Abstract
Aim/hypothesis
It remains unclear whether people with diabetes exhibiting non-albuminuric kidney insufficiency have higher risk of kidney function decline and mortality compared with those exhibiting preserved kidney function without albuminuria. Furthermore, information regarding the incidence of albuminuria in people with this unique phenotype is sparse. Here, we aimed to elucidate the risk of the kidney outcomes and all-cause mortality in people with diabetes exhibiting non-albuminuric kidney insufficiency.
Methods
In this retrospective cohort study, 8320 Japanese adults with type 2 diabetes were classified into four groups based on the presence of albuminuria and kidney insufficiency at baseline, defined as urinary albumin/creatinine ratio of equal to or above 30 mg/g and eGFR of less than 60 ml min−1 1.73 m−2, respectively. The primary composite kidney endpoint was a 50% decrease in eGFR from baseline or the initiation of kidney replacement therapy. The annual percentage change in eGFR slope and progression of albuminuria category were evaluated as the secondary and tertiary kidney endpoints, respectively. All-cause death was also set as the endpoint.
Results
Compared with people exhibiting non-albuminuric preserved kidney function, those with non-albuminuric kidney insufficiency had the higher risk for the primary kidney endpoint (HR 4.1; 95% CI 2.5, 6.7; p < 0.001), steep percentage change in eGFR slope (-1.96%/year vs -1.36%/year, p < 0.001), incidence of albuminuria (HR 2.1; 1.7, 2.6; p < 0.001) and all-cause mortality (HR 1.5; 1.2, 2.0; p = 0.003). In the sensitivity analyses treating the incidence of albuminuria as a competing risk, people with non-albuminuric kidney insufficiency still had higher risk for the primary kidney endpoint and all-cause mortality than those with non-albuminuric preserved kidney function (subdistribution HR 2.8; 1.4, 5.6; p = 0.004; and 1.6; 1.1, 2.2; p = 0.014, respectively).
Conclusions/interpretation
People with type 2 diabetes exhibiting non-albuminuric kidney insufficiency had poorer kidney outcomes and life prognosis than those exhibiting non-albuminuric preserved kidney function.
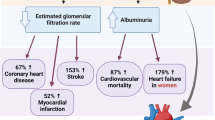
Graphical abstract

Similar content being viewed by others

Introduction
Non-albuminuric kidney insufficiency, a unique phenotype of kidney disease in people with diabetes, has had a great deal of attention [1,2,3,4,5]. Several large, serial cross-sectional studies have shown that the prevalence of this phenotype has increased over the past few decades [6,7,8,9], the reasons for which may be explained, at least in part, by increase in regression of albuminuria owing to the remarkable progress in comprehensive diabetes management, including better glycaemic control and increased use of renin–angiotensin system inhibitors [6,7,8,9,10,11]. On the other hand, previous studies have shown that a decline in kidney function can occur prior to the development of albuminuria [2, 12,13,14,15].
The available evidence so far has shown that albuminuria is a significant risk factor for kidney function decline and all-cause mortality in people with diabetes, regardless of whether kidney insufficiency exists [16,17,18,19,20,21]. However, it is highly controversial whether those with non-albuminuric kidney insufficiency have higher risks of these outcomes than those exhibiting preserved kidney function without albuminuria [18,19,20, 22, 23]. The latest large cohort studies of people with diabetes have concluded that those with non-albuminuric kidney insufficiency were not at a higher risk of decline in kidney function than those exhibiting preserved kidney function without albuminuria [18, 19], which is inconsistent with the findings of previous population-based cohort studies [22, 23]. The aforementioned study from Japan also showed no increase in mortality in those with this phenotype of kidney disease [19], unlike other studies [18, 20, 23]. Furthermore, information regarding the incidence of albuminuria in people with non-albuminuric kidney insufficiency is sparse; therefore, the progression process of kidney disease in this population remains largely unknown. Here, we aimed to elucidate the clinical implications of non-albuminuric kidney insufficiency on kidney outcomes and all-cause mortality in people with diabetes.
Methods
Study design and ethical issues
This single-centre retrospective cohort study, based on the clinical and laboratory databases of our hospital, was designed in adherence to the tenets of the Declaration of Helsinki, and was performed as a part of the ‘Cohort Study Elucidating Factors Associated with the Pathogenesis and Prognosis of Diabetic Kidney Disease’, performed at the Diabetes Center in the Tokyo Women’s Medical University School of Medicine. The local ethics committee approved the protocol, waiving the need for informed consent owing to the non-prospective interventional design (approval no. 3932). Instead, the institution's website offered an opt-out opportunity for participants.
