Abstract
Background
Children with nephrotic syndrome (NS) are vulnerable to infections. Measles infection is an important cause of morbidity and mortality in immunosuppressed children. A suboptimal seroprotection against measles has been shown in immunocompromised children. There is limited published literature on measles immunity in children with difficult-to-treat nephrotic syndrome (DTNS). We compared the proportions of children with DTNS and healthy controls who were seroprotected against measles.
Methods
This was a cross-sectional study. Measles-specific IgG antibodies of 108 children with DTNS (3 to 10 years of age) and an equal number of age-matched healthy controls were measured. All children had received two doses of measles-containing vaccine at 9–12 and 16–24 months of age under routine immunisation programme. Serum measles IgG antibody titres were measured by indirect ELISA. The assay results were interpreted as (1) > 11 NTU (NovaTec Units), positive/seroprotective titres; (2) 9–11, equivocal; and (3) < 9 NTU, negative. Inter- and intra-group comparisons were made to identify the disease characteristics related to seroprotection status.
Results
The proportion of children with protective anti-measles antibodies (n = 70, 65%) was significantly lower in DTNS as compared to controls (n = 88, 81.48%) (p = 0.005). Their median [IQR] antibody titres were also significantly lower than those in controls (14.1 [14] NTU vs. 18.3 [15.2] NTU (p = 0.001). The age, gender, clinical subtype, duration of disease, and type of immunosuppressive therapy were not significantly different between seroprotected and non-seroprotected children with DTNS.
Conclusion
A significantly lower percentage of fully vaccinated children with DTNS were seroprotected against measles compared to healthy controls.
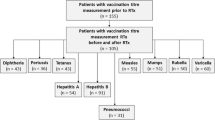
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information.


Similar content being viewed by others
Data availability
Data will be made available upon request.
Code availability
Not applicable.
Change history
12 December 2021
ESM was extended to include the article's Graphical abstract.
References
Mishra OP, Abhinay A, Mishra RN, Prasad R, Pohl M (2013) Can we predict relapses in children with idiopathic steroid-sensitive nephrotic syndrome? J Trop Pediatr 59:343–349
Alwadhi RK, Mathew JL, Rath B (2004) Clinical profile of children with nephrotic syndrome not on glucorticoid therapy, but presenting with infection. J Paediatr Child Health 40:28–32
Alfakeekh K, Azar M, Sowailmi BA, Alsulaiman S, Makdob SA, Omair A et al (2019) Immunosuppressive burden and risk factors of infection in primary childhood nephrotic syndrome. J Infect Public Health 12:90–94
Gulati S, Kher V, Gupta A, Arora P, Rai PK, Sharma RK (1995) Spectrum of infections in Indian children with nephrotic syndrome. Pediatr Nephrol 9:431–434
Patel MK, Goodson JL, Alexander JP Jr et al (2020) Progress toward regional measles elimination – Worldwide, 2000–2019. MMWR Morb Mortal Wkly Rep 69:1700–1705
World Health Organization (2021) Immunization analysis and insights. https://www.who.int/teams/immunization-vaccines-and-biologicals/immunization-analysis-and-insights/surveillance/monitoring/provisional-monthly-measles-and-rubella-data. Accessed 24 April 2021
Pullan CR, Noble TC, Scott DJ, Wisniewsk K, Gardner PS (1976) Atypical measles infections in leukaemic children on immunosuppressive treatment. Br Med J 1:1562–1565
Meadow SR, Weller RO, Archibald RW (1969) Fatal systemic measles in a child receiving cyclophosphamide for nephrotic syndrome. Lancet 294:876–878
Breitfeld V, Hashida Y, Sherman FE, Odagiri K, Yunis EJ (1973) Fatal measles infection in children with leukemia. Lab Invest 28:279–291
Kaplan LJ, Daum RS, Smaron M, McCarthy CA (1992) Severe measles in immunocompromised patients. JAMA 267:1237–1241
Schenk J, Abrams S, Theeten H, Van Damme P, Beutels P, Hens N (2021) Immunogenicity and persistence of trivalent measles, mumps, and rubella vaccines: a systematic review and meta-analysis. Lancet Infect Dis 21:286–295
Fouda AE, Kandil SM, Boujettif F, Salama YS, Fayea NY (2018) Humoral immune response of childhood acute lymphoblastic leukemia survivors against the measles, mumps, and rubella vaccination. Hematology 23:590–595
Rocca S, Santilli V, Cotugno N, Concato C, Manno EC, Nocentini G et al (2016) Waning of vaccine-induced immunity to measles in kidney transplanted children. Medicine (Baltimore) 95:e4738
Kerneis S, Launay O, Turbelin C, Batteux F, Hanslik T, Boelle PY (2014) Long-term immune responses to vaccination in HIV-infected patients: a systematic review and meta-analysis. Clin Infect Dis 58:1130–1139
Mutsaerts EAML, Nunes MC, van Rijswijk MN, Klipstein-Grobusch K, Otwombe K, Cotton MF et al (2019) Measles immunity at 4.5 years of age following vaccination at 9 and 15–18 months of age among human immunodeficiency virus (HIV)-infected, HIV-exposed-uninfected, and HIV-unexposed children. Clin Infect Dis 69:687–696
