Abstract
Current evidence is inconclusive on cognitive benefits or harms of statins among stroke patients, who have high risk of dementia. This observational cohort study investigated the association between statin use and post-stroke dementia using data from the Clinical Practice Research Datalink. Patients without prior dementia who had an incident stroke but received no statins in the preceding year were followed for up to 10 years. We used inverse probability weighted marginal structural models to estimate observational analogues of intention-to-treat (ITT, statin initiation vs. no initiation) and per-protocol (PP, sustained statin use vs. no use) effects on the risk of dementia. To explore potential impact of unmeasured confounding, we examined the risks of coronary heart disease (CHD, positive control outcome), fracture and peptic ulcer (negative control outcomes). In 18,577 statin initiators and 14,613 non-initiators (mean follow-up of 4.2 years), the adjusted hazard ratio (aHR) for dementia was 0.70 (95% confidence interval [CI] 0.64–0.75) in ITT analysis and 0.55 (95% CI 0.50–0.62) in PP analysis. The corresponding aHRITT and aHRPP were 0.87 (95% CI 0.79–0.95) and 0.70 (95% CI 0.62–0.80) for CHD, 1.03 (95% CI 0.82–1.29) and 1.09 (95% CI 0.77–1.54) for peptic ulcer, and 0.88 (95% CI 0.80–0.96) and 0.86 (95% CI 0.75–0.98) for fracture. Statin initiation after stroke was associated with lower risk of dementia, with a potentially greater benefit in patients who persisted with statins over time. The observed association of statin use with post-stroke dementia may in part be overestimated due to unmeasured confounding shared with the association between statin use and fracture.
Similar content being viewed by others
Background
While incident dementia affects 10% of patients with first-ever stroke and 30% with recurrent stroke [1], aggressive treatment of cardiovascular risk factors may potentially decrease the risk of post-stroke dementia [2]. Statins are recommended for the secondary prevention of atherosclerotic cardiovascular disease (ASCVD) including ischaemic stroke [3,4,5]; however, non-persistence with statin therapy remains a major challenge in practice [6, 7]. For intracerebral haemorrhage, there are insufficient data to support or restrict the use of statins in those patients [8].
Observational evidence suggests that statins may also help prevent dementia [9,10,11,12,13], but large-scale randomised controlled trials (RCTs) in people at high risk of cardiovascular events (most without stroke) did not find cognitive benefits (assessed using multiple cognitive tests as secondary outcomes) associated with statin use [14, 15]. Case reports [16,17,18] and small-scale trials [19, 20] have even suggested that statins may cause reversible cognitive impairment. The recent World Health Organisation (WHO) guideline classifies the current evidence on statin use for the prevention of dementia as low-quality [21].
To investigate whether statins could confer cognitive benefits or harms, stroke survivors would be a suitable population as many are likely to start statins and have multiple risk factors that put them at high risk of dementia [22]. Although some statin trials included cognitive assessment as secondary outcomes and enrolled a small proportion of stroke survivors [14, 15], no RCTs have specifically investigated the effect of statins on post-stroke dementia [23]. The only relevant trial published to date is the Prevention of Decline in Cognition after Stroke Trial (PODCAST), which investigated the effect of an intensive low-density lipoprotein (LDL) cholesterol target (< 1.3 mmol/L) versus guideline target (< 3.0 mmol/L) for preventing cognitive decline in 77 stroke patients [24]. The trial found that the intensive target significantly improved some cognitive test scores in the two-year follow-up, with statistically non-significant protective effect on dementia (odds ratio [OR] 0.18, 95% confidence interval [Cl] 0.01–3.98). A limited number of observational studies suggested that statin use may help prevent post-stroke dementia, but these studies are susceptible to biases due to inclusion of pre-stroke statin users and inappropriate control for confounding and selection bias [23].
It remains uncertain whether statins benefit or harm cognition in patients with stroke. We conducted a retrospective cohort study to examine the association of statin use with the risk of dementia among patients with an incident ischaemic stroke or intracerebral haemorrhage.
Methods
Data source
This study used Clinical Practice Research Datalink (CPRD) GOLD and its linked datasets, including hospitalisation data from integrated Hospital Episode Statistics (HES), death data from Office for National Statistics (ONS), and socioeconomic data from Index of Multiple Deprivation (IMD) datasets [25, 26]. The CPRD GOLD provides anonymised data extracted from primary care medical records, with coverage of a representative sample of approximately 7% of the UK population from more than 670 practices [25].
Study population
We included patients aged 18 years or older with an incident stroke (hereafter referred to as index stroke) recorded in the CPRD between 1 January 2006 and 31 December 2017 (diagnosis codes for stroke are listed in Supplementary material of Appendix 1). We stratified stroke subtype into ischaemic stroke and intracerebral haemorrhage in our analysis. Patients were excluded if they had a diagnosis code indicating dementia any time before or within the first 90 days following the index stroke, had any codes related to statin prescription within one year before the index stroke, or had less than 12-month information recorded before the index stroke. In the main analysis, we also excluded those with any missing values for baseline covariates (i.e., smoking or body mass index [BMI]). For the analysis of each control outcome (described below), we additionally excluded patients who had any diagnosis codes related to the control outcome before the index stroke or within 90 days after the index stroke.
