Abstract
This paper presents findings of a second trial evaluating telephone-based motivational enhancement therapy (MET) to motivate untreated and unadjudicated men who abuse their intimate partners to explore treatment options. Participants’ perceptions of how their abuse is negatively affecting them personally are a highlight of the paper. One hundred forty-one adult men were recruited through social marketing and randomly assigned to the intervention (MET) or comparison (Mail) group. The MET condition consisted of two feedback sessions guided by a personalized feedback report on participants’ intimate partner violence (IPV) and substance use. The Mail condition included a mailed educational brochure on IPV and substance use. Results supported the likely effectiveness of MET in short-term reduction of IPV behavior, marijuana use, and increasing motivation for treatment seeking particularly for participants who reported more adverse consequences of IPV to themselves. Findings emphasize the importance of including a focus in interventions on IPV’s impact on the abusers themselves. The study’s virtual participation and success in reaching and retaining a diverse population of male abusers can contribute to transformative justice and communities looking for alternative early interventions for men of color prior to encountering the criminal justice system.
Similar content being viewed by others
Introduction
Most abusers do not voluntarily enter treatment. A majority of those who enter treatment are mandated and even then many drop out prematurely in their first attempts. Yet those who stay through the initial six sessions tend to complete – a critical factor, as treatment completion leads to better outcomes (Gondolf, 2004), such as reduced frequency and/or severity of abuse. Dosage of six treatment sessions is believed to be sufficient in prompting fundamental shifts towards accountability and intrinsic motivation to engage with treatment. However, research is lacking on intervention approaches that may facilitate abusers’ treatment entry and/or prevent dropout prior to the six-session mark. This paper contributes to the limited early-intervention research on intimate partner violence (IPV) by presenting outcomes of a second randomized controlled trial evaluating a telephone-delivered motivational enhancement therapy (MET) with adult male IPV perpetrators who had a concurrent substance use disorder (SUD) and were neither in counseling nor undergoing adjudication (Mbilinyi et al., 2008, 2011; Roffman et al., 2008).
Intimate partner violence (IPV) affects a substantial proportion of individuals in the United States. One-third of women living in the U.S. (36.4%, 43.6 million) have endured sexual violence, physical violence, and/or stalking perpetrated by an intimate partner (National Intimate Partner and Sexual Violence Survey, Smith et al., 2018), with preliminary evidence of rates increasing by 12–20% in recent years due to stay-at-home orders required by the COVID-19 pandemic (Bourgault et al., 2021; Kofman & Garfin, 2020; Kourti et al., 2021). IPV adversely affects the victim’s health and well-being (Bacchus et al., 2018; Campbell et al., 2018; Laskey et al., 2019; Spencer et al., 2019; Stubbs & Szoeke, 2021), the abuser’s well-being and legal status (Walker et al., 2010), as well as children’s well-being, growth, and parental attachment (Boeckel et al., 2017; Noonan & Pilkington, 2020; Taillieu et al., 2021). The public is also economically burdened by IPV in terms of criminal justice costs, health care costs, and lost productivity (Holmes et al., 2018; Peterson et al., 2018a; Peterson, Kearns, et al., 2018; Peterson, Liu, et al., 2018).
Many who abuse their partners also meet criteria for a SUD, with rates from 43 to 90% depending on questions asked and period of time (Martin et al., 2010; Mbilinyi et al., 2011; Stuart, Moore, et al., 2013; Stuart, Shorey, et al., 2013; Thompson & Kingree, 2006). Among men, past-year alcohol use disorder has been associated with a significant 2.66 increase in the odds of perpetration (Afifi et al., 2012), and abusers who consume alcohol before or during an IPV incident cause more harm to the victim than those who do not (Thompson & Kingree, 2006). Past-year use of other drugs has shown significant associations with even greater odds of perpetration, particularly sedatives, cocaine, and marijuana (AORs = 4.60, 5.96, 3.62, respectively), whereas use of three or more substances in the past year increased the odds over eightfold compared to those with no substance use (Afifi et al., 2012).
Given this common co-occurrence, researchers have sought to combine interventions for IPV and substance use. Cognitive-behavioral interventions integrating IPV and SUD treatment have shown promising, yet mixed results in randomized trials. Kraanen et al (2013) found no treatment effect for IPV nor SUD outcomes with a 16-session program, while Easton et al (2007) found their 12-session program to help reduce substance use during treatment, compared to 12-step facilitation, no significant treatment effects were observed at follow-up. In contrast, the integrated IPV-SUD treatments developed by Easton et al., (2018; 12-session) and Satyanarayana et al., (2016; 8-session) were associated with significantly greater reductions in frequency (d = 0.74) and severity (d = 0.20) of violence, respectively, compared to control conditions. Brief motivational interventions are similarly promising. Stuart, Moore, et al. (2013), found that, compared to standard IPV treatment, augmenting that treatment with a single 90-min intervention motivating change in alcohol use yielded significantly greater reductions in drinking quantity and frequency as well as fewer occasions of severe physical aggression and number of injuries inflicted. Reduced drinking frequency and injury incidence persisted at 6-month follow-up. However, no significant treatment effects were observed at 12-months and effect sizes were small. A 4-session alcohol-focused motivational enhancement therapy for abusive men, developed by Murphy et al (2018), failed to show significant effects for both IPV and alcohol use, while a single session of MET focused on both IPV and substance use developed by Mbilinyi et al (2011) did reduce frequency of physical (d = 0.21) and psychological (d = 0.26) abuse at terminal 30-day follow-up, compared to an education control condition. No significant effects on drinking outcomes were observed. Other brief motivational interventions have shown evidence of improving IPV treatment attendance (Crane & Eckhardt, 2013), improvements in stages of change, and acceptance of responsibility for violence (Kistenmacher & Weiss, 2008). This body of research shows relatively modest and transitory effects, yet, as Clark and Messer (2006) argue, even small proportional reductions in violence translate to a meaningful reduction in the incidence of IPV perpetration.
Due to low prevalence of self-initiated treatment engagement among abusers however, most studies on court-referred populations may underestimate potential treatment efficacy in self-referred individuals. Self-referral to treatment for behavioral issues such as SUD is daunting for many individuals. Reaching out can seem insurmountably difficult even for a man who yearns to change, leaving most IPV and its consequences undetected. As a result, IPV treatment programs tend to serve primarily those who have been adjudicated and mandated to treatment. In turn, much IPV research and evaluation has focused on interventions serving court-mandated abusers. This has significantly skewed the research focus toward after-the-fact analysis rather than early intervention or prevention. Feder and et al (2011) concur that the lack of rigorous evaluations of domestic violence programs has severely limited our knowledge about what works, and prevented the development and testing of randomized controlled trials to prevent IPV from occurring or becoming worse. Not surprisingly, the need for improved treatments for partner violence (particularly early interventions), has been voiced by several scholars and clinicians (Butters et al., 2021; Stephens-Lewis et al., 2019).
Further, while the IPV field has excelled in raising awareness about IPV consequences to victims and families, we know far less about how abusers may perceive their violent behaviors to have negative consequences for themselves and how clinically targeting those perceptions may affect motivation for change. In the addiction field, motivational enhancement therapy (MET) has long-focused on eliciting participants’ greater awareness of the unwanted personal consequences of their substance use, which has been shown to strengthen motivation for change (Vader et al., 2010; Walker et al., 2007). Given that the majority of abusers do not voluntarily enter treatment, better understanding of what will motivate them to change and seek treatment is crucial.
