Abstract
Objectives
For patients with polypoidal choroidal vasculopathy (PCV), intravitreal anti-vascular endothelial growth factor (anti-VEGF) combination therapy has been shown to be cost-saving relative to monotherapy in a clinical trial setting. However, whether this also applies to real-world settings is unclear. We aim to compare the real-world functional outcomes and cost-effectiveness of intravitreal anti-VEGF combination therapy relative to monotherapy, to investigate whether combination therapy is truly cost-saving.
Methods
We used a Markov model to simulate a hypothetical cohort of PCV patients treated at Singapore National Eye Centre. Model parameters were informed by coarsened exact matched estimates of a two-year retrospective study of patients who initiated treatment in 2015. Treatment options included intravitreal aflibercept, bevacizumab, or ranibizumab, as monotherapy or in combination with full-fluence verteporfin photodynamic therapy.
Results
The two-year logMAR letters gains were significant for combination therapy ( + 10.6, P = 0.006) but not monotherapy (−2.2, P = 0.459). Over 20 years, a PCV patient would cost the health system SGD 48,790 under monotherapy and SGD 61,020 under combination therapy. Quality-adjusted life-years (QALYs) were estimated to be 7.41 for monotherapy and 7.80 for combination therapy. The incremental cost-effectiveness ratio of combination therapy was SGD 31,460/QALY, which is less than the common willingness-to-pay threshold of per capita gross domestic product of Singapore (SGD 88,990/QALY). Sensitivity analysis showed that combination therapy remained incrementally cost-effective, but not cost-saving.
Conclusions
Our study shows that combination therapy is good value for money but is likely to increase costs when applied in real-world settings.
Similar content being viewed by others
Introduction
Polypoidal choroidal vasculopathy (PCV) is a variant of age-related macular degeneration (AMD), clinically characterized by aneurysmal dilatations at the end of a type 1 neovascularization. These aneurysmal lesions have a propensity to develop large pigment epithelial detachment and massive subretinal haemorrhages. PCV accounts for 20–50% of all cases of exudative AMD in East Asians [1,2,3,4].
Before the advent of anti-vascular endothelial growth factor (VEGF) therapy, photodynamic therapy (PDT) was widely used to treat neovascular AMD (nAMD). However, anti-VEGF therapy achieved greater visual improvements than PDT and overtook PDT as the standard of care. While combining anti-VEGF with PDT did not achieve significant additional benefit compared to anti-VEGF monotherapy in the DENALI and Mont Blanc trials [5], the EVEREST study showed that initial combination therapy in eyes with PCV achieved superior visual gains, higher polyp closure rate, and lower retreatment needs compared to monotherapy with ranibizumab [6, 7]. On the other hand, the PLANET study reported no benefit from combining PDT as a rescue therapy with aflibercept [8, 9]. As such, both anti-VEGF monotherapy and initial combination therapy with verteporfin photodynamic therapy (PDT) are currently accepted as standards of care [6, 8, 10, 11]. While initial combination therapy costs substantially more upfront due to PDT, a higher number of reinjections may be required under monotherapy which would drive up cost in the long run.
Doble et al. recently analysed EVEREST II trial data and reported that initial combination therapy is more effective and less costly (i.e. a dominant strategy) than ranibizumab monotherapy when taking a lifetime perspective, suggesting that it both improves health and saves money [12]. Nevertheless, it is unclear if this finding also holds in a real-world clinical setting as both costs and outcomes are likely to differ from clinical trials [13,14,15]. At least 3 anti-VEGF agents (ranibizumab, aflibercept, off-label use of bevacizumab) are widely used in clinical practice and the cost of these agents vary significantly. Bevacizumab, being used “off-label”, costs significantly less than FDA-approved agents. In the current study, we evaluated the incremental cost-effectiveness of initial combination therapy relative to anti-VEGF monotherapy using the two-year functional outcomes of a recently described real-world patient cohort and simulated costs and effectiveness from the healthcare system perspective over 20 years, which represents the average conditional life expectancy of these patients. To our knowledge, this is the first real-world study comparing initial combination therapy (defined as PDT applied within 3 months of commencing anti-VEGF therapy) and anti-VEGF monotherapy for patients with PCV.