Exposures
The exposure of interest was statin initiation, defined as having any statin prescription within the first 90 days following the index stroke (Fig. 1). This time frame represents an early secondary prevention strategy and is also pragmatic to capture the first statin prescription in general practices after hospital stay. This approach also reduced misclassification of statin initiation given the vast majority of people with stroke should have been discharged within this time frame and had visited their general practitioners for follow-up care. The product codes for statins are shown in Supplementary material of Appendix 1. Patients who received no statins within this time period were included in the statin non-initiation group. The exposure status was then treated as a time-varying variable (updated every 30 days, starting from the 91st day following the index stroke). Statin use was considered sustained until no further statin prescription within the expected end of days-supply (30 days of the previous prescription) plus a 90-day grace period.
Outcomes
The primary outcome of interest was incident post-stroke dementia. We adopted a current consensus definition of post-stroke dementia, which includes any subtype of dementia following stroke [2]. Clinical diagnosis of dementia was determined based on Read codes or International Classification of Diseases, 10th revision (ICD-10) diagnosis codes relating to dementia (Supplementary material of Appendix 1) first recorded in the CPRD, HES, or ONS on or after the 91st day following index stroke (Fig. 1).
To explore the potential impact of unmeasured confounding on the risk of dementia associated with statin use, we used coronary heart disease (CHD) as a positive control outcome and fracture and peptic ulcer as two negative control outcomes. The positive control outcome was expected to be affected by statin use while the negative control outcomes were not. These control outcomes were chosen because a similar set of confounders is shared by the relationship between statin use and each control outcome and that between statin use and dementia, which may or may not have been captured in our study, and high-quality evidence from RCTs has established the impact of statin use on these outcomes. Statin use has been shown to reduce the risk of CHD in patients with cerebrovascular disease in the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial and in the Heart Protection Study (HPS) [27, 28]. While observational studies tended to find an inverse association with fracture (likely due to unmeasured confounding and other biases) [29], statins had no effect on the risk of incident fracture in the HPS or in the Justification for the Use of statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) trial [14, 30]. Statins were not associated with any gastrointestinal disorders in SPARCL and HPS or gastrointestinal bleeding in the Study of Heart and Renal Protection (SHARP) trial, which would mainly occur in peptic ulcers [14, 31, 32]. Thus, we expected to observe an inverse association between statin use and CHD but no association of statin use with fracture or peptic ulcer in the absence of residual confounding and other biases in our analysis. These control outcomes were identified using Read codes or ICD-10 diagnosis codes (Supplementary material of Appendix 1) first recorded in the CPRD, HES or ONS on or after the 91st day following index stroke.
Follow-up
Patients in each group who survived beyond the first 90 days of the index stroke contributed to the time-at-risk period of dementia (Fig. 1). For the observational analogue of intention-to-treat (ITT) effect analysis (described below), patients were followed until the date of incident dementia or the date of censoring (death, transfer-out, the last update of the CPRD data [31 July 2018], or the end of 10-year follow-up), whichever occurred first. The whole follow-up period for each patient was split into discrete 30-day (one-month) intervals. In each interval, information was updated on covariates, outcome, and censoring.
For the observational analogue of per-protocol (PP) effect analysis (described below), patients were additionally artificially censored if they discontinued statin treatment in the statin initiation group or started statin treatment in the non-initiation group. The artificial censoring date was the expected end of days-supply (typically 30 days) of the last prescription plus a 90-day grace period for the statin initiators and was the prescription date of the first statin for the non-initiators.
Potential confounders
Depending on the ascertainment time window, three sets of covariates were considered in our analysis for confounding adjustment: baseline characteristics, characteristics by the 90th day of index stroke, and time-varying characteristics (Fig. 1). The baseline covariates included demographics (age, gender, and socioeconomic status measured by Index of Multiple Deprivation [IMD]), comorbidities (atrial fibrillation, alcohol use disorders, CHD, diabetes, heart failure, hyperlipidaemia, hypertension, peripheral artery disease, transient ischemic attack, anxiety, asthma, chronic obstructive pulmonary disease, depression, epilepsy, Parkinson’s disease and rheumatoid arthritis), lifestyle factors (smoking and BMI), healthcare utilisation, and co-medications (anticoagulant, antiplatelet, antidiabetic, antihypertensive and non-statin lipid-lowering treatments). The by-90th-day and time-varying covariates included comorbidities, lifestyle factors, and co-medications. Definitions of these covariates are detailed in Supplementary material of Appendix 2.
Statistical analysis
All analyses were conducted using Stata 15 after quality control (Supplementary material of Appendix 3). Baseline characteristics were compared between the two exposure groups using standardised mean difference (with an absolute value greater than 0.1 indicating meaningful imbalance) [33]. Incidence rate of post-stroke dementia was calculated for each group.
