Abstract
Skeletal muscle has long been recognized as an inhospitable site for disseminated tumour cells (DTCs). Yet its antimetastatic nature has eluded a thorough mechanistic examination. Here, we show that DTCs traffic to and persist within skeletal muscle in mice and in humans, which raises the question of how this tissue suppresses colonization. Results from mouse and organotypic culture models along with metabolomic profiling suggested that skeletal muscle imposes a sustained oxidative stress on DTCs that impairs their proliferation. Functional studies demonstrated that disrupting reduction–oxidation homeostasis via chemogenetic induction of reactive oxygen species slowed proliferation in a more fertile organ: the lung. Conversely, enhancement of the antioxidant potential of tumour cells through ectopic expression of catalase in the tumour or host mitochondria allowed robust colonization of skeletal muscle. These findings reveal a profound metabolic bottleneck imposed on DTCs and sustained by skeletal muscle. A thorough understanding of this biology could reveal previously undocumented DTC vulnerabilities that can be exploited to prevent metastasis in other more susceptible tissues.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
Raw data for Figs. 1e,f,h, 2c,e–h, 3d,e,g–i, 4b–d,f–h,j, 5a,b,e,g,j, 6a,b,d,g,i,n, 7c–f,h,j,k and 8a,c,d,f–h, and Extended Data Figs. 2b,d, 3b–e, 4b–c,e and 5b,d–f,h–j have been provided as individual source data files. Full metabolomics data pertaining to Fig. 3 and Extended Data Fig. 3 can be found in Supplementary Tables 1–4. Metabolomics data have been deposited in Metabolomics Workbench (study number ST002058) and can be accessed directly via its project: https://doi.org/10.21228/M89135. Additional details pertaining to the AluYb8 qPCR method and the studies described in Fig. 1 and Extended Data Fig. 2 are provided as Supplementary Table 5. Source data are provided with this paper.
Code availability
Code used in this study (for example, ImageJ macros for image analysis) are freely available from the corresponding author upon request.
Change history
24 May 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41556-022-00945-5
References
Paget, S. The distribution of secondary growths in cancer of the breast. Lancet 133, 571–573 (1889).
Elia, I. et al. Breast cancer cells rely on environmental pyruvate to shape the metastatic niche. Nature 568, 117–121 (2019).
Elia, I. et al. Proline metabolism supports metastasis formation and could be inhibited to selectively target metastasizing cancer cells. Nat. Commun. 8, 15267 (2017).
Dupuy, F. et al. PDK1-dependent metabolic reprogramming dictates metastatic potential in breast cancer. Cell Metab. 22, 577–589 (2015).
Tasdogan, A. et al. Metabolic heterogeneity confers differences in melanoma metastatic potential. Nature 577, 115–120 (2020).
Sullivan, M. R. et al. Increased serine synthesis provides an advantage for tumors arising in tissues where serine levels are limiting. Cell Metab. 29, 1410–1421.e4 (2019).
Knott, S. R. V. et al. Asparagine bioavailability governs metastasis in a model of breast cancer. Nature 554, 378–381 (2018).
Ghajar, C. M. et al. The perivascular niche regulates breast tumour dormancy. Nat. Cell Biol. 15, 807–817 (2013).
Gupta, G. P. et al. Mediators of vascular remodelling co-opted for sequential steps in lung metastasis. Nature 446, 765–770 (2007).
Peinado, H. et al. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nat. Med. 18, 883–891 (2012).
Kaplan, R. N. et al. VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature 438, 820–827 (2005).
Hiratsuka, S., Watanabe, A., Aburatani, H. & Maru, Y. Tumour-mediated upregulation of chemoattractants and recruitment of myeloid cells predetermines lung metastasis. Nat. Cell Biol. 8, 1369–1375 (2006).
Kim, S. et al. Carcinoma-produced factors activate myeloid cells through TLR2 to stimulate metastasis. Nature 457, 102–106 (2009).
Oskarsson, T. et al. Breast cancer cells produce tenascin C as a metastatic niche component to colonize the lungs. Nat. Med. 17, 867–874 (2011).
