Abstract
Objective
We present a novel strategy in cardiac surgery with a cardiopulmonary bypass with low-dose heparin and Nafamostat mesylate as an anticoagulant (NM-CPB), which reduces postoperative neurological complications.
Method and results
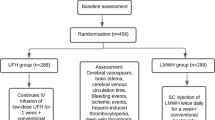
19 patients with a mean age of 63.6 ± 20.2 years (range 24–91) and an indication of early cardiac surgery with intracranial complication (ICC) underwent surgery with NM-CPB. The preoperative diagnoses included seven cases of infective endocarditis and six of left atrial appendage thrombosis. ICC were noticed in seven cases with hemorrhages (hemorrhagic infarction: n = 4, subarachnoid hemorrhage: n = 3) and 12 without hemorrhage (large infarction: n = 10, small-multiple infarction at the risk for hemorrhagic transformation: n = 2). The mean interval between a diagnosis and cardiac surgery was 1.1 ± 1.5 days in the ICH cases and 1.4 ± 1.4 days otherwise.
In-hospital mortality was 5.3%. The mean CPB time was 146.7 ± 66.03 min, the mean dose of NM, heparin were 2.23 ± 1.59 mg/kg/hr and 56.8 ± 20.3 IU/kg, respectively. The mean activated clotting time (ACT) was 426.8 ± 112.4 s. No further intracranial bleeding and no new hemorrhages were observed after surgery.
Conclusions
In early cardiac surgery with ICC, especially with hemorrhage, NM-CPB reduced postoperative neurological complications. We plan to use NM-CPB to expand the indications and to establish an early aggressive treatment.



Similar content being viewed by others
References
Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, et al. 2015 ESC Guidelines for the management of infective endocarditis. Eur Heart J. 2015;36(44):3075–128.
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–226.
Nakamura M, Uzuka T, Sato H, Kondo M, Sakta J, Kodama F. Early surgery with aggressive surgical approach to improve 6-month outcomes in patients with active infective endocarditis: contribution of cerebral preoperative magnetic resonance imaging. Gen Thorac Cardiovasc Surg. 2019;67(5):427–35.
Hitomi Y, Ikari N, Fujii S. Inhibitory effect of a new synthetic protease inhibitor (FUT-175) on the coagulation system. Haemostasis. 1985;15(3):164–8.
Sakamoto T, Kano H, Miyahara S, Inoue T, Izawa N, Gotake Y. Efficacy of nafamostat mesilate as anticoagulation during cardiopulmonary bypass for early surgery in patients with active infective endocarditis complicated by stroke. J Heart Valve Dis. 2014;23(6):744–51.
Ota T, Okada K, Kano H, Okita Y. Cardiopulmonary bypass using nafamostat mesilate for patients with infective endocarditis and recent intracranial hemorrhage. Interact Cardiovasc Thoracic Surg. 2007;6(3):270–3.
Miura T, Eishi K. Current treatment of active infective endocarditis with brain complications. Gen Thorac Cardiovasc Surg. 2013;61(10):551–9.
Hosono M, Sasaki Y, Hirai H, et al. Considerations in timing of surgical intervention for infective endocarditis with cerebrovascular complications. J Heart Valve Dis. 2010;19(3):321–5.
Shang E, Forrest GN, Chizmar T, Chim J, Brown JM, Zhan M. Mitral valve infective endocarditis: benefit of early operation and aggressive use of repair. Ann Thorac Surg. 2009;87(6):1728–34.
Eishi K, Kawazoe K, Kuriyama Y, Kitoh Y, Kawashima Y, Omae T. Surgical management of infective endocarditis associated with cerebral complications. Multi-center retrospective study in Japan. J Thorac Cardiovasc Surg. 1995;110(6):1745–55.
Nakatani S, Ohara T, Ashihara K, et al. JCS 2017 guideline on prevention and treatment of infective endocarditis. Circ J. 2019;83(8):1767–809.
Pettersson GB, Coselli JS, Pettersson GB, Coselli JS, Hussain ST, Griffin B, et al. 2016 The American Association for Thoracic Surgery (AATS) consensus guidelines: surgical treatment of infective endocarditis: executive summary. J Thorac Cardiovasc Surg. 2017;153(6):1241–58.
Baddour LM, Wilson WR, Bayer AS, Fowler VG, Tleyjeh IM, Rybak MJ. Infective endocarditis in adults: Diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435–86.
García-Cabrera E, Fernández-Hidalgo N, Almirante B, Ivanova-Georgieva R, Noureddine M, Plata A. Neurological complications of infective endocarditis risk factors, outcome, and impact of cardiac surgery: a multicenter observational study. Circulation. 2013;127(23):2272–84.
