Abstract
Background
It is anticipated that surgical treatment for gastro-esophageal reflux disease (GERD) in the elderly will increase. This time, using propensity score matching, we examined the results of laparoscopic fundoplication (LF) for GERD-related diseases in the elderly.
Methods
Of 302 cases which underwent initial LF for GERD-related diseases during the period from June 2008 to February 2019, we classified them into elderly (65 years of age or older) and non-elderly groups (64 years of age or younger). 57 cases each were extracted upon performing propensity score matching regarding five factors including: gender; body mass index; esophageal hiatal hernia; extent of reflux esophagitis; and the use of mesh.
Results
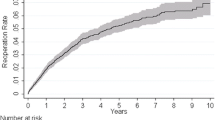
With regard to the preoperative disease status, the pH < 4 holding time was indicated as 2.8% (0.5–10.7%) in the elderly group and 3.4% (0.6–8.0%) in the non-elderly group, with no difference in terms of the illness period as well (p = 0.889 and p = 0.263, respectively). Although there was no difference in terms of the operative time (155 vs. 139 min, p = 0.092) and estimated blood loss (both ≒ 0 ml, p = 0.298), postoperative hospital stay was prolonged in the elderly group [7 (7–9) vs. 7 (7–7), p = 0.007]. On the other hand, esophageal hiatal hernia, reflux esophagitis, and acid reflux time in the esophagus were all improved following surgery in both groups (p < 0.001 in both groups).
Conclusion
The treatment results of LF for GERD-related diseases in the elderly were as good as those in the non-elderly, indicating possible safe implementation.

Similar content being viewed by others
References
Iwakiri K, Kinoshita Y, Habu Y, Oshima T, Manabe N, Fujiwara Y, et al. Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2015. J Gastroenterol. 2016;51(8):751–67.
Håkanson BS, Lundell L, Bylund A, Thorell A. Comparison of laparoscopic 270° posterior partial fundoplication vs total fundoplication for the treatment of gastroesophageal reflux disease: a randomized clinical trial. JAMA Surg. 2019;154(6):479–86.
Beck PE, Watson DI, Devitt PG, Game PA, Jamieson GG. Impact of gender and age on the long-term outcome of laparoscopic fundoplication. World J Surg. 2009;33(12):2620–6.
Bammer T, Hinder RA, Klaus A, Libbey JS, Napoliello DA, Rodriquez JA. Safety and long-term outcome of laparoscopic antireflux surgery in patients in their eighties and older. Surg Endosc. 2002;16(1):40–2.
Tedesco P, Lobo E, Fisichella PM, Way LW, Patti MG. Laparoscopic fundoplication in elderly patients with gastroesophageal reflux disease. Arch Surg. 2006;141(3):289–92 (discussion 292).
Fei L, Rossetti G, Moccia F, Marra T, Guadagno P, Docimo L, et al. Is the advanced age a contraindication to GERD laparoscopic surgery? Results of a long term follow-up. BMC Surg. 2013;13(Suppl 2):S13.
Grotenhuis BA, Wijnhoven BP, Bessell JR, Watson DI. Laparoscopic antireflux surgery in the elderly. Surg Endosc. 2008;22(8):1807–12.
Khajanchee YS, Urbach DR, Butler N, Hansen PD, Swanstrom LL. Laparoscopic antireflux surgery in the elderly. Surg Endosc. 2002;16(1):25–30.
Tolone S, Docimo G, Del Genio G, Brusciano L, Verde I, Gili S, et al. Long term quality of life after laparoscopic antireflux surgery for the elderly. BMC Surg. 2013;13(Suppl 2):S10.
Oelschlager BK, Quiroga E, Parra JD, Cahill M, Polissar N, Pellegrini CA. Long-term outcomes after laparoscopic antireflux surgery. Am J Gastroenterol. 2008;103(2):280–7 (quiz 288).
Tutuian R, Vela MF, Shay SS, Castell DO. Multichannel intraluminal impedance in esophageal function testing and gastroesophageal reflux monitoring. J Clin Gastroenterol. 2003;37(3):206–15 (Review).
Feussner H, Petri A, Walker S, Bollschweiler E, Siewert JR. The modified AFP score: an attempt to make the results of anti-reflux surgery comparable. Br J Surg. 1991;78(8):942–6.
Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45(2):172–80.
Yano F, Tsuboi K, Omura N, Hoshino M, Yamamoto SR, Akimoto S, et al. Treatment strategy for laparoscopic hiatal hernia repair. Asian J Endosc Surg. 2021. https://doi.org/10.1111/ases.12918 (Epub ahead of print. PMID: 33472278).
Hoshino M, Omura N, Yano F, Tsuboi K, Yamamoto SR, Akimoto S, et al. Comparison of laparoscopic Nissen and Toupet fundoplication using a propensity score matching analysis. Surg Today. 2017;47(10):1195–200.
Omura N, Kashiwagi H, Yano F, Tsuboi K, Yanaga K. Postoperative recurrence factors of GERD in the elderly after laparoscopic fundoplication. Esophagus. 2010;7:31–5.
Omura N, Tsuboi K, Yano F. Minimally invasive surgery for large hiatal hernia. Ann Gastroenterol Surg. 2019;3(5):487–95.
Stefanidis D, Hope WW, Kohn GP, Reardon PR, Richardson WS, Fanelli RD, SAGES Guidelines Committee. Guidelines for surgical treatment of gastroesophageal reflux disease. Surg Endosc. 2010;24(11):2647–69.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Masato Hoshino, Nobuo Omura, Fumiaki Yano, Kazuto Tsuboi, Se Ryung Yamamoto, Shunsuke Akimoto, Takahiro Masuda, Yuki Sakashita, Naoko Fukushima and Hideyuki Kashiwagi have no conflicts of interest or financial ties to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and /or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hoshino, M., Omura, N., Yano, F. et al. Therapeutic effect of laparoscopic fundoplication for GERD-related disease in the elderly. Gen Thorac Cardiovasc Surg 70, 72–78 (2022). https://doi.org/10.1007/s11748-021-01713-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-021-01713-2