Materials and methods
Study Design and participants
This is a retrospective study of a previously described cohort of 199 treatment-naïve PCV patients at the Retina clinic at the Singapore National Eye Centre, who commenced anti-VEGF monotherapy or combination therapy with verteporfin PDT between January and December 2015 [13]. The presence of PCV was confirmed at a presentation by the treating physician using analysis of multimodal imaging.
Two-year functional outcomes were collected for this cohort with exclusion of patients who did not complete two-year follow-up (range 20–28 months). This research was conducted in accordance with the Declaration of Helsinki and the local Institutional Review Board (studies 2009/788/A and R697/47/2009). Patients’ individual informed consent was exempted due to the retrospective nature of the study and use of anonymized clinical data. Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Statistical analysis
As treatment was not randomized, we performed coarsened exact matching to control for confounding when comparing outcomes of monotherapy and combination therapy patients [16]. Matching was based on age (45–54, 55–64, 65–74, 75–84, 85 + ), gender, race (Chinese, Malay, Indian/Others), class (subsidized, private, others), and presenting visual acuity (taken as the best visual acuity either aided, unaided, with or without pin hole; 20/20 to 20/40, 20/50 to 20/80, 20/100 to 20/160, worse than 20/160). Matching weights were used in subsequent analysis to account for unequal number of matches per strata.
Changes to visual acuity were measured in terms of logarithm of the minimum angle of resolution (log-MAR) letters. Statistically significant changes in visual acuity over time were determined by a paired Student t-test. Statistically significant differences in baseline characteristics and outcomes between monotherapy and combination therapy patients were determined by the Student t-test allowing for unequal variance. All tests are two-tailed and based on the 5% significance level. Statistical analysis was performed using Stata version 15.1 [17].
Cost-effectiveness analysis
We built a Markov cohort model in TreeAge Pro 2020, version R2.0 [18], to estimate the cost and effectiveness of combination therapy relative to monotherapy in accordance with CHEERS guidelines [19]. Effectiveness was measured in terms of quality-adjusted life-years (QALYs). The model has five health states, four for each visual acuity range and one for death (Fig. 1). The model begins with a representative cohort of patients aged 71 who present at the Retina clinic in the Singapore National Eye Centre. The initial distribution of visual acuity is 24.6% for 20/20 to 20/40, 23.6% for 20/50 to 20/80, 16.6% for 20/100 to 20/160, and 35.2% for worse than 20/160. After each annual cycle, patients may remain in the current health state, transition to a better or worse visual functioning category, or die (absorbing state). Adverse events were not modelled because there were no statistically significant differences in the safety profiles of treatments across the two arms [20].
Transition probabilities between non-death states in the first and second years were estimated from the retrospective data and adjusted for all-cause mortality based on the 2016 Singapore Life Tables [21]. Beyond the second year, we assumed that both treatments allowed patients to maintain their visual functioning at the end of the second year until death. Hence, only transitions to the death state were possible. This assumption was relaxed in sensitivity analyses.
Each non-death health state is associated with an annual healthcare cost, estimated from the retrospective data. Direct healthcare costs were calculated based on individual healthcare resource utilization and 2020 unit costs of unsubsidized private charges from the Singapore National Eye Centre and unsubsidized prices for medicines (eTable 1). These charges are set to ensure cost recovery for non-subsidized patients. As a result, they are a reasonable representation of costs from the healthcare system perspective. A visual acuity-based quality-of-life weight was derived following the same approach as Doble et al [12]. The death state was assigned zero cost and zero quality-of-life weight. We assume treatment futility for patients with worse than 20/160 visual acuity at the end of the third year because this group is considered legally blind. All other patients continue to receive treatment and incur respective costs until death. All costs and QALYs were discounted at 3% per annum, following Singapore Agency for Care Effectiveness guidelines [22]. The incremental cost-effectiveness ratio (ICER) was calculated by dividing the difference in cost between combination and monotherapy by the difference in QALYs. We adopt a willingness-to-pay threshold based on Singapore’s 2019 gross domestic product (GDP), SGD 88,990/QALY, to determine treatment cost-effectiveness in the base case.