We estimated two types of observational effects of statin use on post-stroke dementia: the effect of initiation versus no initiation (observational analogue of ITT effect) and the effect of sustained use versus no use (observational analogue of PP effect). We estimated the hazard ratios (HRs) and their 95% CIs for both effects using inverse probability weighted marginal structural models in a two-stage process. First, we estimated four types of stabilised weights using a logistic regression: baseline treatment weights (to adjust for baseline confounding), baseline selection weights (for baseline selection bias due to the requirement to survive the first 90 days following the index stroke), follow-up weights (for loss to follow-up) and treatment persistence weights (for non-persistence with the initial treatment). In the second stage, we estimated the two observational effects of interest using a weighted pooled logistic regression model, which approximates a time-dependent Cox model [34]. In the ITT analysis, the primary model was conducted with full adjustment for baseline characteristics, baseline selection bias, and loss to follow-up using the product of baseline treatment weight, baseline selection weight, and follow-up weight. In the PP analysis, the primary model additionally accounted for artificial censoring due to deviation from initial treatment during the time-at-risk period using the product of the four weights. The final weights used in the outcome models were truncated at 1st and 99th percentiles to minimise the impact of extreme weights and to improve precision [35]. We estimated the 95% CIs using a robust variance estimator to account for potential correlation introduced by weighting. Details of the two-step estimation approach are described in Supplementary material of Appendix 4.
To explore how the associations of statin initiation and sustained use with dementia were influenced by more adjustment for potential biases, we fit two nested models: the first model only adjusted for baseline confounding using the baseline treatment weights and the second model additionally adjusted for baseline selection bias using the product of baseline treatment weights and baseline selection weights.
To explore the potential impact of unmeasured confounding on the association between statin use and dementia, we repeated the main analysis of ITT and PP effects for the three control outcomes, with all types of weights re-estimated.
We conducted subgroup analysis to explore whether the fully adjusted estimates for dementia differed by age group (18–64, 65–74, 75–84, and ≥ 85 years), gender, stroke subtype (ischaemic and haemorrhagic), and baseline cardiovascular risk factors including atrial fibrillation, heart failure, CHD, peripheral artery disease, transient ischaemic attack, diabetes, hyperlipidaemia, and hypertension. We tested the subgroup difference by including an interaction term to the primary full adjustment models, in which a Bonferroni correction was applied to the significance level that divided 0.05 by 11 subgroups examined (i.e., 0.0045).
Several sensitivity analyses were conducted to examine the robustness of the main results: (1) using original weights, truncation of weights at 0.5th and 99.5th percentiles, or truncation at 0.1 and 10; (2) instead of excluding patients with missing baseline covariates, imputing the missing baseline BMI with 5th or 95th percentiles and assuming missing smoking status as never smoking; (3) separating unspecified stroke from ischaemic stroke subtype; (4) excluding patients without linkage to HES; (5) further excluding any patients with dementia occurring between months 4 and 6 following the index stroke; (6) varying the time window for statin initiation assessment to 1 or 6 months after index stroke, with the time-at-risk period of dementia starting from the 2nd or 7th month of stroke, respectively; and (7) varying the grace period to 1 or 5 months for defining statin discontinuation in the PP analysis. (8) As our negative control outcome analysis showed a significant association between statin use and fracture, we conducted a post-hoc exploratory analysis by including fracture in our weight models, and also performed an indirect adjustment for unmeasured confounding by assuming that the potential associations between the unmeasured confounders and dementia and fracture would be similar in magnitude [36]. For sensitivity analyses (2) to (8), we re-estimated all types of weights considering the study population, statin initiation definition, covariates, or treatment persistence definition were different from those in the main analysis.
Results
Patient inclusion and baseline characteristics
Of 68,677 patients with an incident stroke recorded in the CPRD, 33,190 (mean age, 71.9 years, with about 96.0% of patients aged 45 years or older; female, 51.9%) were included in the study (Fig. 2). Among these eligible patients, 18,577 patients (56.0%) received a statin during the first 90 days after the index stroke (Table 1). Statin initiators were more likely to be younger, males, current smokers, suffer an ischaemic stroke, and have a higher BMI. They tended to have fewer CHD, atrial fibrillation, diabetes, heart failure, hypertension, hearing loss, and cardiovascular related co-medications. Patients excluded from the main analysis due to missing data at baseline (n = 4844) tended to have fewer comorbidities and receive less pre-stroke treatment (Supplementary material of Appendix 5). Within the first 90 days following stroke, 133 patients died and 145 transferred out of their practices in the statin group, while 2774 died and 537 transferred out in the no statin group. Patients who survived during this period tended to have fewer comorbidities and receive less pre-stroke treatment (Supplementary material of Appendix 5).
Flow chart of patient inclusion. a All the 68,677 patients identified in the CPRD were considered potentially eligible, regardless of whether they could be linked to other data sources. b Only those who had consented to participate in the CPRD linkage scheme had HES data (covering about 58% of all UK CPRD practices). Only those who died had linked ONS data. 38,616 patients had patient-level IMD and the other 30,061 patients had practice-level IMD. c The number was not exclusive, with missing smoking data in 344 patients and missing BMI in 4755 patients. d To control potential selection bias, censoring was accounted for using inverse probability weighting in the adjustment models. CPRD, Clinical Practice Research Datalink; HES, Hospital Eisode Statistics; IMD, Index of Multiple Deprivation; ONS, Office for National Statistics
Incidence of post-stroke dementia
Among the 29,601 patients who survived through the first 90 days after the index stroke, 3176 patients (10.7%) were diagnosed with dementia over a mean follow-up of 4.8 years (5.2 years for statin initiators and 4.2 years for statin non-initiators). The incidence of post-stroke dementia was 18.0 per 1000 person-years and 30.6 per 1000 person-years, respectively (Table 2 and Supplementary material of Appendix 6).