Participants
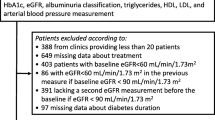
From the hospital database, we initially identified 8810 Japanese people aged ≥ 18 years with type 2 diabetes who visited the Diabetes Center, Tokyo Women’s Medical University School of Medicine from 1 August 2003 to 30 June 2017, without a history of chronic kidney replacement therapy (KRT; chronic dialysis or kidney transplantation). The following data were collected: body weight, blood pressure, HbA1c, serum creatinine and lipid variables, urinary albumin and urinary creatinine, all of which were measured on the same day of a regular outpatient visit. The earliest date of the collected data was set as the index date for each subject if multiple measurements were available during the above-mentioned period.
The exclusion criteria included pregnant women (n = 48), participants with malignant diseases (n = 160), a history of unilateral nephrectomy (n = 7), biopsy-proven diagnosis of non-diabetic nephropathy (n = 2) and an acute kidney injury or postrenal failure at baseline (n = 2). We also excluded 271 participants with no serum creatinine measurements after the index date (n = 257) and missing baseline profile data (n = 14). Eventually, 8320 participants were eligible for this study (Fig. 1). All relevant baseline data were available for the 8320 participants, and their serum creatinine levels were measured at least once after the index date. The baseline characteristics of the 8320 participants and 271 participants with missing data are presented in electronic supplementary material (ESM) Table 1. In this study, the complete-case analysis was adopted.
The 8320 participants were classified into four groups according to the absence or presence of albuminuria and kidney insufficiency at baseline, as defined below.
Measurements
Laboratory data were measured using random blood and first morning urine samples. The direct enzymatic method or the Friedewald formula (if triacylglycerol levels were 4.52 mmol/l) was used for determination of serum LDL-cholesterol levels. HbA1c levels measured as the Japan Diabetes Society (JDS) values were converted into the National Glycohemoglobin Standardization Program (NGSP) values using the formula proposed by the JDS [24]. To estimate GFR, we adopted the formula proposed by the Japanese Society for Nephrology [25]. On the basis of the Clinical Practice Guidelines proposed by Kidney Disease: Improving Global Outcomes (KDIGO) [26, 27], kidney insufficiency and albuminuria, measured using first morning urine samples, were defined as eGFR of < 60 ml min−1 1.73 m−2 and urinary albumin/creatinine ratio (UACR) of ≥ 30 mg/g, respectively. The latter was further classified into microalbuminuria (30 ≤ UACR < 300 mg/g) and macroalbuminuria (UACR ≥ 300 mg/g). Chronic kidney disease (CKD) was defined as having either kidney insufficiency or albuminuria [26, 27].
Endpoints and follow-up
The primary composite kidney endpoint was either a decrease in eGFR of ≥ 50% from baseline or the initiation of KRT, whichever came first. To inadvertently avoid capturing episodes of reversible acute kidney injury, we judged that the endpoint was reached only when the aforementioned criteria lasted for at least 3 months. The secondary kidney endpoints were the absolute eGFR slope (ml min−1 1.73 m−2 per year) and percentage change in eGFR slope (%/year) from baseline, which were restricted to participants who were followed up for ≥ 2 years based on results of a recent meta-analysis [28]. The tertiary kidney endpoint was the category progression of albuminuria (i.e., from non-albuminuria to micro- or macroalbuminuria, or from micro- to macroalbuminuria), determined using at least two consecutive increases in UACR. All-cause death was also set as the endpoint.
The administrative censoring date was set to 31 January 2018. For the survival analyses of the primary and tertiary kidney endpoints, the last follow-up date for each participant was defined as the date when the individual reached the endpoint, or the date when serum creatinine or UACR was last measured during the follow-up period without reaching the endpoint. For the analyses of all-cause mortality, the last follow-up date for each participant was defined as the date when the individual died or last visited our hospital during the follow-up period.
Statistical analysis
All analyses were completed using SAS software version 9.4 (SAS Institute, Cary, NC, USA). A two-tailed p value of < 0.05 was considered statistically significant.
Differences in proportions or means of baseline data between the four groups were compared using the χ2 test, ANOVA or Kruskal–Wallis test as appropriate. The multivariable logistic regression analysis was used to clarify the clinical characteristics of the group exhibiting non-albuminuric kidney insufficiency. The multivariable Cox proportional hazards model or the multivariable linear regression model was used to compare each endpoint between the groups. The adjusted (standardised) cumulative incidence of the endpoints was calculated using regression estimates from the relevant Cox model [29]. The eGFR slope was estimated using the linear mixed-effects model with random intercept and slope. The percentage change in eGFR slope was calculated using the following equation: 100 × eGFR slope/baseline eGFR.
In the multivariable logistic regression analysis treating the group exhibiting non-albuminuric kidney insufficiency as a dependent variable, the following five variables at baseline were incorporated as independent variables: age, sex, history of coronary artery disease or stroke, systolic blood pressure and HbA1c. In all multivariable models used for comparison between the groups in each outcome, these five variables were incorporated as covariates.
