Maternal mental health history is strongly implicated in the developmental trajectory of child emotional development and psychopathology risk (Goodman & Gotlib, Reference Goodman and Gotlib1999; Bijl et al., Reference Bijl, Cuijpers and Smit2002; Swales et al., Reference Swales, Snyder, Hankin, Sandman, Glynn and Davis2020). This intergenerational link between maternal and child psychological wellbeing is especially evident among mothers who have experienced trauma and subsequent symptoms of posttraumatic stress (Lambert et al., Reference Lambert, Holzer and Hasbun2014). Almost 7 out of every 10 adult women will be exposed to a traumatic event in their lifetime (Resnick et al., Reference Resnick, Kilpatrick, Dansky, Saunders and Best1993) and approximately 4%–6% will go on to meet criteria for posttraumatic stress disorder (PTSD) (National Comorbidity Survey, 2017). Notably, PTSD rates are even higher among women living in poverty (Seng et al., Reference Seng, Low, Sperlich, Ronis and Liberzon2009). Maternal trauma and subsequent PTSD symptoms have been shown to have intergenerational consequences, including deleterious effects on child socioemotional development and mental health outcomes, such as elevated risk for anxiety, depression, and behavior problems (Lambert et al., Reference Lambert, Holzer and Hasbun2014).
Consistent with a Developmental Origins of Health and Disease (DOHaD) framework, maternal perinatal PTSD symptoms are associated with their children’s vulnerability to psychopathology via biological mechanisms of fetal programming as well as postnatal environmental cues (e.g., parenting behaviors, quality of parent-child attachments) (Doyle & Cicchetti, Reference Doyle and Cicchetti2018). However, a growing literature suggests that ontogenetic pathways of risk and resilience for the development of psychopathology do not begin at conception (Keenan et al., Reference Keenan, Hipwell, Class and Mbayiwa2018). Rather maternal mental health prior to conception, including PTSD symptoms, may also relate to developmental trajectories of mental health in the next generation via alterations in prenatal stress physiology, epigenetic pathways, and other peripartum mechanisms (Bale, Reference Bale2014; Bowers & Yehuda, Reference Bowers and Yehuda2016; Buss et al., Reference Buss, Entringer, Moog, Toepfer, Fair, Simhan and Wadhwa2017; Keenan et al., Reference Keenan, Hipwell, Class and Mbayiwa2018; Scorza et al., Reference Scorza, Duarte, Hipwell, Posner, Ortin and Canino2019; Swales et al., Reference Swales, Stout-Oswald, Glynn, Sandman, Wing and Davis2018). The current study expands the DOHaD framework to include preconception influences, utilizing a prospective, longitudinal design to examine how maternal PTSD symptoms prior to conception may relate to outcomes in the next generation, such as negative affectivity, which contribute to subsequent vulnerability to later psychopathology (e.g., Clark et al., Reference Clark, Watson and Mineka1994; Derryberry & Rothbart, Reference Derryberry and Rothbart1997; Lonigan et al., Reference Lonigan, Vasey, Phillips and Hazen2004; Muris & Ollendick, Reference Muris and Ollendick2005; Nigg, Reference Nigg2006).
Intergenerational consequences of preconception stress
Experimental research with animals provides compelling evidence that maternal stress exposure prior to conception exerts lasting intergenerational consequences (see Klengel et al., Reference Klengel, Dias and Ressler2016 for review). Maternal stress exposure (e.g., chronic and unpredictable stress, overcrowding, temperature) that is limited to the preconception period adversely impacts rat offspring brain development including anatomical changes in the medial prefrontal cortex (Bock et al., Reference Bock, Poeschel, Schindler, Börner, Shachar-Dadon, Ferdman and Poeggel2016; Harker et al., Reference Harker, Raza, Williamson, Kolb and Gibb2015; Huang et al., Reference Huang, Shi, Xu, Yang, Chen, Chen and Chen2010), altered stress physiology (Zaidan et al., Reference Zaidan, Leshem and Gaisler-Salomon2013), and increased anxious and anhedonic behavior (Bock et al., Reference Bock, Poeschel, Schindler, Börner, Shachar-Dadon, Ferdman and Poeggel2016; Li et al., Reference Li, Zhang, Fang, Lin, Wu and Huang2010; Zaidan et al., Reference Zaidan, Leshem and Gaisler-Salomon2013). These experimental studies provide important evidence that severe stress exposure limited to the preconception period has intergenerational consequences.
