Abstract
Background and Objective
Vancomycin is frequently used to treat Gram-positive bacterial infections in neonates. However, there is still no consensus on the optimal initial dosing regimen. This study aimed to assess the performance of pharmacokinetic model-based virtual trials to predict the dose–exposure relationship of vancomycin in neonates.
Methods
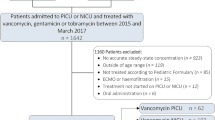
The PubMed database was searched for clinical trials of vancomycin in neonates that reported the percentage of target attainment. Monte Carlo simulations were performed using nonlinear mixed-effect modeling to predict the dose–exposure relationship, and the differences in outcomes between virtual trials and real-world data in clinical studies were calculated.
Results
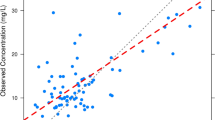
A total of 11 studies with 14 dosing groups were identified from the literature to evaluate dose–exposure relationships. For the ten dosing groups where the surrogate marker for exposure was the trough concentration, the mean ± standard deviation (SD) for the target attainment between original studies and virtual trials was 3.0 ± 7.3%. Deviations between − 10 and 10% accounted for 80% of the included dosing groups. For the other four dosing groups where the surrogate marker for exposure was concentration during continuous infusion, all deviations were between − 10 and 10%, and the mean ± SD value was 2.9 ± 4.5%.
Conclusion
The pharmacokinetic model-based virtual trials of vancomycin exhibited good predictive performance for dose–exposure relationships in neonates. These results might be used to assist the optimization of dosing regimens in neonatal practice, avoiding the need for trial and error.



Similar content being viewed by others
References
Jacqz-Aigrain E, Zhao W, Sharland M, van den Anker JN. Use of antibacterial agents in the neonate: 50 years of experience with vancomycin administration. Semin Fetal Neonatal Med. 2013;18(1):28–34. https://doi.org/10.1016/j.siny.2012.10.003.
Rubin LG, Sanchez PJ, Siegel J, Levine G, Saiman L, Jarvis WR, et al. Evaluation and treatment of neonates with suspected late-onset sepsis: a survey of neonatologists’ practices. Pediatrics. 2002;110(4): e42. https://doi.org/10.1542/peds.110.4.e42.
Hospira. FDA label of vancomycin hydrochloride for injection. https://www.accessdatafdagov/scripts/cder/daf/indexcfm?event=overviewprocess&ApplNo=063076. 2012.
Kadambari S, Heath PT, Sharland M, Lewis S, Nichols A, Turner MA. Variation in gentamicin and vancomycin dosage and monitoring in UK neonatal units. J Antimicrob Chemother. 2011;66(11):2647–50. https://doi.org/10.1093/jac/dkr351.
Leroux S, Zhao W, Betremieux P, Pladys P, Saliba E, Jacqz-Aigrain E, et al. Therapeutic guidelines for prescribing antibiotics in neonates should be evidence-based: a French national survey. Arch Dis Child. 2015;100(4):394–8. https://doi.org/10.1136/archdischild-2014-306873.
Veluzat S, Pauquet E, Sarlangue J. Practice survey on the use of vancomycin in pediatrics in the New Aquitaine region and guidelines of learned societies. Arch Pediatrie. 2020;27(4):176–82. https://doi.org/10.1016/j.arcped.2020.03.013.
Thomson Reuters Y. Neofax, 24th edn. Thomson Reuters, Montvale. 2011.
Tschudy MAK. The Harriet lane handbook. 19th ed. Philadelphia: Elsevier Mosby; 2012.
Lestner JM, Hill LF, Heath PT, Sharland M. Vancomycin toxicity in neonates: a review of the evidence. Curr Opin Infect Dis. 2016;29(3):237–47. https://doi.org/10.1097/QCO.0000000000000263.
Jacqz-Aigrain E, Leroux S, Thomson AH, Allegaert K, Capparelli EV, Biran V, et al. Population pharmacokinetic meta-analysis of individual data to design the first randomized efficacy trial of vancomycin in neonates and young infants. J Antimicrob Chemother. 2019;74(8):2128–38. https://doi.org/10.1093/jac/dkz158.
Zhao W, Lopez E, Biran V, Durrmeyer X, Fakhoury M, Jacqz-Aigrain E. Vancomycin continuous infusion in neonates: dosing optimisation and therapeutic drug monitoring. Arch Dis Child. 2013;98(6):449–53. https://doi.org/10.1136/archdischild-2012-302765.
Cies JJ, Moore WS 2nd, Nichols K, Knoderer CA, Carella DM, Chopra A. Population pharmacokinetics and pharmacodynamic target attainment of vancomycin in neonates on extracorporeal life support. Pediatr Crit Care Med. 2017;18(10):977–85. https://doi.org/10.1097/PCC.0000000000001250.
Gwee A, Cranswick N, McMullan B, Perkins E, Bolisetty S, Gardiner K, et al. Continuous versus intermittent vancomycin infusions in infants: a randomized controlled trial. Pediatrics. 2019. https://doi.org/10.1542/peds.2018-2179.
Reilly AM, Ding MX, Rower JE, Kiser TH. The effectiveness of a vancomycin dosing guideline in the neonatal intensive care unit for achieving goal therapeutic trough concentrations. J Clin Pharmacol. 2019;59(7):997–1005. https://doi.org/10.1002/jcph.1392.
Sosnin N, Curtis N, Cranswick N, Chiletti R, Gwee A. Vancomycin is commonly under-dosed in critically ill children and neonates. Brit J Clin Pharmaco. 2019;85(11):2591–8. https://doi.org/10.1111/bcp.14084.