Sensitivity analysis
In sensitivity analysis, we checked the robustness of the 20-year ICERs to different statistical matching techniques, cost of anti-VEGF agents, and assumptions on patient outcomes beyond the second year. To investigate sensitivity to matching techniques, we re-estimated the model using transition probabilities and healthcare costs derived without any matching, as well as those derived using nearest-neighbour propensity score matching. To investigate sensitivity to cost of anti-VEGF agents, we assumed all anti-VEGF agents used are bevacizumab, which is assumed to be non-inferior. To investigate sensitivity to assumptions after the second year, we re-estimated models allowing for subgroups of patients to continue moving between non-death states until death and incurring treatment cost based on second-year estimates. Probabilistic sensitivity analysis was also conducted to assess how much the uncertainty of model parameters influenced the cost-effectiveness estimates. 1000 Monte Carlo simulations were used to generate costs from Gamma distributions and transition probabilities from Dirichlet distributions based on each parameter’s mean and standard error (eTable 2 and 3).
Results
Participant baseline characteristics and treatment exposure
Of the 199 PCV cases previously reported [13], 28 patients were omitted from this analysis because they received PDT more than 3 months after commencing anti-VEGF treatment. Of the remaining cases, 83 monotherapy patients and 58 combinations therapy patients completed 2 years of follow-up. 21% of monotherapy and 12.1% of combination therapy patients dropped out before the end of 2 years. Differences in patient characteristics and treatment exposure between treatment groups were small and not statistically significant (Table 1). Over the 2 years, patients received 8.3 ± 5.4 intravitreal anti-VEGF treatments under monotherapy (5.2 in first year, 3.1 in the second year) and 9.3 ± 5.2 intravitreal anti-VEGF treatments under combination therapy (5.8 in first year, 3.5 in the second year). The majority of anti-VEGF treatments comprised of bevacizumab (69% for monotherapy, 72% for combination therapy). Use of aflibercept, bevacizumab, and ranibizumab, as well as the number of consultation visits, were not statistically different between treatment groups. On average, combination therapy patients received 1.4 PDT sessions.
Coarsened exact matching produced matches between 56 monotherapy and 43 combination therapy patients. Because exact matches were performed over gender, racial, and patient class, their weighted proportions are identical by construction (Table 1). Other characteristics such as age and presenting visual acuity were also not statistically different. Total number of intravitreal anti-VEGF treatments received were slightly more similar after matching, with 9.9 ± 5.7 under monotherapy vs. 9.6 ± 5.2 under combination therapy.
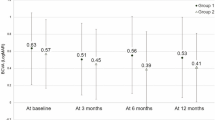
Efficacy
Visual outcomes for matched patients receiving monotherapy and combination therapy during the 2-year study period are shown in Table 2. The mean change in visual acuity at 2 years for the monotherapy group was −2.2 ± 19.9 letters (p = 0.459) compared to a significant vision gain of 10.6 ± 23.5 letters (p = 0.006) for the combination therapy group. For patients presenting with good vision (20/40 or better, 19.5%), the difference between combination and monotherapy groups was small. In contrast, for the subgroup who presented with poor vision (worse than 20/160, 31.7%), combination therapy achieved significantly higher visual acuity gains than monotherapy group. For the remaining eyes presenting with moderate visual loss, combination therapy group achieved numerically higher visual gains although the difference did not meet statistical significance.
Cost-effectiveness
Table 3 reports the cost-effectiveness of monotherapy and combination therapy over 20 years. Among all eyes, those who received monotherapy and combination therapy respectively cost the healthcare system SGD 48,790 and SGD 61,020 and realized 7.41 QALYs and 7.80 QALYs. The incremental cost ratio (ICER) of combination therapy was SGD 31,460/QALY, which is substantially lower than the threshold of SGD 88,990/QALY. Over time horizons shorter than 20 years, ICERs increase since incremental QALY gains accrue over a shorter period (eTable 4). Nevertheless, the 5-year ICER remained below the cost-effectiveness threshold.