Motivational Enhancement Therapy for The Untreated Abuser
MET, generally one to three sessions, involves an assessment, personal feedback of assessment results, and an exploration of problems the client has experienced as a result of the targeted behavior. The counselor uses motivational interviewing skills to develop a trusting and empathic relationship with the client (Miller & Rollnick, 2013). In an earlier trial (Mbilinyi et al., 2011), the authors preliminarily evaluated (in a Stage 1b developmental study) a telephone-delivered MET intervention designed to reach non-adjudicated and non-treatment-seeking abusers who also use alcohol or other drugs. Advertised as the “Men’s Domestic Abuse Check-Up,” the initial goal was to elicit the untreated abusive man’s voluntary participation in a brief conversation described in project publicity as intended to help the individual take stock of his behaviors and think through his options. Subsequent goals were to motivate the participant to seek treatment and to reduce or cease his IPV and substance use.
One hundred twenty-four men were recruited via a multimedia marketing campaign and following a baseline assessment, were randomly assigned to a one-session MET intervention or a comparison group (mailed educational information about IPV and substance use). Participants in the MET condition received a counseling session that reviewed a personalized feedback report on their IPV, substance use behaviors and consequences, and social norms beliefs. The findings, measured at one-month post-treatment, supported the likely effectiveness of MET in facilitating a short-term reduction of IPV behavior, increasing motivation for taking initial steps toward treatment, and correcting inaccurate beliefs concerning the prevalence of IPV and substance use (normative misperceptions). Reaching and enrolling this population in the trial was an important finding in itself, given that a very small percentage of abusers self-refer to treatment (Gondolf, 2002). Additionally, although the trial’s marketing did not include mention of alcohol or drug use (see, Mbilinyi et al., 2008) a substantial percentage (43%) of men enrolled in the trial met criteria for a SUD.
Current Study
In this second trial of the Men's Domestic Abuse Check-Up, another Stage 1b study, we sought to further the preliminary testing of the MET intervention and other methodological elements before conducting a full efficacy trial. Modifications included expanding the MET intervention from one to two sessions, requiring participants to meet DSM IV diagnostic criteria for a SUD rather than simply report prior use of alcohol or other drugs, and extending the terminal follow-up from one to four months. Finally, participating in a conversation with a counselor at an IPV agency that also focuses on SUDs was used to measure the primary outcome of treatment-seeking behavior in this trial.
Method
Procedure
Eligibility criteria were: male in a heterosexual relationship, fluent in English, 18 years or older, recent IPV behavior, evidence of SUD, no recent treatment attendance for IPV or SUD, no recent involvement in criminal or civil proceedings related to IPV or SUD (e.g., arrest, pending charges, probation, active restraining order, etc.), and no reported imminent danger to a partner. Recent was defined as the past 90 days. Assessors, all of whom held a Master’s degree or higher in social work or psychology, were trained to conduct a follow-up risk/lethality assessment if a caller endorsed any recent CTS2 behaviors categorized as “severe.” Similar in content to a brief suicide risk assessment, assessors probed whether the caller had a plan and intention for violent perpetration, access to the means of perpetration and to the partner, as well as ability to control impulse and other important contextual factors. Imminent danger to the partner was based on the totality of this assessment and the assessor’s clinical judgement. No callers were excluded due to disclosure of imminent danger to their partner.
Participants were recruited through a variety of marketing materials (print ads, flyers, radio ads) adapted from protocols successful in the first trial. Potential participants were encouraged to call the project’s toll-free number and were assured that the call would be completely private and anonymous. The marketing images and messages were relevant to adult men of diverse backgrounds engaging in IPV who are in the early stages of change. Upon enrollment, participants were offered up to $150 in incentive payments according to the following schedule: $30 (one-week), $40 (one-month), $50 (four-month), and a bonus payment of $30 if the individual completed all assessments. All procedures were approved by the University of Washington Institutional Review Board.
The screening process was split into two brief phone calls. During the first, the caller was introduced to the project, asked some basic demographic questions, and given an opportunity to talk about concerns that led him to call. Men who met demographic and adjudication eligibility criteria were scheduled to complete a second screening call. The second screening call assessed the man’s substance use and IPV behaviors, and further informed him about the study. Men who met eligibility criteria at the end of this call were asked whether they wished to enroll in the project and were then verbally consented.
Following the screening phone calls, participants were sent a link to complete the baseline assessment online within ten days. At the completion of the baseline assessment, they were randomized to either the experimental condition (MET) or comparison condition (Mail). A computerized Urn randomization procedure was utilized (Stout et al., 1994). Four variables were used for blocking: severity of violence, severity of substance use (abuse vs. dependence), treatment-seeking status, and race (white vs. non-white).
Men who were randomized to MET were scheduled immediately for the first of two phone feedback sessions with a project counselor. Participants who were randomized to the Mail condition received educational materials via mail. Participants in both conditions received a written invitation to have a conversation with a counselor employed by a certified domestic violence program in Washington State. This optional session was described as a private, in-person meeting with a counselor to learn about IPV and SUD treatment resources available in the community. Having this conversation served as an outcome measure indicating motivation for treatment seeking/entry. Three follow-up assessments were completed by phone or online, at one week, one month, and four months post-intervention.
Participants
Participant flow through the study is presented in Fig. 1. Over 69 weeks from June 2010 to October 2011, 615 calls were received from men responding to various forms of marketing including radio, print, and multimedia advertisement (see Mbilinyi et al., 2008 for details on the development of marketing products for the first trial). Of the 615 calls, 156 men met eligibility criteria, and 141 completed the baseline assessment to be enrolled and randomized.
Enrolled participants (N = 141) were primarily white (63%) and non-Hispanic (91%) with an average age of (37.7). Additional demographics and relevant characteristics are reported in Table 1. Notably, while growing up, a majority of participants were exposed to substance use (59%) and abusive behavior (74%) in their homes, and fewer than half had ever received services for SUD (42%) or IPV (26%).
Measures
The referent period for baseline measures was set at the prior 90 days, while referent periods for follow-up measures were based on time since last assessment (e.g., past 30 days at one-month and past 90 days at four-month assessments.
IPV Behaviors
The revised Conflict Tactics Scale (CTS2; Straus et al., 1996) is a widely used measure in IPV research. Results using various forms of the CTS have been reported in studies involving over 70,000 participants. Administered at screening to assess recent IPV behavior for eligibility, the measure was also administered at one- and four-month assessment points. Its use in two national surveys (Straus et al., 1990; Tjaden & Thoennes, 2000) provided comparison data against which to assess participants in the current study. The instrument, which includes five subscales (negotiation, psychological aggression, physical assault, sexual coercion, and injury) asks the respondent to state the number of times he has engaged in each of 39 behaviors over the given referent period. Frequency counts were capped at each assessment point equal to the number of days in the referent period.
