Abstract
Background/Objectives
This meta-analysis investigates the efficacy and safety of intravitreal anti-VEGF injections (IVI) compared to combination laser photocoagulation and IVI (LPC-IVI) in treating macular oedema secondary to retinal vein occlusion (RVO).
Subjects/Methods
A literature search of MEDLINE, EMBASE and Cochrane CENTRAL was conducted from inception until March 2021. Randomized controlled trials that reported relevant efficacy and/or safety parameters following LPC-IVI relative to IVI were included. Meta-analysis was conducted with a random effects model. The primary outcome was best-corrected visual acuity (BCVA), while secondary outcomes were central macular thickness (CMT), central retinal thickness (CRT), central subfield thickness (CST), number of IVIs received, and incidence of adverse events.
Results
A total of 10 studies were included, for which 362 eyes were randomized to LPC-IVI and 365 to IVI. In comparing macular laser photocoagulation with IVI (MLP-IVI) in BRVO patients, no significant differences were seen in final BCVA (p = 0.78) or change in BCVA (p = 0.09) after treatment. Similarly, no significant differences were seen in final CMT (p = 0.54), change in CMT (p = 0.33), final CRT (p = 0.90), change in CRT (p = 0.97), or number of injections required (p = 0.78). The same results were seen in subgroup analyses for macular laser without peripheral laser in BRVO and CRVO patients. Consistent results were observed when considering peripheral LPC-IVI to IVI in BRVO and CRVO.
Conclusions
No significant differences were seen between combination MLP-IVI or peripheral LPC-IVI relative to IVI monotherapy for final BCVA or OCT parameters in macular oedema secondary to RVO.
Similar content being viewed by others
Introduction
Retinal vein occlusion (RVO) is a common retinal vascular disease and cause of blindness, affecting up to 5.2 per 1000 people in the developed world [1, 2]. In clinical practice, RVO is subdivided into either branch (BRVO) or central retinal vein occlusion (CRVO) [2]. Macular oedema (ME) is commonly associated with RVO, where occlusion of the vein leads to increased capillary pressure and vascular permeability, resulting in ME secondary to transudation [3].
Two commonly used therapeutic options for patients with ME secondary to RVO are intravitreal anti-vascular endothelial growth factor injections (IVI) and laser photocoagulation (LPC). Other options include intravitreal steroids such as triamcinolone acetonide as well as dexamethasone intravitreal implants [4]. Anti-VEGF agents prevent angiogenesis that arises secondary to retinal ischaemia in RVO and reduce vascular permeability that causes ME [5]. In previous studies, monthly intravitreal injections of anti-VEGF agents have shown to be associated with clinically significant vision gains in BRVO and CRVO within 6 months of treatment. These gains in visual acuity were then maintained when anti-VEGF treatments were continued on an as needed (PRN) basis at 12 months of follow-up [6].
Meta-analyses have shown that intravitreal anti-VEGF agents are associated with an 80% lower risk of losing at least 15 letters of visual acuity at six months relative to sham injection in CRVO patients [7]. A Cochrane systematic review determined that, at six months, eyes treated with IVI were 2.71 times more likely to have a gain of 15 or more ETDRS letters compared to eyes receiving sham treatment [7]. After a diagnosis of ME secondary to RVO, intravitreal anti-VEGF injections (IVIs) should be used relatively soon, as early treatment has shown to have greater improvements in visual outcomes than treatment at six months post-diagnosis [8].
LPC can be either applied as a grid to the macula directly in macular laser photocoagulation (MLP) or peripherally to ischaemic areas in an effort to reduce the production of VEGF. For ME secondary to RVO, MLP is typically applied in a grid pattern [9]. Common laser wavelengths for grid photocoagulation include 532 nm (green) and 577 nm (yellow), with a spot size of 50–100 μm. The macula is exposed to the laser for 20–100 ms, with the power titrated for desired effect [10]. It has been demonstrated that MLP improves the oxygenation of the inner retina [11]. This in turn increases the oxygen tension and relieves hypoxia in the inner retina, leading to autoregulatory vasoconstriction of vessels and an increase to arteriolar resistance [12]. This reduces hydrostatic pressure in the capillaries and venules, and per Starling’s law, this decreases fluid flux from the intravascular space thus reducing tissue oedema [12]. Studies have shown that BRVO patients receiving macular grid laser have been more likely to have an improved visual acuity (10 or more ETDRS letters) at 36 months after treatment compared to those receiving no treatment [13]. In ME secondary to CRVO, macular grid photocoagulation has been shown to be less effective than bevacizumab in restoring visual acuity [14]. Peripheral LPC has been used in retinal venous occlusive disease to target peripheral areas of retinal nonperfusion [15]. Peripheral LPC may reduce pathologic VEGF levels, retinal neovascularization and ME [15].