Ruttmann E, Willeit J, Ulmer H, Chevtchik O, Höfer D, Poewe W. Neurological outcome of septic cardioembolic stroke after infective endocarditis. Stroke. 2006;37(8):2094–9.
Okita Y, Minakata K, Yasuno S, Uozumi R, Sato T, Ueshima K, et al. Optimal timing of surgery for active infective endocarditis with cerebral complications: A Japanese multicentre study. Eur J Cardiothorac Surg. 2016;50(2):374–82.
Saito S, Shindo S, Tsudaka S, Uchida K, Shirakawa M, Yoshimura S. Resolving thrombus in the left atrial appendage by edoxaban treatment after acute ischemic stroke: report of 2 cases. J Stroke Cerebrovasc Dis. 2016;25(10):e188–91.
Saito S, Tomita H, Kimura Y, Shiroto H, Hagii J, Metoki N, et al. Reduced smoke-like echo and resolved thrombus in the left atrium with rivaroxaban therapy in an acute cardioembolic stroke patient. J Stroke Cerebrovasc Dis. 2014;23(6):1747–9.
Yasaka M, Yamaguchi T, Miyashita T, Tsuchiya T. Regression of intracardiac thrombus after embolic stroke. Stroke. 1990;21(11):1540–4.
Fang BR, Kuo LT. Recurrent cerebral embolism and impending detachment of a previous nonmobile left atrial thrombus following initiation of anticoagulant therapy in a patient with nonvalvular atrial fibrillation. Echocardiography. 2001;18(6):527–9.
Tabata E, Yasaka M, Wakugawa Y, Komori M, Mori K, Tsurusaki Y, et al. Increase in the size of an intracardiac thrombus during dabigatran therapy (110 mg b.i.d.) in an acute cardioembolic stroke patient. Cerebrovasc Dis Extra. 2013;3(1):78–80.
Yamamoto S. Left atrial myxoma surgically resected in acute phase of hemorrhagic cerebral infarction: report of a case. Kyobu Geka. 2007;60(3):237–41.
Yasuda S, Tokunaga S, Matsuki Y, Okamoto H, Machida D, Masuda M. Left atrium ball thrombus in a patient with hemorrhagic cerebral infarction. Ann Thorac Surg. 2013;96(6):2236–8.
Despotis GJ, Gravlee G, Filos K, Levy J. Anticoagulation monitoring during cardiac surgery: a review of current and emerging techniques. Anesthesiology. 1999;91:1122–51.
Miyamoato Y, Nakano S, Kaneko M, Takano H, Matsuda H. Clinical evaluation of a new synthetic protease inhibitor in open heart surgery effect on plasma serotonin and histamine release and blood conservation. ASAIO J. 1992;38(3):395–8.
Tanaka K, Takao M, Yada I, Yusas M, Kusagawa M, Deguchi K. Alterations in coagulation and fibrinolysis associated with cardiopulmonary bypass during open heart surgery. J Cardiothorac Anesth. 1989;3(2):181–8.
Sato S, Tanaka K, Kondo C, Morimoto T, Yada I, Yuasa H, et al. Nafamostat mesilate administration during cardiopulmonary bypass decreases postoperative bleeding after cardiac surgery. ASAIO Trans. 1991;37(3):194–5.
Tanaka K, Kondo C, Takagi K. Effects of nafamostat mesilate on platelets and coagulofibrinolysis during cardiopulmonary bypass surgery. ASAIO J. 1993;39(3):545–9.
Murase M, Usui A, Tomita Y, Maeda M, Koyama T, Abe T. Nafamostat mesilate reduces blood loss during open heart surgery. Circulation. 1993;88(5):432–6.
Fukata Y. Reduction in dose of heparin by combined use of nafamostat mesilate for the control of cardiopulmonary bypass. Iryo. 1994;48(3):196–201.
Acknowledgements
The authors would like to thank Prof. Emeritus Yutaka Okita and the department of cardiovascular surgery Kobe University for their kind guidance and continuous support.
Funding
The authors declare no grants, and sources of funding related to the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest related to the manuscript.
Institutional review board approval
All procedures used in this research were approved by the Ethical Committee of Okinawa Nanbu Prefectural Medical Center and Childrenʼs Medical Center, (No 22, Jun 29, 2017).
Informed consent
Written informed consent was obtained from the patient for publication of this article and accompanying images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yamazato, T., Oyama, N., Fujii, T. et al. Aggressive early surgical strategy in patients with intracranial hemorrhage: a new cardiopulmonary bypass option. Gen Thorac Cardiovasc Surg 70, 602–610 (2022). https://doi.org/10.1007/s11748-021-01743-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-021-01743-w