Scores for each subscale represent the sum of frequency counts for all included behaviors. As such, range of subscale scores vary according to the number of behaviors included in each, with psychological aggression including eight (e.g., insulted or swore at partner; destroyed something that belonged to partner), physical assault including twelve (e.g., slapped my partner; kicked my partner), injurious behavior including six (e.g., [partner had] a sprain, bruise or cut because of a fight [with me]), and sexual coercion including seven (e.g., insisted on sex when my partner did not want to). The negotiation subscale was not a focus of the present study. Due to the relatively low frequency of their constituent behaviors, we combined the physical assault and injurious behavior subscales into a single indicator, scored as a sum of dichotomously coded items indicating whether or not they had engaged in each of the 18 behaviors. We also created a CTS summary score representing the mean of all items.
Perceived Consequences of IPV Behaviors
Our initial trial of this MET intervention (Walker et al., 2010) developed and reported on the Perceived Consequences of Domestic Violence Questionnaire (PCDVQ), a 27-item self-report instrument designed to assess problems and consequences the abuser experiences due to his IPV behaviors. The PCDVQ asks “How many times did the following things happen because of your abuse to your partner in the past [referent period]?” Examples of items include “you were distracted at work or school”, “your behavior scared you,” “your behavior frightened your partner.” The development, psychometrics, frequency and types of consequences reported by the participants are included in a previously published manuscript (see Walker et al., 2010).
Substance Use Disorder
The Psychoactive substance use disorder section of the Structured Clinical Interview for DSM-IV was developed to improve inter-rater diagnostic reliability and kappas for SUD diagnoses, which have typically ranged from 0.75 to 0.84 (First et al., 2002). It was used in this research for eligibility criteria and to characterize the sample in terms of current SUD diagnoses for alcohol and various classes of drugs.
Alcohol Use
The daily drinking questionnaire (DDQ; Collins et al., 1985; Kivlahan et al., 1990) asks the average number of standard drinks consumed and the time period of consumption for each day of the week over the previous month. Scores represent the sum for each of the seven days. It also assesses peak alcohol consumption by asking the most drinks consumed and time period of consumption. Participants completed the DDQ at baseline, one- and four-month follow-ups.
Drug Use
The customary drinking and drug use record (CDDR; Brown et al., 1998) was used to ask participants about their drug use during the referent period. Scores represent the number of days on which participants reported using any drug other than alcohol.
Treatment Seeking
The treatment seeking and preparation questionnaire was created to assess participants’ steps toward seeking IPV or SUD treatment. Items included contacting an agency, requesting information, and attending an intake or treatment session. Participants were also asked whether they had discontinued any treatment during the specified time frame. Behaviors were assessed separately for IPV and SUD treatment seeking. Treatment seeking was scored dichotomously as the presence or absence of any treatment-seeking behaviors during the referent period.
Interventions
Experimental – MET
The MET intervention consisted of two 45- to 60-min. telephone conversations within one to three weeks of the baseline assessment. Counselors created a Personal Feedback Report (PFR) immediately following the baseline assessment and sent it by mail to MET participants. The participant was asked not to open the PFR prior to the phone session. Each PFR was personally tailored to describe the participant’s assessment responses, and was color printed in booklet format with graphics and images. Included in the PFR were: the participant’s IPV, summary of substance use, and their consequences; IPV and substance use normative perceptions; family history of IPV; children’s exposure to IPV; and current alcohol use patterns and blood alcohol concentrations. The second session was a continuation of the first with more emphasis on the participant’s thoughts and ambivalence around treatment seeking.
Comparison – Mail
The printed educational materials received by participants in this condition highlighted health, psychological, legal, and social consequences of substance use and IPV. No personalized feedback was included.
Conversation With an IPV Agency Counselor
The conversation with an IPV agency counselor was delivered in a case management and didactic style. Counselors did not use motivational interviewing techniques in this session to avoid exposing the Mail participants to components of the MET intervention. The 30- to 45-min conversation was focused on providing detailed information about treatment programs such as length, format, fees/cost, and location.
Counselor Training and Supervision
Three master’s-level counselors conducted the MET interventions. Training and supervision were conducted by the clinical co-directors. This process included a two-day training on MET, which included didactic presentation of motivational interviewing principles and techniques as well as experiential exercises. Additionally, counselors completed a one-day training on IPV, two pilot cases with individualized supervision, and reading the treatment manual, Miller and Rollnick’s Motivational Interviewing (2013) book, and readings on IPV.
The counselors attended individual supervision with both supervisors weekly to discuss and plan for pilot cases. All sessions (both pilot and trial) were digitally recorded. Session recordings were listened to by both supervisors. Using an adapted version of the Motivational Interviewing Treatment Integrity coding system (MITI; Moyers et al., 2003), audio files were specifically coded for behavior counts of reflections (parsed by repeat, rephrase, paraphrase, and summary), open- and closed-ended questions, and affirmations. Counselors were provided general and individualized feedback based on the coding results of the sessions. When the counselors demonstrated acceptable behavior counts in the sessions and a mastery of implementing the sessions in accordance with the manual, they were approved to work with enrolled study participants. Each counselor’s first two to three sessions were supervised carefully by both supervisors. Counselors attended group supervision sessions weekly for 90 min. One or two recorded sessions (per counselor) were chosen at random and listened to by supervisors each week. Sessions were discussed and feedback was given to maintain treatment adherence, high level of competence, and to avoid therapist drift. Of the 58 MET1 and 54 MET2 sessions completed by MET participants, recordings of 92 percent of the sessions were listened to by at least one supervisor.
Results
Eighty-one percent of the participants completed their one-week follow-up, 84% completed their one-month follow-up, and 84% completed their four-month follow-up. At baseline there were no significant differences in severity of IPV or desire to change their behavior towards their partner between participants who completed the intervention and the four-month follow-up, and those who did not complete the intervention and follow-up. Across outcomes over the course of the trial, 54.6% of the study participants showed some success in reducing their IPV behaviors at terminal follow-up, having a conversation with an IPV agency counselor (in-person or by phone), or having one or more contacts with any IPV or SUD agency outside the study. The proportion of participants experiencing one or more indicators of success did not differ between the MET and the Mail group, χ2 (1, N = 141) = 0.68, p = 0.79. Overall, 5.7% of our participants (8.6% MET and 2.8% Mail) reported no IPV behavior at either follow-up assessment and 16.30% (20.0% MET and 12.7% Mail) reported no IPV at the terminal follow-up assessment. Differences in proportion of participants engaging in any IPV at follow-up assessments were not statistically significant.
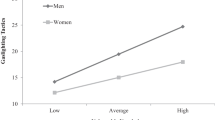
We were also interested in examining whether consequences of IPV might be a predictor of success. Table 2 shows prevalence and chronicity of consequences experienced in the 90 days prior to baseline assessment. Participants who reported more adverse consequences of IPV to themselves at baseline (as assessed by the PCDVQ) were more likely to have the conversation with an IPV agency counselor, χ2 (1, N = 139) = 4.78, p = 0.029, more likely to have one or more contacts with any domestic violence or SUD agency outside our study, χ2(1, N = 141) = 3.93, p = 0.047, but did not differ in absence of IPV behaviors at terminal follow-up. In contrast, participants who reported more adverse consequences of IPV to their partners at baseline (as assessed by the CTS summary scores) were no more likely to have the conversation with an IPV counselor, have one or more contacts with any agency outside our study, or absence of IPV behaviors at terminal follow-up (all p’s > 0.60). Neither adverse consequences to self nor partner at baseline interacted with condition in predicting any of the three overall success indicators.