Both combination LPC-IVI treatment and IVI monotherapy have been used in the management of RVO. There is no definite consensus as to the recommended standard of care approach, and conflicts in the literature remain. For example, Donati et al. found that MLP-IVI significantly reduced the number of IVI injections required compared to IVI monotherapy, while Campochiaro et al. found no significant difference in the number of injections required [9, 16]. Given the conflicting results that currently exist, we conducted a meta-analysis of randomized controlled trials to elucidate the comparative efficacy and safety of combined LPC and IVI relative to IVI monotherapy.
Methods
Search strategy
A systematic search of the literature was performed using OVID MEDLINE, Ovid EMBASE and Cochrane CENTRAL (database inception to March 2021; Supplementary Tables 1 and 2). Reference lists of included articles were also searched for applicable articles. The meta-analysis was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database (ID: CRD42020148978).
Eligibility criteria
Studies were included based on the following criteria: (1) randomized controlled trials, (2) included patients who received IVI monotherapy, (3) included patients who received combination LPC (i.e., either MLP or peripheral laser photocoagulation) and IVI therapy (4) provided efficacy and/or safety data for monotherapy and combination therapy study arms, (5) recruited patients with ME secondary to BRVO or CRVO.
The following exclusion criteria were used in the selection of studies: (1) non-published articles (e.g., abstracts and conference proceedings), (2) non-English articles, (3) repeat data, (4) non-randomized studies, (5) literature reviews, letters to the editor, correspondences, notes, clinical trial registrations, editorials, and forthcoming journal articles, as well as (6) articles that did not provide relevant outcome data. Given that existing studies in the published literature were used for this meta-analysis, institutional review board approval was not necessary. Nonetheless, the study adhered fully to the Declaration of Helsinki.
Study selection, data collection, and outcome measures
Two authors (NB and APS) independently reviewed the search results to select pertinent articles for inclusion via title and abstract screening, followed by full-text review. Uncertainty in inclusion was resolved by consultation with a third author (MMP). The same two authors (NB and APS) extracted the following baseline demographic and clinical data from each study arm: study design, country of origin, number of included eyes, mean cohort age, gender distribution, treatment approach and schedule (i.e., dose and frequency for IVIs and treatment parameters for LPC), duration of follow-up, specific ocular pathology (i.e., BRVO or CRVO), mean corrected distance visual acuity (BCVA), central retinal thickness (CRT), central subfield thickness (CST) and central macular thickness (CMT). Post-procedure outcomes were extracted from the included studies for monotherapy and combination therapy arms and reported using the following headings:
-
1.
Primary visual outcomes: final BCVA and change in BCVA, recorded via logarithm of minimum angle of resolution (logMAR).
-
2.
Primary structural outcomes: mean CRT, change in CRT from baseline, mean CST, change in CST from baseline, mean CMT, and change in CMT from baseline.
-
3.
For IVI treatments, the mean number of IVIs received over the course of follow-up was extracted.
-
4.
Safety parameters: total number of adverse events and incidence of individual adverse events, including generalized eye pain, dry eye, conjunctival hyperaemia, subconjunctival haemorrhage, cataracts, elevated intraocular pressure (IOP), vitreous detachment, and macular fibrosis.
Risk of bias assessment and GRADE evaluation
To assess the risk of bias across included studies, the Cochrane risk of bias tool for randomized trials was used [17]. The included domains were sequence generation, allocation concealment, masking of participants and personnel, masking of outcome assessors, incomplete outcome data, selective outcome reporting and other potential threats to validity [17]. With regards to selective outcome reporting, a 10% loss to follow-up was used to distinguish between low and high-risk studies, with studies not reporting this information being assigned an unclear risk of bias. We also assessed the incidence of authorship conflicts of interest and industry sponsorship. The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) framework was used to assess the quality of evidence (Table 1) [18].
Statistical analysis
Data for all post-treatment outcomes were collected at last follow-up. Microsoft Excel (Microsoft Corporation, Redmond, WA) was used to manage all records used in screening and selection, as well as for compiling extracted data from selected studies. Continuous variables were recorded as means±standard deviations. Categorical variables were reported as percentages of the total sample. The results of the meta-analysis were presented as a weighted mean difference (WMD) with a corresponding 95% confidence interval (95% CI) for continuous parameters, and via a risk ratio (RR) and 95% CI for categorical variables. The weighted mean was defined as \({{{\bar{\mathrm x}}}} = \frac{{\mathop {\sum}\nolimits_{i = 1}^n {w_ix_i} }}{{\mathop {\sum}\nolimits_{i = 1}^n {w_i} }}\) while the weighted standard deviation was represented by \(sd_w = \sqrt {\frac{{\mathop {\sum}\nolimits_{i = 1}^N {w_i(x_i - {{{\bar{\mathrm x}}}}_w)^2} }}{{\frac{{(N\prime - 1)\mathop {\sum}\nolimits_{i = 1}^N {w_i^2} }}{{N\prime }}}}}\). For continuous outcomes, the inverse variance analytic method was used, while a Mantel-Haenszel method was used for categorical variables. For all analyses, a random effects model was used.