A series of sensitivity analyses were conducted. First, to examine the impact of non-albuminuric kidney insufficiency on reaching the primary kidney endpoint and death unaccompanied by the incidence of albuminuria (in other words, to exclude effects of the albuminuria incidence during the follow-up period on these endpoints), the Fine and Gray subdistribution hazards model, which is the competing risks model, was adopted for the comparison between the two groups with non-albuminuric kidney insufficiency and without CKD. In these analyses, the incidence of albuminuria before reaching each endpoint was treated as a competing risk. Second, the Fine and Gray subdistribution hazards model, wherein death before reaching the endpoints was treated as a competing risk, was used for the analyses of the primary and tertiary kidney endpoints (ESM Table 2). For the analysis of all-cause mortality, the initiation of KRT was treated as a competing risk (ESM Table 2). Third, we addressed the exclusion of people with non-diabetic nephropathy. Individuals with haematuria, defined as occult blood with scores ranging from 1 + to 3 + assayed by Uropaper α II (to September 2005) and III (from October 2005) (Eiken Chemical, Tokyo, Japan), were excluded because haematuria has been recognised as an atypical presentation of diabetic nephropathy [30]. Of 8159 people with information on haematuria at baseline, 7423 without haematuria were assessed (Model 1 in ESM Table 3). People without diabetic retinopathy despite exhibiting CKD were likely to have non-diabetic nephropathy. Therefore, of 6746 people with information on diabetic retinopathy at baseline, diagnosed by ophthalmologists in our hospital, 1072 exhibiting CKD without retinopathy were excluded. Eventually, 5674 people were assessed (Model 2 in ESM Table 3). Fourth, in addition to the above-mentioned five variables, the following variables at baseline were incorporated as covariates (ESM Table 4): smoking status (current/former vs never), use of ACE inhibitors or angiotensin receptor blockers (ARBs), BMI and LDL-cholesterol levels (Model 1); the same variables as in Model 1 plus the use of sodium–glucose cotransporter 2 inhibitors or glucagon-like peptide-1 receptor agonists and the date of baseline data, which was classified into the three groups as follows: 2003 to 2007, 2008 to 2012 and 2013 to 2017 (Model 2); and the same variables as in Model 2 plus the number of creatinine or UACR measurements per year (Model 3). The analysis of Model 3 was conducted to mitigate the bias due to differences in the number of these measurements performed during the follow-up period. Fifth, to mitigate the potential impact of bias in the presence of non-albuminuric kidney insufficiency, the propensity score (PS) matching method was used (ESM Table 5). The PS was estimated using the logistic regression model that included the following 12 covariates: the above-mentioned five variables plus smoking status, use of ACE inhibitors or ARBs, BMI, diastolic blood pressure, triacylglycerols, HDL-cholesterol and LDL-cholesterol. Triacylglycerol levels were transformed into common logarithmic values. A 1:2 greedy nearest-neighbour matching with a calliper width equal to 0.2 of the SD of the logit of the PS was conducted. Finally, in people aged over 65 years, the association of non-albuminuric kidney insufficiency with the primary kidney endpoint and all-cause mortality was analysed (ESM Table 6), in which kidney insufficiency was further classified as 50 ≤ eGFR < 60 ml min−1 1.73 m−2 and eGFR < 50 ml min−1 1.73 m−2, referencing a large prospective cohort study of people with chronic kidney insufficiency [31].
Results
Baseline characteristics
The mean (± SD) age of the 8320 participants, including 2988 women and 5332 men, was 61 ± 12 years. As shown in Table 1, individuals with kidney insufficiency were more likely to be older, to have a higher rate of history of coronary artery disease or stroke and to have lower HbA1c levels than those with preserved kidney function, regardless of the presence of albuminuria. Individuals with albuminuria were more likely to have higher usage rate of ACE inhibitors or ARBs, higher BMI and higher systolic blood pressure than those without albuminuria. In the multivariable logistic regression model, non-albuminuric kidney insufficiency was significantly associated with a higher rate of history of coronary artery disease or stroke (OR 1.2; 95% CI 1.1, 1.5; p = 0.010), more advanced age (OR per 10 years: 2.1; 95% CI 2.0, 2.3; p < 0.001), lower systolic blood pressure (OR per 10 mmHg: 0.88; 95% CI 0.85, 0.91; p < 0.001) and lower HbA1c levels (OR per 1%: 0.85; 95% CI 0.80, 0.91; p < 0.001), but not with sex (OR vs female: 1.0; 95% CI 0.8, 1.1; p = 0.693).
