Abstract
Summary
We surveyed primary care physicians in Malaysia for their knowledge, attitude and practice in screening and managing osteoporosis. We found a low level of screening and active management of osteoporosis in the primary care setting despite positive attitudes towards them. We advocate for the active management of osteoporosis at the primary care level.
Introduction
Prevention of osteoporotic fracture is important in primary healthcare for healthy ageing. Little is known about the knowledge, attitude, practice and barriers in the screening and managing osteoporosis among primary care doctors.
Methods
A cross-sectional study, using an online pre-tested questionnaire after face and content validation, was conducted for primary care doctors from 1 June to 30 July 2021 across Malaysia. Pearson’s chi-square test and logistic regression were employed.
Results
A total of 350 primary care doctors in Malaysia, consisting of 113 (32.3%) family medicine specialists (FMS) and 237 (67.7%) medical officers, participated in this study. The mean ± SD score of osteoporosis knowledge was 50.46 ± 15.09 with minimum and maximum values of 0 and 83.64%, respectively. One hundred and ten (31.4%) respondents achieved a satisfactory overall knowledge score of ≥ 60%, 156 (44.6%) were confident in advising patients for initiation of anti-osteoporotic medication, and 243 (69.4%) perceived that bisphosphonate should be made available in health clinics. Only 97 (27.7%) practised osteoporosis screening. Inaccessibility of bone mineral densitometry (BMD) (90.6%), inadequate knowledge (87.7%) and inaccessibility of pharmacotherapy (87.1%) are perceived modifiable barriers to osteoporosis screening and management. Factors associated with a satisfactory knowledge of osteoporosis are designation as a family medicine specialist (AOR 3.034, p = 0.002), attendance at an osteoporosis management update course (AOR 2.095, p = 0.034) and the practice of osteoporosis screening for the elderly (AOR 2.767, p = 0.001).
Conclusion
Given the insufficient knowledge and low level of osteoporosis screening, there is a need for a national structured health programme to address the knowledge gap, increase screening practices and enhance accessibility to BMD and anti-osteoporosis medication in primary care.
Similar content being viewed by others
Introduction
Osteoporosis is characterised by low bone mass and micro-architectural deterioration of bone tissue, resulting in bone fragility and fracture [1]. It is estimated that about one-in-three women and one in five men above the age of 50 years old will suffer from an osteoporotic fracture in their lifetime [2]. Hip fragility fractures are a major health problem related to osteoporosis and are associated with significant mortality and morbidity [3, 4]. While declining hip fracture rates were observed in North America, Oceania and Europe, increasing rates of hip fractures are seen in the Asian region, likely due to the ageing population and increasing urbanisation [5, 6]. Asia is projected to bear half of the global burden for hip fractures by 2050 [5, 7]. In Malaysia, the hip fracture rates in both sexes are expected to increase 3.55-fold in 2050, from an estimated 5,880 hip fractures in 2018 to 20,893 in 2050 [6]. The direct costs of treatment are likewise projected to increase, from 35.3 million USD to 125.4 million USD by 2050 [6]. This projected increase in hip fractures in Malaysia is the highest among countries in Asia [6].
Effective treatment options are available to prevent fragility fractures in patients with osteoporosis, but there is evidence that osteoporosis is underdiagnosed and undertreated worldwide, including in Asia [8, 9]. Likewise in Malaysia, a similar trend of underdiagnosis of osteoporosis is seen [10], and an osteoporosis treatment gap has been observed in secondary fracture prevention in both public and private settings [11, 12].
In Malaysia, osteoporosis is managed by both primary care doctors and specialists from various disciplines such as endocrinology, rheumatology and orthopaedic surgery. Physicians such as endocrinologists and orthopaedic surgeons routinely initiate medical treatment for osteoporosis, while primary care doctors play an important role in detecting cases of osteoporosis, managing them and referring complicated cases such as secondary osteoporosis to specialists. In the Malaysian Ministry of Health setting, the prescription of drugs is categorised into a few prescriber categories where certain medications can only be prescribed by a specialist or consultant. Drugs under category A can only be prescribed by specialists or consultants in the hospital setting. Family medicine specialists (FMS) can only prescribe drugs under category A/KK and below. At the time of the study, medication for osteoporosis is not readily available for prescription in public primary care clinics despite the primary care doctor being well-positioned to screen for, treat and continue osteoporosis care in their setting.