Association of statin use with post-stroke dementia
Compared with the crude model, adjustment for baseline characteristics (Model 1) led to a large numerical difference in effect estimate (Table 2). Progressive adjustment for baseline selection and loss to follow-up (Models 2 and 3) did not lead to further large changes. In the fully adjusted model (Model 3), statin initiation was associated with a 30% (95% CI 25%-36%, P < 0.001) reduction in the risk of dementia compared with no statin initiation (aHRITT 0.70, 95% CI 0.64–0.75, P < 0.001) (Table 2). When non-persistence was further accounted for, sustained statin use was associated with a 45% (95% CI 38–50%, P < 0.001) reduction in the risk of dementia (aHRPP 0.55, 95% CI 0.50–0.62, P < 0.001) compared to no statin use. The estimated stabilised weights were statistically well distributed, with a mean of 1 and no extremely large weights after truncation at 1st and 99th percentiles (Supplementary material of Appendix 7), suggesting no gross misspecification of the weight models.
Association of statin use with control outcomes
The parallel analyses for CHD (positive control outcome) and peptic ulcer (negative control outcome) suggested that unmeasured confounders which may bias the association of statin use with these two outcomes were not likely to distort the inverse association between statin use and dementia (Table 3). In the full adjustment models, statin initiation was associated with decreased risk of CHD (aHRITT 0.87, 95% CI 0.79–0.95; aHRPP 0.70, 95% CI 0.62–0.80). There was no evidence of an association between statin use and peptic ulcer (aHRITT 1.03, 95% CI 0.82–1.29; aHRPP 1.09, 95% CI 0.77–1.54) but evidence of a lower risk of fracture with statin use (aHRITT 0.88, 95% CI 0.80–0.96; aHRPP 0.86, 95% CI 0.75–0.98). Weights after truncation at 1st and 99th percentiles used in the models were statistically well distributed, with means close to one and no extremely large weights (Supplementary material of Appendix 7).
Subgroup analysis
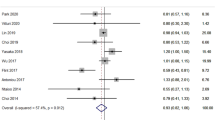
The association of statin initiation with post-stroke dementia was stronger in patients with no hyperlipidaemia than in those with hyperlipidaemia in the ITT analysis (P for interaction = 0.031) (Fig. 3). However, the difference became statistically non-significant after Bonferroni correction. No differences were observed between stroke subtypes or other pre-specified subgroups in the ITT or PP analysis.
Subgroup analysis for statin use. All the outcome models adjusted for baseline characteristics, baseline selection, loss to follow-up and months of follow-up. For PP analysis, artificial censoring due to deviation from initial treatment during time-at-risk period was additionally accounted for. CI, confidence interval
Sensitivity analysis
In general, results from the main analysis were robust under different sensitivity analyses (Supplementary material of Appendix 8). The only difference between the main analysis and sensitivity analyses was that the association of statin use with CHD (in ITT analysis) and fracture (in PP analysis) was not significant when the original (i.e., untruncated) weights were used in the models (Supplementary material of Appendix 8). However, the point estimates changed little with different weight truncation criteria. When including fracture in the full adjustment model for dementia, there was little change to our main findings in both ITT and PP analysis (aHRITT 0.70, 95% CI 0.61–0.80; aHRPP 0.55, 95% CI 0.46–0.66). By assuming the impact of unmeasured confounding on the risk of dementia associated with statin use was similar to that of fracture, the fully adjusted association for dementia attenuated but remained significant (aHRITT 0.80, 95% CI 0.70–0.90; aHRPP 0.64, 95% CI 0.54–0.76).
Discussion
Summary of principal findings
In this study, statin initiation within the first 3 months after an incident stroke (most aged at least 45 years) was associated with a decreased risk of dementia (ITT analysis). When additionally accounting for treatment persistence over time, the magnitude of effect estimate became stronger, with about 50% reduction in the risk of post-stroke dementia in patients with sustained use of statins (PP analysis). One possible explanation is that an ITT analysis is generally more susceptible to exposure misclassification during follow-up, which would bias the results toward the null in our statin use versus non-use comparison. The findings may also suggest enhanced persistence with statin use could potentially lower the risk of post-stroke dementia. There was no clear evidence that the association of statin use with risk of dementia differed by stroke subtype or other pre-specified baseline patient characteristics examined in our subgroup analysis. The observed association may be overestimated in part due to unmeasured confounding which could also affect the association of statin use with fracture but not that with CHD or peptic ulcer. However, indirect adjustment for unmeasured confounding did not substantially change the inverse association. A series of sensitivity analysis to explore the impact of potential bias sources did not show any appreciable changes to our main findings. It should be noted that statin initiators in our study were younger and had fewer comorbidities than no statin initiators (Table 1) due to exclusion of pre-stroke statin users, a design decision aimed to reduce prevalent-user bias [37, 38] but could reduce the generalisability of our main findings to all stroke patients [39].
Strengths and limitations
Compared with previous studies, this study included the largest sample size to date to investigate the association between statin use and post-stroke dementia. This study used a clear definition of statin initiation, new-user design (excluding prevalent statin users) and inverse probability weighted marginal structural models to account for potential selection bias and confounding. Control outcomes were used to assess the impact of unmeasured confounding. This study also benefits from the strengths of the CPRD data, such as representativeness of real practice settings, detailed prescription information, large sample size, and long-term follow-up [25].