Wculek, S. K. & Malanchi, I. Neutrophils support lung colonization of metastasis-initiating breast cancer cells. Nature 528, 413–417 (2015).
Costa-Silva, B. et al. Pancreatic cancer exosomes initiate pre-metastatic niche formation in the liver. Nat. Cell Biol. 17, 816–826 (2015).
Hoshino, A. et al. Tumour exosome integrins determine organotropic metastasis. Nature 527, 329–335 (2015).
Zhang, H. et al. Identification of distinct nanoparticles and subsets of extracellular vesicles by asymmetric flow field-flow fractionation. Nat. Cell Biol. 20, 332–343 (2018).
Barkan, D. et al. Metastatic growth from dormant cells induced by a Col-I-enriched fibrotic environment. Cancer Res. 70, 5706–5716 (2010).
Boudreau, N., Sympson, C. J., Werb, Z. & Bissell, M. J. Suppression of ICE and apoptosis in mammary epithelial cells by extracellular matrix. Science 267, 891–893 (1995).
Petersen, O. W., Ronnov-Jessen, L., Howlett, A. R. & Bissell, M. J. Interaction with basement membrane serves to rapidly distinguish growth and differentiation pattern of normal and malignant human breast epithelial cells. Proc. Natl Acad. Sci. USA 89, 9064–9068 (1992).
Pommier, A. et al. Unresolved endoplasmic reticulum stress engenders immune-resistant, latent pancreatic cancer metastases. Science 360, aao4908 (2018).
Pantel, K. et al. Frequent down-regulation of major histocompatibility class I antigen expression on individual micrometastatic carcinoma cells. Cancer Res. 51, 4712–4715 (1991).
Malladi, S. et al. Metastatic latency and immune evasion through autocrine inhibition of WNT. Cell 165, 45–60 (2016).
Coller, H. A. Cell biology: the essence of quiescence. Science 334, 1074–1075 (2011).
Kuilman, T., Michaloglou, C., Mooi, W. J. & Peeper, D. S. The essence of senescence. Genes Dev. 24, 2463–2479 (2010).
Albrengues, J. et al. Neutrophil extracellular traps produced during inflammation awaken dormant cancer cells in mice. Science 361, eaao4227 (2018).
Willis, R. A. The Spread of Tumours in the Human Body (Butterworth & Co., 1952).
Disibio, G. & French, S. W. Metastatic patterns of cancers: results from a large autopsy study. Arch. Pathol. Lab. Med. 132, 931–939 (2008).
Weiss, L. Biomechanical destruction of cancer cells in skeletal muscle: a rate-regulator for hematogenous metastasis. Clin. Exp. Metastasis 7, 483–491 (1989).
Parlakian, A. et al. Skeletal muscle phenotypically converts and selectively inhibits metastatic cells in mice. PLoS ONE 5, e9299 (2010).
Djaldetti, M., Sredni, B., Zigelman, R., Verber, M. & Fishman, P. Muscle cells produce a low molecular weight factor with anti-cancer activity. Clin. Exp. Metastasis 14, 189–196 (1996).
Fishman, P., Bar-Yehuda, S. & Vagman, L. Adenosine and other low molecular weight factors released by muscle cells inhibit tumor cell growth. Cancer Res. 58, 3181–3187 (1998).
Bar-Yehuda, S., Barer, F., Volfsson, L. & Fishman, P. Resistance of muscle to tumor metastases: a role for A3 adenosine receptor agonists. Neoplasia 3, 125–131 (2001).
Ghajar, C. M. Metastasis prevention by targeting the dormant niche. Nat. Rev. Cancer 15, 238–247 (2015).
Schneider, T., Osl, F., Friess, T., Stockinger, H. & Scheuer, W. V. Quantification of human Alu sequences by real-time PCR—an improved method to measure therapeutic efficacy of anti-metastatic drugs in human xenotransplants. Clin. Exp. Metastasis 19, 571–582 (2002).
Preston Campbell, J. et al. TRIzol and Alu qPCR-based quantification of metastatic seeding within the skeleton. Sci. Rep. 5, 12635 (2015).
