Abstract
Peripartum cardiomyopathy (PPCM) is a rare but potentially life-threatening form of heart failure (HF). Bromocriptine, a dopamine D2 agonist, has been used as an adjunctive treatment for PPCM with controversial benefits. A comprehensive literature search was conducted through June 2021. We included studies comparing the outcomes of PPCM with or without bromocriptine use. Pooled risk ratio (RR) with 95% confidence intervals (CI) and I2 statistics were calculated. Composite major adverse outcomes were defined by a composite of death, need for advanced HF therapies, persistent New York Heart Association (NYHA) functional class III/V, or left ventricular ejection fraction (LVEF) ≤ 35% at 6-month follow-up. LVEF recovery was defined by improvement of LVEF to more than 50%. Eight studies (two randomized-controlled, six observational) involving 593 PPCM patients were included. Bromocriptine use was associated with significantly higher survival (91.6% vs. 83.9%, RR 1.11 p = 0.02). Baseline LVEF was not significantly different between the groups. LVEF at follow-up was significantly higher in the bromocriptine group (53.3% vs. 41.8%, p < 0.001). There was no significant association between bromocriptine use and lower composite major adverse outcomes (13.7% vs. 33.3%, RR 0.60 p = 0.54) or LVEF recovery (46.9% vs. 46.8%, RR 0.94 p = 0.74). In conclusion, the addition of bromocriptine to standard HF treatment in PPCM was associated with significantly higher survival and higher LVEF improvement. No association with lower composite adverse clinical outcomes or LVEF recovery was seen. The findings, although encouraging, warrant larger randomized-controlled studies.





Similar content being viewed by others
Availability of data, material, and code
Data sharing is not applicable to this article as no new data were created.
Abbreviations
- CI:
-
Confidence interval
- DCM:
-
Dilated cardiomyopathy
- ESC:
-
European Society of Cardiology
- HF:
-
Heart failure
- NYHA:
-
New York Heart Association
- LVEF:
-
Left ventricular ejection fraction
- PPCM:
-
Peripartum cardiomyopathy
- RCT:
-
Randomized-controlled trial
- RR:
-
Risk ratio
References
Pearson GD, Veille JC, Rahimtoola S, Hsia J, Oakley CM, Hosenpud JD et al (2000) Peripartum cardiomyopathy: National Heart, Lung, and Blood Institute and Office of Rare Diseases (National Institutes of Health) workshop recommendations and review. JAMA 283:1183–1188
Sliwa K, Hilfiker-Kleiner D, Petrie MC, Mebazaa A, Pieske B, Buchmann E et al (2010) Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on peripartum cardiomyopathy. Eur J Heart Fail 12:767–778
Bauersachs J, Konig T, van der Meer P, Petrie MC, Hilfiker-Kleiner D, Mbakwem A et al (2019) Pathophysiology, diagnosis and management of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy. Eur J Heart Fail 21:827–843
Demakis JG, Rahimtoola SH, Sutton GC, Meadows WR, Szanto PB, Tobin JR et al (1971) Natural course of peripartum cardiomyopathy. Circulation 44:1053–1061
Moulig V, Pfeffer TJ, Ricke-Hoch M, Schlothauer S, Koenig T, Schwab J et al (2019) Long-term follow-up in peripartum cardiomyopathy patients with contemporary treatment: low mortality, high cardiac recovery, but significant cardiovascular co-morbidities. Eur J Heart Fail 21:1534–1542
Elkayam U, Akhter MW, Singh H, Khan S, Bitar F, Hameed A et al (2005) Pregnancy-associated cardiomyopathy: clinical characteristics and a comparison between early and late presentation. Circulation 111:2050–2055
Francis GS, Parks R, Cohn JN (1983) The effects of bromocriptine in patients with congestive heart failure. Am Heart J 106:100–106
Sliwa K, Mebazaa A, Hilfiker-Kleiner D, Petrie MC, Maggioni AP, Laroche C et al (2017) Clinical characteristics of patients from the worldwide registry on peripartum cardiomyopathy (PPCM): EURObservational Research Programme in conjunction with the Heart Failure Association of the European Society of Cardiology Study Group on PPCM. Eur J Heart Fail 19:1131–1141
McNamara DM, Elkayam U, Alharethi R, Damp J, Hsich E, Ewald G et al (2015) Clinical outcomes for peripartum cardiomyopathy in North America: results of the IPAC Study (Investigations of Pregnancy-Associated Cardiomyopathy). J Am Coll Cardiol 66:905–914
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605
Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses Bmj 327:557–560
Sterne JA, Egger M (2001) Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 54:1046–1055
Sliwa K, Blauwet L, Tibazarwa K, Libhaber E, Smedema JP, Becker A et al (2010) Evaluation of bromocriptine in the treatment of acute severe peripartum cardiomyopathy: a proof-of-concept pilot study. Circulation 121:1465–1473
Croix G, Ibrahim M, Chaparro S (2018) Use of bromocriptine in the management of peripartum cardiomyopathy: a systematic review and meta-analysis. Cardiovasc Investig 2:4