However, there are some limitations in this study. First, unmeasured confounding likely existed as indicated by an observed association of statins with fracture (a negative control outcome). Unmeasured confounders shared between both associations for dementia and fracture in our study likely include (but are not limited to) recurrent stroke, ethnicity, education attainment, physical activity, dietary/supplementation (such as vitamin D and calcium), and baseline cognitive function [40, 41], which are poorly recorded in the CPRD and HES. We did not have information on stroke severity, which may be associated with both statin initiation and dementia risk. However, our sensitivity analysis restricting to those who survived for at least six months after stroke, which would have excluded most severe strokes, showed similar results to our main findings. In addition, patient and practitioner preference for statin use, which could reflect underlying health conditions associated with the risk of dementia, was not captured in the databases. While unmeasured confounding may be mitigated by an active comparator (ideally initiators of other lipid-lowering monotherapy), this was not feasible in our new-user study due to very limited number of people initiating these drugs (only 108 initiators among eligible stroke survivors, with 11 developing incident dementia during follow-up).
Second, differential misclassification of measured baseline and time-varying covariates (mainly in relation to diagnosis of comorbidities) may have also resulted in residual confounding. This misclassification was more likely to occur in statin initiators due to less contact with health services (Table 1), with unpredictable impact on our effect estimates. Similarly, as dementia was not systematically assessed in all stroke patients, misclassification can also occur in relation to the issue of underdiagnosis of dementia in clinical practice [42], in particular among statin initiators who had less contact with general practitioners (Table 1). In this case, the real association would be weaker than our estimates. However, the incidence of post-stroke dementia observed in our study was in line with that in the general population when accounting for the higher risk of dementia in stroke patients (Supplementary material of Appendix 6). As per the current consensus definition of post-stroke dementia [2], our study was focused on any dementia, without considering dementia subtype or mild cognitive impairment, which were poorly recorded in the CPRD.
Third, while censoring due to death and transfer-out has been accounted for, the association may still be overestimated to some extent due to death and transfer-out as competing events. Fourth, ideally, separate weights should be calculated for death and transfer-out as their causes might differ. However, this was not feasible due to model convergence issues. For the same reason, overall weights, rather than subgroup-specific weights, were used in the subgroup analysis, which might introduce residual confounding. Fifth, weight truncation might also lead to residual confounding [35]. However, sensitivity analysis using original weights or other truncation criteria still suggested the inverse association of statin use with dementia. Sixth, we defined statin initiation and sustained use based on statin prescriptions, which did not necessarily mean uptake of the medications. Furthermore, there were missing data for stroke subtype, BMI, and smoking. However, this limitation was unlikely to have an important impact on the results as sensitivity analyses dealing with missing data did not materially change the results.
Comparisons with other studies and possible mechanisms
No trials have investigated the effect of statins on the risk of dementia in stroke patients [23]. Only two observational studies have reported on the association of statins with post-stroke dementia [43, 44]. In one study, the inverse association was not statistically significant (crude OR 0.89, 95% CI 0.65–1.21, with no adjusted estimate reported) [43]. The other study suggested a significant inverse association (adjusted HR 0.81, 95% CI 0.73–0.89) with adjustment for age, sex, socioeconomic status, baseline comorbidities and co-medications [44]. Our study found a stronger association of statin use with dementia. Our attempt to overcome the limitations in the previous studies, such as prevalent user bias, immortal time bias, time-varying confounding, and treatment non-persistence, could partially explain the difference in findings. While the exact mechanisms of statins on cognitive protection have not been elucidated, statins may lower the risk of post-stroke dementia by preventing recurrent stroke [45], reducing the production of amyloid-β peptides and neurofibrillary tangles [46, 47], and exerting pleiotropic effects [48].
In terms of the control outcomes, we observed a smaller protective effect on CHD risk in our ITT estimate but a similar risk in our PP analysis when compared with the RCTs [27, 28]. We did not observe an association with peptic ulcer, as would have been anticipated from the trials [14, 31, 32], suggesting the observed association of statin use with dementia would not be substantially confounded by the unmeasured factors shared with that between statin use and peptic ulcer, such as diet, alcohol consumption, gastrointestinal related drugs and gut microbiota. We found that statin use, contrary to the trial results, was associated with a reduced risk of fracture [14, 30]. The lower risk of fracture found in our study suggests the possibility of unmeasured confounding by healthy user effects or the possibility of statins reducing the risk of falls associated with fracture by preventing dementia. This inverse association with fracture was also observed in other observational studies [49], including in stroke patients (aHR 0.66, 95% CI 0.58–0.76) [50].
Implications for practice
We found no evidence that statin use after stroke could accelerate cognitive deterioration as previous studies reported [16,17,18,19,20], but rather was associated with reduced risk of dementia, regardless of stroke subtype. This potential benefit might be enhanced through greater persistence with statins. This underlines the importance of interventions to tackle non-persistence, which has been recognised to compromise the effectiveness of statins in the prevention of ASCVD [6, 7]. Given the potential benefit of statins in preventing post-stroke dementia does not vary by age or cardiovascular risk factors, efforts should be made to increase uptake particularly in older patients and in those without prior cardiovascular risk factors, who have been shown to be less likely to be on statin treatment after stroke [51].