IPV Behaviors
Specific IPV outcomes were analyzed with a series of generalized linear models, which allow models to predict outcomes with non-normal distributions (e.g., binary, Poisson, and negative binomial). Distributions were specified based on model fit where deviance χ2/df values close to 1 represent good fit (Hilbe, 2007). Models were run using the COUNTREG procedure in SAS 9.13 and evaluated outcomes, with appropriate distributional specifications, as a function of group assignment. Except for the evaluation of having the conversation with an IPV counselor, baseline assessment scores were entered as covariates in all analyses.
Table 3 shows means of CTS summary scores, psychological aggression, number of physical/injurious incidents, and proportion of participants engaging in sexual coercion at each time point by condition. CTS summary scores were best fit with a Poisson distribution (χ2/dfs were 1.13 and 0.90 for one- and four-month follow-up respectively). Results indicated no significant difference between MET and Mail participants at one-month follow-up, t (108) = 0.57, p = 0.57, but significantly lower CTS summary scores among the MET group at four-month follow-up, t (114) = -2.03, p = 0.04. Psychological aggression scores were best fit with a negative binomial distribution (χ2/dfs were 0.98 and 0.98 for one- and four-month follow-up respectively). Results again revealed no significant difference between MET and Mail participants at one-month follow-up, t (108) = 0.13, p = 0.89, but significantly lower psychological aggression scores among the MET group at four-month follow-up, t (116) = -2.00, p = 0.045. Physical/injurious behavior scores were best fit with a Poisson distribution (χ2/dfs were 1.55 and 1.57 for one- and four-month follow-up respectively). Following a similar pattern, results again revealed no significant difference between MET and Mail participants at one-month follow-up, t (118) = -1.06, p = 0.280, but significantly lower physical/injurious behaviors among the MET group at four-month follow-up, t (117) = -2.70, p = 0.007. Finally, with respect to sexual coercion, logistic regression analyses revealed no differences between groups at 1-month χ2(1, N = 112) = 0.32, p = 0.57, or 4-month follow-up, χ2 (1, N = 114) = 1.79, p = 0.18.
Conversation With an IPV Agency Counselor
Overall, 18.7% of our participants (14.7% intervention and 22.5% control) participated in a conversation with an IPV agency counselor (in-person or by phone) as part of the trial. This difference was not significant, χ2 (1, N = 139) = 1.38, p = 0.24. An additional 8% of participants (8.8% intervention and 7.0% control) scheduled the conversation with an IPV agency counselor but did not show up. This difference was also not significant.
Treatment Seeking
A minority of participants engaged in treatment-seeking behaviors during the follow-up period. The proportion of participants reporting any treatment seeking behavior for IPV was 28.3%, 29.4%, and 20.3% at one-week, one-month, and four-month follow-ups, respectively. Across all follow-up periods, 37.6% reported any treatment-seeking behavior for IPV and this did not differ by condition. Logistic regression analyses also revealed no difference in IPV treatment seeking between conditions at the one-week follow-up or at the one-month follow-up. However, more participants reported IPV treatment seeking at the four-month follow-up in the Mail condition than in the MET condition (28.3% vs 12.1%; χ2 (1, N = 118) = 4.58, p = 0.03.
Substance Use Outcomes
Substance use outcomes were analyzed using the same strategy as employed for examining IPV behaviors. Alcohol use, defined as number of drinks per week, was fit with a negative binomial distribution (χ2/dfs were 1.24 and 1.21 for one- and four-month follow-up respectively). Controlling for baseline drinks per week, results revealed no differences in MET versus Mail at one-month, t (114) = -0.99, p = 0.32, or four-month follow-up, t (114) = -0.72, p = 0.47. In examining substance use, we first considered marijuana. Most participants reported having ever used marijuana at baseline (91%) and just over half reported recent use at baseline. Controlling for past 90-day use at baseline, negative binomial regressions (χ2/dfs were 0.88 and 0.98 for one- and four-month follow-up respectively) revealed no group differences at one-month follow-up t (106) = -1.25, p = 0.21, but significantly less marijuana use at four-month follow-up in the MET group, t (101) = -2.06, p = 0.04. The prevalence of past 90-day use at baseline for substances other than alcohol and marijuana was relatively low: 6.4% methamphetamines, 7.8% barbiturates, 6.4% hallucinogens, 14.9% cocaine, 0.7% inhalants, and 18.4% opiates. The prevalence of use of substances other than alcohol and marijuana was combined at follow-up to reflect any use of these substances. Overall, 23% and 19% of participants reported using other substances during the one- and four-month follow-up periods respectively. These did not differ by group.
Discussion
Reaching male abusers with a diagnosable SUD and motivating them to call a study to talk about hurting their loved ones is no simple task. To avoid potential substance-using participants screening themselves out (as was the case in our previous trial), we did not mention alcohol or drug use in our marketing (see Mbilinyi et al., 2008). It was therefore necessary to screen more than twice as many callers than the first trial to reach IPV perpetrators who also met SUD criteria, without mentioning alcohol or drug use in marketing products. Still, we received calls from 615 individuals interested in the study in just 16 months. Among them were a higher proportion of Black men (almost three times more) compared to their population in the geographic area from which we were recruiting.
The fact that 615 men from diverse backgrounds were willing to talk with us about their IPV behaviors confirms that there are many individuals deeply concerned about their behaviors toward loved ones, and when given a venue that assures judgment-free confidentiality, they would be willing to reach out for help. The high interest also speaks to our marketing, our ads being the first point of entry for the non-adjudicated person in the general public. The ads intentionally focused on appealing to perpetrators’ latent, or perhaps nascent, desire to be a “good guy” – one who loves his family, is otherwise a good person, but who also has behaviors that could be damaging to himself and his loved ones. This language and strategy was developed through focus groups with IPV treatment providers and with perpetrators who had completed treatment (see Mbilinyi et al., 2008). The ads were intentionally developed and placed to reach a culturally diverse population. Furthermore, men who called our project were greeted with nonjudgmental and empathic interactions that persisted throughout their contacts with the project, and the message was consistent that help is available through our project and beyond.
This second trial attracted a more racially and socioeconomically diverse participant pool with greater barriers to treatment seeking. Still, of those eligible, 90% chose to enroll in a study that had several steps to complete, taking up to six hours over 21 weeks. Moreover, 84% stayed through the follow-up period. This retention rate was impressive considering the participants were struggling with more than IPV. The majority (74%) of the participants had been exposed to IPV in their families of origin. Although all participants met SUD criteria and 36.2 percent had engaged in severe violence such as hitting, choking, or slamming their partner against a wall, 74% had never reached out for help for their IPV and 58% had never sought help for their SUD. More than half of the participants were successful in at least one category (having the conversation with an IPV agency counselor, ceasing IPV behaviors, or initiating contact with a IPV or SUD agency in the community). This is impressive considering the population, targeted behaviors, and brevity of the intervention. Considering the unrest following George Floyd’s murder in 2020 and due to the historical disproportionate law enforcement contact and adjudication among people of color (Hinton & Cook, 2021; Jeffers, 2019; Turney & Wakefield, 2019), communities across the country are looking for alternative early interventions to specifically reach men of color early before encountering the criminal justice system. Findings from the present study give hope that alternative and/or enhanced criminal justice interventions are feasible and attractive for many men struggling with their IPV behaviors.