At present, limited information is available on osteoporosis knowledge, attitude and practice (KAP) of Malaysian primary care doctors. KAP surveys of osteoporosis done among primary care practitioners in other countries have helped identify gaps that could be acted upon to improve osteoporosis care [13, 14]. This study aimed to address the current knowledge and practice gap by assessing the KAP and barriers to osteoporosis screening and management among primary care doctors across Malaysia. Understanding the gaps and issues would help us formulate recommendations for policymakers to prioritise osteoporosis care in primary care settings.
Methods
Study design
This was a cross-sectional study conducted from 1 June to 30 July 2021 involving FMS and medical officers (MOs) working at public health clinics across all the states in Malaysia.
Study instrument
A self-administered online questionnaire available in Google Forms was used in this study. The questionnaire on knowledge for the present study was a modification of a published questionnaire of a related study [13]. The questionnaire consisted of 4 sections: the first section was on sociodemographic information including age, gender, designation, years of practice, the estimated total number of elderly patients (workload)/week in the clinic, availability of bone mineral densitometry (BMD), sources of information for osteoporosis and the last time participants attended an update on osteoporosis management. The second section was on knowledge about osteoporosis and encompassed 10 domains, namely: definition of osteoporosis, risk of osteoporotic fractures, investigations of osteoporosis, daily required dose of vitamin D and calcium supplements, pharmacotherapy for osteoporosis in patients with an eGFR < 30 mL/min/1.73 m2, pharmacotherapy for osteoporotic hip fracture risk reduction, complications of osteoporosis treatment, indications for osteoporosis treatment in the absence of BMD testing, duration of oral bisphosphonate treatment and osteoporosis treatment failure. The third section was on attitude towards osteoporosis as a health issue, its assessment and management. Participants were asked to grade their extent of agreement on each item (assessment for attitude) by using a 3-point Likert scale: agree, neutral or disagree. The fourth section was on the practice of osteoporosis screening and management for osteoporotic fracture risk reduction and the perceived barriers to this practice.
The questionnaire underwent face and content validation based on a conceptual framework. Two geriatricians, two endocrinologists and two family medicine specialists were involved in the content validation processes. The questionnaire was pre-tested among five MOs at a government health clinic to assess the items, flow and ease of understanding the questionnaire.
Sample size
The sample size calculation was done using the single proportion formula, using the Sample Size Calculator for Prevalence Studies (Naing et al., 2006). Based on a study by Fogelman et al., the median percentage of correct responses in the knowledge of osteoporosis was 23% [13]. After taking into account a non-respondent rate of 26% and a precision of 5%, the sample size required was 344 participants [13]. Finally, 350 participants were recruited for our study.
Sampling method
Google Forms links were disseminated to the common FMS groups through WhatsApp, a communication application widely used in Malaysia through the smartphone. The FMS were invited to participate in the research, and the Google Forms link was disseminated to the MOs at each health clinic through their FMS. The participants declared their consent before answering the online questionnaire.
Ethics approval
Ethics approval was obtained from the Medical Research and Ethics Committee (reference no. NMRR-21–421-58735), Ministry of Health, Malaysia. All procedures performed in studies involving human participants were performed according to the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Data analysis
All data collected were analysed using Statistical Package for the Social Sciences (SPSS) version 21. There was no missing value in the data collection. Data were checked for outliers or missing data. Continuous data were checked for normality by looking at the Kolmogorov–Smirnov test. Categorical data were reported in proportions (percentage) while continuous data were reported as medians with interquartile range (IQR) if the distribution was skewed.
Questions on knowledge items answered correctly were given 1 point and questions answered incorrectly were given 0 points. The total point range was 0–55, with the scores being reported in percentages. Conversion of points into percentages was done for the overall test by dividing the score by the total points possible. We categorised the knowledge level using Bloom’s cut-off point [15]. The knowledge level was deemed low if the score was less than 60%. Those with moderate (60–79%) and high (80–100%) scores were deemed as having satisfactory knowledge levels. The reliability of the knowledge, attitude and practice questionnaires was checked and the values of Cronbach’s alpha were 0.899, 0.752 and 0.722, respectively, indicating acceptable internal consistency reliability.
Pearson chi-square test was used to determine the association between basic sociodemographic data with knowledge scores. For multiple logistic regression, variables with a p value of < 0.25 from univariate analyses were included. Adjusted odds ratio (AOR) and 95% confidence interval (CI) were presented. Significance is set at the α level of 0.05.
