Abstract
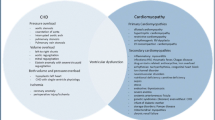
For a long time, pediatric heart failure (HF) with preserved systolic function (HFpEF) has been noted in patients with cardiomyopathies and congenital heart disease. HFpEF is infrequently reported in children and instead of using the HFpEF terminology the HF symptoms are attributed to diastolic dysfunction. Identifying HFpEF in children is challenging because of heterogeneous etiologies and unknown pathophysiological mechanisms. Advances in echocardiography and cardiac magnetic resonance imaging techniques have further increased our understanding of HFpEF in children. However, the literature does not describe the incidence, etiology, clinical features, and treatment of HFpEF in children. At present, treatment of HFpEF in children is extrapolated from clinical trials in adults. There are significant differences between pediatric and adult HF with reduced ejection fraction, supported by a lack of adequate response to adult HF therapies. Evidence-based clinical trials in children are still not available because of the difficulty of conducting trials with a limited number of pediatric patients with HF. The treatment of HFpEF in children is based upon the clinician’s experience, and the majority of children receive off-level medications. There are significant differences between pediatric and adult HFpEF pharmacotherapies in many areas, including side-effect profiles, underlying pathophysiologies, the β-receptor physiology, and pharmacokinetics and pharmacodynamics. This review describes the present and future treatments for children with HFpEF compared with adults. This review also highlights the need to urgently test new therapies in children with HFpEF to demonstrate the safety and efficacy of drugs and devices with proven benefits in adults.

Similar content being viewed by others
References
McDonagh TA, Metra M, Adamo M, ESC Scientific Document Group, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–726.
Campbell RT, Petrie MC, McMurray JJV. Redefining heart failure phenotypes based on ejection fraction. Eur J Heart Fail. 2018;20:1634–5.
Bursi F, Weston SA, Redfield MM, et al. Systolic and diastolic heart failure in the community. JAMA. 2006;296:2209–16.
Recher M, Botte A, Soquet J, Baudelet JB, Godart F, Leteurtre S. Assessment of left ventricular diastolic function in pediatric intensive care patients: a review of parameters and limitations compared with those for adults. World J Pediatr. 2021;17:21–30.
McMahon CJ, Nagueh SF, Pignatelli RH, et al. Characterization of left ventricular diastolic function by tissue Doppler imaging and clinical status in children with hypertrophic cardiomyopathy. Circulation. 2004;109:1756–62.
Friedberg MK, Silverman NH. The systolic to diastolic ratio in children with heart failure secondary to restrictive cardiomyopathy. J Am Soc Echocard. 2006;19:1326–31.
Budts W, Ravekes WJ, Danford DA, Kutty S. Diastolic heart failure with Fontan circulation: a review. JAMA Cardiol. 2020;5:590–7.
Alsaied T, Moore RA, Lang SM, et al. Myocardial fibrosis, diastolic dysfunction and elevated liver stiffness in the Fontan circulation. Open Heart. 2020;7: e001434.
Hui W, Abd El Rahman MY, Schuck R, et al. Diastolic asynchrony and myocardial dysfunction in patients with univentricular heart after Fontan operation. J Echocardiogr. 2013;11:130–7.
Kao AC, Trigt PV, Shaeffer-McCall GS, et al. Allograft diastolic dysfunction and chronotropic incompetence limit cardiac output response to exercise two to six years after heart transplantation. J Heart Lung Transplant. 1995;14:11–22.
Tallaj JA, Kirklin JK, Brown RN, et al. post-heart transplant diastolic dysfunction is a risk factor for mortality. J Am Coll Cardiol. 2007;50:1064–9.
Korang-Asante A, Fickey M, Boucek MM, et al. Diastolic performance assessed by tissue Doppler after pediatric heart transplantation. J Heart Lung Transplant. 2004;23:865–72.
Kindel SJ, Law YM, Chin C, et al. Improved detection of cardiac allograft vasculopathy: a multi-institutional analysis of functional parameters in pediatric heart transplant recipients. J Am Coll Cardiol. 2015;66:547–57.
Blanco J, Muriel-Bombin A, Sagredo V, et al. Incidence, organ dysfunction and mortality in severe sepsis: a Spanish multicenter study. Crit Care. 2008;12:R158.
Jain A, Sankar J, Anubhuti A, Yadav DK, Sankar MJ. Myocardial dysfunction in children with “sepsis” “with” and “without shock”: a prospective observational study. J Trop Pediatr. 2018;64:501–9.