Batzer, M. A. & Deininger, P. L. Alu repeats and human genomic diversity. Nat. Rev. Genet. 3, 370–379 (2002).
Li, W., Germain, R. N. & Gerner, M. Y. Multiplex, quantitative cellular analysis in large tissue volumes with clearing-enhanced 3D microscopy (Ce3D). Proc. Natl. Acad. Sci. USA 114, E7321–E7330 (2017).
Franco-Barraza, J., Beacham, D. A., Amatangelo, M. D. & Cukierman, E. Preparation of extracellular matrices produced by cultured and primary fibroblasts. Curr. Protoc. Cell Biol. 2016, 10.9.1–10.9.34 (2016).
Muir, A., Danai, L. V. & vander Heiden, M. G. Microenvironmental regulation of cancer cell metabolism: Implications for experimental design and translational studies. Dis. Model. Mech. 11, dmm035758 (2018).
Sullivan, M. R. & vander Heiden, M. G. Determinants of nutrient limitation in cancer. Crit. Rev. Biochem. Mol. Biol. 54, 193–207 (2019).
Schild, T., Low, V., Blenis, J. & Gomes, A. P. Unique metabolic adaptations dictate distal organ-specific metastatic colonization. Cancer Cell 33, 347–354 (2018).
Chong, J., Wishart, D. S. & Xia, J. Using MetaboAnalyst 4.0 for comprehensive and integrative metabolomics data analysis. Curr. Protoc. Bioinformatics 68, e86 (2019).
Kanehisa, M. & Goto, S. KEGG: Kyoto Encyclopedia of Genes and Genomes. Nucleic Acids Res. 28, 27–30 (2000).
Bansal, A. & Celeste Simon, M. Glutathione metabolism in cancer progression and treatment resistance. J. Cell Biol. 217, 2291–2298 (2018).
Powers, S. K., Li, Ji,L., Kavazis, A. N. & Jackson, M. J. Reactive oxygen species: impact on skeletal muscle. Compr. Physiol. 1, 941–969 (2011).
Townsend, D. M. S-glutathionylation: indicator of cell stress and regulator of the unfolded protein response. Mol. Interv. 7, 313–324 (2007).
Zitka, O. et al. Redox status expressed as GSH:GSSG ratio as a marker for oxidative stress in paediatric tumour patients. Oncol. Lett. 4, 1247–1253 (2012).
Chai, Y. C., Ashraf, S. S., Rokutan, K., Johnston, R. B. & Thomas, J. A. S-thiolation of individual human neutrophil proteins including actin by stimulation of the respiratory burst: evidence against a role for glutathione disulfide. Arch. Biochem. Biophys. 310, 273–281 (1994).
Piskounova, E. et al. Oxidative stress inhibits distant metastasis by human melanoma cells. Nature 527, 186–191 (2015).
Morgan, B., Sobotta, M. C. & Dick, T. P. Measuring EGSH and H2O2 with roGFP2-based redox probes. Free Radic. Biol. Med. 51, 1943–1951 (2011).
Gutscher, M. et al. Real-time imaging of the intracellular glutathione redox potential. Nat. Methods 5, 553–559 (2008).
Steinhorn, B. et al. Chemogenetic generation of hydrogen peroxide in the heart induces severe cardiac dysfunction. Nat. Commun. 9, 4044 (2018).
Glorieux, C. & Calderon, P. B. Catalase, a remarkable enzyme: targeting the oldest antioxidant enzyme to find a new cancer treatment approach. Biol. Chem. 398, 1095–1108 (2017).
Schriner, S. E. et al. Extension of murine life span by overexpression of catalase targeted to mitochondria. Science 308, 1909–1911 (2005).
Ligtenberg, M. A. et al. Coexpressed ÿcatalase protects chimeric antigen receptor-redirected T cells as well as bystander cells from oxidative stress-induced loss of antitumor activity. J. Immunol. 196, 759–766 (2016).
Grzelak, C. A. et al. Elimination of fluorescent protein immunogenicity permits modeling of metastasis in immune-competent settings. Cancer Cell 40, 1–2 (2021).