Results
Profile and working experience of the study participants (Table 1 )
A total of 350 primary care doctors in Malaysia, consisting of 113 (32.3%) FMS and 237 (67.7%) MOs, participated in this study. Among the doctors, a total of 73 (20.9%) obtained a master’s degree in family medicine, 46 (13.1%) obtained a diploma in family medicine while 191 (54.6%) did not pursue any further training in family medicine. Two hundred and fifty-eight (73.7%) were female. The median age was 35 years old and the median years of practice after graduating was 10 years.
The median number of older patients ≥ 65 years old seen in a week was 30. The Clinical Practice Guideline (CPG) Malaysia for Osteoporosis was used by 299 (85.4%) respondents as the information source for the management of osteoporosis. One hundred and five respondents (30.0%) had attended an update on the management of osteoporosis within the previous 2 to 5 years while 97 (27.7%) have never attended any updates on osteoporosis management. Only 33 (9.4%) had additional training in the management of osteoporosis through attachments with geriatricians, rheumatologists, endocrinologists or orthopaedic surgeons who manage osteoporosis (Table 1).
Knowledge of osteoporosis screening and management (Table 2 )
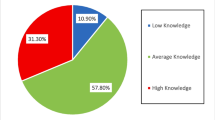
The mean percentage score (± SD) of osteoporosis knowledge among the doctors was 50.46% (± 15.09), with minimum and maximum values of 0 and 83.64%, respectively. Only 110 (31.4%) participants achieved a satisfactory knowledge score of ≥ 60%, while 240 (68.6%) participants obtained a low score of < 60%.
More than half of the respondents obtained a satisfactory score on only four out of the ten domains, namely: risk of osteoporotic fractures, investigations of osteoporosis, indications for osteoporosis treatment in the absence of BMD testing and treatment failure in osteoporosis. The highest number of respondents, at 241 participants (68.9%), achieved satisfactory knowledge scores on investigations of osteoporosis. Respondents scored poorly in domains related to pharmacotherapy: 321 (91.7%) participants scored poorly in the domain of pharmacotherapy for reduction of osteoporotic hip fracture risk, 297 (84.9%) on complications associated with osteoporosis treatment, 287 (82.0%) on pharmacotherapy of an osteoporotic person with an eGFR < 30 mL/min/1.73 m2 and 285 (81.4%) on the duration of oral bisphosphonate treatment.
Attitude on osteoporosis screening and management (Table 3 )
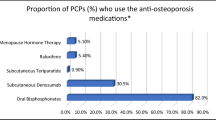
Three hundred and forty-four (98.3%) participants perceived that osteoporosis is an important health issue, 335 (95.7%) felt that osteoporosis screening is beneficial for patients who are ≥ 65 years, 323 (92.3%) felt that BMD should be easily accessible to primary care doctors and 178 (50.9%) were confident in their BMD result interpretation. A total of 280 (80.0%) perceived that all patients with osteoporosis should be offered pharmacotherapy while only 180 (51.4%) participants had confidence in providing non-pharmacotherapy to prevent osteoporosis. Most respondents (243 participants, 64.9%) think that the FMS should be allowed to prescribe bisphosphonates in the clinic and that the prescription should not be limited to hospital specialists. Despite that, only 156 (44.6%) were confident in advising patients for initiation of anti-osteoporotic pharmacotherapy.
Practice of osteoporosis screening and management
Only 97 (27.7%) claimed that they practised osteoporosis screening for the elderly in their clinics. The commonest screening tool used was Fracture Risk Assessment Tool (FRAX) [30 (8.6%)], followed by FRAX/BMD in 19 (5.4%), Osteoporosis Self-Assessment Tool (OSTA)/FRAX in 19 (5.4%), BMD in 12 (3.4%) and OSTA in 12 (3.4%) (Table 1).
There were 158 (45.1%) participants who did not have access to BMD in their district, while 103 (29.4%) participants were allowed direct BMD access in the radiology department in the hospital or health clinic without a referral to the medical or orthopaedic clinic first. Fifty-seven (16.3%) responded that BMD is available at a nearby private hospital and 32 (9.1%) indicated the need for referral to the medical or orthopaedic clinic to get BMD access. Only 63 (18.0%) participants offered BMD to their patients within the past 1 year (Table 1).