The proportion of participants did not differ by condition for all outcome indicators. The experimental condition participants had significantly lower IPV summary scores at the terminal follow-up compared to those in the comparison condition. Group differences were not evident at one-month follow-up but were evident at four-month follow-up. A possible explanation, consistent with the pattern of results, is that involvement in the study and continuously having empathic conversations about one’s behaviors may have had an immediate impact regardless of which group participants were in. Group differences then emerged over time where reductions may have been more maintained or augmented among experimental intervention participants compared to the control participants.
While encouraged by the study’s high interest and high retention among participants, the rates of treatment seeking and having a conversation with an IPV agency counselor were initially disappointing. The burden of engaging in IPV treatment may have been too big a leap for our participants. At the time, the state where the study was conducted had state-certified domestic violence treatment that required a minimum of 12 months of in-person treatment, with initial six months consisting of weekly in-person groups. The IPV agencies’ locations for the conversations with an IPV counselor may have also been an obstacle in thinking of potential future treatment, with the average distance from participants’ home being 15.3 miles in a heavy traffic region.
With IRB approval, we called participants after the trial to learn about their barriers to having the conversation. Of the 54 who responded, most said they would have met with the counselor over the phone if that option had been offered (61.1%) or if they could have chosen the meeting location (53.7%). Nearly half (49.1%) did not consider their problems to be severe enough to need counseling. The majority cited the cost of counseling (58.2%) as a reason they did not have the conversation with a counselor. Although that conversation was free and just to learn about options, considering the cost should they enroll in treatment may have been a barrier. At the same time, Gondolf and Wernik’s (2009) study with abusers mandated to paid treatment, the majority still did not seek the treatment due to transportation and other logistic barriers. Had there been more accessible treatment options such as virtual groups, which would have better reflected our study (telephone) participation, perhaps there would have been more of an uptake.
We expected differential impact on treatment seeking. To our initial surprise, more Mail condition than MET condition participants reported IPV treatment seeking at the four-month follow-up. Furthermore, while overall only 19 percent of the clients had the conversation with an IPV agency counselor (our primary outcome), more Mail participants (23%) held that conversation compared to MET participants (15%), although this difference was not statistically significant. It is possible that Mail participants, whose intervention was receiving a mere brochure in the mail, were hungry for any type of professional interaction and subsequently followed up more with agencies, including having the conversation with an IPV counselor. Similarly, participants who received two MET sessions may have felt they got what they needed and did not pursue other options.
Finally, data from the PCDVQ permitted an exploration of factors that mediate the intervention-outcome relationship. Those who reported higher levels of adverse personal consequences were more likely to have the conversation with an IPV agency counselor compared to those with fewer unfavorable personal consequences (see Table 2 for prevalence of consequences reported at baseline). This is an important finding as the abuser’s perceived personal consequences of his own behavior had not been evaluated prior to our first trial (see Walker et al., 2010), and, prior to the present study, had not been evaluated in relation to targeted IPV outcomes or behavior change. Discussing the pros and cons of continuing a behavior has been an important element in MET sessions in fields such as substance abuse because it gives the individual the opportunity to focus on how his/her behavior results in consequences to self and others (Amrhein et al., 2003; Swan et al., 2008; Walker et al., 2007). During the PCDVQ’s assessment, participants frequently became emotional and there was often a dramatic change in participants’ tone, with comments such as “Wow, I never thought about that before.”
Limitations
The study had several limitations. Although over 600 men called with interest in study participation, a sample of 141 was enrolled due to strict eligibility criteria, a fairly small sample size limiting statistical power for some results (i.e., analysis by condition) as well as generalizability. The goal of this second trial, however, was further preliminary testing of the MET intervention and other methodological elements with abusers who also met SUD criteria before conducting a full efficacy trial.
Similar to the first and other similar trials, abusers’ self-report data continues to be a limitation. While we have continued to guarantee confidentiality and utilized validated measures to reduce risk of biased self-report data (Babor et al., 2000), the validity of abusers’ data may not be as accurate as their partners’ (Easton et al., 2007; Gondolf, 2004). Although we grappled with this issue, we decided to continue relying on self-report data to encourage self-referral from the community. We did also ask the participants for permission to send their partners a brochure consisting of local, state, and national victim resources that we thought their partners may find helpful, as well as our telephone number to use at their discretion for support in locating resources, while maintaining participant confidentiality. Among the 141 enrolled participants, half (51%) gave permission and provided their partner’s mailing address, also equipping us with pilot data for future trials to contact partners directly for data corroboration.
Finally, we recognize that many criticisms of the CTS2 are valid. For example, we agree with Malbon et al (2018) that it fails to assess the contextual factors of IPV, which “are crucial for establishing patterns of coercive control” (p. 4), and we regret that it has been used to draw a false equivalence between male- and female-initiated aggression (e.g., Dutton & Nicholls, 2005; see, Johnson, 2006). Some scholars have also noted specific concerns about reliability (e.g., McCarroll et al., 2000; Vega & O’Leary, 2007), while others have called attention to abusive behaviors not included in the measure (e.g., DeKeseredy & Schwartz, 1998; Hamby, 2017). Despite these valid critiques, the CTS2 was chosen for the present study to measure violence in an all-male sample, because it has routinely shown the high psychometric validity required for a randomized clinical trial (Jones et al., 2017; Newton et al., 2001; Reichenheim et al., 2007; Straus, 2004; Straus et al., 1996; Vega & O’Leary, 2007), and it’s widespread use allows for comparison across studies.
Practice and Research Implications
Despite the limitations, this study has several promising results and contributes significantly to the IPV and SUD literature, particularly the implications for reaching and motivating the understudied target population, the men who make up the majority of abusers who never get “caught in the system.” The men who do not think of themselves as abusers; have managed not to get caught; can begin to entertain multiple truths targeted by the study’s marketing, that “I’m a good guy, with bad behavioral choices”; and can get help without detrimental consequences.
Social marketing in general and the products developed through the two trials are applicable across fields engaged in prevention and early intervention of problem behaviors, including reaching culturally diverse communities. The check-up concept warrants continued development and evaluation. The intention is to reach and intervene with more individuals before arrest. There are, in fact, recent efforts to get mandated clients to encourage other unadjudicated men to self-refer to treatment (E. Gondolf, personal communication, 2013). Direct recruitment through advertising, similar to the check-up model, can be another complementary channel. The study’s successful outreach to men of color, particularly Black men, gives promise and contributes to national discussions on transformative justice and community interventions that promote relational accountability. This article gives researchers, practitioners and policymakers across the country and globally a timely and innovative approach to reaching men engaging in abusive behaviors before arrest and further harm.
Motivational interviewing used in the MET sessions has practical implications for practitioners working with men who abuse their partners. Considering that most abusers who drop out of treatment do so within the first six sessions, and those who make it to six sessions often complete and have successful outcomes, employing motivational interviewing in treatment can potentially make a direct impact on the reduction of recidivism. Crane and Eckhardt’s (2013) study with 82 IPV abusers found that those who were lower in readiness to change and received a brief motivational enhancement session had better treatment attendance and compliance compared to those who did not receive the session. Participants higher in readiness to change had similar attendance rates regardless of condition. However, brief MET in their study was not associated with reduced recidivism regardless of level of readiness to change.