All visual outcomes were converted to logMAR values prior to analysis. For results that were reported in ETDRS letters, logMAR values were calculated using the following formula: logMAR = −0.02x + 1.7, where x represented ETDRS letters. To calculate the change in visual acuity in logMAR units when presented data in ETDRS letters, the change in BCVA in logMAR units was calculated using \(\Delta {{{{{\rm{logMAR}}}}}} = - 0.02x\), where x represented the change in ETDRS letters [19].
Statistical heterogeneity was assessed in two ways: first using an I2 statistic (significance: >75%), which evaluates the percentage of variance attributable to heterogeneity, and second by using a chi-square test. The number of eyes was used as a weighting variable, and a p value of less than 0.05 was used to denote statistical significance.
Meta-analysis was conducted only if there were two or more study arms for each intervention type. Main analyses were performed on studies with BRVO patients and those with CRVO patients separately. The main analysis allowed for studies that administered macular laser with as needed peripheral LPC, while a subgroup analysis was completed on BRVO patients who only received MLP.
Review Manager (RevMan 5.3; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) was used to conduct all analyses.
Results
Study inclusions and baseline demographics
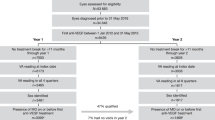
A total of 1078 records were searched, of which 25 articles were advanced to full-text screening. From these, a total of 10 RCTs were included in the meta-analysis (Fig. 1) [9, 16, 20,21,22,23,24,25,26,27]. A total of 727 eyes were included, of which 362 received combination LPC-IVI and 365 received IVI alone. A complete listing of baseline demographic information for each included study can be found in Supplementary Table 3. A complete listing of IVI dosing and laser parameters for each included study can be found in Supplementary Table 4.
A total of 620 eyes were included in BRVO studies (310 LPC-IVI, 310 IVI) and 107 eyes were included in CRVO studies (52 LPC-IVI, 55 IVI). The weighted mean age of participants was 64.0 years, with the mean cohort age ranging from 52.0 to 69.8 years. The mean percentage of male patients was 54.1% and ranged from 37.0% to 70.8% across cohorts. The mean baseline BCVA (logMAR units) was 0.60 (~20/80 Snellen), ranging from 0.30 to 0.85 (~20/40 to ~20/142 Snellen) across cohorts.
One paper had distinct CRVO and BRVO treatment arms, providing us with 11 analysis cohorts. Across the studies, eight analysis groups were BRVO-specific, for which 310 eyes received LPC-IVI and 310 eyes received IVI. Three analysis groups were CRVO-specific, for which 52 eyes received LPC-IVI and 55 received IVI. All eyes included were treated with LPC.
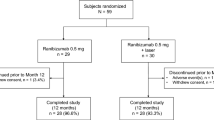
A total of 181 eyes were treated with IVI on a monthly treatment basis (92 LPC-IVI, 89 IVI) and 442 on a pro re nata (PRN) basis (220 LPC-IVI, 222 IVI). A total of 96 eyes were treated with bevacizumab (49 LPC-IVI, 47 IVI), and 545 eyes were treated with ranibizumab (271 LPC-IVI, 274 IVI).
Risk of bias assessment and GRADE evaluation
Overall, there were 55 (79%), 7 (10%), and 8 (11%) domains that had a low, unclear, and high risk of bias, respectively. There was a total of 4 (40%) studies that had at least one high-risk domain. The following domains ranked from the highest to the lowest proportion of low risk of bias: other potential threats to validity (100%), selective outcome reporting (100%), incomplete outcome data (100%), sequence generation (90%), allocation sequence concealment (80%), masking of participants and personnel (40%), and masking of outcome assessors (40%). A listing of each study and their risk of bias rating is available in Supplementary Table 5. Four studies did not specify if or how they masked outcome assessors [9, 23, 24, 27], while two studies explicitly did not mask assessors [21, 22]. Two studies reported funding support from industry sponsors, with two receiving direct funding [20, 27], and one receiving indirect funding [25]. One study disclosed conflicts of interest [20]. In the overall and subgroup analyses, the GRADE evaluation revealed a low-to-medium certainty of evidence (Table 1).
Main analysis: BRVO
A total of six studies were included in this analysis, with 114 eyes receiving MLP-IVI and 110 receiving IVI monotherapy [9, 16, 20, 21, 23, 26]. For this analysis, as needed adjunct peripheral LPC was permitted but not required.