In humans, evidence for the intergenerational transmission of trauma has been supported by epidemiological research as well as studies of collective trauma (e.g., parental exposure to genocide prior to conception) (Class et al., Reference Class, Abel, Khashan, Rickert, Dalman, Larsson and D‘Onofrio2014, Reference Class, Mortensen, Henriksen, Dalman, D’Onofrio and Khashan2015; Flory et al., Reference Flory, Bierer and Yehuda2011; Gangi et al., Reference Gangi, Talamo and Ferracuti2009; Keenan et al., Reference Keenan, Hipwell, Class and Mbayiwa2018; Perroud et al., Reference Perroud, Rutembesa, Paoloni-Giacobino, Mutabaruka, Mutesa, Stenz and Karege2014; Power et al., Reference Power, Atherton, Strachan, Shepherd, Fuller, Davis and Macfarlane2007; Solomon et al., Reference Solomon, Kotler and Mikulincer1988; Yehuda et al., Reference Yehuda, Halligan and Grossman2001, Reference Yehuda, Bell, Bierer and Schmeidler2008). Additionally, maternal retrospective report of traumatic and stressful life experiences, such as history of childhood maltreatment (e.g., Adverse Childhood Events Scale, Felitti et al., Reference Felitti, Anda, Nordenberg, Williamson, Spitz, Edwards and Marks1998; and Childhood Trauma Questionnaires, Bernstein et al., Reference Bernstein, Fink, Handelsman, Foote, Lovejoy, Wenzel and Ruggiero1994), show that maternal trauma can have intergenerational effects. Children of women with trauma histories, assessed by maternal recall of trauma in her own childhood, are more likely to experience dysregulated temperament in infancy, including heightened negative affectivity (Bosquet Enlow et al., Reference Bosquet Enlow, Devick, Brunst, Lipton, Coull and Wright2017; Lang et al., Reference Lang, Gartstein, Rodgers and Lebeck2010) and poor emotional and behavioral outcomes in childhood (Bosquet et al., Reference Bosquet Enlow, Englund and Egeland2018; Khan & Renk, Reference Khan and Renk2019; Plant et al., Reference Plant, Jones, Pariante and Pawlby2017, Reference Plant, Pawlby, Pariante and Jones2018). These studies provide epidemiological and retrospective evidence that maternal history of traumatic and potentially traumatic experiences prior to conception predicts poor emotional outcomes for the next generation. However, additional prospective research is needed to address limitations inherent to such study designs. First, retrospective recall of adverse experiences is only moderately associated with prospectively collected measures (see Baldwin et al., Reference Baldwin, Reuben, Newbury and Danese2019 for meta-analysis and systematic review). Second, retrospective recall of PTSD symptoms is even more susceptible to recall biases than recall of past trauma exposure (Baldwin et al., Reference Baldwin, Reuben, Newbury and Danese2019; Hardt & Rutter, Reference Hardt and Rutter2004; Moffitt et al., Reference Moffitt, Caspi, Taylor, Kokaua, Milne, Polanczyk and Poulton2010; Newbury et al., Reference Newbury, Arseneault, Moffitt, Caspi, Danese, Baldwin and Fisher2018; Reuben et al., Reference Reuben, Moffitt, Caspi, Belsky, Harrington, Schroeder and Danese2016).
Prospective assessment of preconception trauma
Given the inherent limitations of retrospective studies, there has been increasing recognition of the need for prospective, longitudinal studies of preconception stress (Bowers & Yehuda, Reference Bowers and Yehuda2016; Keenan et al., Reference Keenan, Hipwell, Class and Mbayiwa2018). However, a dearth of prospective research has examined women’s mental health prior to pregnancy and child outcomes due to the logistical challenges of recruiting women before conception and following them through their pregnancies. A few published prospective studies show that elevated preconception stress and exposure to stressful life experiences relate to adverse birth outcomes (i.e., shorter gestation and lower birthweight) (Harville et al., Reference Harville, Boynton-Jarrett, Power and Hyppönen2010; Mahrer et al., Reference Mahrer, Guardino, Hobel and Dunkel Schetter2020) and poor sleep quality in infancy (Baird et al., Reference Baird, Hill, Kendrick and Inskip2009). A large prospective study of women in Australia (n = 756) reported that maternal preconception symptoms of depression and anxiety predicted heightened emotional reactivity in infancy (Spry et al., Reference Spry, Moreno-Betancur, Becker, Romaniuk, Carlin, Molyneaux and Macdonald2020). Another study conducted by Hipwell et al. (Reference Hipwell, Tung, Northrup and Keenan2019) prospectively assessed maternal childhood trauma exposure prior to conception via standardized interviews and items from the Parent-Child Conflict Tactics Scale and found that infants of mothers exposed to childhood emotional abuse were more likely to demonstrate low emotional reactivity to the still face procedure, whereas infants of mothers exposed to childhood emotional neglect demonstrated heightened emotional reactivity, even after controlling for postpartum depressive symptoms. Collectively, these few, prospective studies are important as they reduce the influence of recall bias and affirm the need to expand research on preconception maternal trauma and mental health and child emotion regulation outcomes.
A key gap in this literature is that additional studies are needed to prospectively assess whether preconception symptoms of posttraumatic stress predict outcomes for the next generation. It is important to distinguish maternal exposure to trauma or a potentially traumatic event from posttraumatic stress symptoms because not all women who are exposed to a potentially traumatic event will develop subsequent PTSD symptoms. Rather mediating pathways of risk and resilience have been shown to amplify or disrupt the emergence of subsequent psychopathology following trauma exposure (McLaughlin & Lambert, Reference McLaughlin and Lambert2017). Identifying whether preconception maternal PTSD symptoms relate to child outcomes is therefore important next step in exploring whether maternal mental health prior to conception confers vulnerability for subsequent psychopathology in the next generation.
Additional work is also needed to explore potential pathways that may underly this hypothesized link between preconception PTSD symptoms and child psychopathological risk. Perinatal mental health, especially maternal depression, is a plausible candidate pathway because prior work suggests that offspring may be more vulnerable to the biopsychosocial sequelae of maternal trauma during the fetal period of development (Bouvette-Turcot et al., Reference Bouvette-Turcot, Fleming, Unternaehrer, Gonzalez, Atkinson, Gaudreau and Meaney2020; Bowers & Yehuda, Reference Bowers and Yehuda2016; Buss et al., Reference Buss, Entringer, Moog, Toepfer, Fair, Simhan and Wadhwa2017; Davis & Narayan, Reference Davis and Narayan2020; Keenan et al., Reference Keenan, Hipwell, Class and Mbayiwa2018; Swales et al., Reference Swales, Stout-Oswald, Glynn, Sandman, Wing and Davis2018; Yehuda & Meaney, Reference Yehuda and Meaney2018). Past studies demonstrate that retrospective recall of trauma history is associated with elevated internalizing symptoms (e.g., depression, anxiety, and PTSD) during pregnancy (Alvarez-Segura et al., Reference Alvarez-Segura, Garcia-Esteve, Torres, Plaza, Imaz, Hermida-Barros and Burtchen2014; Atzl et al., Reference Atzl, Narayan, Rivera and Lieberman2019; River et al., Reference River, Narayan, Atzl, Rivera and Lieberman2019), and prenatal maternal mental health predicts heightened negative emotionality in offspring during childhood (Blair et al., Reference Blair, Glynn, Sandman and Davis2011; Davis et al., Reference Davis, Glynn, Schetter, Hobel, Chicz-Demet and Sandman2007; Erickson et al., Reference Erickson, Gartstein and Dotson2017; Glynn et al., Reference Glynn, Howland, Sandman, Davis, Phelan, Baram and Stern2018; Werner et al., Reference Werner, Myers, Fifer, Cheng, Fang, Allen and Monk2007). Prenatal depression is a potential pathway of particular interest because PTSD and depression diagnoses are highly comorbid (O’Donnell et al., Reference O’Donnell, Creamer and Pattison2004) and depressive symptoms are commonly screened for in clinical settings and thus offer implications for clinical practice. The current study provides a unique opportunity to investigate these exploratory pathways.