Morales A, Painter T, Li R, Siegfried JD, Li D, Norton N et al (2010) Rare variant mutations in pregnancy-associated or peripartum cardiomyopathy. Circulation 121:2176–2182
Honigberg MC, Cantonwine DE, Thomas AM, Lim KH, Parry SI, McElrath TF (2016) Analysis of changes in maternal circulating angiogenic factors throughout pregnancy for the prediction of preeclampsia. J Perinatol 36:172–177
Liu J, Wang Y, Chen M, Zhao W, Wang X, Wang H et al (2014) The correlation between peripartum cardiomyopathy and autoantibodies against cardiovascular receptors. PLoS One 9:e86770
Honigberg MC, Givertz MM (2019) Peripartum cardiomyopathy. BMJ 364:k5287
Sarojini A, Sai Ravi Shanker A, Anitha M (2013) Inflammatory markers-serum level of C-reactive protein, tumor necrotic factor-alpha, and interleukin-6 as predictors of outcome for peripartum cardiomyopathy. J Obstet Gynaecol India 63:234–9
Roberg K, Ollinger K (1998) Oxidative stress causes relocation of the lysosomal enzyme cathepsin D with ensuing apoptosis in neonatal rat cardiomyocytes. Am J Pathol 152:1151–1156
Hilfiker-Kleiner D, Kaminski K, Podewski E, Bonda T, Schaefer A, Sliwa K et al (2007) A cathepsin D-cleaved 16 kDa form of prolactin mediates postpartum cardiomyopathy. Cell 128:589–600
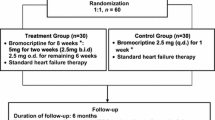
Hilfiker-Kleiner D, Haghikia A, Berliner D, Vogel-Claussen J, Schwab J, Franke A et al (2017) Bromocriptine for the treatment of peripartum cardiomyopathy: a multicentre randomized study. Eur Heart J 38:2671–2679
Hopp L, Weisse AB, Iffy L (1996) Acute myocardial infarction in a healthy mother using bromocriptine for milk suppression. Can J Cardiol 12:415–418
Bernard N, Jantzem H, Becker M, Pecriaux C, Benard-Laribiere A, Montastruc JL et al (2015) Severe adverse effects of bromocriptine in lactation inhibition: a pharmacovigilance survey. BJOG 122:1244–1251
Kolte D, Khera S, Aronow WS, Palaniswamy C, Mujib M, Ahn C et al (2014) Temporal trends in incidence and outcomes of peripartum cardiomyopathy in the United States: a nationwide population-based study. J Am Heart Assoc 3:e001056
Haghikia A, Podewski E, Berliner D, Sonnenschein K, Fischer D, Angermann CE et al (2015) Rationale and design of a randomized, controlled multicentre clinical trial to evaluate the effect of bromocriptine on left ventricular function in women with peripartum cardiomyopathy. Clin Res Cardiol 104:911–917
Goland S, Modi K, Hatamizadeh P, Elkayam U (2013) Differences in clinical profile of African-American women with peripartum cardiomyopathy in the United States. J Card Fail 19:214–218
Azibani F, Pfeffer TJ, Ricke-Hoch M, Dowling W, Pietzsch S, Briton O et al (2020) Outcome in German and South African peripartum cardiomyopathy cohorts associates with medical therapy and fibrosis markers. ESC Heart Fail
Biteker M, Ozlek B, Ozlek E, Cil C, Celik O, Dogan V et al (2020) Predictors of early and delayed recovery in peripartum cardiomyopathy: a prospective study of 52 patients. J Matern Fetal Neonatal Med 33:390–397
Haghikia A, Podewski E, Libhaber E, Roentgen P, Tsikas D, Bauersachs J et al (2013) Phenotyping and outcome on contemporary management of patients with peripartum cardiomyopathy: a German prospective study. Eur J Heart Fail 12:S2
Hoevelmann J, Viljoen CA, Manning K, Baard J, Hahnle L, Ntsekhe M et al (2019) The prognostic significance of the 12-lead ECG in peripartum cardiomyopathy. Int J Cardiol 276:177–184
Mahowald MK, Basu N, Subramaniam L, Scott R, Davis MB (2019) Long-term outcomes in peripartum cardiomyopathy. Open Cardiovasc Med J 13:13–23
Tremblay-Gravel M, Marquis-Gravel G, Avram R, Desplantie O, Ducharme A, Bibas L et al (2019) The effect of bromocriptine on left ventricular functional recovery in peripartum cardiomyopathy: insights from the BRO-HF retrospective cohort study. ESC Heart Fail 6:27–36
Yaméogo N, Kagambèga L, Seghda A (2017) Bromocriptine in management of peripartum cardiomyopathy: a randomized study on 96 women in Burkina Faso. J Cardiol Clin Res 5:1098–1106
Acknowledgements
None
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors have approved this present manuscript for submission. AT: data acquisition and manuscript preparation VK: conception and design, data acquisition, and manuscript preparation SM: data acquisition and manuscript preparation MI: analysis and interpretation of the data. GRSC: analysis and interpretation of the data GAH: validation and manuscript editing. SC: supervision and manuscript editing.
Corresponding author
Ethics declarations
Ethics approval
This is a systematic review and meta-analysis. No ethical approval is required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Disclosure
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Trongtorsak, A., Kittipibul, V., Mahabir, S. et al. Effects of bromocriptine in peripartum cardiomyopathy: a systematic review and meta-analysis. Heart Fail Rev 27, 533–543 (2022). https://doi.org/10.1007/s10741-021-10185-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-021-10185-8