Yun, J. et al. Vitamin C selectively kills KRAS and BRAF mutant colorectal cancer cells by targeting GAPDH. Science 350, 1391–1396 (2015).
Diehn, M. et al. Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature 458, 780–783 (2009).
Gorrini, C., Harris, I. S. & Mak, T. W. Modulation of oxidative stress as an anticancer strategy. Nat. Rev. Drug Discov. 12, 931–947 (2013).
Nguyen, A. et al. PKLR promotes colorectal cancer liver colonization through induction of glutathione synthesis. J. Clin. Invest 126, 681–694 (2016).
Ubellacker, J. M. et al. Lymph protects metastasizing melanoma cells from ferroptosis. Nature 585, 113–118 (2020).
Snijders, T. et al. Satellite cells in human skeletal muscle plasticity. Front. Physiol. 6, 283 (2015).
Hojman, P., Gehl, J., Christensen, J. F. & Pedersen, B. K. Cell metabolism perspective molecular mechanisms linking exercise to cancer prevention and treatment. Cell Metab. 27, 10–21 (2018).
Fujikawa, Y. et al. Mouse redox histology using genetically encoded probes. Sci. Signal. 9, rs1 (2016).
Nemkov, T., Hansen, K. C. & D’Alessandro, A. A three-minute method for high-throughput quantitative metabolomics and quantitative tracing experiments of central carbon and nitrogen pathways. Rapid Commun. Mass Spectrom. 31, 663–673 (2017).
Nemkov, T., Reisz, J. A., Gehrke, S., Hansen, K. C. & D’Alessandro, A. in Methods in Molecular Biology Vol. 1978 (ed. D'Alessandro, A.) 13–26 (Humana Press, 2019).
Acknowledgements
We are grateful to M. J. Bissell (Lawrence Berkeley National Laboratory) and to H. Blau (Stanford University) for inspiring this work. We remain indebted to the Breast Origin Cancer Tissue Donated after Death (BROCADE) programme, funded by the National Breast Cancer Foundation of Australia, for their hard work and especially to the women with MBC who selflessly donated to this study. We would like to thank P. Rabinovitch (University of Washington) and his group for the mCAT transgenics that enabled generation of the C57BL/6 myoblasts used within this manuscript. We thank W. J. Valente and J. Bielas (FHCRC) for providing the pBMN-IRES-GFP-mCAT and -cCAT vectors, and S. Beronja (FHCRC) for his critical feedback. This study was supported principally by the W. M. Keck Foundation (to C.M.G., K.C.H. and P.S.N.), and by start-up funds from the FHCRC (to C.M.G.). The Comparative Medicine and Proteomics Shared Resources of the FHCRC/University of Washington Cancer Consortium helped support this work and are funded by the NCI (P30 CA015704). BioRender.com was used to create mouse/human schematics. S.B.C. was supported by a Cellular and Molecular Biology Training Grant from the NIH (T32GM007270). J.D. was supported by a Postdoctoral Breakthrough award (W81XWH-18-1-0028) by the DoD Breast Cancer Research Program. P.S.N., L.D.T. and R.F.D. are also supported by P50CA097186.
Author information
Authors and Affiliations
Contributions
S.B.C. performed experiments and analysed and interpreted data. T.N. and K.C.H. conducted metabolomics and associated data analysis and interpretation. J.D. assisted with animal experiments. A.S. facilitated the collection of human SkM specimens. R.F.D. stained and analysed the human SkM specimens (findings were confirmed by L.D.T.). S.B.C., L.B.S., S.J.T., P.S.N. and K.C.H. provided scientific insight. C.M.G. conceived the study. S.B.C. and C.M.G. wrote the manuscript. All authors read and provided feedback on the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Cell Biology thanks Sarah-Maria Fendt, Vittorio Sartorelli and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
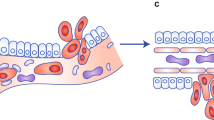
Extended Data Fig. 1 Human SkM from a metastatic breast cancer patient harbours panCK+/ER+/PR+ breast cancer cells.