The current study
The current study prospectively evaluates the association between maternal preconception symptoms of posttraumatic stress and child negative affectivity. Mothers were from a socioeconomically, racially, and ethnically diverse larger cohort of women who were studied following a birth. This subset was then followed when mothers became pregnant again with the study child and until the study child was 3–5 years of age. Preconception is defined in the current study as prior to conception of the study child (which for all participants in the study sample is also an interconception period between consecutive births). As the primary aim of the current analyses, we evaluated whether preconception maternal PTSD symptoms predict child negative affectivity after accounting for sociodemographic covariates and concurrent maternal depressive symptoms (an indicator of concurrent maternal psychopathology and reporter bias). In exploratory post hoc analyses, we tested maternal prenatal and postpartum symptoms of depression as potential mediators in the relation between preconception symptoms of PTSD and child negative affectivity. Prenatal and postpartum levels of perceived stress were additionally considered as mediators in secondary, exploratory analyses.
Method
Participants
Participants were 118 mother-child dyads. Women were recruited from three study sites in the Community Child Health Network (CCHN) (i.e., North Carolina, Washington, DC, and Lake County, IL). CCHN is a multisite research network designed to investigate disparities in maternal and child mental health (see Dunkel Schetter et al., Reference Dunkel Schetter, Schafer, Lanzi, Clark-Kauffman, Raju and Hillemeier2013; O’Campo et al., Reference O’Campo, Schetter, Guardino, Vance, Hobel and Ramey2016; and Ramey et al., Reference Ramey, Schafer, DeClerque, Lanzi, Hobel, Shalowitz and Raju2015 for overview of CCHN recruitment procedures, study design, data collection methods, and cohort demographics). Two hundred and forty-five women from the three selected CCHN study sites who became pregnant again between 2009 and 2013 and were assessed prospectively from preconception (i.e., between births and prior to conception of the study child) through their pregnancy and into the postpartum period. One hundred and twenty-seven women then went on to participate in a follow-up assessment when the study child was 3–5 years of age.
Additional inclusion criteria for the current analyses were mothers who provided: (a) ratings of preconception PTSD or completed at least one prenatal study visit (i.e., provided at least one rating of mood or stress during pregnancy), and (b) ratings of child negative affectivity in early childhood. One hundred and nineteen women met these criteria. One dyad was excluded from analyses due to preterm birth less than 34 weeks’ gestation. See Figure 1 for overview of study design.
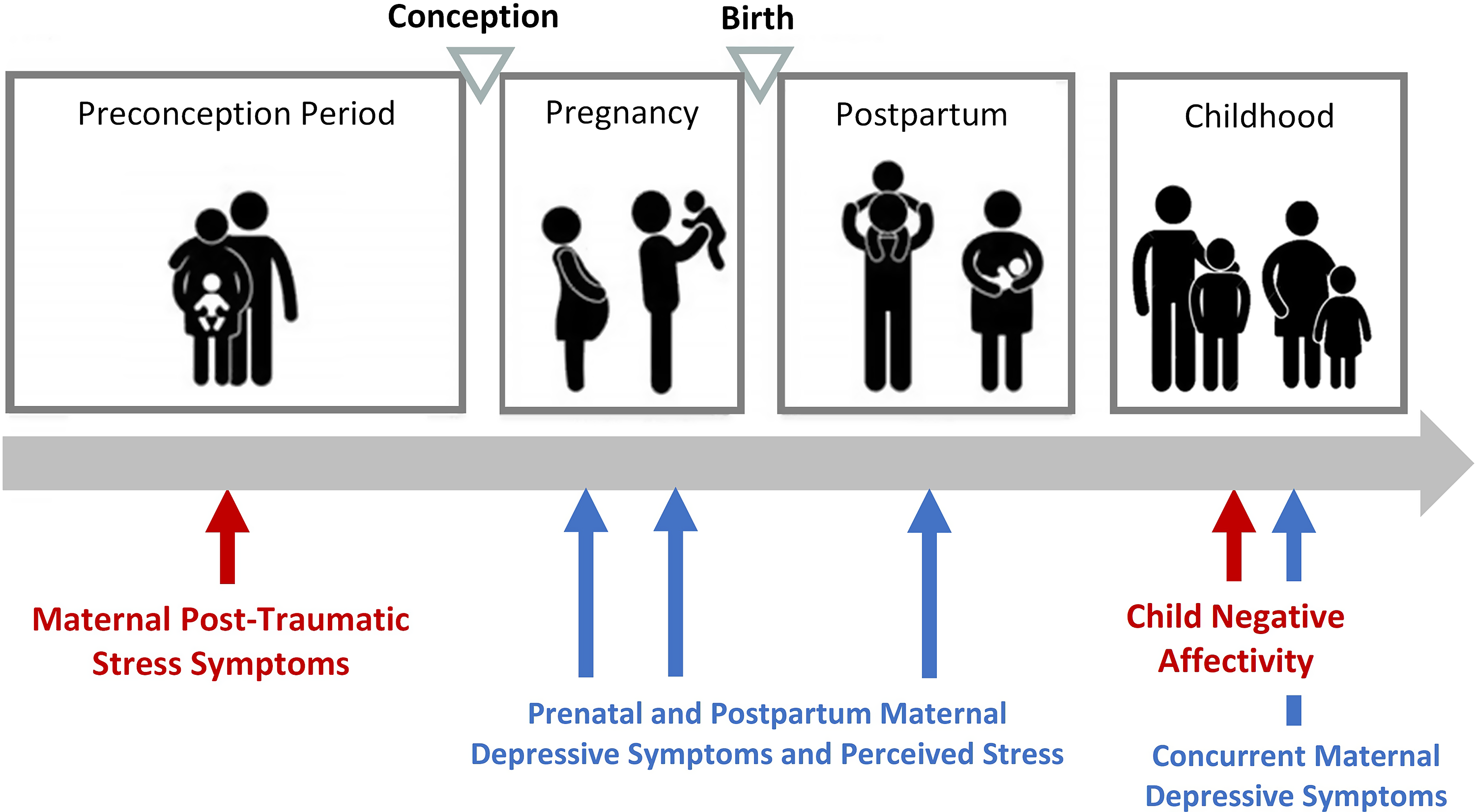
Figure 1. Overview of study measures from preconception to early childhood.
The 118 women in the current study analyses were more likely to be older in age (t = 4.1, p < .001), have a longer interpregnancy interval (t = 2.6, p = .002), have a lower adjusted household income (t = −2.0, p = .049), be Latina/Hispanic (X 2 = 8.6, p = .003), and be born outside of the United States (X 2 = 8.6, p = .003), in comparison to women who became pregnant during the eligibility window but were not included in the present analyses (either because they did not participate in the follow-up assessment in early childhood and/or were missing preconception or prenatal study measures). Sample attrition was not associated with maternal education (t = −1.1, p = .275), concurrent depressive symptoms (t = 0.7, p = .484), study site (X 2 = 0.8, p = .655), cohabitation status (X 2 = 2.4, p = .124), or PTSD symptoms (t = 1.0, p = .326).