In seven analyses, no significant differences were seen between MLP-IVI and IVI. There was no significant difference between MLP-IVI and IVI alone for final BCVA (p = 0.78, mean follow-up = 14.6 ± 9.8 months, Fig. 2A) or change in BCVA (p = 0.09, mean follow-up = 14.6 ± 9.8 months, Fig. 2B). Similarly, there was no significant difference between MLP-IVI and IVI alone in OCT parameters, such as final CMT (p = 0.54, mean follow-up = 10.0 ± 2.8 months, Fig. 2C), change in CMT (p = 0.33, mean follow-up = 10.0 ± 2.8 months, Fig. 2D), final CRT (p = 0.90, mean follow-up = 10.8 ± 1.3 months, Fig. 2E), or change in CRT (p = 0.97, mean follow-up = 10.8 ± 1.3 months, Fig. 2F). As well, there was no significant difference between MLP-IVI and IVI alone in the number of injections (p = 0.78, mean follow-up = 24.0 ± 12.0 months, Fig. 2G).
Subgroup analysis: BRVO–macular laser photocoagulation
A total of four studies were included in this comparison, which included all BRVO studies in the main analysis but removed those that administered as needed adjunct peripheral LPC. In this subgroup analysis, 74 eyes received macular MLP-IVI combination therapy and 70 received IVI alone [9, 16, 23, 26]. No significant differences were found between MLP-IVI and MLP for five analyses, which were all consistent with the main analysis (Fig. 3).
Systematic review: LPC-IVI vs IVI in BRVO
Two studies compared non-macular LPC used in combination with IVI (LPC-IVI) to IVI [22, 24, 27]. Across these studies, 170 eyes received LPC-IVI while 178 received IVI alone. These studies are reviewed below.
Goel et al. compared ranibizumab used in combination with targeted retinal laser for ME secondary to BRVO. Specifically, they used ultra-wide-field fluorescein angiography (UWFFA)-guided targeted retinal photocoagulation [22]. In this study, 17 treatment-naive BRVO patients with ME were randomized to receive 0.5 mg ranibizumab (IVI) and 18 were randomized to receive ranibizumab with UWFFA-guided laser (LPC-IVI). For each group, three injections were given at monthly intervals with PRN treatment afterwards. The study found that both groups had a statistically significant improvement (p < 0.001 in each group) in BCVA after 9 months, with the LPC-IVI group gaining 23.38 ± 7.56 letters and the IVI group gaining 25.7 ± 8.19 letters. At 9 months, both groups achieved a significant reduction in mean central subfoveal thickness (CSFT), with a reduction of 379.12 ± 242.7 μm in the IVI group (p < 0.001) and 253.75 ± 137.9 μm in the LPC-IVI group (p < 0.001). The gain in BCVA and the reduction in CSFT between LPC-IVI and IVI alone groups was not statistically significant. Between the groups, the number of injections was significantly greater in the IVI group (5.76 ± 1.3 IVI, 4.06 ± 0.99 LPC-IVI, p < 0.001).
Tadayoni et al. compared ranibizumab (IVI), ranibizumab plus laser (LPC-IVI), and laser alone (LPC) in patients with ME secondary to BRVO over 24 months [27]. No description of the laser parameters was provided by the study. After month 6, patients receiving LPC alone were eligible to receive PRN ranibizumab if visual impairment due to ME was present (LPC-IVI from month 6 arm). One hundred eighty-three eyes received IVI, 180 received LPC-IVI, 25 received LPC alone, and 63 received LPC with IVI after month 6. BCVA improvements were seen in IVI and LPC-IVI arms at 6 months and were sustained over the 24-month study duration. The mean BCVA change was significantly greater in the LPC-IVI group (15.4 ± 10.76) than the IVI group (15.0 ± 10.86) over 24 months (p < 0.001). At the end of the follow-up period, the LPC-IVI group achieved a final mean BCVA of 73.9 ± 14.59 letters, while the IVI group achieved 75.0 ± 14.65 letters. No significant differences in CSFT at 24 months were found between any of the three arms. As well, between the LPC-IVI and IVI arms, no significant difference was found in the number of ranibizumab injections required over the full follow-up period (p = 0.4259).
CRVO
A total of three studies reported on LPC used for CRVO patients, with 51 eyes receiving MLP-IVI and 47 eyes receiving IVI [20, 25]. Given that a meta-analysis could not be performed on most outcomes due to insufficient studies, we systematically review the included CRVO studies below.