Implications for future research
Confirmatory evidence of the effect of statins on preventing dementia is needed. The ongoing placebo-controlled trial, Pragmatic Evaluation of Events and Benefits of Lipid-Lowering in Older Adults (PREVENTABLE), assesses the overall benefits and risks of statins for preventing dementia in 20,000 adults aged 75 years or older without cardiovascular disease [52]. Such a trial would not be possible to conduct in ischaemic stroke because of the proven benefits in reducing risk of future cardiovascular events [3,4,5]. Since our study only provided evidence on the average estimate of association for statin use regardless of potencies and doses, further real-world evidence could illuminate whether potency, dose, and lipophilicity of statins can influence the risk of dementia following ischaemic stroke. With cumulative observational evidence on functional benefits of statins for intracerebral haemorrhage [53, 54], cognitive outcomes could be assessed in future statin trials conducted in these patients. Development and testing of interventions to enhance the use of and persistence with statins after stroke are needed.
Conclusions
Statin initiation after stroke was associated with a lower risk of dementia, regardless of stroke subtype. This potential benefit is greater in patients persistent with statins. The observed association between statin use and post-stroke dementia may be overestimated in part due to unmeasured confounding shared with the association between statin use and fracture. Further trials with cognitive outcomes and more real-world observational evidence are needed to confirm the potential benefit of statins for preventing post-stroke dementia.
Data availability
The data that support the findings of this study are available from CPRD but restrictions apply to the availability of these data, which were used under licence for the current study, and so are not publicly available.
References
Pendlebury ST, Rothwell PM. Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: a systematic review and meta-analysis. Lancet Neurol. 2009;8(11):1006–18. https://doi.org/10.1016/S1474-4422(09)70236-4.
Mijajlovic MD, Pavlovic A, Brainin M, et al. Post-stroke dementia: a comprehensive review. BMC Med. 2017;15(1):11. https://doi.org/10.1186/s12916-017-0779-7.
NICE Guideline. Cardiovascular disease: risk assessment and reduction, including lipid modification. 2014. Accessed 10 September 2020. Available from: https://www.nice.org.uk/guidance/cg181/chapter/1-recommendations.
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88. https://doi.org/10.1093/eurheartj/ehz455.
Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1046–81. https://doi.org/10.1161/CIR.0000000000000624.
Bates TR, Connaughton VM, Watts GF. Non-adherence to statin therapy: a major challenge for preventive cardiology. Expert Opin Pharmacother. 2009;10(18):2973–85. https://doi.org/10.1517/14656560903376186.
De Vera MA, Bhole V, Burns LC, Lacaille D. Impact of statin adherence on cardiovascular disease and mortality outcomes: a systematic review. Br J Clin Pharmacol. 2014;78(4):684–98. https://doi.org/10.1111/bcp.12339.
Hemphill JC, Greenberg SM, Anderson CS, et al. Guidelines for the management of spontaneous intracerebral hemorrhage a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46(7):2032–60. https://doi.org/10.1161/Str.0000000000000069.
Larsson SC, Markus HS. Does treating vascular risk factors prevent dementia and Alzheimer’s disease? A systematic review and meta-analysis. J Alzheimers Dis. 2018;64(2):657–68. https://doi.org/10.3233/Jad-180288.
Xu W, Tan L, Wang HF, et al. Meta-analysis of modifiable risk factors for Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2015;86(12):1299–306. https://doi.org/10.1136/jnnp-2015-310548.
Macedo AF, Taylor FC, Casas JP, Adler A, Prieto-Merino D, Ebrahim S. Unintended effects of statins from observational studies in the general population: systematic review and meta-analysis. BMC Med. 2014;12:51. https://doi.org/10.1186/1741-7015-12-51.
Swiger KJ, Manalac RJ, Blumenthal RS, Md MJB, Martin SS. Statins and cognition: a systematic review and meta-analysis of short- and long-term cognitive effects. Mayo Clin Proc. 2013;88(11):1213–21. https://doi.org/10.1016/j.mayocp.2013.07.013.
Power MC, Weuve J, Sharrett AR, Blacker D, Gottesman RF. Statins, cognition, and dementia-systematic review and methodological commentary. Nat Rev Neurol. 2015;11(4):220–9. https://doi.org/10.1038/nrneurol.2015.35.
Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360(9326):7–22. https://doi.org/10.1016/S0140-6736(02)09327-3.
Trompet S, van Vliet P, de Craen AJM, et al. Pravastatin and cognitive function in the elderly. Results of the PROSPER study. J Neurol. 2010;257(1):85–90. https://doi.org/10.1007/s00415-009-5271-7.
Evans MA, Golomb BA. Statin-associated adverse cognitive effects: survey results from 171 patients. Pharmacotherapy. 2009;29(7):800–11. https://doi.org/10.1592/phco.29.7.800.
Orsi A, Sherman O, Woldeselassie Z. Simvastatin-associated memory loss. Pharmacotherapy. 2001;21(6):767–9. https://doi.org/10.1592/phco.21.7.767.34577.
Wagstaff LR, Mitton MW, Arvik BM, Doraiswamy PM. Statin-associated memory loss: analysis of 60 case reports and review of the literature. Pharmacotherapy. 2003;23(7):871–80. https://doi.org/10.1592/phco.23.7.871.32720.
