Abstract
Background and Objective
Piperacillin is a broad-spectrum β-lactam antibiotic commonly prescribed in intensive care units. Many piperacillin population pharmacokinetic models have been published, but few underwent an external evaluation. External evaluation is an important process to determine a model’s capability of being generalized to other hospitals. We aimed to assess the predictive performance of these models with an external validation dataset.
Methods
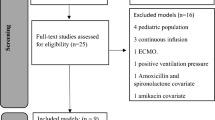
Six models were evaluated with a dataset consisting of 30 critically ill patients (35 samples) receiving piperacillin by continuous infusion. Models were subject to prediction-based (bias and imprecision) and simulation-based evaluations. When a model had an acceptable evaluation, it was used for dosing simulations to evaluate the probability of target attainment.
Results
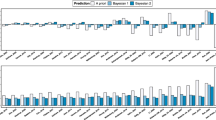
Bias and imprecision ranged from − 35.7 to 295% and from 22.7 to 295%, respectively. The models of Klastrup et al. and of Udy et al. were acceptable according to our criteria and were used for dosing simulations. Simulations showed that a loading dose of 4 g followed by a maintenance dose of 16 g/24 h of piperacillin infused continuously was necessary to remain above a pharmacokinetic-pharmacodynamic target set as a minimal inhibitory concentration of 16 mg/L in 90% of patients, for a median patient with a creatinine clearance of 76 mL/min.
Conclusions
Despite the considerable variation in the predictive performance of the models with the external validation dataset, this study was able to validate two of these models and led to the elaboration of a dosing nomogram for piperacillin by continuous infusion that can be used by clinicians in intensive care units.





Similar content being viewed by others
References
Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998;26(1):1–12. https://doi.org/10.1086/516284%JClinicalInfectiousDiseases.
Abdulziz MH, Alffenaar JWC, Bassetti M, et al. Antimicrobial therapeutic drug monitoring in critically ill adult patients: a position paper. Intensive Care Med. 2020;46(6):1127–53. https://doi.org/10.1007/s00134-020-06050-1.
Guilhaumou R, Benaboud S, Bennis Y, et al. Optimization of the treatment with beta-lactam antibiotics in critically ill patients—guidelines from the French Society of Pharmacology and Therapeutics (Société Française de Pharmacologie et Thérapeutique—SFPT) and the French Society of Anaesthesia and Intensive Care Medicine (Société Française d’Anesthésie et Réanimation—SFAR). Crit Care. 2019;23(1):104. https://doi.org/10.1186/s13054-019-2378-9.
Sumi CD, Heffernan AJ, Lipman J, et al. What antibiotic exposures are required to suppress the emergence of resistance for gram-negative bacteria? A systematic review. Clin Pharm. 2019;58(11):1407–43. https://doi.org/10.1007/s40262-019-00791-z.
Abdul-Aziz MH, Sulaiman H, Mat-Nor M-B, et al. Beta-Lactam Infusion in Severe Sepsis (BLISS): a prospective, two-centre, open-labelled randomised controlled trial of continuous versus intermittent beta-lactam infusion in critically ill patients with severe sepsis. Intensive Care Med. 2016;42(10):1535–45. https://doi.org/10.1007/s00134-015-4188-0.
Dulhunty JM, Roberts JA, Davis JS, et al. A Multicenter randomized trial of continuous versus intermittent β-lactam infusion in severe sepsis. Am J Respir Crit Care Med. 2015;192(11):1298–305. https://doi.org/10.1164/rccm.201505-0857OC.
Fawaz S, Barton S, Nabhani-Gebara S. Comparing clinical outcomes of piperacillin-tazobactam administration and dosage strategies in critically ill adult patients: a systematic review and meta-analysis. BMC Infect Dis. 2020;20(1):430. https://doi.org/10.1186/s12879-020-05149-6.
Hagel S, Bach F, Brenner T, et al. Effect of therapeutic drug monitoring-based dose optimization of piperacillin/tazobactam on sepsis-related organ dysfunction in patients with sepsis: a randomized controlled trial. Intensive Care Med. 2022;48(3):311–21. https://doi.org/10.1007/s00134-021-06609-6.
Blot SI, Pea F, Lipman J. The effect of pathophysiology on pharmacokinetics in the critically ill patient—concepts appraised by the example of antimicrobial agents. Adv Drug Deliv Rev. 2014;77:3–11. https://doi.org/10.1016/j.addr.2014.07.006.
