Abstract
Purpose
Programmed cell death-1 (PD-1)/programmed death-ligand 1 (PD-L1) inhibitors plus chemotherapy have become the standard first line of treatment in patients with advanced non-small-cell lung cancer (NSCLC). However, few studies have explicitly focused on the impact of weight loss on the efficacy of PD-1/PD-L1 inhibitors plus chemotherapy. Thus, we evaluated the clinical implications of weight loss on the survival outcomes in patients who received this treatment.
Methods
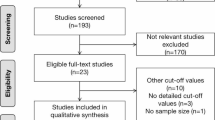
We conducted a retrospective review of medical records of patients with advanced NSCLC who were treated with PD-1/PD-L1 inhibitors plus chemotherapy from December 2018 to December 2020. Significant weight loss was defined as an unintentional weight loss of 5% or more over 6 months. We evaluated the progression-free survival (PFS) and overall survival (OS) of patients with or without weight loss.
Results
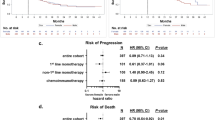
Among the 80 included patients, 37 (46%) had weight loss, and were associated with a lower objective response rate (30 vs 51%, P < 0.05), poorer PFS (2.3 vs 12.0 months, P < 0.05), and poorer OS (10.8 vs 23.9 months, P < 0.05) than those without weight loss. The Cox proportional-hazard ratios (95% confidence interval) of weight loss were 1.77 (1.01–3.10) for PFS and 2.90 (1.40–6.00) for OS, with adjustments for Eastern Cooperative Oncology Group performance status, PD-L1 tumour proportion score, histology, and central nervous system metastases.
Conclusion
Pre-treatment weight loss may reduce treatment efficacy and shorten survival time in patients receiving PD-1/PD-L1 inhibitors plus chemotherapy. Early evaluation and intervention for weight loss might improve oncological outcomes in patients with advanced NSCLC.



Similar content being viewed by others
Data availability
All data and material are available on reasonable request.
Code availability
Not applicable.
References
Mok TSK, Wu YL, Kudaba I et al (2019) Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet 393:1819–1830. https://doi.org/10.1016/S0140-6736(18)32409-7
Shaverdian N, Lisberg AE, Bornazyan K et al (2017) Previous radiotherapy and the clinical activity and toxicity of pembrolizumab in the treatment of non-small-cell lung cancer: a secondary analysis of the KEYNOTE-001 phase 1 trial. Lancet Oncol 18:895903. https://doi.org/10.1016/S1470-2045(17)30380-7
Reck M, Rodríguez-Abreu D, Robinson AG et al (2019) Updated analysis of KEYNOTE-024: Pembrolizumab versus Platinum-based chemotherapy for advanced non-small-cell lung cancer with PD-L1 tumour proportion score of 50% or greater. J Clin Oncol 37:537–546. https://doi.org/10.1200/JCO.18.00149
Rittmeyer A, Barlesi F, Waterkamp D et al (2017) Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet 389:255–265. https://doi.org/10.1016/S0140-6736(16)32517-X
Gandhi L, Rodríguez-Abreu D, Gadgeel S et al (2018) Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med 378:2078–2092. https://doi.org/10.1056/NEJMoa1801005
Paz-Ares L, Luft A, Vicente D et al (2018) Pembrolizumab plus chemotherapy for squamous non-small-cell lung cancer. N Engl J Med 379:2040–2051. https://doi.org/10.1056/NEJMoa1810865
Socinski MA, Jotte RM, Cappuzzo F et al (2018) Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med 378:2288–2301. https://doi.org/10.1056/NEJMoa1716948
Fearon K, Arends J, Baracos V (2013) Understanding the mechanisms and treatment options in cancer cachexia. Nat Rev Clin Oncol 10:90–99. https://doi.org/10.1038/nrclinonc.2012.209