Mothers included in the current study sample were an average of 33 years of age at the time of child assessment (SD = 5.5 years) and 39% identified as Latina/Hispanic, 32% non-Latina/Hispanic Black, and 29% non-Latina/Hispanic White (see Supplemental Table S1 for descriptive information on study measures stratified by maternal race/ethnicity). Additionally, 40% of women were born outside of the United States (46 out of the 47 of whom also identified as Latina or Hispanic). Further, 38% lived below the federal poverty line (FPL), and 21% lived near poverty at 100%–200% FPL. Children were on average 3.8 years of age at the time of assessment (SD = 0.4 years) and 58% were female (see Table 1). All study procedures were approved by the Institutional Review Board for the protection of human subjects at the relevant institutions, and each mother provided written and informed consent for herself and her child.
Table 1. Sample characteristics

Procedures
All self-report data were collected through semistructured interviews by trained interviewers in participants’ homes (see Dunkel Schetter et al., Reference Dunkel Schetter, Schafer, Lanzi, Clark-Kauffman, Raju and Hillemeier2013). Maternal ratings of posttraumatic stress symptoms and demographic data were collected before women became pregnant with the study child. For present purposes, the preconception assessment occurred an average of 52.9 weeks prior to conception of the study child, although time from assessment to conception varied (SD = 47.3, Range: 2.0–175.0 weeks). The beginning of the pregnancy was determined using the first day of the last menstrual period and/or ultrasound examinations, obtained via medical record abstraction. Standardized measures of maternal depression symptoms and perceived stress were administered twice during pregnancy in second and third trimesters, on average at 20.2 weeks gestation (SD = 5.0) and 32.7 weeks gestation (SD = 3.8). Maternal depression symptoms were assessed once during the postpartum period on average at 12.5 weeks after birth (SD = 4.7). Additional perinatal and birth outcomes data were extracted from neonatal records. Mother-child dyads participated in an early childhood study visit when the child was 3–5 years of age, at which time child’s negative affectivity was assessed. Early childhood visits were conducted in participants’ homes, in the mother’s preferred language (English or Spanish).
Measures
Maternal measures
Sociodemographic and pregnancy factors
Sociodemographic characteristics, including maternal age, years of education, per capita household income adjusted for cost of living, cohabitation status (i.e., living with partner), parity, foreign birth (i.e., whether mother was born in a country outside of the United States), and race/ethnicity, were assessed during interviews. An outlier for adjusted household income (i.e., >8 SD above the mean) was replaced with a value 3 SD above the mean, retaining its rank as the highest value. Maternal education and per capita household income adjusted for cost of living were standardized and averaged together to create a composite of socioeconomic status (SES; Cohen et al., Reference Cohen, Doyle and Baum2006). Maternal early life adversity was assessed by the 10-item Risky Families Questionnaire (Taylor et al., Reference Taylor, Lerner, Sage, Lehman and Seeman2004), a measure of family stressors during the mother’s childhood (e.g., childhood abuse, parental warmth). Mothers completed the measure during the early childhood visit, rating each item on a 5-point Likert scale, with a range of 1 (not at all) to 5 (very often). Final sum scores could range from 10 to 50, with higher scores indicating greater early life adversity. Gestational age at birth was determined from medical record abstraction.