Dersch-Mills D, Bengry T, Akierman A, Alshaikh B, Yusuf K. Assessment of initial vancomycin dosing in neonates. Paed Child Healt-Can. 2014;19(6):E30–4. https://doi.org/10.1093/pch/19.6.291.
Sinkeler FS, de Haan TR, Hodiamont CJ, Bijleveld YA, Pajkrt D, Mathot RAA. Inadequate vancomycin therapy in term and preterm neonates: a retrospective analysis of trough serum concentrations in relation to minimal inhibitory concentrations. BMC Pediatr. 2014. https://doi.org/10.1186/1471-2431-14-193.
Tan W-H. Dose regimen for vancomycin not needing serum peak levels? Arch Dis Child Fetal Neonatal Ed. 2002;87(3):214–6. https://doi.org/10.1136/fn.87.3.F214.
Irikura M, Fujiyama A, Saita F, Fukushima S, Kitaoka H, Fukuda T, et al. Evaluation of the vancomycin dosage regimen based on serum creatinine used in the neonatal intensive care unit. Pediatr Int. 2011;53(6):1038–44. https://doi.org/10.1111/j.1442-200X.2011.03441.x.
Rybak MJ, Le J, Lodise TP, Levine DP, Bradley JS, Liu C, et al. Therapeutic monitoring of vancomycin for serious methicillin-resistant staphylococcus aureus infections: a revised consensus guideline and review by the American society of health-system pharmacists, the infectious diseases society of America, the pediatric infectious diseases society, and the society of infectious diseases pharmacists. Clin Infect Dis. 2020;71(6):1361–4. https://doi.org/10.1093/cid/ciaa303.
Pacifici GM, Allegaert K. Clinical pharmacokinetics of vancomycin in the neonate: a review. Clinics (Sao Paulo). 2012;67(7):831–7. https://doi.org/10.6061/clinics/2012(07)21.
Pawlotsky F, Thomas A, Kergueris MF, Debillon T, Roze JC. Constant rate infusion of vancomycin in premature neonates: a new dosage schedule. Br J Clin Pharmacol. 1998;46(2):163–7. https://doi.org/10.1046/j.1365-2125.1998.00763.x.
Madigan T, Teng CB, Koshaish J, Johnson KR, Graner KK, Banerjee R. Optimization of vancomycin dosing in very low-birth-weight preterm neonates. Am J Perinat. 2015;32(1):83–6. https://doi.org/10.1055/s-0034-1376183.
de Hoog M, Schoemaker RC, Mouton JW, van den Anker JN. Vancomycin population pharmacokinetics in neonates. Clin Pharmacol Ther. 2000;67(4):360–7. https://doi.org/10.1067/mcp.2000.105353.
Leroux S, Biran V, Lopez E, Madeleneau D, Wallon C, Zana-Taieb E, et al. The clinical utility and safety of a model-based patient-tailored dose of vancomycin in neonates. Fund Clin Pharmacol. 2016;30:19-.
Tang BH, Wu YE, Kou C, Qi YJ, Qi H, Xu HY, et al. Population Pharmacokinetics and dosing optimization of amoxicillin in neonates and young infants. Antimicrob Agents Chemother. 2019. https://doi.org/10.1128/AAC.02336-18.
Zheng Y, Liu SP, Xu BP, Shi ZR, Wang K, Yang JB, et al. Population pharmacokinetics and dosing optimization of azithromycin in children with community-acquired pneumonia. Antimicrob Agents Chemother. 2018. https://doi.org/10.1128/AAC.00686-18.
Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52(3):285–92. https://doi.org/10.1093/cid/cir034.
Holford N, Ma SC, Ploeger BA. Clinical trial simulation: a review. Clin Pharmacol Ther. 2010;88(2):166–82. https://doi.org/10.1038/clpt.2010.114.
Li CH, Sherer EA, Lewis LD, Bies RR. Clinical trial simulation to evaluate population pharmacokinetics and food effect: capturing abiraterone and nilotinib exposures. J Clin Pharmacol. 2015;55(5):556–62. https://doi.org/10.1002/jcph.449.
Acknowledgements
The authors thank all the patients who participated in this study and all the participants and research staff in our hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the National Natural Science Foundation of China (grant number 82173897); Young Taishan Scholars Program of Shandong Province; and Distinguished Young and Middle-aged Scholar of Shandong University.
Conflict of Interest
Bu-Fan Yao, Yue-E Wu, Bo-Hao Tang, Guo-Xiang Hao, Evelyne Jacqz-Aigrain, John van den Anker and Wei Zhao have no conflicts of interest relevant to this article.
Availability of Data and Material
Research data will not be shared.
Code Availability
Research code will not be shared.
Consent to participate
All participants received written informed consent.
Consent for publication
Written informed consent for publication was obtained from all participants.
Author Contributions
Bu-Fan Yao contributed to the interpretation of the data for the work, the literature search, the PPK modeling analysis, drafting of the initial manuscript, and revising of the subsequent drafts. Yue-E Wu, Bo-Hao Tang, and Guo-Xiang Hao designed the study and reviewed the data. Evelyne Jacqz-Aigrain and John van den Anker interpreted the data for the work, provided advice, and critically reviewed and revised the manuscript. Wei Zhao contributed to the conception and design of the work, supervised the data, and critically reviewed and revised the manuscript. All authors performed the study, participated in the drafting of the manuscript, and approved the final version of the manuscript for submission.
Ethics Approval
All the data were obtained from our previous studies. These studies were approved by the institutional ethics committee.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yao, BF., Wu, YE., Tang, BH. et al. Predictive Performance of Pharmacokinetic Model-Based Virtual Trials of Vancomycin in Neonates: Mathematics Matches Clinical Observation. Clin Pharmacokinet 61, 1027–1038 (2022). https://doi.org/10.1007/s40262-022-01128-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-022-01128-z