a) Representative multiplex IHC images from an ER+/PR+ primary breast tumour specimen, used as a positive staining control. ER/PR (breast cell marker) staining in purple, pan-cytokeratin (panCK, epithelial cell marker) staining in yellow. Scale bar: 1 mm (left), 100 μm (centre) and 10 μm (right). b) Representative multiplex IHC images from human SkM, used as a negative staining control. ER/PR staining in purple, panCK staining in yellow. Scale bar, 10 μm. c) Representative IHC image of the three human SkM sites sampled (tibialis anterior, quadriceps and gastrocnemius) from a patient with metastatic breast cancer (MBC). Scale bar, 1 cm. d) Multiplex IHC panels of three panCK+/ER+/PR+ cells located inside the quadriceps muscle. ER/PR staining in purple, pan-cytokeratin staining in yellow. Scale bar 100 μm, Inset 10 μm. e-f) Two micropictographs of serial sections (4 µm) of FFPE SkM tissue from an individual with metastatic breast cancer. The slides were stained with hematoxylin and eosin or sequentially stained with a multiplex IHC panel consisting of ER/PR (purple) and panCK (yellow). Two ER+/PR+/panCK+ breast cancer cells were identified in a vessel located within the quadriceps muscle. Scale bar, 10 μm.
Extended Data Fig. 2 AluYb8 qPCR reveals that DTCs travel to and persist within multiple mouse SkMs following intracardiac injection of breast cancer cells.
a) Schematic of mouse study to examine frequency of DTCs across organ site at early and late timepoints. b) AluYb8 amplification (fold change) at Day 3 post ic injection. n = 11 inoculated and 3 uninoculated mice. Lung, brain and TA, P < 0.0001 when multiple unpaired two-tailed t-tests, followed by the Holm-Sidak method, were run for comparison of tumour-bearing tissues to uninoculated controls. c) Representative IF images of matched brain, lung, SkM and bone marrow (BoMa) with DTCs at the early timepoint. Scale bar: 100 μm for lung, brain and BoMa. 10 μm for muscle. d) AluYb8 amplification (fold change) at Week 7. n = 11 inoculated and 3 uninoculated mice. Lung, brain, liver, BoMa and TA, **** P < 0.0001 when multiple unpaired two-tailed t-tests, followed by Holm-Sidak method, were run for comparison of tumour-bearing tissues to uninoculated controls. e) Representative IF images of matched brain, lung, SkM and BoMa with DTCs at the late timepoint. Scale bar: 100 μm for lung, brain and BoMa; 10 μm for muscle. f) Representative IF images of DTCs or clusters of tumour cells in the brain, lung or SkM. Ki67+ marks proliferating cells. Scale bar: 100 μm for lung, brain and BoMa; 10 μm for muscle. n = 15 cells each. For c, e and g, centre line represents the mean, and error bars the standard error of the mean (s.e.m.).
Extended Data Fig. 3 Metabolic comparison of SkM-metastatic 4T1 cells pre- and post-injection reveal that 4T1-SkM adapt to SkM.
a) PLS-DA score plot comparing 4T1-parental and 4T1-SkM cells in tissue culture against 4T1-SkM SkM metastases, 4T1-SkM lung metastases, healthy SkM and healthy lung. b) Fold change enrichment of GSH-related metabolites (defined by KEGG’s GSH metabolism set) for 4T1-SkM v. 4T1-parental in culture, SkM metastases v. 4T1-SkM in culture, and lung metastases v. 4T1-SkM in culture. c) Metabolite Set Enrichment of the metabolites that were 2-fold enriched in healthy SkM versus healthy lung. Over Representation Analysis used the hypergeometric test; one-tailed P-values were provided after adjusting for multiple testing. d) Table displaying the mean values for the GSH-related metabolites in healthy SkM and healthy lung, followed by the fold-change difference between the two. e) Dot-plot of the ratio of reduced to oxidized glutathione (GSH:GSSG) for 4T1-SkM and 4T1-parental in culture, healthy SkM and healthy lung, and SkM- and lung- metastases. n = 3 replicates for 4T1-parental and 4T1-SkM culture samples. n = 4 muscle- and 3 lung- metastases, 6 healthy muscle and 3 healthy lung. An one-way ANOVA, followed by uncorrected Fisher’s LSD, was performed where *** P = 0.0004 for 4T1-parental v 4T1-SkM, **** P < 0.0001 for healthy SkM v. lung, * P = 0.037 for SkM metastases v. lung metastases. For e, centre line represents the mean, and error bars the standard error of the mean (s.e.m.).