A total of 195 (55.7%) participants often or always advised patients for weight-bearing exercise, 301 (86%) often or always advised patients on fall prevention, and 197 (56.3%) often or always advised patients to limit caffeinated drinks intake to less than 1–2 (240–360 ml in each serving) servings per day to reduce fracture risk. There were 167 (47.7%) participants who often or always prescribe calcium supplements only, while 193 (55.2%) never or seldom prescribe calcium with vitamin D supplements and 212 (60.5%) never or seldom refer to a medical or orthopaedic specialist for anti-osteoporotic medications (Table 3).
The barriers to osteoporosis screening and management (Fig. 1 )
A total of 317 (90.6%) participants perceived that the inaccessibility of BMD in the district is the commonest barrier to osteoporosis screening and management in the primary care clinic. Three-hundred and seven (87.7%) felt that inadequate knowledge and patients’ coexisting multiple medical conditions that need more priority were the barriers, 305 (87.1%) felt that the barrier was the inaccessibility of pharmacotherapy at primary care clinics, and 297 (84.9%) felt that lack of doctor-patient time had hindered the screening and management of osteoporosis.
Association between participants’ profile and knowledge level (Table 4 )
There was a significant association between a satisfactory knowledge score among the participants and the following items: designation as an FMS (p < 0.001), additional training in the management of osteoporosis (p < 0.001), prior attendance to an osteoporosis management update course (p < 0.001), years of practice (p < 0.001), the use of the osteoporosis CPG (p = 0.022), offering BMD in clinical practice (p = 0.014) and experience of screening of osteoporosis in the older person in clinical practice (p < 0.001). After using multiple logistic regression, three factors were found to predict satisfactory knowledge in osteoporosis management: designation as FMS (AOR 3.034, CI 1.517–6.068; p = 0.002), prior attendance in an update on the management of osteoporosis (AOR 2.095, CI 1.057–4.154; p = 0.034) and practice of osteoporosis screening for the elderly (AOR 2.767, CI 1.524–5.024; p = 0.001).
Discussion
Key findings from our study were as follows: (a) the mean knowledge score was 50.46% out of a maximum score of 100%; (b) participants scored poorly in questions on pharmacotherapy; (c) most participants agreed that osteoporosis is an important health issue and screening for it is beneficial in older person; (d) only 27.7% of participants practised osteoporosis screening; (e) only 29.4% of our participants had direct access to BMD service; (f) approximately half of the participants were confident in interpreting BMD result and providing non-pharmacological prevention advice for osteoporosis and (g) less than half of the participants were confident in advising patients for initiation of anti-osteoporotic pharmacotherapy.
It is premature to conclude whether the knowledge level of osteoporosis among our primary care doctors was satisfactory or not as we did not undergo the full validation of scoring for our questionnaire. However, our overall findings suggest that the knowledge level of osteoporosis among our doctors is lacking. Globally, studies had shown knowledge of osteoporosis was inadequate among primary care doctors [16,17,18,19,20]. While our participants showed satisfactory knowledge level in domains on the risk of osteoporotic fractures and investigations of osteoporosis, most of them did not score satisfactorily in questions on pharmacotherapy, specifically on pharmacotherapy for an osteoporotic person with reduced kidney function, pharmacotherapy that effectively reduce the risk of osteoporotic hip fracture, their associated complications and duration of use for oral bisphosphonate. Our findings are consistent with studies elsewhere which showed a gap of knowledge in pharmacotherapy for osteoporosis among primary care doctors [18, 20, 21]. This knowledge gap would explain why only 44.6% of our participants were confident in advising patients on the initiation of anti-osteoporotic pharmacotherapy. Medication for osteoporosis is only readily available in hospitals under prescription category A, contributing to the lack of familiarity, knowledge and confidence in this area [22]. Thus, the majority perceived the need of downgrading bisphosphonate category prescriber from the current category A (can be prescribed only by hospital specialist) to A/KK (can be prescribed by FMS in the primary care setting).
