all the items of the MLG-R classification, the intra-observer and inter-observer reliability was excellent (k > 0.93) except for fibres blurring (κ = 0.68).
Conclusions
The main determinant for a long return to play after a hamstring injury is the injury affecting the connective tissue structures of the hamstring. We developed a reliable hamstring muscle injury classification system based on magnetic resonance imaging that showed excellent results in terms of reliability, prognosis capability and objectivity. It is easy to use in clinical daily practice, and can be further adapted to future knowledge. The adoption of this system by the medical community would allow a uniform diagnosis leading to better injury management.




Similar content being viewed by others
References
Ekstrand J, Hägglund M, Waldén M. Epidemiology of muscle injuries in professional football (soccer). Am J Sports Med. 2011;39(6):1226–32.
Williams S, Trewartha G, Kemp S, Stokes K. A meta-analysis of injuries in senior men’s professional rugby union. Sports Med. 2013;43(10):1043–55.
Olson D, Sikka RS, Labounty A, Christensen T. Injuries in professional football: current concepts. Curr Sports Med Rep. 2013;12(6):38–90.
Feddermann-Demont N, Junge A, Edouard P, Branco P, Alonso J-M. Injuries in 13 international athletics championships between 2007–2012. Br J Sports Med. 2014;48(7):513–22.
Ekstrand J, Healy JC, Waldén M, Lee JC, English B, Hägglund M. Hamstring muscle injuries in professional football: the correlation of MRI findings with return to play. Br J Sports Med. 2012;46(2):112–7.
Orchard J, Best TM, Verrall GM. Return to play following muscle strains. Clin J Sport Med. 2005;15(6):436–41.
Carling C, Le Gall F, Orhant E. A four-season prospective study of muscle strain reoccurrences in a professional football club. Res Sports Med. 2011;19(2):92–102.
Koulouris G, Connell DA, Brukner P, Schneider-Kolsky M. Magnetic resonance imaging parameters for assessing risk of recurrent hamstring injuries in elite athletes. Am J Sports Med. 2007;35(9):1500–6.
Ekstrand J, Waldén M, Hägglund M. Hamstring injuries have increased by 4% annually in men’s professional football, since 2001: a 13-year longitudinal analysis of the UEFA Elite Club injury study. Br J Sports Med. 2016;50(12):731–7.
Delvaux F, Rochcongar P, Bruyère O, Bourlet G, Daniel C, Diverse P, et al. Return-to-play criteria after hamstring injury: actual medicine practice in professional soccer teams. J Sports Sci Med. 2014;13(3):721.
Barnes C, Archer D, Hogg B, Bush M, Bradley P. The evolution of physical and technical performance parameters in the English Premier League. Int J Sports Med. 2014;35(13):1095–100.
Valle X, L.Tol J, Hamilton B, Rodas G, Malliaras P, et al. Hamstring Muscle Injuries, a Rehabilitation Protocol Purpose. Asian J Sports Med. 2015;6(4):e25411
Dellal A, Lago-Peñas C, Rey E, Chamari K, Orhant E. The effects of a congested fixture period on physical performance, technical activity and injury rate during matches in a professional soccer team. Br J Sports Med. 2015;49(6):390–4.
Vermeulen R, Almusa E, Buckens S, et al. Complete resolution of a hamstring intramuscular tendon injury on MRI is not necessary for a clinically successful return to play. Br J Sports Med. 2021;55:397–402.
Isern-Kebschull J, Mechó S, Pruna R, Kassarjian A, Valle X, Yanguas X, et al. Sports-related lower limb muscle injuries: pattern recognition approach and MRI review. Insights Imaging. 2020;11(1):108.
Valle X, Alentorn-Geli E, Tol JL, Hamilton B, Garrett WE, Pruna R, et al. Muscle injuries in sports: a new evidence-informed and expert consensus-based classification with clinical application. Sports Med. 2017;47(7):1241–53.
Hamilton B, Valle X, Rodas G, Til L, Grive RP, Rincon JAG, et al. Classification and grading of muscle injuries: a narrative review. Br J Sports Med. 2015;49(5):306.
Patel A, Chakraverty J, Pollock N, Chakraverty R, Suokas A, James S. British athletics muscle injury classification: a reliability study for a new grading system. Clin Radiol. 2015;70(12):1414–20.
Wangensteen A, Tol JL, Roemer FW, Bahr R, Dijkstra HP, Crema MD, et al. Intra-and interrater reliability of three different MRI grading and classification systems after acute hamstring injuries. Eur J Radiol. 2017;89:182–90.
Hamilton B, Alonso J-M, Best TM. Time for a paradigm shift in the classification of muscle injuries. J Sport Health Sci. 2017;6(3):255–61.