Extended Data Fig. 4 H2O2 is generated upon D-alanine treatment in a dose-dependent fashion in DAAO-expressing tumour cells and lung fibroblasts.
a) Workflow to test if D-/L-alanine stimulated H2O2 in MDA231-WT and -DAAO. b) Extracellular H2O2 of MDA231-WT and -DAAO treated with D-/L-alanine. n = 3 replicates, performed twice. Two-way ANOVA was used, followed by Dunnett’s test. Compared against untreated MDA231-DAAO mean- 1 h: *P = 0.028,100 mM D-ala. 4 h: ***P = 0.0001, 100 mM D-ala; **P = 0.0017, 20 mM D-ala; **P = 0.0019, 100 mM D-ala MDA231-WT. 8 h: ***P = 0.0001, 100 mM L-ala, 20 mM L-ala. *P = 0.023, 100 mM D-ala MDA231-WT; * P = 0.018, 20 mM D-ala MDA231-WT. 24 h: ***P = 0.000, 100 mM D-ala; *P = 0.011, 100 mM L-ala. 48 h: ***P = 0.000, 100 mM D-ala. All other P > 0.05. c) MDA231-WT and -DAAO outgrowth with D-/L-alanine. n = 3 replicates, performed twice. Two-way ANOVA, followed by Dunnett’s test: compared against untreated MDA231-DAAO- 48 h: ***P = 0.0001, 100 mM D-ala; **P = 0.0011, 100 mM D-ala MDA231-WT; **P = 0.0036, 20 mM D-ala MDA231-WT; *P = 0.04, untreated MDA231-WT. 72 h: ***P = 0.0001, 100 mM D-ala, untreated MDA231-WT, 20 mM L-ala MDA231-WT. All others P > 0.05. d) Workflow to test if D-/L-alanine stimulates H2O2 in LF-DAAO. e) Extracellular H2O2 in LF-DAAO and LF treated with D-/L-alanine. n = 3 replicates per condition, performed twice. Two-way ANOVA, followed by uncorrected Fisher’s LSD: ****P < 0.0001, LF-DAAO 100 mM D-ala v. LF 100 mM D-ala, LF-DAAO 100 mM D-ala v. LF-DAAO 100 mM L-ala (4 h). 8 h: *P = 0.03, LF-DAAO 50 mM D-ala v. LF 50 mM D-ala; ****P < 0.0001, 70-, 100-mM D-ala LF-DAAO v. LF. 24 h: * P = 0.033, LF-DAAO 20 mM D-ala v. LF 20 mM D-ala; ** P = 0.004, LF-DAAO 30 mM D-ala v. LF 30 mM D-ala. **** P < 0.0001, 40-, 50-, 70-, 100-mM D-ala LF-DAAO v. LF. 48 h: *** P = 0.0006, LF-DAAO 30 mM D-ala v. LF 30 mM D-ala. **** P < 0.0001, 40-, 50-, 70-, 100-mM D-ala LF-DAAO v. LF. Other LF-DAAO v. LF comparisons with D-ala P > 0.05. For b-c and e, error bars represent the s.e.m.
Extended Data Fig. 5 Targeting catalase to the tumour cell mitochondria does not promote lung colonization.
