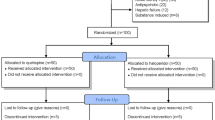
Abstract
Neuroinflammation is associated with the development of hypoactive delirium, which results in poor clinical outcomes. Drugs effective against hypoactive sur have not yet been established. Yokukansan has an anti-neuroinflammatory effect, making it potentially effective against hypoactive delirium. This study aimed to examine the effect of Yokukansan on the pentobarbital-induced loss of righting reflex duration extended with lipopolysaccharide (LPS)-induced neuroinflammation and diazepam-induced gamma-aminobutyric acid receptor stimulation in a mouse model. The active ingredients in Yokukansan and its anti-neuroinflammatory effect on the hippocampus were also investigated. Furthermore, we examined the in vitro anti-inflammatory effects of Yokukansan on LPS-stimulated BV2 cells, a murine microglial cell line. Findings revealed that treatment with Yokukansan significantly decreased the duration of pentobarbital-induced loss of righting reflex by attenuating the LPS-induced increase in interleukin-6 and tumor necrosis factor-alpha levels in the hippocampus. Moreover, treatment with Yokukansan significantly decreased the number of ionized calcium-binding adapter molecule-1-positive cells in the hippocampal dentate gyrus after 24 h of LPS administration. In addition, glycyrrhizic acid, an active ingredient in Yokukansan, partially decreased the duration of pentobarbital-induced loss of righting reflex. Treatment with Yokukansan also suppressed the expression of inducible nitric oxide, interleukin-6, and tumor necrosis factor mRNA in LPS-stimulated BV2 cells. Thus, these findings suggest that Yokukansan and glycyrrhizic acid may be effective therapeutic agents for treating neuroinflammation-induced hypoactive delirium.
Graphical abstract









Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Material availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Alam A, Hana Z, Jin Z, Suen KC, Ma D (2018) Surgery, neuroinflammation and cognitive impairment. EBioMedicine 37:547–556. https://doi.org/10.1016/j.ebiom.2018.10.021
Yang T, Velagapudi R, Terrando N (2020) Neuroinflammation after surgery: from mechanisms to therapeutic targets. Nat Immunol 21:1319–1326. https://doi.org/10.1038/s41590-020-00812-1
Simone MJ, Tan ZS (2011) The role of inflammation in the pathogenesis of delirium and dementia in older adults: a review. CNS Neurosci Ther 17:506–513. https://doi.org/10.1111/j.1755-5949.2010.00173.x
Wang Y, Shen X (2018) Postoperative delirium in the elderly: the potential neuropathogenesis. Aging Clin Exp Res 30:1287–1295. https://doi.org/10.1007/s40520-018-1008-8
Muangpaisan W, Wongprikron A, Srinonprasert V, Suwanpatoomlerd S, Sutipornpalangkul W, Assantchai P (2015) Incidence and risk factors of acute delirium in older patients with hip fracture in Siriraj Hospital. J Med Assoc Thai 98:423–430
Raats JW, Steunenberg SL, de Lange DC, van der Laan L (2016) Risk factors of post–operative delirium after elective vascular surgery in the elderly: a systematic review. Int J Surg 35:1–6. https://doi.org/10.1016/j.ijsu.2016.09.001
Cascella M, Fiore M, Leone S, Carbone D, Di Napoli R (2019) Current controversies and future perspectives on treatment of intensive care unit delirium in adults. World J Crit Care Med 8:18–27. https://doi.org/10.5492/wjccm.v8.i3.18
Wilson JE, Mart MF, Cunningham C, Shehabi Y, Girard TD, MacLullich AMJ, Slooter AJC, Ely EW (2020) Delirium. Nat Rev Dis Primers 6:90. https://doi.org/10.1038/s41572-020-00223-4
Henry CJ, Huang Y, Wynne A, Hanke M, Himler J, Bailey MT, Sheridan JF, Godbout JP (2008) Minocycline attenuates lipopolysaccharide (LPS)–induced neuroinflammation, sickness behavior, and anhedonia. J Neuroinflammation 5:15. https://doi.org/10.1186/1742-2094-5-15
Kitamura Y, Hongo S, Yamashita Y, Yagi S, Otsuki K, Miki A, Okada A, Ushio S, Esumi S, Sendo T (2019) Influence of lipopolysaccharide on diazepam–modified loss of righting reflex duration by pentobarbital treatment in mice. Eur J Pharmacol 842:231–238. https://doi.org/10.1016/j.ejphar.2018.10.049