Muldoon MF, Barger SD, Ryan CM, et al. Effects of lovastatin on cognitive function and psychological well-being. Am J Med. 2000;108(7):538–46. https://doi.org/10.1016/s0002-9343(00)00353-3.
Muldoon MF, Ryan CM, Sereika SM, Flory JD, Manuck SB. Randomized trial of the effects of simvastatin on cognitive functioning in hypercholesterolemic adults. Am J Med. 2004;117(11):823–9. https://doi.org/10.1016/j.amjmed.2004.07.041.
WHO. Risk reduction of cognitive decline and dementia: WHO Guidelines. Geneva, USA: WHO. 2019.
Brainin M, Tuomilehto J, Heiss WD, et al. Post-stroke cognitive decline: an update and perspectives for clinical research. Eur J Neurol. 2015;22(2):229-e16. https://doi.org/10.1111/ene.12626.
Yang Z, Wang H, Edwards D, et al. Association of blood lipids, atherosclerosis and statin use with dementia and cognitive impairment after stroke: a systematic review and meta-analysis. Ageing Res Rev. 2020;57:100962. https://doi.org/10.1016/j.arr.2019.100962.
Bath PM, Scutt P, Blackburn DJ, et al. Intensive versus guideline blood pressure and lipid lowering in patients with previous stroke: main results from the pilot “prevention of decline in cognition after stroke trial” (PODCAST) randomised controlled trial. PLoS ONE. 2017;12(1):e0164608. https://doi.org/10.1371/journal.pone.0164608.
Herrett E, Gallagher AM, Bhaskaran K, et al. Data resource profile: clinical practice research datalink (CPRD). Int J Epidemiol. 2015;44(3):827–36. https://doi.org/10.1093/ije/dyv098.
Padmanabhan S, Carty L, Cameron E, Ghosh RE, Williams R, Strongman H. Approach to record linkage of primary care data from clinical practice research datalink to other health-related patient data: overview and implications. Eur J Epidemiol. 2019;34(1):91–9. https://doi.org/10.1007/s10654-018-0442-4.
Amarenco P, Goldstein LB, Sillesen H, et al. Coronary heart disease risk in patients with stroke or transient ischemic attack and no known coronary heart disease findings from the stroke prevention by aggressive reduction in cholesterol levels (SPARCL) trial. Stroke. 2010;41(3):426–30. https://doi.org/10.1161/Strokeaha.109.564781.
Collins R, Armitage J, Parish S, Sleight P, Peto R, Heart Protection Study Collaborative Group. Effects of cholesterol-lowering with simvastatin on stroke and other major vascular events in 20536 people with cerebrovascular disease or other high-risk conditions. Lancet. 2004;363(9411):757–67. https://doi.org/10.1016/S0140-6736(04)15690-0.
Toh S, Hernandez-Diaz S. Statins and fracture risk. A systematic review. Pharmacoepidemiol Drug Saf. 2007;16(6):627–40. https://doi.org/10.1002/pds.1363.
Pena JM, Aspberg S, MacFadyen J, Glynn RJ, Solomon DH, Ridker PM. Statin therapy and risk of fracture: results from the JUPITER randomized clinical trial. JAMA Intern Med. 2015;175(2):171–7. https://doi.org/10.1001/jamainternmed.2014.6388.
Amarenco P, Bogousslavsky J, Callahan A 3rd, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355(6):549–59. https://doi.org/10.1056/NEJMoa061894.
Reith C, Staplin N, Herrington WG, et al. Effect on non-vascular outcomes of lowering LDL cholesterol in patients with chronic kidney disease: results from the study of heart and renal protection. BMC Nephrol. 2017;18(1):147. https://doi.org/10.1186/s12882-017-0545-2.
Mamdani M, Sykora K, Li P, et al. Reader’s guide to critical appraisal of cohort studies: 2. Assessing potential for confounding. BMJ. 2005;330(7497):960–2. https://doi.org/10.1136/bmj.330.7497.960.
Dagostino RB, Lee ML, Belanger AJ, Cupples LA, Anderson K, Kannel WB. Relation of pooled logistic-regression to time-dependent Cox regression analysis: the Framingham Heart Study. Stat Med. 1990;9(12):1501–15. https://doi.org/10.1002/sim.4780091214.
Cole SR, Hernan MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168(6):656–64. https://doi.org/10.1093/aje/kwn164.
Richardson DB, Laurier D, Schubauer-Berigan MK, Tchetgen Tchetgen E, Cole SR. Assessment and indirect adjustment for confounding by smoking in cohort studies using relative hazards models. Am J Epidemiol. 2014;180(9):933–40. https://doi.org/10.1093/aje/kwu211.
Danaei G, Tavakkoli M, Hernan MA. Bias in observational studies of prevalent users: lessons for comparative effectiveness research from a meta-analysis of statins. Am J Epidemiol. 2012;175(4):250–62. https://doi.org/10.1093/aje/kwr301.
Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158(9):915–20. https://doi.org/10.1093/aje/kwg231.
Filion KB, Yu YH. Invited commentary: the prevalent new-user design in pharmacoepidemiology-challenges and opportunities. Am J Epidemiol. 2021;190(7):1349–52. https://doi.org/10.1093/aje/kwaa284.