Valle X, Mechó S, Pruna R, Pedret C, Isern J, Monllau JC, et al. The MLG-R muscle injury classification for hamstrings: examples and guidelines for its use. Apunts Medicina de l" Esport (English Edition). FC Barcelona and Consell Catala de l'Esport. Madrid: Elsevier; 2018.
Gillies AR, Lieber RL. Structure and function of the skeletal muscle extracellular matrix. Muscle Nerve. 2011;44(3):318–31.
Wilke J, Hespanhol L, Behrens M. Is it all about the fascia? A systematic review and meta-analysis of the prevalence of extramuscular connective tissue lesions in muscle strain injury. Orthop J Sports Med. 2019;7(12):2325967119888500.
McLoon LK, Vicente A, Fitzpatrick KR, Lindström M, Domellöf FP. Composition, architecture, and functional implications of the connective tissue network of the extraocular muscles. Invest Ophthalmol Vis Sci. 2018;59(1):322–9.
de Dios B-J, Garrigosa AL, Cuevas PD, Riaza LM, Terés XP, Alonso JM, et al. Translation into Spanish and proposal to modify the Orchard Sports Injury Classification System (OSICS) version 12. Apunts Sports Med. 2020;55(207):105–9.
Pérez LT, Orchard J, Rae K. El sistema de clasificación y codificación OSICS-10 traducido del inglés. Apunts Medicina de l’Esport. 2008;43(159):109–12.
Pruna R, Andersen TE, Clarsen B, McCall A, HUB BI. Muscle injury guide: prevention of and return to play from muscle injuries, 1st edn. 2019. FC Barcelona: Barça Innovation Hub
Moen M, Reurink G, Weir A, Tol J, Maas M, Goudswaard GJ. Predicting return to play after hamstring injuries. Br J Sports Med. 2014;48(18):1358–63.
Jacobsen P, Witvrouw E, Muxart P, Tol JL, Whiteley R. A combination of initial and follow-up physiotherapist examination predicts physician-determined time to return to play after hamstring injury, with no added value of MRI. Br J Sports Med. 2016;50(7):431–9.
Breiman L. Bagging predictors. Mach Learn. 1996;24(2):123–40.
Chen T, Guestrin C, editors. XGBoost: a scalable tree boosting system. Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining; 13–17 Aug 2016; San Francisco (CA).
Lundberg SM, Lee SI. A unified approach to interpreting model predictions. Adv Neural Inform Process Syst. 2017;30.
Apley DW, Zhu J. Visualizing the effects of predictor variables in black box supervised learning models. arXiv preprint. 2016:161208468.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria; 2020. https://www.R-project.org/.
Mueller-Wohlfahrt H-W, Haensel L, Mithoefer K, Ekstrand J, English B, McNally S, et al. Terminology and classification of muscle injuries in sport: the Munich consensus statement. Br J Sports Med. 2013;47(6):342–50.
Pollock N, Patel A, Chakraverty J, Suokas A, James SL, Chakraverty R. Time to return to full training is delayed and recurrence rate is higher in intratendinous (‘c’) acute hamstring injury in elite track and field athletes: clinical application of the British Athletics Muscle Injury Classification. Br J Sports Med. 2016;50(5):305–10.
Fournier-Farley C, Lamontagne M, Gendron P, Gagnon DH. Determinants of return to play after the nonoperative management of hamstring injuries in athletes: a systematic review. Am J Sports Med. 2016;44(8):2166–72.
Brukner P, Connell D. ‘Serious thigh muscle strains’: beware the intramuscular tendon which plays an important role in difficult hamstring and quadriceps muscle strains. Br J Sports Med. 2016;50(4):205–8.
Lempainen L, Kosola J, Pruna R, Puigdellivol J, Sarimo J, Niemi P, et al. Central tendon injuries of hamstring muscles: case series of operative treatment. Orthop J Sports Med. 2018;6(2):2325967118755992.
Garrett JRWE, Nikolaou PK, Ribbeck BM, Glisson RR, Seaber AV. The effect of muscle architecture on the biomechanical failure properties of skeletal muscle under passive extension. Am J Sports Med. 1988;16(1):7–12.
Nikolaou PK, Macdonald BL, Glisson RR, Seaber AV, Garrett JRWE. Biomechanical and histological evaluation of muscle after controlled strain injury. Am J Sports Med. 1987;15(1):9–14.
Valle X, Malliaropoulos N, Párraga Botero JD, Bikos G, Pruna R, Mónaco M, et al. Hamstring and other thigh injuries in children and young athletes. Scand J Med Sci Sports. 2018;28(12):2630–7.