Importantly, two main principles of MET are that the client has the capacity to change and that taking stock of options to address problematic behavior can facilitate that change. The weighing of options in a check-up model for IPV is necessarily constrained by the ethics of talking about "safer" or "reduced" violence. Thus, MET with abusers of IPV may need to encourage treatment engagement more proactively than MET might with other problem behaviors. More research is needed on the use of MET with IPV perpetrators.
The PCDVQ provides practitioners with a tool to better understand the abuser’s views about his personal costs. In this population, the best predictor of treatment seeking was the impact of their IPV on themselves. Those negative consequences should be an early and important counseling focus to help motivate treatment engagement, helping the client answer: “What’s in it for me?”.
Targeting both IPV and SUD in the MET intervention has direct implications for practitioners who are continuously faced with clients with both problems. If not addressed simultaneously, their co-occurrence may jeopardize retention and successful outcomes. Furthermore, as Oberleitner and colleagues (Oberleitner et al., 2013) point out, participants with more severe IPV may need longer and more intense treatment to maintain outcomes beyond the treatment course due to their increased risk of IPV recidivism and SUD relapse.
Finally, a key question for future research is how to maintain the momentum of motivation in IPV abusers who voluntarily enroll in a check-up and comply with its numerous demands. What “next steps” might be offered to him following a check-up that would overcome the psychological and logistical barriers he faces and would keep him engaged in change? One area to explore in future research is more convenient and affordable treatment, including virtual (phone- or web-based) IPV treatment.
References
Afifi, T. O., Henriksen, C. A., Asmundson, G. J. G., & Sareen, J. (2012). Victimization and Perpetration of Intimate Partner Violence and Substance Use Disorders in a Nationally Representative Sample. Journal of Nervous & Mental Disease, 200(8), 684–691. https://doi.org/10.1097/NMD.0b013e3182613f64
Amrhein, P. C., Miller, W. R., Yahne, C. E., Palmer, M., & Fulcher, L. (2003). Client commitment language during motivational interviewing predicts drug use outcomes. Journal of Consulting and Clinical Psychology, 71(5), 862–878. https://doi.org/10.1037/0022-006X.71.5.862
Babor, T. F., Steinberg, K., Anton, R., & Del Boca, F. (2000). Talk is cheap: Measuring drinking outcomes in clinical trials. Journal of Studies on Alcohol, 61(1), 55–63. https://doi.org/10.15288/jsa.2000.61.55
Bacchus, L. J., Ranganathan, M., Watts, C., & Devries, K. (2018). Recent intimate partner violence against women and health: A systematic review and meta-analysis of cohort studies. British Medical Journal Open, 8(7), e019995. https://doi.org/10.1136/bmjopen-2017-019995
Boeckel, M. G., Wagner, A., & Grassi-Oliveira, R. (2017). The Effects of Intimate Partner Violence Exposure on the Maternal Bond and PTSD Symptoms of Children. Journal of Interpersonal Violence, 32(7), 1127–1142. https://doi.org/10.1177/0886260515587667
Bourgault, S., Peterman, A., & O’Donnell, M. (2021). Violence Against Women and Children During COVID-19—One Year On and 100 Papers In (p. 10) [CGD Note]. Center for Global Development. https://prevention-collaborative.org/wp-content/uploads/2021/08/CGD_2021_VAWC-Covid-19-Fourth-Research-Round-Up.pdf
Brown, S. A., Myers, M. G., Lippke, L., Tapert, S. F., Stewart, D. G., & Vik, P. W. (1998). Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): A measure of adolescent alcohol and drug involvement. Journal of Studies on Alcohol, 59(4), 427–438. https://doi.org/10.15288/jsa.1998.59.427
Butters, R. P., Droubay, B. A., Seawright, J. L., Tollefson, D. R., Lundahl, B., & Whitaker, L. (2021). Intimate Partner Violence Perpetrator Treatment: Tailoring Interventions to Individual Needs. Clinical Social Work Journal, 49(3), 391–404. https://doi.org/10.1007/s10615-020-00763-y
Campbell, J. C., Anderson, J. C., McFadgion, A., Gill, J., Zink, E., Patch, M., Callwood, G., & Campbell, D. (2018). The Effects of Intimate Partner Violence and Probable Traumatic Brain Injury on Central Nervous System Symptoms. Journal of Women’s Health, 27(6), 761–767. https://doi.org/10.1089/jwh.2016.6311
Clark, J. C., & Messer, S. C. (2006). Intimate Partner Violence in the U.S. Military: Rates, Risks, and Responses. In T. W. Britt, A. B. Adler, & C. A. Castro (Eds.), Military life: The psychology of serving in peace and combat (pp. 193–219). Praeger Security International.
Collins, R. L., Parks, G. A., & Marlatt, G. A. (1985). Social Determinants of Alcohol Consumption: The Effects of Social Interaction and Model Status on the Self-Administration of Alcohol. Journal of Consulting and Clinical Psychology, 53(2), 189–200.
Crane, C. A., & Eckhardt, C. I. (2013). Evaluation of a single-session brief motivational enhancement intervention for partner abusive men. Journal of Counseling Psychology, 60(2), 180–187. https://doi.org/10.1037/a0032178
DeKeseredy, W. S., & Schwartz, M. D. (1998). Measuring the Extent of Woman Abuse in Intimate Heterosexual Relationships: A Critique of the Conflict Tactics Scales (p. 7) [Applied Research Forum]. VAWNet: The National Online Resource Center on Violence Against Women. https://vawnet.org/material/measuring-extent-woman-abuse-intimate-heterosexual-relationships-critique-conflict-tactics
Dutton, D. G., & Nicholls, T. L. (2005). The gender paradigm in domestic violence research and theory: Part 1—The conflict of theory and data. Aggression and Violent Behavior, 10(6), 680–714. https://doi.org/10.1016/j.avb.2005.02.001
Easton, C. J., Crane, C. A., & Mandel, D. (2018). A Randomized Controlled Trial Assessing the Efficacy of Cognitive Behavioral Therapy for Substance-Dependent Domestic Violence Offenders: An Integrated Substance Abuse-Domestic Violence Treatment Approach (SADV). Journal of Marital and Family Therapy, 44(3), 483–498. https://doi.org/10.1111/jmft.12260
Easton, C. J., Mandel, D., Babuscio, T., Rounsaville, B. J., & Carroll, K. M. (2007). Differences in treatment outcome between male alcohol dependent offenders of domestic violence with and without positive drug screens. Addictive Behaviors, 32(10), 2151–2163. https://doi.org/10.1016/j.addbeh.2007.01.031
Feder, L., Holditch Niolon, P., Campbell, J., Wallinder, J., Nelson, R., & Larrouy, H. (2011). The Need for Experimental Methodology in Intimate Partner Violence: Finding Programs That Effectively Prevent IPV. Violence against Women, 17(3), 340–358. https://doi.org/10.1177/1077801211398620
First, M. B., Spitzer, R. L., Gibbon, M., & William, J. B. W. (2002). Structured Clinical Interview for DSM–IV–TR Axis I Disorders, Patient Edition (SCID-I/P). Biometric Research Department, New York State Psychiatric Institute.
Gondolf, E. W. (2002). Batterer intervention systems: Issues, outcomes, and recommendations. Sage Publications.