Baracos VE, Martin L, Korc M et al (2018) Cancer-associated cachexia. Nat Rev Dis Primers 4:17105. https://doi.org/10.1038/nrdp.2017.105
Roch B, Coffy A, Jean-Baptiste S et al (2020) Cachexia – sarcopenia as a determinant of disease control rate and survival in non-small lung cancer patients receiving immune-checkpoint inhibitors. Lung Cancer 143:19–26. https://doi.org/10.1016/j.lungcan.2020.03.003
Nishioka N, Uchino J, Hirai S et al (2019) Association of sarcopenia with and efficacy of anti-PD-1/PD-L1 therapy in non-small-cell lung cancer. J Clin Med 8:450. https://doi.org/10.3390/jcm8040450
Miyawaki T, Naito T, Kodama A et al (2020) Desensitizing effect of cancer cachexia on immune checkpoint inhibitors in patients with advanced NSCLC. JTO Clin Res Rep 1:100020. https://doi.org/10.1016/j.jtocrr.2020.100020
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247. https://doi.org/10.1016/j.ejca.2008.10.026
Goldstraw P, Chansky K, Crowley J et al (2016) The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol 11:39–51. https://doi.org/10.1016/j.jtho.2015.09.009
Schwartz LH, Litière S, de Vries E et al (2016) RECIST 1.1-Update and clarification: from the RECIST committee. Eur J Cancer 62:132–137. https://doi.org/10.1016/j.ejca.2016.03.081
Langer CJ, Socinski MA, Patel JD et al (2016) Isolating the role of bevacizumab in elderly patients with previously untreated nonsquamous non–small cell lung cancer. Am J Clin Oncol 39:441–447. https://doi.org/10.1097/COC.0000000000000163
Kenmotsu H, Yamamoto N, Yamanaka T et al (2020) Randomized phase III study of Pemetrexed Plus Cisplatin Versus Vinorelbine Plus Cisplatin for completely resected stage II to IIIA nonsquamous non-small-cell lung cancer. J Clin Oncol 38:2187–2196. https://doi.org/10.1200/JCO.19.02674
Okamoto I, Nokihara H, Nomura S et al (2020) Comparison of Carboplatin plus Pemetrexed followed by Maintenance Pemetrexed with Docetaxel monotherapy in elderly patients with advanced nonsquamous non–small cell lung cancer: a phase 3 randomized clinical trial. JAMA Oncol 6:e196828. https://doi.org/10.1001/jamaoncol.2019.6828
Ross PJ, Ashley S, Norton A et al (2004) Do patients with weight loss have a worse outcome when undergoing chemotherapy for lung cancers? Br J Cancer 90:1905–1911. https://doi.org/10.1038/sj.bjc.6601781
Patel JD, Pereira JR, Chen J et al (2016) Relationship between efficacy outcomes and weight gain during treatment of advanced, non-squamous, non-small-cell lung cancer patients. Ann Oncol 27:1612–1619. https://doi.org/10.1093/annonc/mdw211
Naito T, Okayama T, Aoyama T et al (2017) Skeletal muscle depletion during chemotherapy has a large impact on physical function in elderly Japanese patients with advanced non-small-cell lung cancer. BMC Cancer 17:571. https://doi.org/10.1186/s12885-017-3562-4
Martin L, Baracos VE et al (2015) Diagnostic criteria for the classification of cancer-associated weight loss. J Clin Oncol 33:90–99. https://doi.org/10.1200/JCO.2014.56.1894
Morel H, Raynard B et al (2018) Prediagnosis weight loss, a stronger factor than BMI, to predict survival in patients with lung cancer. Lung Cancer 126:55–63. https://doi.org/10.1016/j.lungcan.2018.07.005
Jizu Z, Sean K, Deborah K et al (2018) Association of baseline body mass index (BMI) with overall survival (OS) in patients (pts) with metastatic non-small cell lung cancer (mNSCLC) treated with nivolumab (N) and pembrolizumab (P). J Clin Oncol 36:6553–6553. https://doi.org/10.1200/JCO.2018.36.15_suppl.6553