Campochiaro et al. divided their subjects into CRVO and BRVO arms and randomized each cohort into patients receiving MLP plus ranibizumab versus ranibizumab alone [20]. All patients first received monthly injections of 0.5 or 2.0 mg ranibizumab for 24 weeks before re-randomizing to PRN treatment groups consisting of the same dose of ranibizumab, with or without MLP. A total of 18 CRVO patients received MLP-IVI combination therapy, and 19 CRVO patients received IVI monotherapy. In comparing the change in BCVA after 144 weeks, patients who received the combination therapy saw a gain of 0.008 ± 0.086 logMAR units (0.4 ± 4.3 ETDRS letters), compared to a reduction in visual acuity of 0.134 ± 0.074 logMAR units (6.7 ± 3.7 ETDRS letters) in those who received IVI alone (p = 0.22). Similarly, there was no significant difference in the change in CST between the two groups at 144 weeks (p = 0.94). However, the number of ranibizumab injections was significantly different (p = 0.05) between treatment groups, with the combination therapy arm requiring 17.9 ± 2.1 injections compared to IVI monotherapy requiring 12.4 ± 1.6 injections over 144 weeks [20].
Rehak et al. compared monthly ranibizumab injections (n = 12) and monthly ranibizumab plus MPL (n = 10) over a 3-month period. Both groups received ranibizumab treatment monthly for 3 months, followed by PRN injections for an additional 3 months. BCVA in patients treated with ranibizumab showed no change after 6 months (0.48 logMAR or 61 ETDRS letters at both baseline and 6 months). However, there was an improvement of 0.1 logMAR in the MLP-IVI group (5 ETDRS letters) after 6 months. There was no significant difference in the change in CRT in the MLP-IVI group (−178.5 ± 301.2 μm) relative to IVI monotherapy (−159 ± 336.7 μm) [25].
Nourinia et al. compared peripheral retinal photocoagulation to ischaemic retina in combination with intravitreal bevacizumab (LPC-IVI) to intravitreal bevacizumab alone (IVI) in the treatment of ME secondary to CRVO. In this study, 24 treatment-naive eyes received LPC-IVI and 24 eyes received IVI injections. Both groups received IVI PRN and were followed up for 9 months after the first injection. The LPC-IVI group received wide-field fluorescein angiography-guided highly selective photocoagulation of the areas of retinal capillary nonperfusion with a green diode laser of 350 μm spot size and a duration of 20 ms. In both groups, a significant improvement in BCVA was observed from the second to ninth month (p = 0.04–0.001) when adjusted for baseline values. Mean BCVA was greater in the LPC-IVI group at the sixth, seventh, and eighth months but with statistical significance only in the sixth month (p = 0.031). Between groups, the IVI-LPC arm achieved significantly greater BCVA in months four to eight (p = 0.002, 0.004, 0.002, 0.002, and 0.012) but not at the end of the follow-up period. Both groups also achieved a statistically significant reduction in CMT compared to respective baselines (p < 0.001 for both groups), but with a significant difference in thickness in the LPC-IVI group only in months four to six (p = 0.005, p = 0.022, p = 0.005). Finally, there was a statistically significant difference between the number of IVI injections required, with the LPC-IVI group requiring fewer in months four, six, seven, and eight (p = 0.022, <0.001, 0.012 and 0.038). Over the entire follow-up period of nine months, the LPC-IVI group received significantly fewer (p < 0.001) injections than the IVI group (4.05 ± 1.09 vs. 5.83 ± 1.95). No adverse events were reported in either group.
Safety analysis and complications
Seven included studies did not report any information regarding adverse events of the interventions administered [9, 20,21,22,23,24,25]. Callizo et al. reported an IOP spike in two patients (one in each group) that returned to normal levels after topical therapy [16]. Tadayoni et al. noted adverse events in 48.3% of the IVI group and 53.6% of the MLP-IVI group. They noted that eye pain, increased IOP, and conjunctival haemorrhage were the most frequently reported ocular adverse events across both groups. They also classified serious adverse events (SAEs) separately, with 1.1% of IVI patients and 2.2% of LPC-IVI patients having SAEs. Ocular SAEs included reduced BCVA (n = 2) and cataract (n = 1). Song et al. noted that three patients in the IVI group and one patient in the MLP-IVI group had an increase in IOP during the study period. As well, they reported two patients who withdrew from the study due to lacunar infarction [26].
Discussion
While IVI has proven benefit in improving the BCVA of RVO patients, it is less clear whether there are differences in outcomes with supplemental LPC [28, 29]. In this analysis, we analyzed ten randomized controlled trials, all of which compared IVI treatments to combination LPC-IVI regimens. To determine if LPC could improve the efficacy or safety profile of IVI, we analyzed BCVA, structural parameters such as CMT, the number of IVIs required, and safety endpoints.