Most participants agreed that osteoporosis is an important health issue and screening for it is beneficial in the older person. However, this sentiment is not reflected in actual practice as only 27.7% of our participants performed screening for osteoporosis. Among those who screened, FRAX was the preferred tool followed by OSTA. Only 29.4% of our participants had direct access to BMD, thus explaining why BMD is not the preferred screening tool. Again, this would probably explain why only approximately 50.9% of our participants were confident in interpreting BMD results. Even in those who had access to BMD, only 18% offered BMD to their patients. Lack of access to BMD in the primary care setting is not a new problem [19]. Malaysia is underresourced and has an inadequate number of BMD machines, providing only 2.5 BMD machines per one million of the population [2]. Previous studies had reported that only about 27% of primary care doctors had access to BMD, almost similar to our figure of 29.4%. In a study in the USA, the main barriers to prescribing a BMD test were the perception that patients could be treated without BMD testing, and that patients were too old or frail for testing [23]. It is interesting to note that the uptake of BMD screening in Australia had been poor for the older person in primary care settings despite government reimbursement, suggesting that a simplified screening process for primary care settings may be warranted [24].
In our study, FRAX was the preferred screening modality (8.6%), likely owing to its ease of use without the need for BMD. Concerning the use of FRAX and OSTA, a study in the neighbouring country, Singapore had shown that FRAX and OSTA performed almost similarly in identifying osteoporosis with FRAX having a role in screening the postmenopausal woman [25]. It is worth pointing out that while Malaysia and Singapore share almost similar multi-ethnic demographics; the difference is in the ethnic proportion. The highest ethnic proportion in Singapore is the Chinese population (74.2%), while in Malaysia Bumiputera including the Malay population (approximately 70%) is the majority [26, 27]. OSTA was found to be unsuitable to identify osteoporosis among postmenopausal women in a Malaysian study [28]. However, we need to be cautious in promoting FRAX alone as the screening modality for osteoporosis as it may or may not be cost-effective to screen with FRAX, depending on the setting [29, 30]. We do not have any local cost-effectiveness data on the screening modalities for osteoporosis.
The low percentage of osteoporosis screening in our study is a concern because primary care doctors are in the best position to screen for osteoporosis and to treat it accordingly as disease prevention and screening are part of the principle of primary care medicine. Studies worldwide had pointed out that osteoporosis was generally less prioritised by primary care doctors compared to other chronic diseases such as diabetes mellitus and hypertension [18, 31]. Awareness of the importance of recognising osteoporosis does not seem to be the issue as reflected in our study. A previous Malaysian study had shown that awareness of osteoporosis did not correlate with the tendency to treat [32]. We believe the same trend still prevails and the reasons could be multifactorial as demonstrated in our study: limited access to BMD and medication, lack of doctor-patient time, patients’ coexisting multiple medical conditions that need more priority and inadequate knowledge [23]. Primary care doctors were more likely to treat osteoporosis among those aged < 65 years, female and independent in their activities of daily living, taking into consideration of the safety and efficacy of anti-osteoporotic medications [23]. From a pragmatic point of view, while immediate improvements to increase access to BMD and medication may not be possible, strengthening the non-pharmacological intervention to prevent osteoporosis is something that primary care doctors can strive for. Only 51.4% of our participants were confident in providing non-pharmacotherapy to prevent osteoporosis. This is one area that we can improve on.
The issues that we identified in this study such as lack of screening practice among primary care doctors, limited access to BMD and unavailability of anti-osteoporotic medication in primary care are rudimentary. However, these issues have to be tackled before we even consider the more complex issues surrounding the management of osteoporosis. They also underscore the importance of a structured programme at the national level to promote better osteoporosis care. In Malaysia, osteoporosis is not yet prioritised as a national health agenda, more so in primary care. We advocate a national structured screening programme in primary care which is supported by better access to bone measurement tests (such as BMD) and anti-osteoporotic medication. Further research on the nationwide incidence of osteoporosis and hip fragility fractures and the cost-effectiveness of screening for osteoporosis in a local context would be helpful.
According to the World Organization of Family Doctors (WONCA), family medicine is aimed to “promote personal, comprehensive and continuing care for the individual in the context of the family and the community” [33]. Family medicine specialists are well-positioned to improve the screening and management of osteoporosis in the primary care setting. Our study has shown that FMS had a better knowledge level on osteoporosis and additional training in osteoporosis was associated with better knowledge. Addressing the gap in knowledge, particularly in pharmacotherapy, will be an important first step to improving the management of osteoporosis in the primary care setting. Family medicine specialists can also spearhead the utilisation of pharmacotherapy for osteoporosis in the primary care setting. The involvement of other stakeholders such as the public health policymakers will be crucial to pushing the osteoporosis agenda forward.