Kimura M, Naito T, Kenmotsu H et al (2015) Prognostic impact of cancer cachexia in patients with advanced non-small cell lung cancer. Support Care Cancer 23:1699–1708. https://doi.org/10.1007/s00520-014-2534-3
Fujio T, Nakashima K, Naito T et al (2019) Platinum combination chemotherapy is poorly tolerated in malnourished advanced lung cancer patients with poor performance status. Nutr Cancer 71:767–771. https://doi.org/10.1080/01635581.2018.1559941
Miyawaki E, Naito T, Nakashima K et al (2020) Management of anorexia prevents skeletal muscle wasting during cisplatin-based chemotherapy for thoracic malignancies. JCSM Clinical Reports 5:8–15. https://doi.org/10.1002/crt2.8
Doroshow DB, Bhalla S, Beasley MB et al (2021) PD-L1 as a biomarker of response to immune-checkpoint inhibitors. Nat Rev Clin Oncol 18:345–362. https://doi.org/10.1038/s41571-021-00473-5
Flint TR, Fearon DT, Janowitz T (2017) Connecting the metabolic and immune responses to cancer. Trends Mol Med 23:451–464. https://doi.org/10.1016/j.molmed.2017.03.001
Flint TR, Janowitz T, Connell CM et al (2016) Tumor-induced IL-6 reprograms host metabolism to suppress anti-tumour immunity. Cell Metab 24:672–684. https://doi.org/10.1016/j.cmet.2016.10.010
Kaplanov I, Carmi Y, Kornetsky R et al (2019) Blocking IL-1beta reverses the immunosuppression in mouse breast cancer and synergizes with anti-PD-1 for tumour abrogation. Proc Natl Acad Sci U. S A 116:1361–1369. https://doi.org/10.1073/pnas.1812266115
Bertrand F, Montfort A, Marcheteau E et al (2017) TNF alpha blockade overcomes resistance to anti-PD-1 in experimental melanoma. Nat Commun 8:2256. https://doi.org/10.1038/s41467-017-02358-7
Teng MW, Ngiow SF, Ribas A, Smyth MJ (2015) Classifying cancers based on T-cell infiltration and PD-L1. Cancer Res 75:2139–2145. https://doi.org/10.1158/0008-5472.CAN-15-0255
Nishie K, Yamamoto S, Nagata C et al (2017) Anamorelin for advanced non-small-cell lung cancer with cachexia: systematic review and meta-analysis. Lung Cancer 112:25–34. https://doi.org/10.1016/j.lungcan.2017.07.023
Temel JS, Abernethy AP, Currow DC et al (2016) Anamorelin in patients with non-small-cell lung cancer and cachexia (ROMANA 1 and ROMANA 2): results from two randomised, double-blind, phase 3 trials. Lancet Oncol 17:519–531. https://doi.org/10.1016/S1470-2045(15)00558-6
Author information
Authors and Affiliations
Contributions
TM and TN wrote the manuscript and researched data. TN reviewed and edited the manuscript. KM is a professional biostatistician and responsible for statistical analysis. All authors reviewed, approved the final version of the manuscript, and certified that they comply with the ethical guidelines for publishing in the Supportive care in Cancer.
Corresponding author
Ethics declarations
Ethics approval
The ethical review board of our institution approved the study (registration no. J2020-176–2020-1). All procedures performed in studies involving human participants were in accordance with 1964 Helsinki declaration and its later amendments or with comparable ethical standards.
Consent to participate
For this type of study, formal consent is not required. However, we also employed an opt-out method to obtain consent for this study by posting a document about this study. The document has been approved by the institutional ethics review board of Shizuoka Cancer Center.
Consent for publication
Not applicable.