For patients presenting with 20/40 or better, combination therapy dominates monotherapy as it is less expensive and marginally more effective. Unlike the rest of the cohort, the predominant anti-VEGF agent in this subgroup using monotherapy was aflibercept (eTable 5). Consistent with Table 2, incremental effectiveness of combination therapy is greater for those patients presenting with the poorest visual functions. However, the incremental cost of treating these patients under monotherapy also increased substantially while remaining below the cost-effectiveness threshold.
Sensitivity
For sensitivity analysis, we tested the robustness of our results to the matching procedure. Including unmatched patients in the analysis (n = 83 for monotherapy, n = 58 for combination therapy) reduced the incremental cost and effectiveness of combination therapy (eTable 6). This was expected as patients who were administered combination therapy tended to have larger lesions and more advanced disease. As a result, the unmatched estimates are likely to underestimate the incremental benefits and costs of combination therapy. Even with the biased estimates, we find that combination therapy is still cost-effective relative to monotherapy over the 20-year time horizon. Estimates based on propensity score matching produced a lower ICER.
We performed sensitivity analysis by assuming all anti-VEGF agents are bevacizumab (eTable 7). There was little change to incremental cost or cost-effectiveness since the use of more costly anti-VEGF agents are similar for both treatment groups as a whole. When stratified by baseline visual acuity, combination therapy still dominates monotherapy for the best vision group and remains incrementally cost-effective for other vision groups.
We also tested the sensitivity of our findings to a variety of assumptions regarding cost and visual outcomes beyond the second year (eTable 8). In the first scenario, patients with visual acuity worse than 20/160 continue to incur treatment cost until death. In the second scenario, all patients continue to transition among non-death states. ICERs for both scenarios are only slightly higher compared to the base case, suggesting that, separately, assumptions on treatment futility for the poorest vision group and whether patients maintain visual functionality beyond the second year do not materially affect findings. In the third scenario, patients whose visual acuity becomes worse than 20/160 after the second year never improve and discontinue treatment, while those whose visual acuity is 20/160 or better continue to transition between health states and incur treatment cost. Under these assumptions, combination therapy is only marginally cost-effective with an ICER of SGD 80,020/QALY.
At the threshold of one times the GDP per capita per QALY (SGD 88,990/QALY), combination therapy is incrementally cost-effective compared to monotherapy or dominates monotherapy in 66.6% of iterations over the 10-year horizon, and in 69.7% of iterations over the 20-year horizon (eFigure 1). As willingness-to-pay increases, the percentage of iterations where combination is cost-effective or dominates plateaus around 80% due to the uncertainty surrounding model parameters. At a threshold of SGD 50,300/QALY for the 10-year horizon and SGD 39,300/QALY for the 20-year horizon (i.e., where the lines cross), we would be indifferent to both treatments from a cost-effectiveness perspective.
Discussion
The two-year follow-up of the matched monotherapy and combination therapy cohorts showed that vision did not significantly change from baseline for cases with presenting vision between 20/20 and 20/160, while those with baseline vision worse than 20/160 retained their significant one-year visual gains up to two years. These findings are comparable to real-world outcomes reported elsewhere [13, 23,24,25] and highlight generally poorer presenting vision in real-world practice and greater potential for visual improvement in these patients.
A previous study comparing anti-VEGF ranibizumab monotherapy with PDT combination therapy using randomized trial data found that combination therapy was more effective and cost-saving compared to monotherapy over a 20-year horizon [12]. In this study using real-world clinical data, we confirm that combination therapy is more effective but found that it was more costly for the same time horizon. Even so, combination therapy remained highly cost-effective based on per capita GDP as the willingness-to-pay threshold. We also found that time on treatment is an important factor influencing cost-effectiveness. Combination therapy was incrementally cost-effective over a 5-year horizon or longer, but not over a 2-year horizon. This suggests that treatment recommendations for very elderly PCV patients might differ as they would incur greater costs at the start of treatment under combination therapy but are unlikely to accrue enough QALY gains over their remaining years of life for the treatment to be cost-effective for them.