Vallabhajosyula S, Pruthi S, Shah S, Wiley BM, Mankad SV, Jentxer JC. Basic and advanced echocardiographic evaluation of myocardial dysfunction in sepsis and septic shock. Anaesth Intensive Care. 2018;46:13–24.
Mitsnefes MM, Kimball TR, Border WL, et al. Impaired left ventricular diastolic function in children with chronic renal failure. Kidney Int. 2004;65:1461–6.
Mitsnefes MM. Cardiovascular complications of pediatric chronic kidney disease. Pediatr Nephrol. 2008;23:27–39.
Unger ED, Dubin RF, Deo R, et al. Association of chronic kidney disease with abnormal cardiac mechanics and adverse outcomes in patients with heart failure and preserved ejection fraction. Eur J Heart Fail. 2016;18:103–12.
Doyon A, Haas P, Erdem S, et al. Impaired systolic and diastolic left ventricular function in children with chronic kidney disease: results from the 4C Study. Sci Rep. 2019;9:11462.
Mehta SK, Holliday C, Hayduk L, et al. Comparison of myocardial function in children with body mass indexes 25 versus those < 25 kg/m2. Am J Cardiol. 2004;93:1567–9.
Casagrande SS, Menke A, Linder B, Osganian SK, Cowie CC. Cardiovascular risk factors in adolescents with prediabetes. Diabet Med. 2018. https://doi.org/10.1111/dme.13661.
Procar-Almela M, Codoner-Franch P, Tuzon M, Navarro-Solera M, Carrasco-Luna J, Ferrando J. Left ventricular diastolic function and cardiometabolic factors in obese normotensive children. Nutr Metab Cardiovasc Dis. 2015;25:108–15.
Amin RS, Kimball TR, Kalra M, et al. Left ventricular function in children with sleep-disordered breathing. Am J Cardiol. 2005;95:801–4.
Hui W, Slorach C, Guerra V, et al. Effect of obstructive sleep apnea on cardiovascular function in obese youth. Am J Cardiol. 2019;123:341–7.
Seliem MA, Al-Saad HI, Bou-Holaaigah IH, Khan MN, Palileo MR. Left ventricular diastolic dysfunction in congenital chronic anemias during childhood as determined by comprehensive echocardiographic imaging including acoustic quantification. Eur J Echocardiogr. 2002;3:103–10.
Allen KY, Jones S, Jackson T, et al. Echocardiographic screening of cardiovascular status in pediatric sickle cell disease. Pediatric Cardiol. 2019;40:1670–8.
Lipshultz SE, Miller TL, Wilkinson JD, et al. Cardiac effects in perinatally HIV-infected and HIV-exposed but uninfected children and adolescents: a view from the United States of America. J Int AIDS Soc. 2013;16:18597.
Perez-Atayde AR, Kearney DI, Bricker JT, P2C2 HIV Study Group, et al. Cardiac, aortic, and pulmonary arteriopathy in HIV-infected children: the prospective P2C2 HIV multicenter study. Pediatr Dev Pathol. 2004;7:61–70.
Antony I, Kannichamy V, Banerjee A, Gandhi AB, Valaiyaduppu Subas S, Hamid P. An outlook on the impact of HIV infection and highly active antiretroviral therapy on the cardiovascular system: a review. Cureus. 2020;12: e11539.
Casaretti L, Paolillo S, Formisano R, et al. Metabolic and cardiovascular effects of combined antiretroviral therapy in patients with HIV infection: systematic review of literature. Monaldi Arch Chest Dis. 2011;76:175–82.
Nicol M, Baudet M, Cohen-Solal A. Subclinical left ventricular dysfunction during chemotherapy. Card Fail Rev. 2019;5:31–6.
Adams MJ, Lipsitz SR, Colan SD, et al. Cardiovascular status in long-term survivors of Hodgkin’s disease treated with chest radiotherapy. J Clin Oncol. 2004;22:3139–48.
Singh GK, Holland MR. Diastolic dysfunction in pediatric cardiac patients: evaluation and management. Curr Treat Options Cardiovasc Med. 2010;12:503–17.
Dragulescu A, Mertens L, Friedberg MK. Interpretation of left ventricular diastolic dysfunction in children with cardiomyopathy by echocardiography: problems and limitations. Circ Cardiovasc Imaging. 2013;6:254–61.