Indian Pediatric Nephrology Group, Indian Academy of Pediatrics, Bagga A, Ali U, Banerjee S, Kanitkar M, Phadke KD, Senguttuvan P et al (2008) Management of steroid sensitive nephrotic syndrome: revised guidelines. Indian Pediatr 45:203–214
National Health Portal – India (2019) Universal Immunisation Programme. https://www.nhp.gov.in/universal-immunisation-programme_pg. Accessed 24 April 2021
Han JW, Lee KY, Hwang JY, Koh DK, Lee JS (2010) Antibody status in children with steroid-sensitive nephrotic syndrome. Yonsei Med J 51:239–243
Ajay M, Mantan M, Dabas A, Asraf A, Yadav S, Chakravarti A (2021) Seroprotection for diphtheria, pertussis, tetanus and measles in children with nephrotic syndrome. Indian Pediatr 58:233–236
Deen WM, Bridges CR, Brenner BM, Myers BD (1985) Heteroporous model of glomerular size selectivity: application to normal and nephrotic humans. Am J Physiol 249:F374-389
Kaysen GA, al Bander H (1990) Metabolism of albumin and immunoglobulins in the nephrotic syndrome. Am J Nephrol 10:36–42
Kemper MJ, Altrogge H, Ganschow R, Müller-Wiefel DE (2002) Serum levels of immunoglobulins and IgG subclasses in steroid sensitive nephrotic syndrome. Pediatr Nephrol 17:413–417
Baris HE, Baris S, Karakoc-Aydiner E, Gokce I, Yildiz N, Cicekkoku D et al (2016) The effect of systemic corticosteroids on the innate and adaptive immune system in children with steroid responsive nephrotic syndrome. Eur J Pediatr 175:685–693
Kemper MJ, Zepf K, Klaassen I, Link A, Muller-Wiefel DE (2005) Changes of lymphocyte populations in pediatric steroid-sensitive nephrotic syndrome are more pronounced in remission than in relapse. Am J Nephrol 25:132–137
Ulinski T, Leroy S, Dubrel M, Danon S, Bensman A (2008) High serological response to pneumococcal vaccine in nephrotic children at disease onset on high-dose prednisone. Pediatr Nephrol 23:1107–1113
Poyrazoğlu HM, Düşünsel R, Gündüz Z, Patiroğlu T, Köklü S (2004) Antibody response to influenza A vaccination in children with nephrotic syndrome. Pediatr Nephrol 19:57–60
Furth SL, Arbus GS, Hogg R, Tarver J, Chan C, Fivush BA, Southwest Pediatric Nephrology Study Group (2003) Varicella vaccination in children with nephrotic syndrome: a report of the southwest pediatric nephrology study group. J Pediatr 142:145–148
Marks JS, Halpin TJ, Orenstein WA (1978) Measles vaccine efficacy in children previously vaccinated at 12 months of age. Pediatrics 62:955–960
Job JS, John TJ, Joseph A (1984) Antibody response to measles immunization in India. Bull World Health Organ 62:737–741
Gupta M, Tripathy JP, Verma M, Singh MP, Kaur R, Ratho RK et al (2019) Seroprevalence of measles, mumps & rubella antibodies among 5–10 years old children in north India. Indian J Med Res 149:396–403
Hansashree P, Verma S, Rawat A, Sankhyan N, Bharti B (2018) Long-term seroprotection rates following second dose of measles as MMR vaccine at 15 months in Indian children. Indian Pediatr 55:405–407
Kroger A, Bahta L, Hunter P (2020) General best practice guidelines for immunization. Best practices guidance of the advisory committee on immunization practices (ACIP). https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/downloads/general-recs.pdf
Papp KA, Haraoui B, Kumar D, Marshall JK, Bissonnette R, Bitton A et al (2019) Vaccination guidelines for patients with immune-mediated disorders taking immunosuppressive therapies: executive summary. J Rheumatol 46:751–754
Acknowledgements
The authors wish to thank the study participants and their parents, and the resident doctors, nurses and technicians from the Departments of Pediatrics and Microbiology.
Author information
Authors and Affiliations
Contributions
ST, VC, MJ, and JKS were involved in the study design and data acquisition. ST and VC were involved in data analysis and interpretation. ST, VC, MJ, and JKS drafted the manuscript, performed critical revisions, and gave final approval for submission.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Institutional Ethics Committee (LHMC/ECHR/2018/791), and conducted in accordance with Good Clinical Practice and the Declaration of Helsinki.
Consent to participate
Written informed consent was obtained from the parents or legal guardians of all children. When possible, consent from the patients themselves was also obtained.
Consent for publication
Study participants gave written informed consent for publication of the results of the study before their enrolment in the study.
Conflict of interest/Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sahoo, J.K., Tiwari, S., Chhapola, V. et al. Seroprotection against measles in previously vaccinated children with difficult-to-treat nephrotic syndrome. Pediatr Nephrol 37, 843–848 (2022). https://doi.org/10.1007/s00467-021-05290-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05290-7