Strength and limitation
This is the first nationwide study that looked into the knowledge, attitude, practice and perceived barriers to osteoporosis screening and management among primary care doctors across Malaysia. The results of this study justify the allowance of prescription of bisphosphonates in the primary care setting and training of primary care doctors in the management of osteoporosis at the same time to reduce the burden of referring patients with osteoporosis to tertiary care centres just for initiation of therapy.
There were several limitations in this study. This was a self-reported study with a possibility of recall bias. In addition, this was an online survey disseminated via link-sharing, where the response rate was unknown. As this was a cross-sectional study conducted using a questionnaire without open-ended questions, we could not discount the possibility that there might be confounding factors not accounted for. We did not explore whether cost, logistics or other issues limited the use of BMD testing among doctors who had access to BMD machines. This study was conducted during the movement control order of the COVID-19 pandemic, where attention was diverted to combating the pandemic and primary care doctors were mobilised to the front line. Thus, any information collected on the current state of service might not reflect the usual practice.
We used an online survey in this study where respondents completed the questionnaires via digital devices such as smartphones. In Malaysia, the mobile phone penetration rate was at 130.2% in 2018 with the percentage of smartphone users rising from 68.7% in 2016 to 78.0% in 2018 [34]. An online survey was appropriate during the time of study considering the need to limit face-to-face contact during the COVID-19 pandemic. Online dissemination had allowed us to reach a wider range of respondents from all states in Malaysia. Another advantage of the online survey is that we expect less socially desirable responses to our questions on attitude and practice. However, we were unable to determine the response rate via this online method. We acknowledge that some doctors may opt not to answer the survey due to their unfamiliarity, dislike or distrust of digital surveys. Thus, the findings from this survey may not be generalizable to all primary care doctors in Malaysia.
Conclusion
Despite awareness of the importance of osteoporosis, there was a knowledge gap in the management of osteoporosis particularly in pharmacotherapy and a poor level of screening and non-pharmacological practice for osteoporosis among primary care doctors. A national structured health programme for osteoporosis is proposed to address the knowledge gap, increase screening practices and enhance accessibility to BMD and anti-osteoporosis medication in primary care. Future studies are needed to evaluate the cost-effectiveness of screening for osteoporosis and the outcome of a structured health programme to improve knowledge, screening and treatment practices of osteoporosis in primary care.
References
NIH consensus development panel on osteoporosis prevention (2001) diagnosis, and therapy. JAMA 285(6):785–795
Ambrish Mithal PE (2013) Carey S Kyer, Charanjit K Jagait, Laura Misteli, Dominique Pierroz, The Asia-Pacific regional audit: epidemiology, costs & burden of osteoporosis in. Int Osteoporos Foundation 2013:19–20
Downey C, Kelly M, Quinlan JF (2019) Changing trends in the mortality rate at 1-year post hip fracture - a systematic review. World J Orthop 10(3):166–175
Vochteloo AJ et al (2013) More than half of hip fracture patients do not regain mobility in the first postoperative year. Geriatr Gerontol Int 13(2):334–341
Ballane G et al (2014) Secular trends in hip fractures worldwide: opposing trends east versus west. J Bone Miner Res 29(8):1745–1755
Cheung CL et al (2018) An updated hip fracture projection in Asia: the Asian Federation of Osteoporosis Societies study. Osteoporos Sarcopenia 4(1):16–21
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7(5):407–413
Harvey NC et al (2017) Mind the (treatment) gap: a global perspective on current and future strategies for prevention of fragility fractures. Osteoporos Int 28(5):1507–1529
Cheung EYN et al (2016) Osteoporosis in East Asia: current issues in assessment and management. Osteoporos Sarcopenia 2(3):118–133
Abdulameer SA, Sahib MN, Sulaiman SAS (2018) The prevalence of osteopenia and osteoporosis among Malaysian type 2 diabetic patients using quantitative ultrasound densitometer. Open Rheumatol J 12:50–64