Eidem BW, McMahon CJ, Cohen RR, et al. Impact of cardiac growth on Doppler tissue imaging velocities: a study in healthy children. J Am Soc Echocardiogr. 2004;17:212–21.
Schmitz L, Xanthopoulos A, Koch H, Lange PE. Doppler flow parameters of left ventricular filling in infants: how long does it take for the maturation of the diastolic function in a normal left ventricle to occur? Pediatr Cardiol. 2004;25:482–91.
Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29:277–314.
Margossian R, Sleeper LA, Pearson GD, Pediatric Heart Network Investigators, et al. Assessment of diastolic function in single-ventricle patients after the Fontan procedure. J Am Soc Echocardiogr. 2016;29:1066–73.
McMohan CJ, Pignatelli RH, Naguesh SF, et al. Left ventricular non-compaction cardiomyopathy in children: characterization of clinical status using tissue Doppler-derived indices of left ventricular diastolic relaxation. Heart. 2007;93:676–81.
Niemann M, Liu D, Hu K, et al. Echocardiographic quantification of regional deformation helps to distinguish isolated left ventricular non-compaction from dilated cardiomyopathy. Eur J Heart Failure. 2012;14:155–61.
Nagueh SF, Lakkis NM, Middleton KJ, et al. Doppler estimation of left ventricular filling pressures in patients with hypertrophic cardiomyopathy. Circulation. 1999;99:254–61.
Geske JB, Sorajja P, Nishimura RA, et al. Evaluation of left ventricular filling pressures by Doppler echocardiography in patients with hypertrophic cardiomyopathy: correlation with direct left atrial pressure measurement at cardiac catheterization. Circulation. 2007;116:2702–8.
Haland TF, Edvardsen T. The role of echocardiography in management of hypertrophic cardiomyopathy. J Echocardiogr. 2020;8:77–85.
Ryan TD, Madueme PC, Jefferies JL, et al. Utility of echocardiography in the assessment of left ventricular diastolic function and restrictive physiology in children and young adults with restrictive cardiomyopathy: a comparative echocardiography-catheterization study. Pediatr Cardiol. 2017;38:381–9.
Butz T, Piper C, Langer C, et al. Diagnostic superiority of a combined assessment of the systolic and early diastolic mitral annular velocities by tissue Doppler imaging for the differentiation of restrictive cardiomyopathy from constrictive pericarditis. Clin Res Cardiol. 2010;99:207–15.
Afonso L, Kondur A, Simegn M, et al. Two- dimensional strain profiles in patients with physiological and pathological hypertrophy and preserved left ventricular systolic function: a comparative analyses. BMJ Open. 2012;2: e001390.
Margossian R, Schwartz ML, Prakash A, et al. Comparison of echocardiographic and cardiac magnetic resonance imaging measurements of functional single ventricular volumes, mass, and ejection fraction (from the Pediatric Heart Network Fontan Cross-Sectional Study). Am J Cardiol. 2009;104:419–28.
Chowdhury SM, Butts RJ, Hlavacek AM, et al. Echocardiographic detection of increased ventricular diastolic stiffness in pediatric heart transplant recipients: a pilot study. J Am Soc Echocardiogr. 2018;31:342-8.e1.
Matsubara D, Chang J, Kauffman HL, et al. Longitudinal assessment of cardiac outcomes of multisystem inflammatory syndrome in children associated with COVID-19 infections. J Am Heart Assoc. 2022;19: e023251.
Rihal CS, Nishimura RA, Hatle LK, et al. Systolic and diastolic dysfunction in patients with a clinical diagnosis of dilated cardiomyopathy: relation to symptoms and prognosis. Circulation. 1994;90:2772–9.
Dujardin KS, Tei C, Yeo T, et al. Prognostic value of a Doppler index combining systolic and diastolic performance in idiopathic dilated cardiomyopathy. Am J Cardiol. 1998;82:1071–6.
Eidem BW, McMohan CJ, Ayres NA. Impact of chronic left ventricular preload and afterload on Doppler tissue imaging velocities; a study in congenital heart disease. J Am Soc Echocardiogr. 2005;18:830–8.
Masutani S, Saiki H, Kurishima C, Ishido H, Tamura M, Senzaki H. Heart failure with preserved ejection fraction in children: hormonal imbalance between aldosterone and brain natriuretic peptide. Circ J. 2013;77:2375–82.