Wehren LE, Magaziner J. Hip fracture: risk factors and outcomes. Curr Osteoporos Rep. 2003;1(2):78–85. https://doi.org/10.1007/s11914-003-0013-8.
Chen JH, Lin KP, Chen YC. Risk factors for dementia. J Formos Med Assoc. 2009;108(10):754–64. https://doi.org/10.1016/S0929-6646(09)60402-2.
Connolly A, Gaehl E, Martin H, Morris J, Purandare N. Underdiagnosis of dementia in primary care: variations in the observed prevalence and comparisons to the expected prevalence. Aging Ment Health. 2011;15(8):978–84. https://doi.org/10.1080/13607863.2011.596805.
Biffi A, Bailey D, Anderson CD, et al. Risk factors associated with early vs delayed dementia after intracerebral hemorrhage. JAMA Neurol. 2016;73(8):969–76.
Pan ML, Hsu CC, Chen YM, Yu HK, Hu GC. Statin use and the risk of dementia in patients with stroke: a nationwide population-based cohort study. J Stroke Cerebrovasc Dis. 2018;27(11):3001–7.
McGuinness B, Craig D, Bullock R, Passmore P. Statins for the prevention of dementia. Cochrane Database Syst Rev. 2016;1:CD003160. https://doi.org/10.1002/14651858.CD003160.pub3.
Shobab LA, Hsiung GY, Feldman HH. Cholesterol in Alzheimer’s disease. Lancet Neurol. 2005;4(12):841–52. https://doi.org/10.1016/s1474-4422(05)70248-9.
Kandiah N, Feldman HH. Therapeutic potential of statins in Alzheimer’s disease. J Neurol Sci. 2009;283(1–2):230–4. https://doi.org/10.1016/j.jns.2009.02.352.
Miida T, Takahashi A, Ikeuchi T. Prevention of stroke and dementia by statin therapy: experimental and clinical evidence of their pleiotropic effects. Pharmacol Ther. 2007;113(2):378–93. https://doi.org/10.1016/j.pharmthera.2006.09.003.
Shi R, Mei Z, Zhang Z, Zhu Z. Effects of statins on relative risk of fractures for older adults: an updated systematic review with meta-analysis. J Am Med Dir Assoc. 2019;20(12):1566-78.e3. https://doi.org/10.1016/j.jamda.2019.06.027.
Lin SM, Wang JH, Liang CC, Huang HK. Statin use is associated with decreased osteoporosis and fracture risks in stroke patients. J Clin Endocrinol Metab. 2018;103(9):3439–48. https://doi.org/10.1210/jc.2018-00652.
Yang Z, Edwards D, Massou E, Saunders CL, Brayne C, Mant J. Statin use and high-dose statin use after ischemic stroke in the UK: a retrospective cohort study. Clin Epidemiol. 2019;11:495–508. https://doi.org/10.2147/CLEP.S201983.
NCT04262206. Pragmatic evaluation of events and benefits of lipid-lowering in older adults (PREVENTABLE). 2020. Accessed 10 September 2020. Available from: clinicaltrials.gov/ct2/show/NCT04262206.
Jung JM, Choi JY, Kim HJ, Seo WK. Statin use in spontaneous intracerebral hemorrhage: a systematic review and meta-analysis. Int J Stroke. 2015;10(Suppl A100):10–7. https://doi.org/10.1111/ijs.12624.
Ziff OJ, Banerjee G, Ambler G, Werring DJ. Statins and the risk of intracerebral haemorrhage in patients with stroke: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2019;90(1):75–83. https://doi.org/10.1136/jnnp-2018-318483.
Acknowledgements
We thank the CPRD@Cambridge team for developing the code lists used in this study. We thank Dr. Jessica Young (Department of Population Medicine, Harvard Medical School & Harvard Pilgrim Health Care Institute) for her advice on inverse probability weighted marginal structural model analysis.
Funding
This work was supported by an independent grant from the National Institute for Health Research (NIHR) School of Primary Care Research [SPCR-2014-10043, reference number 340]. Mant and Brayne are NIHR Senior Investigators. Yang was supported by the Cambridge Commonwealth, European and International Trust. Li was supported in part by NIH/NIA R03AG070661. The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The views expressed are those of the authors and not necessarily those of the National Health Service, the National Institute for Health Research, the National Institutes of Health, or the Department of Health in the United Kingdom.
Author information
Authors and Affiliations
Contributions
Conceptualisation: ZY, JM; Data curation: ZY, DE; Statistical analysis: ZY, ST, XL; Methodology: ZY, ST, XL, JM; Result interpretation: ZY, ST, XL, DE, CB, JM; Writing—original draft: ZY, JM; Writing—review & editing: ZY, ST, XL, DE, CB, JM.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest related to the submitted work.
Ethics approval and consent to participate
Ethics approval was obtained from the Independent Scientific Advisory Committee of the CPRD (protocol number 17_201R), with no written consent from participants required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yang, Z., Toh, S., Li, X. et al. Statin use is associated with lower risk of dementia in stroke patients: a community-based cohort study with inverse probability weighted marginal structural model analysis. Eur J Epidemiol 37, 615–627 (2022). https://doi.org/10.1007/s10654-022-00856-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-022-00856-7