El-Haffaf I, Caissy J-A, Marsot A. Piperacillin-tazobactam in intensive care units: a review of population pharmacokinetic analyses. Clin Pharmacokinet. 2021. https://doi.org/10.1007/s40262-021-01013-1.
US Food and Drug Administration. Population pharmacokinetics: guidance for industry (draft guidance) 2019. https://www.fda.gov/media/128793/download. Accessed 15 Feb 2022
Brendel K, Dartois C, Comets E, et al. Are population pharmacokinetic and/ or pharmacodynamic models adequately evaluated? Clin Pharmacokinet. 2007;46(3):221–34. https://doi.org/10.2165/00003088-200746030-00003.
Cheng Y, Wang C-Y, Li Z-R, et al. Can population pharmacokinetics of antibiotics be extrapolated? Implications of External Evaluations. Clin Pharm. 2021;60(1):53–68. https://doi.org/10.1007/s40262-020-00937-4.
Verdier M-C, Tribut O, Tattevin P, et al. Simultaneous determination of 12 beta-lactam antibiotics in human plasma by high-performance liquid chromatography with UV detection: application to therapeutic drug monitoring. Antimicrob Agents Chemother. 2011;55(10):4873–9. https://doi.org/10.1128/AAC.00533-11.
Pfizer. Piperacillin sodium and tazobactam sodium (Zosyn) product information New York 2012 [August 8th 2021]. https://labeling.pfizer.com/showlabeling.aspx?id=416.
Varvel JR, Donoho DL, Shafer SL. Measuring the predictive performance of computer-controlled infusion pumps. J Pharmacokinet Biopharm. 1992;20(1):63–94. https://doi.org/10.1007/BF01143186.
Sheiner LB, Beal SL. Some suggestions for measuring predictive performance. J Pharmacokinet Biopharm. 1981;9(4):503–12. https://doi.org/10.1007/bf01060893.
Miyabe-Nishiwaki T, Masui K, Kaneko A, et al. Evaluation of the predictive performance of a pharmacokinetic model for propofol in Japanese macaques (Macaca fuscata fuscata). J Vet Pharmacol Ther. 2013;36(2):169–73. https://doi.org/10.1111/j.1365-2885.2012.01404.x.
Minichmayr IK, Roberts JA, Frey OR, et al. Development of a dosing nomogram for continuous-infusion meropenem in critically ill patients based on a validated population pharmacokinetic model. J Antimicrob Chemother. 2018;73(5):1330–9. https://doi.org/10.1093/jac/dkx526%JJournalofAntimicrobialChemotherapy.
Quinton MC, Bodeau S, Kontar L, et al. Neurotoxic concentration of piperacillin during continuous infusion in critically ill patients. Antimicrob Agents Chemother. 2017. https://doi.org/10.1128/aac.00654-17.
Bue M, Sou T, Okkels ASL, et al. Population pharmacokinetics of piperacillin in plasma and subcutaneous tissue in patients on continuous renal replacement therapy. Int J Infect Dis. 2020;92:133–40. https://doi.org/10.1016/j.ijid.2020.01.010.
Klastrup V, Thorsted A, Storgaard M, et al. Population pharmacokinetics of piperacillin following continuous infusion in critically ill patients and impact of renal function on target attainment. Antimicrob Agents Chemother. 2020;64(7):e02556-e2619. https://doi.org/10.1128/AAC.02556-19.
Öbrink-Hansen K, Juul RV, Storgaard M, et al. Population pharmacokinetics of piperacillin in the early phase of septic shock: does standard dosing result in therapeutic plasma concentrations? Antimicrob Agents Chemother. 2015;59(11):7018. https://doi.org/10.1128/AAC.01347-15.
Roberts DM, Liu X, Roberts JA, et al. A multicenter study on the effect of continuous hemodiafiltration intensity on antibiotic pharmacokinetics. Crit Care. 2015;19(1):84. https://doi.org/10.1186/s13054-015-0818-8.
Roberts JA, Kirkpatrick CMJ, Roberts MS, et al. First-dose and steady-state population pharmacokinetics and pharmacodynamics of piperacillin by continuous or intermittent dosing in critically ill patients with sepsis. Int J Antimicrob Agents. 2010;35(2):156–63. https://doi.org/10.1016/j.ijantimicag.2009.10.008.
Udy AA, Lipman J, Jarrett P, et al. Are standard doses of piperacillin sufficient for critically ill patients with augmented creatinine clearance? Crit Care. 2015;19(1):28. https://doi.org/10.1186/s13054-015-0750-y.