Andrade AC, Jerosch-Herold M, Wegner P, et al. Determinants of left ventricular dysfunction and remodeling in patients with corrected Tetralogy of Fallot. J Am Heart Assoc. 2019;8(17):e009618.48.
Klitsie LM, Hazekamp MG, Roest AA, et al. Tissue Doppler imaging detects impaired biventricular performance shortly after congenital heart defect surgery. Pediatr Cardiol. 2013;34:630–8.
Harada K, Tamura M, Yasuoka K, Toyono M, Takada G. A comparison of tissue Doppler imaging and velocities of transmitral flow in children with elevated left ventricular preload. Cardio Young. 2001;11:261–8.
Vassalos A, Lilley S, Young D, et al. Tissue Doppler imaging following pediatric cardiac surgery: early patterns of change and relationship to outcome. Interact Cardiovasc Thoracic Surg. 2009;9:173–7.
Panesar D, Burch M. Assessment of diastolic function in congenital heart disease. Front Cardiovasc Med. 2017;4:5.
Mawad W, Friedberg MK. The continuing challenges of evaluating diastolic function by echocardiography in children: developing concepts and newer modalities. Curr Opin Cardiol. 2017;32:93–100.
Schiattarella GG, Alcaide P, Condorelli G, et al. Immunometabolic mechanisms of heart failure with preserved ejection fraction. Nat Cardiovasc Res. 2022;1:211–22.
Lipshultz SE. Ventricular dysfunction clinical research in infants, children, and adolescents. Prog Pediatr Cardiol. 2000;12:1–28.
van Heerebeek L, Hamdani N, Falcao-Pires I, et al. Low myocardial protein kinase G activity in heart failure with preserved ejection fraction. Circulation. 2012;126:830–9.
Schiattarella GG, Altamirano F, Tong D, et al. Nitrosative stress drives heart failure with preserved ejection fraction. Nature. 2019;568:351–6.
Adeniran I, Maclver DH, Hancox JC, Zhang H. Abnormal calcium homeostasis in heart failure with preserved ejection fraction is related to reduced contractile function and incomplete relaxation: an electromechanically detailed biophysical modeling study. Front Physiol. 2015;6:78. https://doi.org/10.3389/fphys.2015.00078.
Peana D, Doeier TL. Cardiomyocyte Ca2+ homeostasis as a therapeutic target in heart failure with reduced and preserved ejection fraction. Curr Opin Pharmacol. 2017;33:17–26.
Selby DE, Palmer BM, LeWinter MM, Meyer M. Tachycardia-induced diastolic dysfunction and resting tone in myocardium from patients with a normal ejection fraction. J Am Coll Cardiol. 2011;58:147–54.
Price JF, Younan S, Cabrera AG, et al. Diuretic responsiveness and its prognostic significance in children with heart failure. J Cardiac Fail. 2019;25:941–7.
Weber KT, Brilla CG. Pathological hypertrophy and cardiac interstitium: fibrosis and renin-angiotensin-aldosterone system. Circulation. 1991;83:1849–65.
Silvestre JS, Heymes C, Oubénaissa A, et al. Role of cardiac aldosterone in post-infarction ventricular remodeling in rats. Arch Mal Coeur Vaiss. 1999;92:991–6.
Degre S, Detry JM, Unger P, Cosyns J, Brochet C, Kormos N. Effects of spironolactone-altizide on left ventricular hypertrophy. Acta Cardiol. 1998;53:261–7.
Edelmann F, Wachter R, Schmidt AG, et al. Effects of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection function: the Aldo-DHF randomized controlled trial. JAMA. 2013;309:781–91.
Böckmann I, Lischka J, Richter B, et al. FGF23-mediated activation of local RAAS promotes cardiac hypertrophy and fibrosis. Int J Mol Sci. 2019;20:4634.
Lu M, Qin Q, Yao J, Sun L, Qin X. Induction of LOX by TGF-beta1/Smad/AP-1 signaling aggravates rat myocardial fibrosis and heart failure. IUBMB Life. 2019;71:1729–39.
Brilla CG, Rupp H, Funck R, Maisch B. The renin-angiotensin-aldosterone system and myocardial collagen matrix remodeling in congestive heart failure. Eur Heart J. 1995;Suppl. O:107–9.
Ramirez Gil JF, Delcayre C, Robert V, et al. In vivo left ventricular function and collagen expression in aldosterone/salt-induced hypertension. J Cardiovasc Pharmacol. 1998;32:927–34.