Gondolf, E. W. (2004). Evaluating batterer counseling programs: A difficult task showing some effects and implications. Aggression and Violent Behavior, 9(6), 605–631. https://doi.org/10.1016/j.avb.2003.06.001
Gondolf, E. W., & Wernik, H. (2009). Clinician Ratings of Batterer Treatment Behaviors in Predicting Reassault. Journal of Interpersonal Violence, 24(11), 1792–1815. https://doi.org/10.1177/0886260508325493
Hamby, S. (2017). A Scientific Answer to a Scientific Question: The Gender Debate on Intimate Partner Violence. Trauma, Violence, & Abuse, 18(2), 145–154. https://doi.org/10.1177/1524838015596963
Hilbe, J. M. (2007). Negative Binomial Regression. Cambridge University Press. https://doi.org/10.1017/CBO9780511811852
Hinton, E., & Cook, D. (2021). The Mass Criminalization of Black Americans: A Historical Overview. Annual Review of Criminology, 4(1), 261–286. https://doi.org/10.1146/annurev-criminol-060520-033306
Holmes, M. R., Richter, F. G. C., Votruba, M. E., Berg, K. A., & Bender, A. E. (2018). Economic Burden of Child Exposure to Intimate Partner Violence in the United States. Journal of Family Violence, 33(4), 239–249. https://doi.org/10.1007/s10896-018-9954-7
Jeffers, J. L. (2019). Justice Is Not Blind: Disproportionate Incarceration Rate of People of Color. Social Work in Public Health, 34(1), 113–121. https://doi.org/10.1080/19371918.2018.1562404
Johnson, M. P. (2006). Conflict and Control: Gender Symmetry and Asymmetry in Domestic Violence. Violence against Women, 12(11), 1003–1018. https://doi.org/10.1177/1077801206293328
Jones, R. T., Browne, K., & Chou, S. (2017). A critique of the revised Conflict Tactics Scales-2 (CTS-2). Aggression and Violent Behavior, 37, 83–90. https://doi.org/10.1016/j.avb.2017.08.005
Kistenmacher, B. R., & Weiss, R. L. (2008). Motivational Interviewing as a Mechanism for Change in Men Who Batter: A Randomized Controlled Trial. Violence and Victims, 23(5), 558–570. https://doi.org/10.1891/0886-6708.23.5.558
Kivlahan, D. R., Marlatt, G. A., Fromme, K., Coppel, D. B., & Williams, E. (1990). Secondary prevention with college drinkers: Evaluation of an alcohol skills training program. Journal of Consulting and Clinical Psychology, 58(6), 805–810. https://doi.org/10.1037/0022-006X.58.6.805
Kofman, Y. B., & Garfin, D. R. (2020). Home is not always a haven: The domestic violence crisis amid the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S199–S201. https://doi.org/10.1037/tra0000866
Kourti, A., Stavridou, A., Panagouli, E., Psaltopoulou, T., Spiliopoulou, C., Tsolia, M., Sergentanis, T. N., & Tsitsika, A. (2021). Domestic Violence During the COVID-19 Pandemic: A Systematic Review. Trauma, Violence, & Abuse, 152483802110386,. https://doi.org/10.1177/15248380211038690
Kraanen, F., Vedel, E., Scholing, A., & Emmelkamp, P. (2013). The comparative effectiveness of Integrated treatment for Substance abuse and Partner violence (I-StoP) and substance abuse treatment alone: A randomized controlled trial. BMC Psychiatry, 13, 189. https://doi.org/10.1186/1471-244X-13-189
Laskey, P., Bates, E. A., & Taylor, J. C. (2019). A systematic literature review of intimate partner violence victimisation: An inclusive review across gender and sexuality. Aggression and Violent Behavior, 47, 1–11. https://doi.org/10.1016/j.avb.2019.02.014
Malbon, E., Carson, L., & Yates, S. (2018). What can policymakers learn from feminist strategies to combine contextualised evidence with advocacy? Palgrave Communications, 4(1), 104. https://doi.org/10.1057/s41599-018-0160-2
Martin, S. L., Gibbs, D. A., Johnson, R. E., Sullivan, K., Clinton-Sherrod, M., Walters, J. L. H., & Rentz, E. D. (2010). Substance Use by Soldiers Who Abuse Their Spouses. Violence against Women, 16(11), 1295–1310. https://doi.org/10.1177/1077801210387038
Mbilinyi, L. F., Neighbors, C., Walker, D. D., Roffman, R. A., Zegree, J., Edleson, J., & O’Rourke, A. (2011). A Telephone Intervention for Substance-Using Adult Male Perpetrators of Intimate Partner Violence. Research on Social Work Practice, 21(1), 43–56. https://doi.org/10.1177/1049731509359008
Mbilinyi, L. F., Zegree, J., Roffman, R. A., Walker, D., Neighbors C., Edleson, J. (2008) Development of a marketing campaign to recruit non-adjudicated and untreated abusive men for a brief telephone intervention. Journal of Family Violence, 23(5), 343–351. https://doi.org/10.1007/s10896-008-9157-8
McCarroll, J. E., Thayer, L. E., Ursano, R. J., Newby, J. H., Norwood, A. E., & Fullerton, C. S. (2000). Are Respondents Who Omit Conflict Tactics Scale Items More Violent Than Those Who Omit None?: A Methodological Note. Journal of Interpersonal Violence, 15(8), 872–881. https://doi.org/10.1177/088626000015008006
Miller, W. R., & Rollnick, S. (2013). Motivational interviewing: Helping people change (3rd ed.). Guilford Press.