Visual acuity and structural outcomes
No significant differences were seen between IVI monotherapies and combination MLP-IVI therapies with respect to visual acuity. In the BRVO analysis, no significant differences were seen in final BCVA or change in BCVA. The same results were observed in the BRVO subgroup analysis that included patients who received macular laser only. While a paucity of data prohibited a CRVO-specific analysis, both CRVO studies presented non-significant differences in BCVA between MLP-IVI and IVI treatment arms [20, 25]. In papers comparing LPC-IVI to IVI, one study found no significant difference in change in BCVA between LPC-IVI and IVI arms at last follow-up in BRVO patients [22], and a second study found no significant difference in CRVO patients [24]. However, Tadayoni et al. found that the mean BCVA change was significantly greater in the LPC-IVI arm compared to the IVI arm (p < 0.001) in BRVO patients [27].
In the main BRVO analysis, no significant differences were seen in CMT, change in CMT, CRT or change in CRT. No significant changes in CRT or CMT were found in the BRVO macular laser subgroup analysis. Of the two CRVO studies with MLP-IVI and IVI arms, neither study reported any significant differences in CST, CRT, or CMT between IVI and MLP-IVI arms at last follow-up [20, 25]. However, several sources of between-study heterogeneity were found. Specifically, studies treated patients with differing modalities of MLP, different anti-VEGF agents, and different anti-VEGF dosing schedules. Of the 12 forest plots included, two (Figs. 2G and 3A) had an I2 value greater than 75%, indicating significant heterogeneity in the data of certain analyses. Of the three LPC-IVI vs. IVI studies, two did not find significant differences in structural outcomes between the two arms at last follow-up in BRVO patients [22, 27], and the third found no significant difference in CRVO patients [24].
From these data, LPC as an adjunct to IVI does not further improve visual acuity or structural parameters of the retina more effectively than IVI alone.
Number of Injections
Despite the non-significant results for visual and structural outcomes, the possibility of reducing the number of IVIs needed to control symptoms would make supplemental LPC a useful adjunct therapy to IVI. If this were true, the cost and burden of treatment could be reduced [30].
In the main BRVO analysis, no significant difference was seen between the MLP-IVI and IVI arms with respect to the number of IVIs required to reduce symptoms. These same results were observed in the BRVO macular laser subgroup.
One BRVO paper indicated that MLP-IVI led to a lower number of injections required [9], while one BRVO paper found that patients in the IVI arm required fewer injections [20]. Interestingly, the studies that showed no benefit from MLP-IVI for injection burden treated all patients with IVI on a PRN basis, while the study that showed a benefit all treated patients monthly for three treatments followed by PRN treatment for 12 months [9]. Compared to IVI given on a PRN basis based on disease severity, additional MLP does not appear to reduce the number of IVIs needed.
In studies with other forms of LPC and IVI versus IVI arms, Goel et al., and Nourinia et al., found a significantly greater number of injections in the IVI arms compared to the LPC-IVI arms [22, 24]. However, Tadayoni et al. did not find any significant difference between the LPC-IVI and IVI arms in the number of injections required [27].
Complications
Few studies reported adverse events associated with IVI or MLP-IVI. Callizo et al. found the same number of complications in each treatment arm, all of which resolved before the end of the study [16]. Similarly, Tadayoni et al. found few SAEs, with 2 (1.1%) IVI patients and 4 (2.2%) IVI-LPC patients reporting SAEs. From our analysis, both treatment modalities appear to be well-tolerated options. However, many studies included in our analyses had small sample sizes, and are likely underpowered for being able to detect rare sight-threatening complications, such as endophthalmitis secondary to IVI [25]. Based on prior literature, complications of IVI include endophthalmitis, intraocular inflammation, rhegmatogenous retinal detachment, IOP elevation and ocular haemorrhage [31], while complications of macular grid laser include choroidal neovascularization and subretinal fibrosis [32].
Dosing and treatment schedules
All papers used the same IVI parameters for their IVI and MLP-IVI arms, except for Kumar et al., who randomized the IVI treatment arm to receive 3 monthly IVR injections followed by PRN administration, and the MLP-IVI treatment arm to receive a single IVR dose, followed by MLP 7 days later with PRN MLP at 4 months and beyond [23]. In this study, more frequent IVI administration in the IVI monotherapy arm could explain why this arm was associated with significantly greater BCVA gains compared to the MLP-IVI arm [23]. No other studies included in this analysis used different IVI parameters between their treatment arms, nor did they find a statistically significant difference in BCVA gain between IVI and MLP-IVI arms [9, 16, 20, 21, 25].
Campochiaro et al. treated all patients with either 0.5 mg or 2.0 mg of ranibizumab for the first 24 weeks, followed by re-randomization to MLP-IVI and IVI arms, where patients received the same dose of ranibizumab as initially assigned, along with added MLP. From weeks 24 to 144, the MLP-IVI and IVI arms received their treatments PRN, based on disease severity criteria. Campochiaro et al. did not report data for individual doses in the re-randomized MLP-IVI and IVI arms. We could not differentiate whether the dose of ranibizumab may have affected our outcomes in this or any other study.