Zhang WW, Zheng RH, Bai F, et al. Steroidogenic acute regulatory protein/aldosterone synthetase mediates angiotensin II-induced cardiac fibrosis and hypertrophy. Mol Biol Rep. 2020;47:1207–22.
Gang C, Qiang C, Xiangli C, Shifen P, Chong S, Lihong L. Puerarin suppresses angiotensin II-induced cardiac hypertrophy by inhibiting NADPH oxidase activation and oxidative stress-triggered AP-1 signaling pathways. J Pharm Sci. 2015;18:235–48.
Stas S, Whaley-Connell A, Habibi J, et al. Mineralocorticoid receptor blockade attenuates chronic overexpression of the renin–angiotensin–aldosterone system stimulation of reduced nicotinamide adenine dinucleotide phosphate oxidase and cardiac remodeling. Endocrinology. 2007;148:3773–80.
Brunner-La Rocca HP, Vaddadi G, Esler MD. Recent insight into therapy of congestive heart failure: focus on ACE inhibition and angiotensin-II antagonism. J Am Coll Cardiol. 1999;33:1163–73.
Brilla CG, Maisch B, Rupp H, Funck R, Zhou G, Weber KT. Pharmacological modulation of cardiac fibroblast function. Herz. 1995;20:127–34.
Chrysant SG. Vascular remodeling: the role of angiotensin-converting enzyme inhibitors. Am Heart J. 1998;135:S21-30.
Saha SA, Molnar J, Arora RR. Tissue ACE inhibitors for secondary prevention of cardiovascular disease in patients with preserved left ventricular function: a pooled meta-analysis of randomized placebo-controlled trials. J Cardiovasc Pharmacol Ther. 2007;12:192–204.
Hsu DT, Zak V, Mahony L, Pediatric Heart Network Investigators, et al. Enalapril in infants with single ventricle: results of a multicenter randomized trial. Circulation. 2010;122:333–40.
Giardini A, Formigari R, Bronzetti G, et al. Modulation of neurohormonal activity after treatment of children in heart failure with carvedilol. Cardiol Young. 2003;13:333–6.
Miyamoto SD, Stauffer BL, Nakano S, et al. Beta-adrenergic adaptation in paediatric idiopathic dilated cardiomyopathy. Eur Heart J. 2014;35:33–41.
Mamidi R, Li J, Doh CY, et al. Impact of the myosin modulator mavacamten on force generation and cross-bridge behavior in a murine model of hypercontractility. J Am Heart Assoc. 2018;7(17): e009627.
del Rio CL, Ueyama Y, Baker DC, et al. In vivo cardiac effects of mavacamten (MYK-461): evidence for negative inotropy and improved compliance. Circulation. 2017;136(Suppl. 1):A20593.
Setaro JF, Zaret BL, Schulman DS, Black HR, Soufer R. Usefulness of verapamil for congestive heart failure associated with abnormal left ventricular diastolic filling and normal left ventricular systolic performance. Am J Cardiol. 1990;66:981–6.
Betocchi S, Chiariello M. Effects of calcium antagonists on left ventricular structure and function. J Hypertens Suppl. 1993;11:S33–7.
Iliceto S. Left ventricular dysfunction: which role for calcium antagonists? Eur Heart J. 1997;18 Suppl. A:A87-91.
Hoffman TM, Wernovsky G, Atz AM, et al. Efficacy and safety of milrinone in preventing low cardiac output syndrome in infants and children after corrective surgery for congenital heart disease. Circulation. 2003;107:996–1002.
Price JF, et al. Outpatient continuous parenteral inotropic therapy as bridge to transplantation in children with advanced heart failure. J Card Fail. 2006;12(2):139–43.
Rossano JW, Cabrera AG, Jefferies JL, Naim M, Humlicek T. Pediatric cardiac intensive care society 2014 consensus statement: pharmacotherapies in cardiac critical care chronic heart failure. Pediatr Crit Care Med. 2016;17:S20-34.
Lechner E, Hofer A, Leitner-Pender G, et al. Levosimendan versus milrinone in neonates and infants after corrective open-heart surgery: a pilot study. Ped Crit Care Med. 2012;13:542–8.
Wang A, Cui C, Fan Y, et al. Prophylactic use of levosimendan in pediatric patients undergoing cardiac surgery: a prospective randomized controlled trial. Crit Care. 2019;23:428.
Namachivayam P, Crossland DS, Butt WW, Shekherdemian LS. Early experience with levosimendan in children with ventricular dysfunction. Pediatr Crit Care Med. 2006;7:445–8.