Sieghart W (1995) Structure and pharmacology of gamma–aminobutyric acid A receptor subtypes. Pharmacol Rev 47:181–234
Marcantonio ER, Juarez G, Goldman L, Mangione CM, Ludwig LE, Lind L, Katz N, Cook EF, Orav EJ, Lee TH (1994) The relationship of postoperative delirium with psychoactive medications. JAMA 272:1518–1522. https://doi.org/10.1001/jama.1994.03520190064036
Furukawa K, Tomita N, Uematsu D, Okahara K, Shimada H, Ikeda M, Matsui T, Kozaki K, Fujii M, Ogawa T, Umegaki H, Urakami K, Nomura H, Kobayashi N, Nakanishi A, Washimi Y, Yonezawa H, Takahashi S, Kubota M, Wakutani Y, Ito D, Sasaki T, Matsubara E, Une K, Ishiki A, Yahagi Y, Shoji M, Sato H, Terayama Y, Kuzuya M, Araki N, Kodama M, Yamaguchi T, Arai H (2017) Randomized double–blind placebo–controlled multicenter trial of Yokukansan for neuropsychiatric symptoms in Alzheimer’s disease. Geriatr Gerontol Int 17:211–218. https://doi.org/10.1111/ggi.12696
Liu Y, Nakamura T, Toyoshima T, Lu F, Sumitani K, Shinomiya A, Keep RF, Yamamoto T, Tamiya T, Itano T (2014) Ameliorative effects of yokukansan on behavioral deficits in a gerbil model of global cerebral ischemia. Brain Res 1543:300–307. https://doi.org/10.1016/j.brainres.2013.11.015
Ikarashi Y, Mizoguchi K (2016) Neuropharmacological efficacy of the traditional Japanese Kampo medicine yokukansan and its active ingredients. Pharmacol Ther 166:84–95. https://doi.org/10.1016/j.pharmthera.2016.06.018
Sugano N, Aoyama T, Sato T, Kamiya M, Amano S, Yamamoto N, Nagashima T, Ishikawa Y, Masudo K, Taguri M, Yamanaka T, Yamamoto Y, Matsukawa H, Shiraisi R, Oshima T, Yukawa N, Rino Y, Masuda M (2017) Randomized phase II study of TJ–54 (Yokukansan) for postoperative delirium in gastrointestinal and lung malignancy patients. Mol Clin Oncol 7:569–573. https://doi.org/10.3892/mco.2017.1357
Darias V, Abdala S, Martin-Herrera D, Tello ML, Vega S (1998) CNS effects of a series of 1,2,4–triazolyl heterocarboxylic derivatives. Pharmazie 53:477–481
Wolfman C, Viola H, Marder M, Wasowski C, Ardenghi P, Izquierdo I, Paladini AC, Medina JH (1996) Anxioselective properties of 6,3’–dinitroflavone, a high–affinity benzodiazepine receptor ligand. Eur J Pharmacol 318:23–30. https://doi.org/10.1016/S0014-2999(96)00784-4
Hui B, Yao X, Zhang L, Zhou Q (2020) Dexamethasone sodium phosphate attenuates lipopolysaccharide-induced neuroinflammation in microglia BV2 cells. Naunyn Schmiedebergs Arch Pharmacol 393:1761–1768. https://doi.org/10.1007/s00210-019-01775-3
Serantes R, Arnalich F, Figueroa M, Salinas M, Andrés-Mateos E, Codoceo R, Renart J, Matute C, Cavada C, Cuadrado A, Montiel C (2006) Interleukin–1beta enhances GABAA receptor cell–surface expression by a phosphatidylinositol 3–kinase/Akt pathway: relevance to sepsis–associated encephalopathy. J Biol Chem 281:14632–14643. https://doi.org/10.1074/jbc.M512489200
Kassie GM, Nguyen TA, Kalisch Ellett LM, Pratt NL, Roughead EE (2017) Preoperative medication use and postoperative delirium: a systematic review. BMC Geriatr 17:298. https://doi.org/10.1186/s12877-017-0695-x
Dehkordi NG, Noorbakhshnia M, Ghaedi K, Esmaeili A, Dabaghi M (2015) Omega–3 fatty acids prevent LPS–induced passive avoidance learning and memory and CaMKII–α gene expression impairments in hippocampus of rat. Pharmacol Rep 67:370–375. https://doi.org/10.1016/j.pharep.2014.10.014
Mirahmadi SM, Shahmohammadi A, Rousta AM, Azadi MR, Fahanik-Babaei J, Baluchnejadmojarad T, Roghani M (2018) Soy isoflavone genistein attenuates lipopolysaccharide–induced cognitive impairments in the rat via exerting anti–oxidative and anti–inflammatory effects. Cytokine 104:151–159. https://doi.org/10.1016/j.cyto.2017.10.008
Cazareth J, Guyon A, Heurteaux C, Chabry J, Petit-Paitel A (2014) Molecular and cellular neuroinflammatory status of mouse brain after systemic lipopolysaccharide challenge: importance of CCR2/CCL2 signaling. J Neuroinflammation 11:132. https://doi.org/10.1186/1742-2094-11-132
Egashira N, Nogami A, Iwasaki K, Ishibashi A, Uchida N, Takasaki K, Mishima K, Nishimura R, Oishi R, Fujiwara M (2011) Yokukansan enhances pentobarbital-induced sleep in socially isolated mice: possible involvement of GABA(A)-benzodiazepine receptor complex. J Pharmacol Sci 116:316–320. https://doi.org/10.1254/jphs.11079SC