Summary of KRT initiation, mortality and each kidney endpoint
Of the 8320 people, 501 died during the median follow-up period of 6.7 years (IQR: 3.2–10.9 years). There were 471 cases of KRT initiation. The incidence rates per 1000 person-years of KRT and death were 8.2 and 8.5, respectively. There were 90 cases of death after KRT initiation. Of the 501 deceased cases, 161, 47, 98 and 195 resulted from malignancy, coronary artery disease or stroke, other known causes and undetermined causes, respectively.
Of the 8320 people, 787 reached the primary kidney composite endpoint, including 611 with a ≥ 50% decrease in eGFR and 176 who initiated KRT before experiencing a ≥ 50% decrease in eGFR during the median follow-up of 5.7 years (IQR: 2.6–10.1 years). The median number of creatinine measurements performed during the follow-up period was 4.7 per year (IQR: 2.9–7.3 per year). There were 381 cases of death prior to reaching the primary kidney endpoint.
In the analyses to estimate eGFR slope, which was the secondary kidney endpoint, 6720 people with a follow-up period of ≥ 2 years were assessed. The median follow-up period was 7.6 years (IQR: 4.4–11.4 years). The median absolute eGFR slope (ml min−1 1.73 m−2 per year) and percentage change in eGFR slope (%/year) from baseline were -1.27 (IQR: -2.27 to -0.52) and -1.75 (IQR: -3.24 to -0.71), respectively. The median number of creatinine measurements performed during the follow-up period was 4.3 per year (IQR: 2.7–6.7 per year).
In the 6335 people with non- and microalbuminuria at baseline, in whom UACR levels were measured at least once after the index date, the median follow-up period for category progression of albuminuria, which was the tertiary kidney endpoint, was 5.1 years (IQR: 2.2–9.1 years). Of the 4763 people with normoalbuminuria and the 1572 with microalbuminuria, 607 and 304 reached the tertiary endpoint, respectively. The median number of UACR measurements performed during the follow-up period was 1.2 per year (IQR: 0.9–1.8 per year). There were 250 cases of death prior to reaching the tertiary kidney endpoint.
Association of non-albuminuric kidney insufficiency with each kidney endpoint and mortality
People with non-albuminuric kidney insufficiency had a significantly higher risk for reaching the primary kidney endpoint than those without CKD (Table 2, Fig. 2a). When kidney insufficiency and albuminuria were further classified as 45 ≤ eGFR < 60 ml min−1 1.73 m−2, 30 ≤ eGFR < 45 ml min−1 1.73 m−2 and eGFR < 30 ml min−1 1.73 m−2, and micro- and macroalbuminuria, respectively, the result analysed in the 12 groups was consistent with the above-mentioned findings (Table 3).
(a) Adjusted cumulative incidence of the primary composite kidney endpoint in four groups classified based on the absence or presence of albuminuria and kidney insufficiency at baseline. In this analysis, 8320 people were assessed. (b) Adjusted cumulative incidence of the category progression of albuminuria in the four groups. In this analysis, 6335 people with non- and microalbuminuria at baseline, in whom UACR levels were measured at least once after the index date, were assessed. (c) Adjusted cumulative incidence of all-cause mortality in the four groups. In this analysis, 8320 people were assessed. ‘No CKD’ was defined as UACR < 30 and eGFR ≥ 60. The primary composite kidney endpoint was either a decrease in eGFR of ≥ 50% from baseline or the initiation of KRT, whichever came first. The following variables were used as covariates in the analyses: age, sex, history of coronary artery disease or stroke, systolic blood pressure and HbA1c
As shown in Fig. 3b, the group with non-albuminuric kidney insufficiency had more individuals with greater percentage change in eGFR slope than the group without CKD, unlike the case in the absolute eGFR slope (Fig. 3a). The adjusted percentage change in eGFR slope, but not the absolute adjusted eGFR slope, for people with non-albuminuric kidney insufficiency was significantly steeper than that for those without CKD (Table 2).
(a) Overlay histograms of eGFR slopes in people with no CKD and in those with non-albuminuric kidney insufficiency. (b) Overlay histograms of percentage changes in eGFR slope in people with no CKD, and in those with non-albuminuric kidney insufficiency. In the two overlay histograms, 4603 people exhibiting non-albuminuria at baseline with a follow-up period of ≥ 2 years were assessed. Red and blue bars show the proportion of people with no CKD and non-albuminuric kidney insufficiency, respectively. The purple region shows the overlap between the two distributions. ‘No CKD’ was defined as UACR < 30 and eGFR ≥ 60
People with non-albuminuric kidney insufficiency had a higher risk of the incidence of albuminuria than those without CKD (Table 2, Fig. 2b).
Non-albuminuric kidney insufficiency was also at a higher risk of all-cause mortality than non-CKD (Tables 2, 4, Fig. 2c).