Our results were influenced by two major differences between the real-world evidence generated from clinical practice and results from the randomized trial. First, unlike the trial data, bevacizumab, a low-cost off-label anti-VEGF agent, is used more commonly than ranibizumab and aflibercept in many clinical practices worldwide. Assuming bevacizumab is non-inferior to ranibizumab and aflibercept (which is the case for other macular conditions) [26,27,28,29] the use of bevacizumab will lower the incremental cost-effectiveness of combination therapy [12]. Second, compared to PCV patients recruited for EVEREST II [12], PCV patients that presented at these clinics were slightly older (by 3 years on average) and more likely to have baseline vision worse than 20/160 (35.2% vs. 5.9%) and less likely to have baseline vision 20/40 or better (24.6% vs. 32.1%). Since combination therapy tends to be less cost-effective for patients with poorer baseline vision, overall cost-effectiveness was reduced in the clinical settings. These results highlight the importance of real-world evidence as it shows that neither cost nor effectiveness results should be assumed to generalize from randomized trials, which often have high internal validity but poor external validity [30].
Limitations
Our study is subject to several limitations inherent in non-randomized trial data. First, the selection of patients into monotherapy or combination therapy is likely based on factors that also influence treatment outcomes. While we controlled for these to the extent possible via matching, other potential confounders (such as PCV lesion size, structural damage to the central macula, presence of massive subretinal haemorrhage) remain. If patients with more advanced PCV tend to be assigned combination therapy because they are less likely to improve under monotherapy, the unmatched estimators would understate the incremental effectiveness of combination therapy. Hence, our estimates may be interpreted as conservative. Second, the study’s 2-year outcomes could be biased by selective attrition, which is difficult to verify. However, comparing the baseline characteristics and first-year outcomes of those who completed two years of study and those who dropped out did not reveal statistically significant differences (eTable 9). Third, in the absence of data on long-term outcomes, ICERs are highly dependent on assumptions on treatment futility and whether patients maintain visual functioning after the second year. If patients do not maintain vision gains and that treatment is futile when vision worsens below 20/160, we find that combination therapy is only marginally cost-effective based on a threshold of per capita GDP per QALY gained. Lastly, given it is doubtful whether bevacizumab is truly non-inferior to other agents, the results of our study may only be generalizable to countries where bevacizumab is predominantly used [31].
Conclusion
This is the first study to demonstrate the incremental effectiveness and cost-effectiveness of combination therapy over monotherapy for PCV patients in a real-world clinical setting. Matched analysis of clinical data from Singapore National Eye Centre showed that combination therapy patients achieved statistically greater visual acuity gains after 2 years of follow-up. However, unlike prior studies based on clinical trials, our study did not find combination therapy to be cost-saving. This is due to the popularity of low-cost anti-VEGF agents and a larger proportion of patients presenting with poor vision. Nevertheless, it remains a cost-effective option, especially in the long run, for patients presenting with polypoidal choroidal vasculopathy.
SUMMARY
What was known before
-
Anti-vascular endothelial growth factor (anti-VEGF) combination therapy is cost-saving relative to monotherapy in a clinical trial setting for treating polypoidal choroidal vasculopathy (PCV).
-
It is unclear whether this applies in real-world settings.
What this study adds
-
Combination therapy is incrementally cost-effective to monotherapy in this real-world multi-ethnic Asian cohort, but not cost-saving.
-
While combination therapy is good value for money, it is likely to increase costs.
References
Jordan-Yu JM, Teo K, Fan Q, Gana JC, Leopando AK, Nunes S, et al. Phenotypic and genetic variations between Asian and Caucasian polypoidal choroidal vasculopathy. Br J Ophthalmol. 2020. https://doi.org/10.1136/bjophthalmol-2020-317537.
Cheung CMG, Lai TYY, Teo K, Ruamviboonsuk P, Chen SJ, Kim JE, et al. Polypoidal choroidal vasculopathy: consensus nomenclature and non-indocyanine green angiograph diagnostic criteria from the Asia-Pacific ocular imaging society PCV workgroup. Ophthalmology. 2020;128:443–52.