Egan JE, Clarke AJB, Williams S, et al. Levosimendan for low cardiac output: a pediatric experience. J Intensive Care Med. 2006;21:183–7.
Bayes-Genis A, Barallat J, Richards AM. A test in context: neprilysin: function, inhibition, and biomarker. J Am Coll Cardiol. 2016;68:639–53.
Gori M, D’Elia E, Senni M. Sacubitril/valsartan therapeutic strategy in HFpEF: clinical insights and perspectives. Int J Cardiol. 2019;281:158–65.
Vaduganathan M, Claggett BL, Desai AS, et al. Prior heart failure hospitalization, clinical outcomes, and response to sacubitril/valsartan compared with valsartan in HFpEF. J Am Coll Cardiol. 2020;75:245–54.
Cunningham JW, Claggett BL, O’Meara E, Prescott MF, Pfeffer MA, Shah SJ, et al. Effect of sacubitril/valsartan on biomarkers of extracellular matrix regulation in patients with HFpEF. J Am Coll Cardiol. 2020;76:503–14.
Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, et al. Angiotensin–neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381:1609–20.
FDA approves Entresto for pediatric heart failure patients. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/207620s013lbl.pdf. Accessed 13 Oct 2021.
McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008.
Packer M, Anker SD, Butler J, et al. Effect of empagliflozin on the clinical stability of patients with heart failure and reduced ejection fraction: the EMPEROR-reduced trial. Circulation. 2021;143:326–36.
Januzzi JL Jr, Ibrahim NE. Understanding the mechanistic benefit of heart failure drugs matters. J Am Coll Cardiol. 2020;76:2752–4.
Omar M, Jensen J, Frederiksen PH, et al. Effect of empagliflozin on hemodynamics in patients with heart failure and reduced ejection fraction. J Am Coll Cardiol. 2020;76:2740–51.
Lee MT, George J, Shahab H, Hermel M, Rana JS, Virani SS. Highlights of cardiovascular disease studies presented at the 2021 American Heart Association Scientific Sessions. Curr Atheroscler Rep. 2022;24:1–12. https://doi.org/10.1007/s11883-022-00985-0.
Iborra-Egea O, Santiago-Vacas E, Yurista SR, et al. Unraveling the molecular mechanism of action of empagliflozin in heart failure with reduced ejection fraction with or without diabetes. JACC Basic Transl Sci. 2019;4:831–40.
Nassif ME, Kosiborod M. Effects of sodium-glucose cotransporter type 2 inhibitors on heart failure. Diabetes Obes Metab. 2019;Suppl. 2:19–23.
Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. 2013;62:263–71.
Takimoto E, Belardi D, Tocchetti C, et al. Compartmentalization of cardiac beta-adrenergic inotropy modulation by phosphodiesterase type 5. Circulation. 2007;115:2159–67.
Redfield MM, Chen HH, Borlaug BA, et al. Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: a randomized clinical trial. (RELAX) trial: rationale and design. JAMA. 2013;309:1268–77.
Borbely A, van der Velden J, Papp Z, et al. Cardiomyocyte stiffness in diastolic heart failure. Circulation. 2005;111:774–81.
Rochette L, Lorin J, Zeller M, et al. Nitric oxide synthase inhibition and oxidative stress in cardiovascular diseases: possible therapeutic targets? Pharmacol Ther. 2013;140:239–57.
Jeong EM, Monasky MM, Gu L, et al. Tetrahydrobiopterin improves diastolic dysfunction by reversing changes on myofilament properties. J Mol Cell Cardiol. 2013;56:44–54.
Alkaitis MS, Crabtree MJ. Recoupling the cardia nitric oxide synthases: tetrahydrobiopterin synthesis and recycling. Curr Heart Fail Rep. 2012;9:200–10.
Follmann M, Ackerstaff J, Redlich G, et al. Discovery of the soluble guanylate cyclase stimulator vericiguat (BAY 1021189) for the treatment of chronic heart failure. J Med Chem. 2017;60:5146–61.
De Angelis A, Cappetta D, Piegari E, et al. Long-term administration of ranolazine attenuates diastolic dysfunction and adverse myocardial remodeling in a model of heart failure with preserved ejection fraction. Int J Cardiol. 2016;217:69–79.