Leong J, Teh J, Zainodin A, Belani L, Ashraff M, Ariff M et al (2021) Osteoporosis care gap following fragility fracture in a tertiary teaching hospital. J Commu Med Publ Health Rep 2(4):1–5
Yeap SS et al (2017) Trends in post osteoporotic hip fracture care from 2010 to 2014 in a private hospital in Malaysia. Osteoporos Sarcopenia 3(2):112–116
Fogelman YGI, Segal E, Ish-Shalom S (2016) Managing osteoporosis: a survey of knowledge, attitudes and practices among primary care physicians in Israel. PLoS ONE 11(8):e0160661
Ahmed Z et al (2019) Knowledge, attitude and practice towards osteoporosis among general practitioners working in Al Majmaah Province, KSA. Asian J Pharma Res Health Care 11(2–4):45–54
Bloom BS (1956) Taxonomy of educational objectives, handbook I: the cognitive domain. David McKay Co Inc., New York
Chenot R et al (2007) German primary care doctors’ awareness of osteoporosis and knowledge of national guidelines. Exp Clin Endocrinol Diabetes 115(9):584–589
Jaglal SB, Carroll J, Hawker G, McIsaac WJ, Jaakkimainen L, Cadarette SM, Cameron C, Davis D (2003) How are family physicians managing osteoporosis? Qualitative study of their experiences and educational needs. Can Fam Physician 49:462–468
Otmar R, Reventlow SD, Nicholson GC, Kotowicz MA, Pasco JA (2012) General medical practitioners’ knowledge and beliefs about osteoporosis and its investigation and management. Arch Osteoporos 7:107–114
Perez-Edo L et al (2004) Management of osteoporosis in general practice: a cross-sectional survey of primary care practitioners in Spain. Osteoporos Int 15(3):252–257
Werner P, Vered I (2000) Management of osteoporosis: a survey of Israeli physicians’ knowledge and attitudes. Isr Med Assoc J 2(5):361–364
Fogelman YGI, Segal E, Ish-Shalom S (2016) Knowledge, attitudes and practices among primary care physicians in Israel. PLoS One 11(8):e0160661
Leonard E et al (2019) Factors affecting health care provider knowledge and acceptance of biosimilar medicines: a systematic review. J Manag Care Spec Pharm 25(1):102–112
Simonelli C et al (2002) Barriers to osteoporosis identification and treatment among primary care physicians and orthopedic surgeons. Mayo Clin proceed Mayo Clin 77:334–338
Davis SR et al (2011) Simplifying screening for osteoporosis in Australian primary care: the Prospective Screening for Osteoporosis; Australian Primary Care Evaluation of Clinical Tests (PROSPECT) study. Menopause 18(1):53–59
Chandran M et al (2020) Comparison of the osteoporosis self-assessment tool for Asians and the fracture risk assessment tool - FRAX to identify densitometric defined osteoporosis: a discriminatory value analysis in a multi-ethnic female population in Southeast Asia. Osteoporos Sarcopenia 6(2):53–58
World population review (2019) Accessed August 14, 2021. http://worldpopulationreview.com/countries
Department of Statistic Malaysia (2021) Current population estimates, Malaysia, 2021. July 15, 2021. Accessed August 14, 2021. https://www.dosm.gov.my.
Toh LS et al (2019) A comparison of 6 osteoporosis risk assessment tools among postmenopausal women in Kuala Lumpur. Malaysia Osteoporos Sarcopenia 5(3):87–93
Martin-Sanchez M et al (2019) Cost-effectiveness of the screening for the primary prevention of fragility hip fracture in spain using FRAX((R)). Calcif Tissue Int 105(3):263–270
Turner DA et al (2018) The cost-effectiveness of screening in the community to reduce osteoporotic fractures in older women in the UK: economic evaluation of the SCOOP study. J Bone Miner Res 33(5):845–851
Salminen H, Piispanen P, Toth-Pal E (2019) Primary care physicians’ views on osteoporosis management: a qualitative study. Arch Osteoporos 14(1):48
Gupta EDGE, Gun SC et al (2013) Osteoporosis awareness among primary care physicians in Malaysia. EXCLI J 12:521–522
World Organization of Family Doctors. Global family doctor (2021) Accessed Sept 12, 2021. https://www.globalfamilydoctor.com/aboutwonca/brief.aspx
Hand phone users survey (2018) 2018, Malaysian Communications and Multimedia Commission: Cyberjaya. Selangor, Malaysia
Acknowledgements
We would like to thank the Director-General of Health for his permission to publish this article and the Malaysian Family Medicine Specialist Associations (FMSA) for their assistance with the data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tay, C.L., Ng, W.L., Beh, H.C. et al. Screening and management of osteoporosis: a survey of knowledge, attitude and practice among primary care physicians in Malaysia. Arch Osteoporos 17, 72 (2022). https://doi.org/10.1007/s11657-022-01111-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01111-y