Limitations
The limitations of this meta-analysis include the paucity of studies comparing MLP-IVI and LPC-IVI to IVI in ME secondary to RVO. There was an observed heterogeneity in laser parameters and anti-VEGF dosing and agents. As several studies have low sample sizes and short durations of follow-up, rare complications due to treatment may not have been captured. Conclusions made at the level of the study cohort may not be directly applicable to the level of the individual patient.
Conclusion
In comparing MLP-IVI combination therapies to IVI monotherapy, combination therapies appear to be of no added benefit in treating ME secondary to RVO in terms of final BCVA and structural outcomes. There was also no significant difference between LPC-IVI combination therapies and IVI monotherapy for the same endpoints. Future studies should examine whether the same results are observed beyond the controlled setting of RCTs.
References
Woo SCY, Lip GYH, Lip PL. Associations of retinal artery occlusion and retinal vein occlusion to mortality, stroke, and myocardial infarction: a systematic review. Eye. 2016;30:1031–8.
Blair K, Czyz CN. Central retinal vein occlusion. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2019. http://www.ncbi.nlm.nih.gov/books/NBK525985/. Accessed 3 Dec 2019.
Rhoades W, Dickson D, Nguyen QD, Do DV. Management of macular edema due to central retinal vein occlusion – the role of aflibercept. Taiwan J Ophthalmol. 2017;7:70–6.
Gewaily D, Muthuswamy K, Greenberg PB. Intravitreal steroids versus observation for macular edema secondary to central retinal vein occlusion. Cochrane Database Syst Rev. 2015;9:CD007324.
Kimoto K, Kubota T. Anti-VEGF agents for ocular angiogenesis and vascular permeability. J Ophthalmol. 2012. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3216356/. Accessed 27 Dec 2020.
Thach AB, Yau L, Hoang C, Tuomi L. Time to Clinically Significant Visual Acuity Gains after Ranibizumab Treatment for Retinal Vein Occlusion: BRAVO and CRUISE trials. Ophthalmology. 2014;121:1059–66.
Braithwaite T, Nanji AA, Lindsley K, Greenberg PB. Anti-vascular endothelial growth factor for macular oedema secondary to central retinal vein occlusion. Cochrane Database Syst Rev. 2014;5:CD007325.
Brown DM, Campochiaro PA, Singh RP, Li Z, Gray S, Saroj N, et al. Ranibizumab for macular edema following central retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010;117:1124–1133.e1.
Donati S, Barosi P, Bianchi M, Oum MA, Azzolini C. Combined intravitreal bevacizumab and grid laser photocoagulation for macular edema secondary to branch retinal vein occlusion. Eur J Ophthalmol. 2012;22:607–14.
He L, Blumenkranz MS. Retinal vein occlusion. Am Acad Ophthalmol. https://www.aao.org/munnerlyn-laser-surgery-center/retinal-vein-occlusion. Accessed 4 June 2020.
Stefánsson E, Machemer R, de Juan E, McCuen BW, Peterson J. Retinal oxygenation and laser treatment in patients with diabetic retinopathy. Am J Ophthalmol. 1992;113:36–8.
Stefansson E, Landers MB, Wolbarsht ML. Increased retinal oxygen supply following pan-retinal photocoagulation and vitrectomy and lensectomy. Trans Am Ophthalmol Soc. 1981;79:307–34.
Lam FC, Chia SN, Lee RM. Macular grid laser photocoagulation for branch retinal vein occlusion. Cochrane Database Syst. Rev. 2015. http://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD008732.pub2/full. Accessed 5 Dec 2020.
Russo V, Barone A, Conte E, Prascina F, Stella A, Noci ND. Bevacizumab compared with macular laser grid photocoagulation for cystoid macular edema in branch retinal vein occlusion. Retina. 2009;29:511–5.
Wykoff CC, Ou WC, Wang R, Brown DM, Cone C, Zamora D, et al. Peripheral laser for recalcitrant macular edema owing to retinal vein occlusion: the WAVE Trial. Ophthalmology. 2017;124:919–21.
Callizo J, Atili A, Striebe NA, Bemme S, Feltgen N, Hoerauf H, et al. Bevacizumab versus bevacizumab and macular grid photocoagulation for macular edema in eyes with non-ischemic branch retinal vein occlusion: results from a prospective randomized study. Graefes Arch Clin Exp Ophthalmol. 2019;257:913–20.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343. https://www.bmj.com/content/343/bmj.d5928. Accessed 5 July 2020.
Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64:380–2.
Khoshnood B, Mesbah M, Jeanbat V, Lafuma A, Berdeaux G. Transforming scales of measurement of visual acuity at the group level: visual acuity transformation. Ophthalmic Physiol Opt. 2010;30:816–23.