Felton TW, Goodwin J, O’Connor L, et al. Impact of bolus dosing versus continuous infusion of piperacillin and tazobactam on the development of antimicrobial resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2013;57(12):5811–9. https://doi.org/10.1128/AAC.00867-13.
De Schepper PJ, Tjandramaga TB, Mullie A, et al. Comparative pharmacokinetics of piperacillin in normals and in patients with renal failure. J Antimicrob Chemother. 1982;9(1):49–57. https://doi.org/10.1093/jac/9.suppl_B.49.
Chen IH, Nicolau DP. Augmented renal clearance and how to augment antibiotic dosing. Antibiotics (Basel). 2020;9(7):393. https://doi.org/10.3390/antibiotics9070393.
Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41. https://doi.org/10.1159/000180580 (PubMed PMID: 1244564).
Dhaese SAM, Farkas A, Colin P, et al. Population pharmacokinetics and evaluation of the predictive performance of pharmacokinetic models in critically ill patients receiving continuous infusion meropenem: a comparison of eight pharmacokinetic models. J Antimicrob Chemother. 2018;74(2):432–41. https://doi.org/10.1093/jac/dky434%JJournalofAntimicrobialChemotherapy.
Monteiro JF, Hahn SR, Gonçalves J, et al. Vancomycin therapeutic drug monitoring and population pharmacokinetic models in special patient subpopulations. Pharmacol Res Perspect. 2018;6(4):e00420. https://doi.org/10.1002/prp2.420 (PubMed PMID: 30156005; PubMed Central PMCID: PMCPMC6113434).
Wang YL, Guilhaumou R, Blin O, et al. External evaluation of population pharmacokinetic models for continuous administration of meropenem in critically ill adult patients. Eur J Clin Pharmacol. 2020;76(9):1281–9. https://doi.org/10.1007/s00228-020-02922-z.
Miller RD, Eriksson L, Fleisher LA, et al. Miller's anesthesia. 7th ed. Philadephia: Churchill Livingstone/Elsevier; 2010.
Pea F, Viale P. Bench-to-bedside review: appropriate antibiotic therapy in severe sepsis and septic shock—does the dose matter? Crit Care. 2009;13(3):214. https://doi.org/10.1186/cc7774.
Landersdorfer CB, Bulitta JB, Kirkpatrick CMJ, et al. Population pharmacokinetics of piperacillin at two dose levels: influence of nonlinear pharmacokinetics on the pharmacodynamic profile. Antimicrob Agents Chemother. 2012;56(11):5715–23. https://doi.org/10.1128/AAC.00937-12.
Nicasio AM, VanScoy BD, Mendes RE, et al. Pharmacokinetics-pharmacodynamics of tazobactam in combination with piperacillin in an in vitroinfection model. Antimicrob Agents Chemother. 2016;60(4):2075–80. https://doi.org/10.1128/AAC.02747-15.
Kalaria SN, Gopalakrishnan M, Heil EL. A population pharmacokinetics and pharmacodynamic approach to optimize tazobactam activity in critically ill patients. Antimicrob Agents Chemother. 2020;64(3):e02093-e2119. https://doi.org/10.1128/AAC.02093-19.
Komuro M, Maeda T, Kakuo H, et al. Inhibition of the renal excretion of tazobactam by piperacillin. J Antimicrob Chemother. 1994;34(4):555–64. https://doi.org/10.1093/jac/34.4.555.
Hayashi Y, Roberts JA, Paterson DL, et al. Pharmacokinetic evaluation of piperacillin-tazobactam. Expert Opin Drug Metab Toxicol. 2010;6(8):1017–31. https://doi.org/10.1517/17425255.2010.506187.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this article.
Conflict of interest
The authors have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Ethical approval was granted by the local Ethics Committee of Aix Marseille Université (no. 2016-28-09-04).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Data related to the evaluated models weres collected from the already published articles in the literature. Patient data obtained from the Hôpital de la Timone are not publicly available.
Code availability
Not applicable.
Author contribution
IE evaluated the models, analyzed the data, and wrote the manuscript. RG, LV, and AM validated the manuscript. AM supervised the work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
El-Haffaf, I., Guilhaumou, R., Velly, L. et al. Using a Validated Population Pharmacokinetic Model for Dosing Recommendations of Continuous Infusion Piperacillin for Critically Ill Adult Patients. Clin Pharmacokinet 61, 895–906 (2022). https://doi.org/10.1007/s40262-022-01118-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-022-01118-1