Cheung CMG, Lai TYY, Ruamviboonsuk P, Chen SJ, Chen Y, Freund KB, et al. Polypoidal choroidal vasculopathy: definition, pathogenesis, diagnosis, and management. Ophthalmology 2018;125:708–24.
Yannuzzi LA, Sorenson J, Spaide RF, Lipson B. Idiopathic polypoidal choroidal vasculopathy (IPCV). Retina 2012;32:1–8.
Cheung GCM, Lai TYY, Gomi F, Ruamviboonsuk P, Koh A, Lee WK. Anti-VEGF therapy for neovascular AMD and polypoidal choroidal vasculopathy. Asia-Pacific J Ophthalmol. 2017;6:527–34.
Koh A, Lee WK, Chen LJ, Chen SJ, Hashad Y, Kim H, et al. EVEREST study: efficacy and safety of verteporfin photodynamic therapy in combination with ranibizumab or alone versus ranibizumab monotherapy in patients with symptomatic macular polypoidal choroidal vasculopathy. Retina. 2012;32:1453–64.
Lim TH, Lai TYY, Takahashi K, Wong TY, Chen LJ, Ruamviboonsuk P, et al. Comparison of Ranibizumab with or without Verteporfin Photodynamic therapy for polypoidal choroidal vasculopathy: the EVEREST II randomized clinical trial. JAMA Ophthalmol. 2020;138:935–42.
Lee WK, Iida T, Ogura Y, Chen SJ, Wong TY, Mitchell P, et al. Efficacy and safety of intravitreal aflibercept for polypoidal choroidal vasculopathy in the PLANET study: a randomized clinical trial. JAMA Ophthalmol. 2018;136:786–93.
Wong TY, Ogura Y, Lee WK, Iida T, Chen SJ, Mitchell P, et al. Efficacy and safety of intravitreal aflibercept for polypoidal choroidal vasculopathy: 2-year results of the PLANET Study. Am J Ophthalmol. 2019;204:80–9.
Chan WM, Lam DS, Lai TY, Liu DT, Li KK, Yao Y, et al. Photodynamic therapy with verteporfin for symptomatic polypoidal choroidal vasculopathy: one-year results of a prospective case series. Ophthalmology 2004;111:1576–84.
Spaide RF, Donsoff I, Lam DL, Yannuzzi LA, Jampol LM, Slakter J, et al. Treatment of polypoidal choroidal vasculopathy with photodynamic therapy. 2002. Retina 2012;32:529–35. Suppl 1
Doble B, Finkelstein EA, Tian Y, Saxena N, Patil S, Wong TY, et al. Cost-effectiveness of intravitreal Ranibizumab With verteporfin photodynamic therapy compared with ranibizumab monotherapy for patients with polypoidal choroidal vasculopathy. JAMA Ophthalmol. 2020;138:251–9.
Fenner BJ, Ting DSW, Tan ACS, Teo K, Chan CM, Mathur R, et al. Real-world treatment outcomes of age-related macular degeneration and polypoidal choroidal vasculopathy in Asians. Ophthalmol Retin. 2020;4:403–14.
Mehta H, Tufail A, Daien V, Lee AY, Nguyen V, Ozturk M, et al. Real-world outcomes in patients with neovascular age-related macular degeneration treated with intravitreal vascular endothelial growth factor inhibitors. Prog Retin Eye Res. 2018;65:127–46.
Finger RP, Puth MT, Schmid M, Barthelmes D, Guymer RH, Gillies M, Lifetime outcomes of anti-vascular endothelial growth factor treatment for neovascular age-related macular degeneration. JAMA Ophthalmol. 2020;138:1234–40.
Iacus SM, King G, Porro G Causal inference without balance checking: Coarsened exact matching. Political analysis. 2012:1–24.
StataCorp LLC. Stata Statistical Software. College Station, TX 2017.
TreeAge Software. TreeAge Pro. Williamstown, MA 2020.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated health economic evaluation reporting standards (CHEERS)—explanation and elaboration: a report of the ispor health economic evaluation publication guidelines good reporting practices task force. Value Health. 2013;16:231–50.