Campochiaro PA, Hafiz G, Mir TA, Scott AW, Solomon S, Zimmer-Galler I, et al. Scatter photocoagulation does not reduce macular edema or treatment burden in patients with retinal vein occlusion. Ophthalmology. 2015;122:1426–37.
Cao W, Cui H, Biskup E. Combination of grid laser photocoagulation and a single intravitreal ranibizumab as an efficient and cost-effective treatment option for macular edema secondary to branch retinal vein occlusion. Rejuvenation Res. 2019;22:335–41.
Goel S, Kumar A, Ravani R, Chandra P, Chandra M, Kumar V. Comparison of ranibizumab alone versus ranibizumab with targeted retinal laser for branch retinal vein occlusion with macular edema. Indian J Ophthalmol. 2019;67:1105.
Kumar P, Sharma YR, Chandra P, Azad R, Meshram GG. Comparison of the safety and efficacy of intravitreal ranibizumab with or without laser photocoagulation versus dexamethasone intravitreal implant with or without laser photocoagulation for macular edema secondary to branch retinal vein occlusion. Folia Med. 2019;61:240–8.
Nourinia R, Emamverdi M, Ramezani A, Amizadeh Y, Khorshidifar M, Behnaz N, et al. Peripheral ischemic retinal photocoagulation in addition to intravitreal bevacizumab versus intravitreal bevacizumab alone for the treatment of macular edema secondary to central retinal vein occlusion: a randomized double-masked controlled clinical trial. Retina. 2020;40:1110–7.
Rehak M, Tilgner E, Franke A, Rauscher FG, Brosteanu O, Wiedemann P. Early peripheral laser photocoagulation of nonperfused retina improves vision in patients with central retinal vein occlusion (Results of a proof of concept study). Graefes Arch Clin Exp Ophthalmol. 2014;252:745–52.
Song S, Yu X, Zhang P, Gu X, Dai H. Combination of ranibizumab with macular laser for macular edema secondary to branch retinal vein occlusion: one-year results from a randomized controlled double-blind trial. BMC Ophthalmology. 2020;20:1–9.
Tadayoni R, Waldstein SM, Boscia F, Gerding H, Gekkieva M, Barnes E, et al. Sustained benefits of ranibizumab with or without laser in branch retinal vein occlusion. Ophthalmology. 2017;124:1778–87.
Spooner K, Fraser-Bell S, Hong T, Chang AA. Five-year outcomes of retinal vein occlusion treated with vascular endothelial growth factor inhibitors. BMJ Open Ophthalmol. 2019;4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6440600/. Accessed 4 Jan 2020.
Li C, Wang R, Liu G, Ge Z, Jin D, Ma Y, et al. Efficacy of panretinal laser in ischemic central retinal vein occlusion: a systematic review. Exp Ther Med. 2019;17:901–10.
Anon. Retinal physician - the cost-effectiveness of anti-VEGF treatment in diabetes. Retin Physician. https://www.retinalphysician.com/issues/2017/june-2017/the-cost-effectiveness-of-anti-vegf-treatment-in-d. Accessed 22 Nov 2020.
Ghasemi Falavarjani K, Nguyen QD. Adverse events and complications associated with intravitreal injection of anti-VEGF agents: a review of literature. Eye. 2013;27:787–94.
Deschler EK, Sun JK, Silva PS. Side-effects and complications of laser treatment in diabetic retinal disease. Semin Ophthalmol. 2014;29:290–300.
Author information
Authors and Affiliations
Contributions
NB was responsible for screening potentially eligible studies, extracting and analyzing data, interpreting results, and writing the manuscript. APS contributed to data extraction, data analysis and critical revision of the manuscript. MMP was responsible for designing the review protocol, conducting the search, conducting the meta-analyses, interpreting results and critical revision of the manuscript. RHM and PJK assisted in designing the review protocol, interpreting results, and critical revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
MMP: Financial Support (to institution)—PSI Foundation. PJK: Advisory board—Novartis, Alcon, Bayer Roche, Novelty Nobility; Financial support (to institution)—Bayer, Roche, Novartis; Financial support—Novartis, Bayer; Equity owner—ArcticDx. RHM: Advisory board— Bayer, Novartis, Allergan, Roche; Financial Support (to institution)—Bayer, Novartis.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bhambra, N., Sayal, A.P., Popovic, M.M. et al. Combination intravitreal anti-vascular endothelial growth factor inhibitors and macular laser photocoagulation relative to intravitreal injection monotherapy in macular oedema secondary to retinal vein occlusion: a meta-analysis of randomized controlled trials. Eye 36, 2271–2278 (2022). https://doi.org/10.1038/s41433-021-01833-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01833-2