a) Representative Western blots of MDA231 and EO771 -Ctl, -mCAT and -cCAT. b) Dot-plots of MDA231 and EO771 -Ctl, -mCAT or -cCAT outgrowth on LF. n = 10-15 replicates, performed in triplicate. One-way ANOVA, followed by Dunnett’s test, was performed. Mean of each condition compared against Ctl mean: P = 0.43, MDA231-Ctl v mCAT; P = 0.35, MDA231-Ctl v cCAT,; **** P < 0.0001, EO771-Ctl v mCAT, EO771-Ctl v cCAT. c) NOD-SCID study to examine if ectopic catalase promoted lung colonization. d) BLI measurements (total flux, photon/second) for MDA231-Ctl, -mCAT and -cCAT. n = 5 mice per cohort. Two-way ANOVA, followed by Tukey’s test, was performed. Week5- *P = 0.032, MDA231-Ctl v mCAT; *P = 0.027, MDA231-Ctl v cCAT. Week6- ****P < 0.0001, MDA231-Ctl v. mCAT, Ctl v. cCAT, e) BLI total flux for MDA231-Ctl, -mCAT and -cCAT in lung ex vivo. n = 5 mice per cohort. One-way ANOVA, followed by Tukey’s test, was performed: * P = 0.028, Ctl v mCAT; *P = 0.026, Ctl v cCAT. f) Quantification of MDA231-Ctl, -mCAT and -cCAT lesions in lung, with representative images of tumour burden. Arrows point to small GFP+ lesions. n = 5 mice per cohort. Scale bar, 1 mm. One-way ANOVA was performed, followed by Dunnett’s test, to determine **P = 0.0044, MDA231-Ctl v. mCAT; *** P = 0.0008, MDA231-Ctl v. cCAT. g) C57BL/6 study to examine if ectopic catalase promoted lung colonization. h) BLI total flux for EO771-Ctl and -mCAT. n = 5 mice per cohort. Two-way ANOVA, followed by Sidak’s test, was performed. Week2- *P = 0.039, EO771-Ctl v mCAT. i) BLI total flux for EO771-Ctl and -mCAT tumours in lung ex vivo. n = 5 mice per cohort. Unpaired two-tailed t-test was performed, where EO771-Ctl v mCAT, *P = 0.026. j) Quantification of EO771-Ctl and -mCAT lesions in lung, with representative images of tumour burden. Scale bar, 1 mm. Unpaired two-tailed t-test was performed where **P = 0.0036. For b, e-f and i-j, centre line represents mean, and error bars the s.e.m.
Supplementary information
Supplementary Tables
Supplementary Table 1: Details of the metabolomics study; glutathione ratios. Supplementary Table 2: Raw dataset for the metabolomics study (first run: paired metastases and healthy tissues). Supplementary Table 3: Raw dataset for the metabolomics study (second run: parental-4T1 cells and 4T1-SkM cells cultured on tissue culture plastic). Supplementary Table 4: Combined raw datasets of the metabolomics studies (cells cultured on tissue culture plastic combined with metastases and healthy tissues). Supplementary Table 5: Technical details and validation for the AluYb8 qPCR method.
Source data
Source Data Fig. 1
Source data.
Source Data Fig. 2
Source data.
Source Data Fig. 3
Source data.
Source Data Fig. 4
Source data.
Source Data Fig. 5
Source data.
Source Data Fig. 6
Source data.
Source Data Fig. 7
Source data.
Source Data Fig. 8
Source data.
Source Data Extended Data Fig. 2
Source data.
Source Data Extended Data Fig. 3
Source data.
Source Data Extended Data Fig. 4
Source data.
Source Data Extended Data Fig. 5
Source data.
Source Data Extended Data Fig. 5
Unprocessed western blots.
Rights and permissions
About this article
Cite this article
Crist, S.B., Nemkov, T., Dumpit, R.F. et al. Unchecked oxidative stress in skeletal muscle prevents outgrowth of disseminated tumour cells. Nat Cell Biol 24, 538–553 (2022). https://doi.org/10.1038/s41556-022-00881-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41556-022-00881-4
This article is cited by
-
Metabolic heterogeneity in cancer
Nature Metabolism (2024)
-
Lung endothelium exploits susceptible tumor cell states to instruct metastatic latency
Nature Cancer (2024)
-
How much do we know about the metastatic process?
Clinical & Experimental Metastasis (2024)
-
Intravital imaging to study cancer progression and metastasis
Nature Reviews Cancer (2023)
-
Dormant cancer cells: programmed quiescence, senescence, or both?
Cancer and Metastasis Reviews (2023)