Koh A, Lai TYY, Takahashi K, Wong TY, Chen LJ, Ruamviboonsuk P, et al. Efficacy and safety of Ranibizumab with or without verteporfin photodynamic therapy for polypoidal choroidal vasculopathy: a randomized clinical trial. JAMA Ophthalmol. 2017;135:1206–13.
Singapore Department of Statistics. Complete Life Tables 2015-2016 for Singapore Resident Population 2017. Available from: https://www.singstat.gov.sg/-/media/files/publications/population/lifetable15-16.pdf.
Agency for Care Effectiveness. Drug Evaluation Methods and Process Guide 2019. Available from: https://www.ace-hta.gov.sg/public-data/our-process-and-methods/ACE%20methods%20and%20process%20guide%20for%20drug%20evaluation%20(20%20Dec%202019).pdf.
Miyata M, Ooto S, Yamashiro K, Tamura H, Hata M, Ueda-Arakawa N, et al. Five-year visual outcomes after anti-VEGF therapy with or without photodynamic therapy for polypoidal choroidal vasculopathy. Br J Ophthalmol. 2019;103:617–22.
Wataru K, Sugiyama A, Yoneyama S, Matsubara M, Fukuda Y, Parikh R, et al. Five-year outcomes of photodynamic therapy combined with intravitreal injection of ranibizumab or aflibercept for polypoidal choroidal vasculopathy. PLoS One. 2020;15:e0229231.
Koh A, Lai TYY, Wei WB, Mori R, Wakiyama H, Park KH, et al. Real-world effectiveness and safety of ranibizumab treatment in patients with and without polypoidal choroidal vasculopathy: twelve-month results from the luminous study. Retina 2020;40:1529–39.
Group CR, Martin DF, Maguire MG, Ying GS, Grunwald JE, Fine SL, et al. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N. Engl J Med. 2011;364:1897–908.
Scott IU, VanVeldhuisen PC, Ip MS, Blodi BA, Oden NL, Awh CC, et al. Effect of bevacizumab vs aflibercept on visual acuity among patients with macular edema due to central retinal vein occlusion: the score2 randomized clinical trial. JAMA 2017;317:2072–87.
Hykin P, Prevost AT, Vasconcelos JC, Murphy C, Kelly J, Ramu J, et al. Clinical effectiveness of intravitreal therapy with ranibizumab vs aflibercept vs bevacizumab for macular edema secondary to central retinal vein occlusion: a randomized clinical trial. JAMA Ophthalmol. 2019;137:1256–64.
Cai S, Bressler NM. Aflibercept, bevacizumab or ranibizumab for diabetic macular oedema: recent clinically relevant findings from DRCR.net Protocol T. Curr Opin Ophthalmol. 2017;28:636–43.
Deaton A, Cartwright N. Understanding and misunderstanding randomized controlled trials. Soc Sci Med. 2018;210:2–21.
Bro T, Derebecka M, Jørstad ØK, Grzybowski A. Off-label use of bevacizumab for wet age-related macular degeneration in Europe. Graefes Arch Clin Exp Ophthalmol. 2020;258:503–11.
Acknowledgements
We thank Wee Siang Tay and Wei Han Melvin Wong for excellent research assistance.
Funding
This work was supported by Duke-NUS Medical School and Singapore Eye Research Institute.
Author information
Authors and Affiliations
Contributions
CMGC and EAF contributed to the study design. BJF contributed to data acquisition. JC, EAF, BJF and CMGC contributed to analysis and interpretation of results. JC and BJF drafted the manuscript with critical input from EAF, KYCT and CMGC. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval statement
This research was conducted in accordance with the Declaration of Helsinki and the local Institutional Review Board (studies 2009/788/A and R697/47/2009). Patients’ individual informed consent was exempted due to the retrospective nature of the study and use of anonymized clinical data. Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Chay, J., Fenner, B.J., Finkelstein, E.A. et al. Real-world cost-effectiveness of anti-VEGF monotherapy and combination therapy for the treatment of polypoidal choroidal vasculopathy. Eye 36, 2265–2270 (2022). https://doi.org/10.1038/s41433-021-01856-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01856-9