Lovelock JD, Monasky MM, Jeong EM, et al. Ranolazine improves cardiac diastolic dysfunction through modulation of myofilament calcium sensitivity. Circ Reas. 2012;110:841–50.
Maier LS, Layug B, Karwatowska-Prokopczuk E, et al. Ranolazine for the treatment of diastolic heart failure in patients with preserved ejection fraction: the RALI-DHF proof-of-concept study. JACC Heart Fail. 2013;1:115–22.
Lipshultz SE, Messiah SE, Miller TL. (Editors). Pediatric metabolic syndrome: comprehensive clinical review and related health issues. Springer-Verlag London Ltd., London, 2012; p. 1–378
Antoniades C, Bakogiannis C, Leeson P, et al. Rapid, direct effects of statin treatment on arterial redox state and nitric oxide bioavailability in human atherosclerosis via tetrahydrobiopterin-mediated endothelial nitric oxide synthase coupling. Circulation. 2011;124:335–45.
Nochioka K, Sakata Y, Miyata S, et al. Prognostic impact of statin use in patients with heart failure and preserved ejection fraction: a report from the CHART-2 study. Circ J. 2015;79:574–658.
Marume K, Takashio S, Nagai T, et al. Effect of statins on mortality in heart failure with preserved ejection fraction without coronary artery disease: report from the JASPER Study. Circ J. 2019;83:357–67.
Oikawa T, Sakata Y, Nochioka K, et al. Prognostic impact of statin intensity in heart failure patients with ischemic heart disease: a report from the CHART-2 Study. J Am Heart Assoc. 2018;7: e007524.
de Ferranti SD, Steinberger J, Ameduri R, et al. Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association. Circulation. 2019;139:e603–4.
Aoki T. Failure with preserved ejection fraction (HFpEF) patients: HFpEF as a manifestation of systemic disease. Circ J. 2019;83:277–8.
Graziani F, Lillo R, Crea F. Rationale for the use of pirfenidone in heart failure with preserved ejection fraction. Front Cardiovasc Med. 2021;8: 678530.
Van Tassell BW, Arena R, Biondi-Zoccai G, et al. Effects of interleukin-1 blockade with anakinra on aerobic exercise capacity in patients with heart failure and preserved ejection fraction (from the D-HART pilot study). Am J Cardiol. 2014;113:321–7.
Rosalia L, Ozturk C, Shoar S, et al. Device-based solutions to improve cardiac physiology and hemodynamics in heart failure with preserved ejection fraction. JACC Basic Transl Sci. 2021;6(9–10):772–95. https://doi.org/10.1016/j.jacbts.2021.06.002.
Burkoff D, Maurer MS, Joseph SM, et al. Left atrial decompression pump for severe heart failure with preserved ejection fraction. JACC Heart Fail. 2015;3:275–82.
Søndergaard L, Reddy V, Kaye D, et al. Transcatheter treatment of heart failure with preserved or mildly reduced ejection fraction using a novel interatrial implant to lower left atrial pressure. Eur J Heart Fail. 2014;16:796–801.
Hasenfuß G, Hayward C, Burkhoff D, REDUCE LAP-HF Study Investigators, et al. A transcatheter intracardiac shunt device for heart failure with preserved ejection fraction (REDUCE LAP-HF): a multicentre, open-label, single-arm, phase 1 trial. Lancet. 2016;387:1298–304.
Emani S, Burkhoff D, Lilly SM. Interatrial shunt devices for the treatment of heart failure. Trends Cardiovasc Med. 2021;31:427–32.
Feldman T, Mauri L, Kahwash R, et al. Age- and gender-related ventricular-vascular stiffening: a community-based study. Circulation. 2005;112:2254–62.
Kaye DM, Hasenfuß G, Neuzil P, et al. One-year outcomes after transcatheter insertion of an interatrial shunt device for the management of heart failure with preserved ejection fraction. Circ Heart Fail. 2016;9: e003662.
Shah SJ, Feldman T, Ricciardi MJ, et al. One-year safety and clinical outcomes of a transcatheter interatrial shunt device for the treatment of heart failure with preserved ejection fraction in the reduce elevated left atrial pressure in patients with heart failure (REDUCE LAP-HF I) trial: a randomized clinical trial. JAMA Cardiol. 2018;3:968–77.
Gupta A, Bailey SR. Update on devices for diastolic dysfunction: options for a no option condition? Curr Cardiol Rep. 2018;20:85. https://doi.org/10.1007/s11886-018-1027-2.