The sequence of the incidence of the primary kidney endpoint, albuminuria and death in people without CKD and in those with non-albuminuric kidney insufficiency
As shown in Fig. 4a, of the 3971 people without CKD at baseline, in whom UACR levels were measured at least once after the index date, 45 (1.1%) experienced the primary kidney endpoint, 458 (11.5%) experienced the incidence of albuminuria and 138 (3.5%) died during the study period. Of the 45 people who reached the primary kidney endpoint, 18 did not experience the incidence of albuminuria during the study. Of the 138 deceased cases, 113 did not experience the incidence of albuminuria.
(a) Sequence of the incidence of the primary kidney endpoint, albuminuria and death in 3971 people with no CKD at baseline, in whom UACR levels were measured at least once after the index date. (b) Sequence of the incidence of the primary kidney endpoint, albuminuria and death in 792 people with non-albuminuric kidney insufficiency at baseline, in whom UACR levels were measured at least once after the index date. ‘No CKD’ was defined as UACR < 30 and eGFR ≥ 60. The primary composite kidney endpoint was either a decrease in eGFR of ≥ 50% from baseline or the initiation of KRT, whichever came first
Of the 792 people with non-albuminuric kidney insufficiency at baseline, in whom UACR levels were measured at least once after the index date, 25 (3.2%) experienced the primary kidney endpoint, 149 (18.8%) experienced the incidence of albuminuria and 67 (8.5%) died during the study period. Of the 25 people who reached the primary kidney endpoint, 15 did not experience the incidence of albuminuria during the study. Of the 67 deceased cases, 55 did not experience the incidence of albuminuria (Fig. 4b).
Sensitivity analyses
The analysis that treated the incidence of albuminuria before reaching the primary kidney endpoint as a competing risk in 4763 people with non-albuminuria at baseline, in whom UACR levels were measured at least once after the index date, showed that those with non-albuminuric kidney insufficiency (n = 792) remained at a significantly higher risk of the primary kidney endpoint than those without CKD (n = 3971; subdistribution HR 2.8; 95% CI 1.4, 5.6; p = 0.004). In the analysis in which all-cause mortality was set as the endpoint, this phenotype of kidney disease was associated with a higher risk for all-cause mortality unaccompanied by incidence of albuminuria than non-CKD (subdistribution HR 1.6; 95% CI 1.1, 2.2; p = 0.014). Results of other sensitivity analyses were also consistent with the above-mentioned findings (ESM Tables 2–6). In the PS matching analysis, the two groups were well balanced on all baseline covariates except for eGFR, with a standardised difference of < 0.1 for each variable (ESM Tables 7–9).
Discussion
This single-centre, large retrospective cohort study of Japanese adults with type 2 diabetes showed that those with non-albuminuric kidney insufficiency had a significantly higher risk for the decline in kidney function, assessed based on both the time to kidney events and time-series data, incidence of albuminuria and all-cause mortality than those without CKD. In the sensitivity analyses using the Fine and Gray subdistribution hazards model, in which the incidence of albuminuria before reaching the primary kidney endpoint or death was treated as a competing risk, the present study confirmed that non-albuminuric kidney insufficiency was a risk factor for reaching the primary kidney endpoint and death unaccompanied by incidence of albuminuria. Other sensitivity analyses also strengthened the robustness of the findings.
In contrast to the present findings, a cohort study from the USA involving 10,185 participants with type 2 diabetes enrolled in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) clinical trial found no increase in the incidence rate of end-stage kidney disease (ESKD) in 432 people with non-albuminuric kidney insufficiency compared with those without CKD [18]. A cohort study of 2953 Japanese people with type 2 diabetes also showed that the HR of a 30% decrease in eGFR was not higher in 203 people with non-albuminuric kidney insufficiency than in those without CKD [19]. These conflicting results may be explained, at least in part, by the small number of individuals with non-albuminuric kidney insufficiency, which was overcome in the present study. Indeed, a cohort study of over 1 million participants from the general population showed that people with non-albuminuric kidney insufficiency had a significantly higher risk of ESKD than those without CKD [23], as was the case in a population-based study of 65,589 participants [22], supporting our findings.
The absolute eGFR slope in people with diabetes exhibiting non-albuminuric kidney insufficiency varied widely among studies, between 0.17 and 1.9 ml min−1 1.73 m−2 per year [16,17,18,19], unlike the approximated 1.0 ml min−1 1.73 m−2 per year in those without CKD, evaluated in larger cohorts including the present study [18, 19]. Furthermore, only one study showed an annual percentage change in eGFR slope [18], which is especially crucial for the comparison of groups with completely different levels of GFR at baseline. In the present study, the percentage change in eGFR slope of people with non-albuminuric kidney insufficiency was significantly steeper than that of those without CKD, supporting the higher rate of reaching the primary kidney endpoint.