Egashira N, Goto Y, Iba H, Kawanaka R, Takahashi R, Taniguchi C, Watanabe T, Kubota K, Katsurabayashi S, Iwasaki K (2021) Kamishoyosan potentiates pentobarbital-induced sleep in socially isolated, ovariectomized mice. J Ethnopharmacol 281:114585. https://doi.org/10.1016/j.jep.2021.114585
Furuya M, Miyaoka T, Tsumori T, Liaury K, Hashioka S, Wake R, Tsuchie K, Fukushima M, Ezoe S, Horiguchi J (2013) Yokukansan promotes hippocampal neurogenesis associated with the suppression of activated microglia in Gunn rat. J Neuroinflammation 10:145. https://doi.org/10.1186/1742-2094-10-145
Cheng CY, Ho TY, Lee EJ, Su SY, Tang NY, Hsieh CL (2008) Ferulic acid reduces cerebral infarct through its antioxidative and anti–inflammatory effects following transient focal cerebral ischemia in rats. Am J Chin Med 36:1105–1119. https://doi.org/10.1142/S0192415X08006570
Khaksa G, Zolfaghari ME, Dehpour AR, Samadian T (1996) Anti–inflammatory and anti–nociceptive activity of disodium glycyrrhetinic acid hemiphthalate. Planta Med 62:326–328. https://doi.org/10.1055/s-2006-957894
Nukaya H, Yamashiro H, Fukazawa H, Ishida H, Tsuji K (1996) Isolation of inhibitors of TPA–induced mouse ear edema from Hoelen, Poria cocos. Chem Pharm Bull (Tokyo) 44:847–849. https://doi.org/10.1248/cpb.44.847
Seo MJ, Kim SJ, Kang TH, Rim HK, Jeong HJ, Um JY, Hong SH, Kim HM (2011) The regulatory mechanism of β–eudesmol is through the suppression of caspase–1 activation in mast cell–mediated inflammatory response. Immunopharmacol Immunotoxicol 33:178–185. https://doi.org/10.3109/08923973.2010.491082
Yuan D, Ma B, Yang JY, Xie YY, Wang L, Zhang LJ, Kano Y, Wu CF (2009) Anti–inflammatory effects of rhynchophylline and isorhynchophylline in mouse N9 microglial cells and the molecular mechanism. Int Immunopharmacol 9:1549–1554. https://doi.org/10.1016/j.intimp.2009.09.010
Tabuchi M, Imamura S, Kawakami Z, Ikarashi Y, Kase Y (2012) The blood–brain barrier permeability of 18β-glycyrrhetinic acid, a major metabolite of glycyrrhizin in Glycyrrhiza root, a constituent of the traditional Japanese medicine Yokukansan. Cell Mol Neurobiol 32:1139–1146. https://doi.org/10.1007/s10571-012-9839-x
Song JH, Lee JW, Shim B, Lee CY, Choi S, Kang C, Sohn NW, Shin JW (2013) Glycyrrhizin alleviates neuroinflammation and memory deficit induced by systemic lipopolysaccharide treatment in mice. Molecules 18:15788–15803. https://doi.org/10.3390/molecules181215788
Nomura T, Bando Y, You H, Tanaka T, Yoshida S (2017) Yokukansan reduces cuprizone-induced demyelination in the corpus callosum through anti-inflammatory effects on microglia. Neurochem Res 42:3525–3536. https://doi.org/10.1007/s11064-017-2400-z
Acknowledgements
We would like to thank Soichiro Ushio for his advice on experimental design.
Funding
This work was supported by MEXT/JSPS KAKENHI [Grant number 20H01008].
Author information
Authors and Affiliations
Contributions
KK: conceptualization, methodoloigy, Investigation, writing—original Draft, project administration, funding acquisition. TI: conceptualization, methodology, formal analysis, investigation, writing—review and editing. KJ: validation, investigation, resources, writing—review and editing. SM: investigation. TK: investigation. MN: investigation. SN: investigation. NT: investigation. SY: investigation, data curation. MM: resources, writing—review and editing, supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
Animal experiments were conducted with approval from the Kochi University Animal Experiment Ethics Committee (approval no. N-00028, July 30, 2020).
Consent to participate
Not applicable.
Consent for publiction
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kawada, K., Ishida, T., Jobu, K. et al. Yokukansan suppresses neuroinflammation in the hippocampus of mice and decreases the duration of lipopolysaccharide- and diazepam-mediated loss of righting reflex induced by pentobarbital. J Nat Med 76, 634–644 (2022). https://doi.org/10.1007/s11418-022-01612-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11418-022-01612-7