Maternal posttraumatic stress symptoms
Maternal symptoms of posttraumatic stress were assessed prior to conception using the PTSD Checklist – Civilian Version (PCL-C; Blanchard et al., Reference Blanchard, Jones-Alexander, Buckley and Forneris1996). Participants provided ratings of how often they have been bothered by various symptoms of PTSD in the past month, on a 5-point Likert scale with a range of 1 (not at all) to 5 (extremely). Final sum scores could range from 17 to 85, with higher scores indicating more PTSD symptoms (see Table 2). A cut-off score of 30 was used to indicate clinically elevated symptoms and a probable diagnosis of PTSD. This threshold and scoring approach were selected because prior research demonstrates that utilizing a cut-off score of 30 maximizes the sensitivity and specificity of accurately detecting a PTSD diagnosis amongst civilian women (McDonald & Calhoun, Reference McDonald and Calhoun2010; Walker et al., Reference Walker, Newman, Dobie, Ciechanowski and Katon2002). The PCL-C is a reliable and well-validated measure of PTSD symptoms (Ruggiero et al., Reference Ruggiero, Del Ben, Scotti and Rabalais2003), and has been previously utilized in studies of women across pregnancy and the postpartum period (e.g., Huth-Bocks et al., Reference Huth-Bocks, Krause, Ahlfs-Dunn, Gallagher and Scott2013; Thomas, Carter, et al., Reference Thomas, Carter, Dunkel Schetter and Sumner2021; Thomas, Cleveland, et al., Reference Thomas, Cleveland, Pietrzak, Dunkel Schetter and Sumner2021). Within the current study sample, the PCL-C demonstrated excellent internal consistency (α = .92) and 18 participants (21%) reported scores above the clinical threshold. Notably, the rate of probable PTSD diagnosis was higher in this sample than in the general population (Breslau, Reference Breslau2009), likely reflecting the converging risk factors for trauma and PTSD symptoms experienced by many of the women in the study (e.g., poverty, low education, acculturative stress) (Breslau et al., Reference Breslau, Davis and Andreski1995; Pole et al., Reference Pole, Gone and Kulkarni2008; Trickey et al., Reference Trickey, Siddaway, Meiser-Stedman, Serpell and Field2012). Indeed, women who experienced elevated symptoms of PTSD in the study sample were more likely to be born outside of the United States (t = −2.62, p = .012), to have completed fewer years of education (r = −.367, p < .001), and to have a lower per capita income adjusted for cost of living (r = −.31, p = .004). PCL-C scores were not associated with race/ethnicity or cohabitation status.
Table 2. Descriptive statistics for maternal and child measures across all timepoints

Maternal depressive symptoms
Maternal depressive symptoms were assessed using the 9-item short form of the Center for Epidemiological Studies Depression Inventory (CES-D-9; Santor & Coyne, Reference Santor and Coyne1997). The CES-D is a reliable and widely used self-report measure of depressive symptoms. Participants rated the frequency at which each depressive symptom occurred during the past week on a four-point Likert scale, ranging from 0 (rarely or none of the time [less than 1 day]) to 3 (most of the time [5–7 days]). Final sum scores could range from 0 to 27 (see Table 2). The CES-D scores utilized in the current analyses were assessed twice during pregnancy, once during the postpartum period, and once at the time of child assessment. CES-D scores across both prenatal timepoints were averaged to create a composite score of prenatal depressive symptoms. The CES-D-9 demonstrated fair to good internal consistency across study time points (αs ranging from .76 to .85). The CES-D-9 has also been shown in prior work to be a well-validated measure of depression in adults (Corcoran & Fisher, Reference Corcoran and Fisher1987; Santor & Coyne, Reference Santor and Coyne1997), including pregnant and postpartum women (Mosack & Shore, Reference Mosack and Shore2006).
Maternal perceived stress
Maternal perceived stress symptoms were evaluated using the 10-item version of Cohen’s Perceived Stress Scale (PSS; Cohen et al., Reference Cohen, Kamarck and Mermelstein1983). The PSS is a self-report measure of generalized or nonspecific stress, which evaluates participants’ feelings about how they were able to handle day-to-day problems and hassles, how often they felt nervous and stressed, and how often they felt things were going well during the past week. Responses were made on a 5-point Likert scale, ranging from 0 (never) to 4 (almost always), with a final sum score which could range from 0 to 40 and higher scores indicating greater impairment (see Table 2). The PSS scores utilized in the current analyses were assessed twice during pregnancy, once during the postpartum period, and once at the time of child assessment. PSS scores across both prenatal timepoints were averaged to create a composite score of prenatal levels of perceived stress. The PSS demonstrated good internal consistency across study time points (αs ranging from .84 to .87). The PSS has been widely used to evaluate perceived stress symptoms in women during prenatal and postpartum periods (Nast et al., Reference Nast, Bolten, Meinlschmidt and Hellhammer2013).
Child negative affectivity
Child negative affectivity was assessed using the very short form of the Children’s Behavior Questionnaire (CBQ-VSF), a parent report measure of child temperament (Putnam & Rothbart, Reference Putnam and Rothbart2006; Rothbart et al., Reference Rothbart, Ahadi, Hershey and Fisher2001). The very short form of the CBQ is a 36-item questionnaire, yielding three factor scores, of which Negative Affectivity was used in the current analyses. The 12-item Negative Affectivity scale reflects mood instability and tendency to experience dysregulated negative emotions. When completing the scale, mothers were asked the degree to which each statement (e.g., “gets quite frustrated when prevented from doing something s/he wants to do”) described their child’s behavior over the past six months on a 7-point Likert scale, ranging from 1 (extremely untrue of your child) to 7 (extremely true of your child) (see Table 2). An average rating was calculated for the negative affectivity scale. The CBQ-VSF has been shown to demonstrate adequate internal consistency and substantial interrater reliability (Putnam & Rothbart, Reference Putnam and Rothbart2006; Rothbart et al., Reference Rothbart, Ahadi, Hershey and Fisher2001), and has been widely used in studies of child temperament and negative affectivity. Further, the CBQ-VSF takes advantage of mother’s ability to observe her child across a wide range of contexts and relies on maternal observation of concrete behaviors rather than abstract judgments of temperament to reduce the potential influence of maternal bias in reporting. Within the study sample, the CBQ-VSF demonstrated good internal consistency on the Negative Affectivity subscale (α = .84).