In the present study, the incidence rate per 1000 person-years of death was 8.5, which was comparable to the rates of 5.0–12.0 reported by other large cohort studies of Japanese people with type 2 diabetes [19, 32, 33]. The mortality rates in the aforementioned US study and the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicentre study [18, 20] were obviously higher than those in the present and other Japanese studies [19, 32, 33], yielding more statistical power to detect significant associations with mortality. Indeed, unlike the aforementioned study from Japan [19], in those studies, people with non-albuminuric kidney insufficiency had a significantly higher risk of all-cause mortality than those without CKD [18, 20]. In the present study with a large number of people with this phenotype of kidney disease, the number of deaths was comparable to that in the US study [18], allowing the detection of a higher risk of mortality in this population in Japan.
When people exhibiting non-albuminuric kidney insufficiency at baseline had albuminuria thereafter, the phenotype was no longer non-albuminuric kidney insufficiency at that time. In the sensitivity analysis treating incidence of albuminuria as a competing risk, the present study showed that people exhibiting this phenotype of kidney disease still had a higher risk for reaching the primary kidney endpoint and all-cause mortality unaccompanied by incidence of albuminuria than those without CKD, suggesting that non-albuminuric kidney insufficiency itself is a risk factor for these outcomes. Nonetheless, in people with non-albuminuric kidney insufficiency at baseline, the incidence of albuminuria preceded the primary composite kidney endpoint at a much higher frequency, as was the case in those exhibiting non-CKD at baseline in the present and previous studies [12, 13, 15]. Furthermore, people with non-albuminuric kidney insufficiency at baseline were more likely to have albuminuria than those without CKD at baseline, consistent with previous studies [12, 34]. These findings suggest that the development of ESKD in the absence of albuminuria may occur rarely in people with diabetes. Indeed, a cohort study of 2420 Pima Indians with type 2 diabetes showed that among the 287 individuals who initiated KRT or died because of diabetic nephropathy, only two (0.7%) did not experience albuminuria during the follow-up period [35], as was the case in a cohort study of people with type 1 diabetes [13].
Consistent with the available evidence to date [16,17,18,19,20,21, 36, 37], the results of the present study confirmed that albuminuria was associated with kidney function decline and all-cause mortality, regardless of whether kidney insufficiency existed. However, when albuminuria was further classified into microalbuminuria and macroalbuminuria, an increased risk of all-cause mortality in people with microalbuminuria was not observed (Table 4), unlike in the case of the primary kidney endpoint (Table 3). Meanwhile, a cohort study of people with CKD from Italy reported that those with diabetes exhibiting moderate proteinuria (0.15 to 0.49 g/day) had a higher risk of all-cause mortality but not ESKD than those without proteinuria [21]. These inconsistent results may reflect racial differences in the effects of moderately increased albuminuria/proteinuria on kidney function decline and mortality.
The present study has several limitations. First, our participants were an ethnically homogeneous population from a single urban university hospital in Japan, limiting the generalisability of the current findings. Second, we did not have information on histological examinations in people with CKD; therefore, the present cohort may include people with non-diabetic nephropathy, such as glomerular nephritis, although we excluded two individuals with biopsy-proven diagnosis of non-diabetic nephropathy at baseline. Third, the categorisation of albuminuria at baseline may have been improper in some individuals owing to the single measurement of UACR, although we restricted the timing of urine collection to the first in the morning to minimise the misclassification [38]. Fourth, the category progression of albuminuria might have been underestimated owing to the study design. Finally, the present study did not evaluate time-dependent changes in laboratory data, blood pressure, BMI and medications during the follow-up period or the occurrence of pregnancy, malignancy and cardiovascular disease after baseline, which might influence the endpoints.