Moyers, T., Martin, T., Catley, D., Harris, K. J., & Ahluwalia, J. S. (2003). Assessing the Integrity of Motivational Interviewing Interventions: Reliability of the Motivational Interviewing Skills Code. Behavioural and Cognitive Psychotherapy, 31(2), 177–184. https://doi.org/10.1017/S1352465803002054
Murphy, C. M., Ting, L. A., Jordan, L. C., Musser, P. H., Winters, J. J., Poole, G. M., & Pitts, S. C. (2018). A randomized clinical trial of motivational enhancement therapy for alcohol problems in partner violent men. Journal of Substance Abuse Treatment, 89, 11–19. https://doi.org/10.1016/j.jsat.2018.03.004
Newton, R. R., Connelly, C. D., & Landsverk, J. A. (2001). An Examination of Measurement Characteristics and Factorial Validity of the Revised Conflict Tactics Scale. Educational and Psychological Measurement, 61(2), 317–335. https://doi.org/10.1177/0013164401612011
Noonan, C. B., & Pilkington, P. D. (2020). Intimate partner violence and child attachment: A systematic review and meta-analysis. Child Abuse & Neglect, 109, 104765. https://doi.org/10.1016/j.chiabu.2020.104765
Oberleitner, L. M. S., Mandel, D. L., & Easton, C. J. (2013). Treatment of co-occurring alcohol dependence and perpetration of intimate partner violence: The role of anger expression. Journal of Substance Abuse Treatment, 45(3), 313–318. https://doi.org/10.1016/j.jsat.2013.03.001
Peterson, C., Kearns, M. C., McIntosh, W. L., Estefan, L. F., Nicolaidis, C., McCollister, K. E., Gordon, A., & Florence, C. (2018). Lifetime Economic Burden of Intimate Partner Violence Among U. S. Adults. American Journal of Preventive Medicine, 55(4), 433–444. https://doi.org/10.1016/j.amepre.2018.04.049
Peterson, C., Liu, Y., Kresnow, M., Florence, C., Merrick, M. T., DeGue, S., & Lokey, C. N. (2018b). Short-term Lost Productivity per Victim: Intimate Partner Violence, Sexual Violence, or Stalking. American Journal of Preventive Medicine, 55(1), 106–110. https://doi.org/10.1016/j.amepre.2018.03.007
Reichenheim, M. E., Klein, R., & Moraes, C. L. (2007). Assessing the physical violence component of the Revised Conflict Tactics Scales when used in heterosexual couples: An item response theory analysis. Cadernos De Saúde Pública, 23(1), 53–62. https://doi.org/10.1590/S0102-311X2007000100007
Roffman, R. A., Edleson, J. L., Neighbors, C., Mbilinyi, L., Walker, D. (2008) The Men's Domestic Abuse Check-Up. Violence Against Women, 14(5), 589–605. https://doi.org/10.1177/1077801208315526
Satyanarayana, V. A., Nattala, P., Selvam, S., Pradeep, J., Hebbani, S., Hegde, S., & Srinivasan, K. (2016). Integrated Cognitive Behavioral Intervention Reduces Intimate Partner Violence Among Alcohol Dependent Men, and Improves Mental Health Outcomes in their Spouses: A Clinic Based Randomized Controlled Trial from South India. Journal of Substance Abuse Treatment, 64, 29–34. https://doi.org/10.1016/j.jsat.2016.02.005
Smith, S. G., Zhang, X., Basile, K. C., Merrick, M. T., Wang, J., Kresnow, M., & Chen, J. (2018). The National Intimate Partner and Sexual Violence Survey: 2015 Data Brief—Updated Release (p. 32). National Center for Injury Prevention and Control, Centers for Disease Control and Prevention.
Spencer, C., Mallory, A. B., Cafferky, B. M., Kimmes, J. G., Beck, A. R., & Stith, S. M. (2019). Mental health factors and intimate partner violence perpetration and victimization: A meta-analysis. Psychology of Violence, 9(1), 1–17. https://doi.org/10.1037/vio0000156
Stephens-Lewis, D., Johnson, A., Huntley, A., Gilchrist, E., McMurran, M., Henderson, J., Feder, G., Howard, L. M., & Gilchrist, G. (2019). Interventions to Reduce Intimate Partner Violence Perpetration by Men Who Use Substances: A Systematic Review and Meta-Analysis of Efficacy. Trauma, Violence, & Abuse, 1524838019882357,. https://doi.org/10.1177/1524838019882357
Stout, R. L., Wirtz, P. W., Carbonari, J. P., & Del Boca, F. K. (1994). Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol, Supplement, s12, 70–75. https://doi.org/10.15288/jsas.1994.s12.70
Straus, M. A. (2004). Cross-Cultural Reliability and Validity of the Revised Conflict Tactics Scales: A Study of University Student Dating Couples in 17 Nations. Cross-Cultural Research, 38(4), 407–432. https://doi.org/10.1177/1069397104269543
Straus, M. A., Gelles, R. J., & Smith, C. (1990). Physical violence in American families: Risk factors and adaptations to violence in 8,145 families. Transaction Publishers.
Straus, M. A., Hamby, S. L., & BONEY-McCOY, S., & Sugarman, D. B. (1996). The Revised Conflict Tactics Scales (CTS2): Development and Preliminary Psychometric Data. Journal of Family Issues, 17(3), 283–316. https://doi.org/10.1177/019251396017003001
Stuart, G. L., Moore, T. M., Elkins, S. R., O’Farrell, T. J., Temple, J. R., Ramsey, S. E., & Shorey, R. C. (2013a). The temporal association between substance use and intimate partner violence among women arrested for domestic violence. Journal of Consulting and Clinical Psychology, 81(4), 681–690. https://doi.org/10.1037/a0032876
Stubbs, A., & Szoeke, C. (2021). The Effect of Intimate Partner Violence on the Physical Health and Health-Related Behaviors of Women: A Systematic Review of the Literature. Trauma, Violence, & Abuse, 1524838020985541,. https://doi.org/10.1177/1524838020985541
Swan, M., Schwartz, S., Berg, B., Walker, D., Stephens, R., & Roffman, R. (2008). The Teen Marijuana Check-Up: An In-School Protocol for Eliciting Voluntary Self-Assessment of Marijuana Use. Journal of Social Work Practice in the Addictions, 8(3), 284–302. https://doi.org/10.1080/15332560802223305
Taillieu, T. L., Brownridge, D. A., & Brownell, M. (2021). Screening for intimate partner violence in the early postpartum period: Maternal and child health and social outcomes from birth to 5-years post-delivery. Child Abuse & Neglect, 111, 104865. https://doi.org/10.1016/j.chiabu.2020.104865
Thompson, M. P., & Kingree, J. B. (2006). The Roles of Victim and Perpetrator Alcohol Use in Intimate Partner Violence Outcomes. Journal of Interpersonal Violence, 21(2), 163–177. https://doi.org/10.1177/0886260505282283
Tjaden, P., & Thoennes, N. (2000). Full Report of the Prevalence, Incidence, and Consequences of Violence Against Women. U.S. Department of Justice. https://doi.org/10.1037/e514172006-001
Turney & Wakefield. (2019). Criminal Justice Contact and Inequality. RSF: The Russell Sage Foundation Journal of the Social Sciences, 5(1), 1. https://doi.org/10.7758/rsf.2019.5.1.01
Vader, A. M., Walters, S. T., Prabhu, G. C., Houck, J. M., & Field, C. A. (2010). The language of motivational interviewing and feedback: Counselor language, client language, and client drinking outcomes. Psychology of Addictive Behaviors, 24(2), 190–197. https://doi.org/10.1037/a0018749
Vega, E. M., & O’Leary, K. D. (2007). Test-Retest Reliability of the Revised Conflict Tactics Scales (CTS2). Journal of Family Violence, 22(8), 703–708. https://doi.org/10.1007/s10896-007-9118-7
Walker, D. D., Neighbors, C., Mbilinyi, L. F., O’Rourke, A., Zegree, J., Roffman, R. A., & Edleson, J. L. (2010). Evaluating the Impact of Intimate Partner Violence on the Perpetrator: The Perceived Consequences of Domestic Violence Questionnaire. Journal of Interpersonal Violence, 25(9), 1684–1698. https://doi.org/10.1177/0886260509354592
Walker, D. D., Roffman, R. A., Picciano, J. F., & Stephens, R. S. (2007). The check-up: In-person, computerized, and telephone adaptations of motivational enhancement treatment to elicit voluntary participation by the contemplator. Substance Abuse Treatment, Prevention, and Policy, 2(1), 2. https://doi.org/10.1186/1747-597X-2-2
Acknowledgements
Eli Crawford, Devon Bushnell, Sara Dyson, Marti Hickey, Heather Spielvogle, and Sorina Zielinski.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Authors declare they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mbilinyi, L.F., Neighbors, C., Walker, D.D. et al. What’s In It for Me? Motivating the Untreated Abuser to Consider Treatment. J Fam Viol 38, 333–346 (2023). https://doi.org/10.1007/s10896-022-00375-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10896-022-00375-9