Adamson PB, Abraham WT, Bourge RC, et al. Wireless pulmonary artery pressure monitoring guides management to reduce decompensation in heart failure with preserved ejection fraction. Circ Heart Fail. 2014;7:935–44.
Abraham WT, Stevenson LW, Bourge RC, Lindenfeld JA, Bauman JG, Adamson PB, CHAMPION Trial Study Group. Sustained efficacy of pulmonary artery pressure to guide adjustment of chronic heart failure therapy: complete follow-up results from the CHAMPION randomized trial. Lancet. 2016;387:453–61.
Vardas PE, Auricchio A, Blanc JJ, et al. Guidelines for cardiac pacing and cardiac resynchronization therapy. The Task Force for Cardiac Pacing and Cardiac Resynchronization Therapy of the European Society of Cardiology. Developed in collaboration with the European Heart Rhythm Association. Europace. 2007;9:959–98.
Penicka M, Bartunek J, Trakalova H, et al. Cardiac resynchronization therapy for the causal treatment of heart failure with preserved ejection fraction: insight from a pressure-volume loop analysis. Eur J Heart Fail. 2010;12:634–6.
Morris DA, Vaz Perez A, Blaschke F, Eichstadt H, Ozcelik C, Haverkamp W. Myocardial systolic and diastolic consequences of left ventricular mechanical dyssynchrony in heart failure with normal left ventricular ejection fraction. Eur Heart J Cardiovasc Imaging. 2012;13:556–67.
Tschöpe C, Kherad B, Klein O, et al. Cardiac contractility modulation: mechanisms of action in heart failure with reduced ejection fraction and beyond. Eur J Heart Fail. 2019;21:14–22.
Feld Y, Dubi S, Reisner Y, et al. Energy transfer from systole to diastole: a novel device-based approach for the treatment of diastolic heart failure. Acute Card Care. 2011;13:232–42.
Corolla® TAA for heart failure with preserved ejection fraction (HFpEF) and diastolic dysfunction (DD). October 8, 2020. ClinicalTrials.gov identifier: NCT02499601. https://clinicaltrials.gov/ct2/show/NCT02499601. Accessed 18 Oct 2021.
Brandt MC, Mahfoud F, Reda S, et al. Renal sympathetic denervation reduces left ventricular hypertrophy and improves cardiac function in patients with resistant hypertension. J Am Coll Cardiol. 2012;59:901–9.
Mahfoud F, Urban D, Teller D, et al. effect of renal denervation on left ventricular mass and function in patients with resistant hypertension: data from a multicentre cardiovascular magnetic resonance imaging trial. Eur Heart J. 2014;35:2224–31.
Schirmer SH, Sayed MMYA, Reil J-C, et al. Atrial remodeling following catheter-based renal denervation occurs in a blood pressure and heart rate-independent manner. JACC Cardiovasc Interv. 2015;8:972–80.
Patel HC, Rosen SD, Hayward C, et al. Renal denervation in heart failure with preserved ejection fraction (RDT-PEF): a randomized controlled trial. Eur J Heart Fail. 2016;18:703–12.
Granegger M, Dave H, Knirsch W, Thasmen B, Schweiger M, Hobler M. A valveless pulsatile pump for the treatment of heart failure with preserved ejection fraction: a simulation study. Cardiovasc Eng Techn. 2019;10:69–79.
Landesberg A, Shenhav A, Shofty R, et al. Effects of synchronized cardiac assist device on cardiac energetics. Ann N Y Acad Sci. 2006;1080:466–78.
Tate CA, Helgason T, Hyek MF, et al. SERCA2a and mitochondrial cytochrome oxidase expression are increased in the hearts of exercise-trained old rats. Am J Physiol. 1996;271:H68-72.
Schmidt U, del Monte F, Miyamoto MI, et al. Restoration of diastolic function in senescent rat hearts through adenoviral gene transfer of sarcoplasmic reticulum Ca2+-ATPase. Circulation. 2000;101:790–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this article.
Conflict of interest/competing interests
Bibhuti Das has no potential conflicts of interest that might be relevant to the contents of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for Publication
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
BBD conceptualized, wrote, and revised this article.
Rights and permissions
About this article
Cite this article
Das, B.B. Therapeutic Approaches in Heart Failure with Preserved Ejection Fraction (HFpEF) in Children: Present and Future. Pediatr Drugs 24, 235–246 (2022). https://doi.org/10.1007/s40272-022-00508-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-022-00508-z