Statistical analysis
Identification of covariates
Spearman’s rank correlations (utilized to address skewness in tested covariates), t-tests, and ANOVAs were used to identify maternal (SES composite score, age, cohabitation status, race/ethnicity, foreign-born, concurrent depressive symptoms, early life adversity, parity) and child factors (gestational age at birth, sex, age at early childhood assessment) that might influence child negative affectivity. Study site and time from preconception assessment to conception also were considered as potential covariates. Variables associated with child negative affectivity at p < .10 level of significance were included as a covariate in all subsequent regression analyses. Only maternal age and the SES composite score met criterion for inclusion as a covariate (see Table 3).
Table 3. Associations between participant characteristics and child negative affectivity

Note. Reported tests statistics are aSpearman’s rho, b t, or c F. Maternal childhood adversity was assessed via the Risk Families Questionnaire. Concurrent maternal depressive symptoms were assessed via the Center for Epidemiological Studies Depression Inventory (CES-D). ^p < .1. *p < .05. **p < .01.
Bivariate correlations
Preliminary analyses were conducted using bivariate Pearson’s correlation coefficients, assessing the relations between preconception PTSD symptoms, prenatal and postpartum depressive symptoms and perceived stress, and child negative affectivity. Pearson’s correlations were utilized because tested variables were normally distributed (i.e., Skewness > −2 and < 2; see Table 2; George & Mallery, Reference George and Mallery2010). Spearman’s rank correlations are also available in Supplement Table S2.
Data imputation
To address data missingness, missing preconception PTSD data was imputed. Eighty-seven women provided PTSD symptom ratings prior to conception (as well as ratings of child negative affectivity) and 31 participants completed a prenatal mood or stress measure and completed the child negative affectivity measure but were missing PTSD ratings prior to conception (26% rate of missingness). Multiple imputations of missing data were generated using MPlus (Asparouhov & Muthén, Reference Asparouhov and Muthén2010; Muthén & Muthén, Reference Muthén and Muthén1998–2017), generating 20 imputed data sets. When running subsequent analyses, parameter estimates were computed and averaged over the 20 sets. Sensitivity tests were performed to assess the influence of imputation on study findings by repeating all regression and mediational models analyses including only participants with complete data.
Testing of study aims
Preconception maternal PTSD symptoms and child negative affectivity
Linear regression was run in Mplus to test the primary hypothesis that preconception maternal symptoms of posttraumatic stress predict child negative affectivity after inclusion of identified covariates. Concurrent maternal depressive symptoms were then added as a covariate to evaluate whether any effect of preconception maternal PTSD symptoms on child negative affectivity remains after accounting for maternal mental health at the time of child assessment.
Assessment of prenatal and postpartum depressive symptoms and perceived stress as mediating pathways
Finally, mediational pathways were added in exploratory analyses to examine whether prenatal and/or postpartum maternal depression symptoms may mediate the relation between maternal preconception PTSD symptoms and child negative affectivity. Prenatal and postpartum levels of perceived stress were also tested as mediators in secondary, exploratory analyses.
Results
Bivariate correlations
Preliminary bivariate correlations between maternal preconception PTSD, maternal prenatal and postpartum depressive symptoms, and child negative affectivity are presented in Table 4. Maternal preconception PTSD symptoms were positively associated with child negative affectivity on the CBQ-VSF (r = .26, p = .014). PTSD symptoms also were associated with higher prenatal and postpartum depressive symptoms (r = .46, p < .001; and r = .26, p = .020, respectively) and prenatal and postpartum perceived stress (r = .59, p <.001; and r = .48, p <.001, respectively). Prenatal and postpartum depressive symptoms in turn were associated with higher child negative affectivity scores (r = .20, p = .043; and r = .20, p = .048, respectively). Postpartum but not prenatal levels of perceived stress positively correlated with elevated child negative affectivity (r = .21, p = .037; and r = .12, p = .210, respectively).
Table 4. Pearson’s correlations between preconception PTSD symptoms, prenatal and postpartum depressive symptoms and perceived stress, and child negative affectivity

Note. *p < .05. **p < .01. ***p < .001.
Testing of study aims
Preconception maternal PTSD symptoms and child negative affectivity
Regression analyses testing the primary hypothesis revealed that greater maternal symptoms of PTSD measured prior to conception predicted heightened child negative affectivity in early childhood (β = 0.20, SE = 0.09, p = .022) even after inclusion of sociodemographic covariates (R 2 = .093; see Table 5, Model 1). Further, this association remained after covarying concurrent symptoms of maternal depression (β = 0.19, SE = 0.10, p = .045; R 2 = .096; R 2 change = .003 see Table 5, Model 2). Sensitivity analyses were performed including only participants with complete data, and as shown in Supplemental Table S3, the effect size and significance of this finding remained.
Table 5. Regression models of preconception maternal PTSD symptoms and child negative affectivity

Note. Missing preconception PTSD data was imputed (n = 118). SES = socioeconomic status (composite of maternal education and per capita household income adjusted for cost of living). *p < .05.