In conclusion, the present retrospective cohort study of Japanese adults with type 2 diabetes provides evidence that those exhibiting non-albuminuric kidney insufficiency have poorer kidney outcomes and life prognosis than those without CKD. Attention to occasional decline in kidney function unaccompanied by albuminuria may be necessary in people with this unique phenotype of kidney disease. Multicentre prospective cohort studies with larger sample sizes are warranted to confirm these findings.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARBs:
-
Angiotensin receptor blockers
- CKD:
-
Chronic kidney disease
- ESKD:
-
End-stage kidney disease
- JDS:
-
Japan Diabetes Society
- KRT:
-
Kidney replacement therapy
- PS:
-
Propensity score
- UACR:
-
Urinary albumin/creatinine ratio
References
Lane PH, Steffes MW, Mauer SM (1992) Glomerular structure in IDDM women with low glomerular filtration rate and normal urinary albumin excretion. Diabetes 41:581–586
Tsalamandris C, Allen TJ, Gilbert RE et al (1994) Progressive decline in renal function in diabetic patients with and without albuminuria. Diabetes 43:649–655
Kramer HJ, Nguyen QD, Curhan G, Hsu CY (2003) Renal insufficiency in the absence of albuminuria and retinopathy among adults with type 2 diabetes mellitus. JAMA 289:3273–3277
MacIsaac RJ, Tsalamandris C, Panagiotopoulos S, Smith TJ, McNeil KJ, Jerums G (2004) Nonalbuminuric renal insufficiency in type 2 diabetes. Diabetes Care 27:195–200
So WY, Kong AP, Ma RC et al (2006) Glomerular filtration rate, cardiorenal end points, and all-cause mortality in type 2 diabetic patients. Diabetes Care 29:2046–2052
de Boer IH, Rue TC, Hall YN, Heagerty PJ, Weiss NS, Himmelfarb J (2011) Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA 305:2532–2539
Afkarian M, Zelnick LR, Hall YN et al (2016) Clinical manifestations of kidney disease among US adults with diabetes, 1988–2014. JAMA 316:602–610
Kume S, Araki SI, Ugi S et al (2019) Secular changes in clinical manifestations of kidney disease among Japanese adults with type 2 diabetes from 1996 to 2014. J Diabetes Investig 10:1032–1040
Tanaka N, Yamamoto Y, Yokoyama Y, Mori T, Hanai K, Babazono T (2019) Temporal trends in the prevalence of albuminuria and reduced eGFR in Japanese patients with type 2 diabetes. Diabetol Int 10:279–287
Yokoyama H, Araki SI, Kawai K et al (2018) Declining trends of diabetic nephropathy, retinopathy and neuropathy with improving diabetes care indicators in Japanese patients with type 2 and type 1 diabetes (JDDM 46). BMJ Open Diabetes Res Care 6:e000521
Pugliese G, Penno G, Natali A et al (2019) Italian Diabetes Society and the Italian Society of Nephrology. Diabetic kidney disease: New clinical and therapeutic issues. Joint position statement of the Italian Diabetes Society and the Italian Society of Nephrology on “The natural history of diabetic kidney disease and treatment of hyperglycemia in patients with type 2 diabetes and impaired renal function.” Nutr Metab Cardiovasc Dis 29:1127–1150
Retnakaran R, Cull CA, Thorne KI, Adler AI, Holman RR, UKPDS Study Group (2006) Risk factors for renal dysfunction in type 2 diabetes: U.K. Prospective Diabetes Study 74. Diabetes 55:1832–1839
Costacou T, Ellis D, Fried L, Orchard TJ (2007) Sequence of progression of albuminuria and decreased GFR in persons with type 1 diabetes: a cohort study. Am J Kidney Dis 50:721–732
Perkins BA, Ficociello LH, Ostrander BE et al (2007) Microalbuminuria and the risk for early progressive renal function decline in type 1 diabetes. J Am Soc Nephrol 18:1353–1361
Molitch ME, Steffes M, Sun W, Epidemiology of Diabetes Interventions and Complications Study Group et al (2010) Development and progression of renal insufficiency with and without albuminuria in adults with type 1 diabetes in the Diabetes Control and Complications Trial and the Epidemiology of Diabetes Interventions and Complications study. Diabetes Care 33:1536–1543
Koye DN, Magliano DJ, Reid CM et al (2018) Risk of progression of nonalbuminuric CKD to end-stage kidney disease in people with diabetes: The CRIC (Chronic Renal Insufficiency Cohort) study. Am J Kidney Dis 72:653–661
Vistisen D, Andersen GS, Hulman A, Persson F, Rossing P, Jørgensen ME (2019) Progressive decline in estimated glomerular filtration rate in patients with diabetes after moderate loss in kidney function—even without albuminuria. Diabetes Care 42:1886–1894
Buyadaa O, Magliano DJ, Salim A, Koye DN, Shaw JE (2020) Risk of rapid kidney function decline, all-cause mortality, and major cardiovascular events in nonalbuminuric chronic kidney disease in type 2 diabetes. Diabetes Care 43:122–129
Yokoyama H, Araki SI, Kawai K, JDDM Study Group et al (2020) The Prognosis of Patients With Type 2 Diabetes and Nonalbuminuric Diabetic Kidney Disease Is Not Always Poor: Implication of the Effects of Coexisting Macrovascular Complications (JDDM 54). Diabetes Care 43:1102–1110
Penno G, Solini A, Orsi E, Renal Insufficiency And Cardiovascular Events (RIACE) Study Group et al (2018) Non-albuminuric renal impairment is a strong predictor of mortality in individuals with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicentre study. Diabetologia 61:2277–2289