Schache AG, Koulouris G, Kofoed W, Morris HG, Pandy MG. Rupture of the conjoint tendon at the proximal musculotendinous junction of the biceps femoris long head: a case report. Knee Surg Sports Traumatol Arthrosc. 2008;16(8):797–802.
Hijikata T, Ishikawa H. Functional morphology of serially linked skeletal muscle fibers. Cells Tissues Organs. 1997;159(2–3):99–107.
Roberts TJ, Eng CM, Sleboda DA, Holt NC, Brainerd EL, Stover KK, et al. The multi-scale, three-dimensional nature of skeletal muscle contraction. Physiology. 2019;34(6):402–8.
Järvinen TA, Józsa L, Kannus P, Järvinen TL, Järvinen M. Organization and distribution of intramuscular connective tissue in normal and immobilized skeletal muscles. J Muscle Res Cell Motility. 2002;23(3):245–54.
Gillies AR, Chapman MA, Bushong EA, Deerinck TJ, Ellisman MH, Lieber RL. High resolution three-dimensional reconstruction of fibrotic skeletal muscle extracellular matrix. J Physiol. 2017;595(4):1159–71.
Chan O, Del Buono A, Best TM, Maffulli N. Acute muscle strain injuries: a proposed new classification system. Knee Surg Sports Traumatol Arthrosc. 2012;20(11):2356–62.
Entwisle T, Ling Y, Splatt A, Brukner P, Connell D. Distal musculotendinous T junction injuries of the biceps femoris: an MRI case review. Orthop J Sports Med. 2017;5(7):2325967117714998.
Pasta G, Nanni G, Molini L, Bianchi S. Sonography of the quadriceps muscle: examination technique, normal anatomy, and traumatic lesions. J Ultrasound. 2010;13(2):76–84.
Connell DA, Schneider-Kolsky ME, Hoving JL, Malara F, Buchbinder R, Koulouris G, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. Am J Roentgenol. 2004;183(4):975–84.
Cross TM, Gibbs N, Houang MT, Cameron M. Acute quadriceps muscle strains: magnetic resonance imaging features and prognosis. Am J Sports Med. 2004;32(3):710–9.
Pomeranz SJ, Heidt R Jr. MR imaging in the prognostication of hamstring injury: work in progress. Radiology. 1993;189(3):897–900.
Bianchi S, Martinoli C, Waser N, Bianchi-Zamorani M, Federici E, Fasel J. Central aponeurosis tears of the rectus femoris: sonographic findings. Skeletal Radiol. 2002;31(10):581–6.
Muscle SGot, Traumatology TSftSSoS, Balius R, Blasi M, Pedret C, Alomar X, et al. A histoarchitectural approach to skeletal muscle injury: searching for a common nomenclature. Orthop J Sports Med. 2020;8(3):2325967120909090.
Adstrum S, Nicholson H. A history of fascia. Clin Anat. 2019;32(7):862–70.
Schleip R, Hedley G, Yucesoy CA. Fascial nomenclature: update on related consensus process. Clin Anat. 2019;32(7):929–33.
Kjær M, Magnusson P, Krogsgaard M, Møller JB, Olesen J, Heinemeier K, et al. Extracellular matrix adaptation of tendon and skeletal muscle to exercise. J Anat. 2006;208(4):445–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the present study.
Conflict of interest
None of the authors has a conflict of interest related to the present investigation.
Ethics Approval
This study was assessed and approved by the Ethics Committee of the “Consell Català de l’Esport” with the number 10/CEICGC/2020. The present study was performed in accordance with the standards of ethics outlined in the Declaration of Helsinki.
Consent to Participate
Appropriate written informed consent to participate in research projects was obtained from all FC Barcelona football players.
Consent for Publication
Appropriate written informed consent for publication was obtained from all participants in the present study.
Availability of Data and Material
The datasets generated during and/or analysed during the current study are not publicly available because of the fact that many of the players had their injury status publicly informed in the mass media and, therefore, some personal information from the players regarding their injuries could be deduced. This could imply a violation of the patients’ privacy and confidentiality noted in statement number 24 of the Declaration of Helsinki. We could make it available from the corresponding author on reasonable request, from a medical institution.
Code Availability
Not applicable.
Author Contributions
XV and XY collected all the data. XV and SM analysed the magnetic resonance images. AM conducted all the statistical analyses. XV, SM, EAG, TJ and AM prepared the manuscript. RP, LL, GR, JCM, JI, MG and RB were the major contributors to the preparation of the manuscript. All authors contributed to the last editing and approval of the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Valle, X., Mechó, S., Alentorn-Geli, E. et al. Return to Play Prediction Accuracy of the MLG-R Classification System for Hamstring Injuries in Football Players: A Machine Learning Approach. Sports Med 52, 2271–2282 (2022). https://doi.org/10.1007/s40279-022-01672-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-022-01672-5