Assessment of prenatal and postpartum depressive symptoms and perceived stress as mediating pathways
Exploratory, post hoc analyses evaluated maternal prenatal and postpartum depressive symptoms as possible mediational pathways. This mediational model is summarized in Supplementary Figure S1. The total effect of the model was significant (β = 0.21, SE = 0.09, p = .022), however prenatal and postpartum depressive symptoms were not significant mediators (total indirect effect: β = 0.04, SE = 0.04, p = .289; specific indirect effect of prenatal depressive symptoms: β = 0.02, SE = 0.03, p = .511; specific indirect effect of postpartum depressive symptoms: β = 0.02, SE = 0.03, p = .506). Next, prenatal and postpartum levels of perceived stress were considered as mediational pathways. This mediational model is summarized in Supplementary Figure S2. The total effect of the model was significant (β = 0.20, SE = 0.09, p = .022) although neither prenatal nor postpartum levels of perceived mediated the relation between preconception PTSD symptoms and child negative affectivity (total indirect effect: β = 0.04, SE = 0.06, p = .448; specific indirect effect of prenatal levels of perceived stress: β = −0.02, SE = 0.04, p = .653; specific indirect effect of postpartum levels of perceived stress: β = 0.06, SE = 0.05, p = .250).
Discussion
The current study advances our understanding of the intergenerational impact of PTSD by prospectively evaluating maternal posttraumatic stress symptoms prior to conception and negative affectivity in the next generation. Using this prospective, longitudinal approach within a socioeconomically diverse sample of women and children, we found that more severe maternal symptoms of PTSD prior to conception predicted higher negative affectivity in their children during early childhood. Notably, the relation between maternal preconception PTSD symptoms and child negative affectivity persisted when covarying SES and concurrent maternal depressive symptoms, suggesting that this association is likely not fully accounted for by postnatal shared environmental circumstances or current maternal mental health. Further, maternal early life adversity was not associated with child negative affectivity and thus did not meet covariate criteria, suggesting that maternal mental health symptoms prior to conception may be a more robust predictor of child development than history of adverse experiences. Collectively, these results build upon our understanding of the enduring effects of PTSD on development in the next generation, suggesting that elevated PTSD symptoms prior to conception are an indicator of risk for heightened negative affectivity in the offspring. Findings also underscore the crucial importance of considering the mental health of women prior to pregnancy in the intergenerational sequelae of trauma.
The current study directly builds upon the retrospective and epidemiological literature, linking maternal recall of preconception traumatic events to poor emotional outcomes in children (Bosquet Enlow et al., Reference Bosquet Enlow, Englund and Egeland2018; Briggs et al., Reference Briggs, Silver, Krug, Mason, Schrag, Chinitz and Racine2014; McDonnel & Valentino, Reference McDonnell and Valentino2016) and adds to a very small number of prospective studies exploring the impact of preconception stress on emotional outcomes for the next generation (Hipwell et al., Reference Hipwell, Tung, Northrup and Keenan2019; Spry et al., Reference Spry, Moreno-Betancur, Becker, Romaniuk, Carlin, Molyneaux and Macdonald2020). Current findings extend the work of Hipwell et al. (Reference Hipwell, Tung, Northrup and Keenan2019), who reported that in a prospective cohort, children of women exposed to traumatic events in their own childhoods were more likely to exhibit emotion dysregulation in infancy. With our direct evaluation of PTSD symptoms (rather than exposure to traumatic events), we provide novel evidence of an intergenerational association between posttraumatic stress symptoms and child negative affectivity outcomes. This finding provides evidence that PTSD symptoms are likely part of a pathway by which maternal trauma history may have a dysregulating impact on child negative affectivity; and that PTSD symptoms measured prior to conception may be a useful indicator of intergenerational risk.
Potential mediating pathways underlying the intergenerational impact of trauma
Preconception PTSD symptoms were positively associated with symptoms of depression during pregnancy. These findings align with retrospective studies linking maternal recall of trauma history to her mental health during pregnancy (Alvarez-Segura et al., Reference Alvarez-Segura, Garcia-Esteve, Torres, Plaza, Imaz, Hermida-Barros and Burtchen2014; Atzl et al., Reference Atzl, Narayan, Rivera and Lieberman2019; River et al., Reference River, Narayan, Atzl, Rivera and Lieberman2019). Further, prenatal maternal depressive symptoms were correlated with child negative affectivity, consistent with a vast fetal programming literature prospectively documenting the influence of prenatal depression on the processes of fetal development and subsequent child socioemotional outcomes (Blair et al., Reference Blair, Glynn, Sandman and Davis2011; Davis et al., Reference Davis, Glynn, Schetter, Hobel, Chicz-Demet and Sandman2007; Erickson et al., Reference Erickson, Gartstein and Dotson2017; Glynn et al., Reference Glynn, Howland, Sandman, Davis, Phelan, Baram and Stern2018; Letourneau et al., Reference Letourneau, Dewey, Kaplan, Ntanda, Novick and Thomas2019; Werner et al., Reference Werner, Myers, Fifer, Cheng, Fang, Allen and Monk2007). We did not find evidence that maternal depressive symptoms or perceived stress during pregnancy or the postpartum period mediated the relation between preconception PTSD and child emotional outcomes, nor did the direct effect of prenatal depressive symptoms on child negative affectivity reach statistical significance in this mediational model. It is plausible that the current study was underpowered to detect the role of perinatal depression symptoms or perceived stress in mediating this relation. Given the relatively small sample size, mediational analyses should be interpreted with caution. It is also possible that other candidate pathways may be involved in this intergenerational association. For example, other domains of maternal mental health may be more directly implicated in the intergenerational impact of PTSD, including persistent perinatal PTSD symptoms. Although depression and PTSD are often comorbid (Shalev et al., Reference Shalev, Freedman, Peri, Brandes, Sahar, Orr and Pitman1998), the unique features of PTSD symptomatology such as heightened vigilance may have a more potent impact