Minutolo R, Gabbai FB, Provenzano M et al (2018) Cardiorenal prognosis by residual proteinuria level in diabetic chronic kidney disease: pooled analysis of four cohort studies. Nephrol Dial Transplant 33:1942–1949
Hallan SI, Ritz E, Lydersen S, Romundstad S, Kvenild K, Orth SR (2009) Combining GFR and albuminuria to classify CKD improves prediction of ESRD. J Am Soc Nephrol 20:1069–1077
Levey AS, de Jong PE, Coresh J et al (2011) The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int 80:17–28
Kashiwagi A, Kasuga M, Araki E, Committee on the Standardization of Diabetes Mellitus-Related Laboratory Testing of Japan Diabetes Society et al (2012) International clinical harmonization of glycated hemoglobin in Japan: From Japan Diabetes Society to National Glycohemoglobin Standardization Program values. J Diabetes Investig 3:39–40
Matsuo S, Imai E, Horio M, Collaborators developing the Japanese equation for estimated GFR et al (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992
Inker LA, Astor BC, Fox CH et al (2014) KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis 63:713–735
Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO (2020) Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney Int 2020(98):S1–S115
Grams ME, Sang Y, Ballew SH et al (2019) Evaluating glomerular filtration rate slope as a surrogate end point for ESKD in clinical trials: An individual participant meta-analysis of observational data. J Am Soc Nephrol 30:1746–1755
SAS Institute Inc. 2018. SAS/STAT 15.1 User's Guide. The PHREG Procedure. Example 89.8 survival curves. Available from http://documentation.sas.com/?docsetId=statug&docsetTarget=statug_phreg_examples08.htm&docsetVersion=15.1&locale=ja. Accessed 31 Aug 2020
Jiang S, Wang Y, Zhang Z, Dai P, Yang Y, Li W (2018) Accuracy of hematuria for predicting non-diabetic renal disease in patients with diabetes and kidney disease: A systematic review and meta-analysis. Diabetes Res Clin Pract 143:288–300
Lash JP, Go AS, Appel LJ, Chronic Renal Insufficiency Cohort (CRIC) Study Group et al (2009) Chronic Renal Insufficiency Cohort (CRIC) Study: baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol 4:1302–1311
Sone H, Tanaka S, Tanaka S, Japan Diabetes Complications Study Group et al (2013) Leisure-time physical activity is a significant predictor of stroke and total mortality in Japanese patients with type 2 diabetes: analysis from the Japan Diabetes Complications Study (JDCS). Diabetologia 56:1021–1030
Hayashino Y, Okamura S, Tsujii S, Ishii H, Diabetes Distress and Care Registry at Tenri Study Group (2020) The joint association of diabetes distress and depressive symptoms with all-cause mortality in Japanese individuals with type 2 diabetes: a prospective cohort study (Diabetes Distress and Care Registry in Tenri [DDCRT 20]). Diabetologia 63:2595–2604
Ekinci EI, Barr ELM, Barzi F et al (2019) Is hyperfiltration associated with higher urine albumin-to-creatinine ratio at follow up among Indigenous Australians? The eGFR follow-up study. J Diabetes Complications 33:343–349
Berhane AM, Weil EJ, Knowler WC, Nelson RG, Hanson RL (2011) Albuminuria and estimated glomerular filtration rate as predictors of diabetic end-stage renal disease and death. Clin J Am Soc Nephrol 6:2444–2451
Yamanouchi M, Furuichi K, Hoshino J, Research Group of Diabetic Nephropathy, the Ministry of Health, Labour and Welfare, and the Japan Agency for Medical Research and Development et al (2019) Nonproteinuric Versus Proteinuric Phenotypes in Diabetic Kidney Disease: A Propensity Score-Matched Analysis of a Nationwide Biopsy-Based Cohort Study. Diabetes Care 42:891–902
Yamanouchi M, Furuichi K, Hoshino J, Ubara Y, Wada T (2020) Nonproteinuric diabetic kidney disease. Clin Exp Nephrol 24:573–581
Babazono T, Takahashi C, Iwamoto Y (2004) Definition of microalbuminuria in first-morning and random spot urine in diabetic patients. Diabetes Care 27:1838–1839
Acknowledgements
We are grateful to E. Tauchi, S. Yamashita and I. Nyumura (Diabetes Center, Tokyo Women’s Medical University School of Medicine) for their assistance in data collection.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
Y. Yamamoto, KH and TB contributed to the conception and design of the study. Y. Yamamoto, KH, TM, Y. Yokoyama, NY and HM contributed to the data collection and preparation. KH and TS contributed to the analysis and interpretation of data. Y. Yamamoto and KH were responsible for drafting the manuscript. KH, TM, Y. Yokoyama, NY, HM, TS and TB revised the manuscript. All authors have approved the final version of the manuscript. TB is the guarantor of this work, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yamamoto, Y., Hanai, K., Mori, T. et al. Kidney outcomes and all-cause mortality in people with type 2 diabetes exhibiting non-albuminuric kidney insufficiency. Diabetologia 65, 234–245 (2022). https://doi.org/10.1007/s00125-021-05590-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-021-05590-5