on fetal development. Multiple perinatal biological mechanisms, including stress physiology (e.g., perinatal maternal and placental HPA axis activity), epigenetic mechanisms (beginning even prior to conception), immune functioning, and gut microbiota, have also been implicated in models of intergenerational stress (Bouvette-Turcot et al., Reference Bouvette-Turcot, Fleming, Unternaehrer, Gonzalez, Atkinson, Gaudreau and Meaney2020; Bowers & Yehuda, Reference Bowers and Yehuda2016; Buss et al., Reference Buss, Entringer, Moog, Toepfer, Fair, Simhan and Wadhwa2017; Davis & Narayan, Reference Davis and Narayan2020; Keenan et al., Reference Keenan, Hipwell, Class and Mbayiwa2018; Scorza et al., Reference Scorza, Duarte, Hipwell, Posner, Ortin and Canino2019; Swales et al., Reference Swales, Stout-Oswald, Glynn, Sandman, Wing and Davis2018; Yehuda & Meaney, Reference Yehuda and Meaney2018). Additionally, maternal parenting (such as maternal warmth and sensitivity) and the security of attachment relationships have been frequently implicated in the intergenerational sequelae PTSD, as trauma history has been shown to be a risk factor for negative parent-child interactions (Cohen et al., Reference Cohen, Hien and Batchelder2008; Savage et al., Reference Savage, Tarabulsy, Pearson, Collin-Vézina and Gagné2019). It is important that future studies continue to explore possible mediating pathways and broaden the scope of candidate mechanisms considered.
Strengths, limitations, and future directions
The current study has several key strengths. Due to the challenges of recruiting and assessing women prior to pregnancy, few prospective studies of preconception mental health exist. Further, the multifaceted diversity of the study sample is a notable strength. The women in the study sample came from racial, ethnic, geographical, and socioeconomic backgrounds which are underrepresented in maternal and child health research (e.g., over a third of women identified as Latina or Hispanic and approximately a third of women identified as African American or Black) (Conradt et al., Reference Conradt, Carter and Crowell2020). Another key advantage of the current study is the use of multiple assessment timepoints. Although PTSD symptoms were only measured once in the preconception period, maternal depressive symptoms and levels of perceived stress were evaluated twice during pregnancy, once postpartum, and once during the time of childhood assessment. This approach allowed for continued evaluation of maternal mental health across the peripartum period and into early childhood.
Despite these strengths, there also are also several limitations and key identified areas for future research. First, the sample includes only mothers who had at least one prior pregnancy at the time of recruitment. There was also a high rate of attrition amongst eligible participants (48%), reflecting the usual challenges of recruiting participants prior to conception and retaining them until 3–5 years postpartum. Participants included in the current analyses were more likely to be older, Latina, and born outside of the United States, and had a longer interpregnancy interval than those who did not participate in the present study, and notably, PTSD symptoms did not differ between the two groups. These demographic predictors of attrition should be considered in interpreting study findings. Additionally, maternal PTSD symptoms were only assessed at one time point and not during pregnancy or at any postnatal time points. Future studies should evaluate maternal PTSD symptoms over time. We also evaluated PTSD symptoms dimensionally within an at-risk community sample, with 21% of participants surpassing the clinical threshold for likely PTSD diagnosis. Future work would also benefit from exploring these associations within samples of participants recruited from clinical settings and including full diagnostic assessment of PTSD symptoms. Another limitation is that child negative affectivity was assessed via maternal report of child behavior. The likelihood of bias is reduced by the CBQ measure design which asks about behavior in concrete situations. Further, we covaried maternal depressive symptoms at the time of reporting to partially account for the influence of concurrent mental health on reporting biases; however, future studies should also seek to obtain ratings from other caregivers and through direct observations of child temperament. Finally, future studies should consider additional processes of risk and resilience that may impact the intergenerational transmission of maternal stress, such as cultural factors (considering the role of enculturation, acculturation, acculturative stress and discrimination, and community and identity based protective factors) as well as benevolent childhood experiences and other maternal characteristics which may buffer against the impact of preconception PTSD symptoms.
Conclusion
The current findings have important implications for understanding the intergenerational impact of PTSD and stress. This study supports the continued expansion of the DOHaD model to consider how experiences prior to pregnancy may have lasting intergenerational consequences. Specifically, these findings carry important clinical significance, as heightened negative affectivity in early childhood is a key predictor of later psychopathology (Nigg, Reference Nigg2006), suggesting that elevated preconception PTSD symptoms may indicate risk for later mental health problems in the child. Findings underscore the critical importance of early identification of trauma and PTSD symptoms, and subsequent implementation of effective therapeutic interventions. Such screenings and therapeutic supports should be targeted not only during pregnancy and for new mothers, but also before women enter motherhood. This is important as targeted preconception interventions may confer a two-generational benefit, supporting the mental health of trauma survivors as well as disrupting intergenerational risk pathways to foster positive emotional development in children.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S0954579421001760
Acknowledgments
None.
Funding statement
This research was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD072021; Dunkel Schetter, PI) and earlier work by the Child Community Health Network (CCHN), supported through cooperative agreements with the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; U HD44207, U HD44219, U HD44226, U HD44245, U HD44253, U HD54791, U HD54019, U HD44226-05S1, U HD44245-06S1, R03 HD59584) and the National Institute for Nursing Research (U NR008929). Author N.E.M. received support from the National Institute of Mental Health (T32 MH015750).
Conflicts of interest
None.