Conflict of interest
Dr. Taichi Miyawaki — Declarations of interest: none.
Dr. Naito, Dr. Yabe, Dr. Kodama, Dr. Nishioka, Dr. Eriko Miyawaki, Dr. Mori — Declarations of interest: none.
Dr. Mamesaya reports personal fees from AstraZeneca KK, Pfizer Japan, Inc.; personal fees from Chugai Pharmaceutical Co., Ltd.; grants and personal fees from Boehringer Ingelheim; personal fees from MSD K.K.; personal fees from TAIHO PHARMACEUTICAL CO., LTD.; and personal fees from ONO PHARMACEUTICAL CO., LTD., outside the submitted work.
Dr. Kobayashi reports personal fees from Eli Lilly K.K, personal fees from Taiho Pharmaceutical, personal fees from AstraZeneca, outside the submitted work.
Dr. Omori reports personal fees from Chugai Pharmaceutical Co., Ltd., Ono Pharmaceutical, AstraZeneca K.K., Boehringer Ingelheim, Taiho Pharmaceutical, and MSD, which are unrelated to the submitted work.
Dr. Wakuda reports grants and personal fees from Chugai Pharmaceutical Co., Ltd.; personal fees from Taiho Pharmaceutical; personal fees from Boehringer Ingelheim; personal fees from Eli Lilly K.K.; personal fees from Ono Pharmaceutical, personal fees from MSD; grants from Novartis; grants from Abbvie; and grants and personal fees from AstraZeneca, outside the submitted work.
Dr. Ono reports grants from Taiho Pharmaceutical, grants from Ono Pharmaceutical, grants from Chugai Pharmaceutical Co., Ltd., and grants from Novartis Pharma K.K., outside the submitted work.
Dr. Kenmotsu reports grants and personal fees from Chugai Pharmaceutical Co, Ltd.; personal fees from Ono Pharmaceutical Co, Ltd.; personal fees from Boeringer Ingelheim; personal fees from Eli Lilly K.K; personal fees from Kyowa Hakko Kirin Co., Ltd.; personal fees from Bristol-Myers Squibb; personal fees from MSD; grants and personal fees from Novartis Pharma K.K.; grants and personal fees from Daiichi-Sankyo Co., Ltd.; grants and personal fees from AstraZeneca K.K.; personal fees from Pfizer; and personal fees from Taiho Pharma, outside the submitted work.
Dr. Murakami reports personal fees from AstraZeneca K.K., Ono Pharmaceutical, Bristol-Myers Squibb Japan, Chugai Pharmaceutical Co., Ltd., Pfizer Inc., Novartis Pharma K.K., Boehringer Ingelheim, Taiho Pharmaceutical, Eli Lilly K.K., and MSD, which are unrelated to the submitted work.
Dr. Harada reports personal fees from Daiichi Sankyo Pharmaceutical Co. during the conduct of the study as well as personal fees from Daiichi Sankyo Pharmaceutical Co., AstraZeneca K.K., Brain Labo Co., and Chugai Pharmaceutical Co. and grants from the Japan Agency for Medical Research and Development and the National Cancer Center Research and Development Fund, which are unrelated to the submitted work.
Dr. Kazuhisa Takahashi reports grants and personal fees from AstraZeneca K.K., Pfizer Japan, Inc., Eli Lilly K.K., MSD, and Boehringer Ingelheim as well as grants from Takeda Pharmaceutical Company Ltd., Chugai Pharmaceutical Co., Ltd., Taiho Pharmaceutical Co., Ltd., KYORIN Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., GlaxoSmithKline Consumer Healthcare Japan K.K., SHIONOGI & CO., LTD., and Novartis Pharma K.K., which are unrelated to the submitted work.
Dr. Toshiaki Takahashi reports grants and personal fees from AstraZeneca KK, Pfizer Japan, Inc.; grants and personal fees from Eli Lilly Japan K.K.; grants and personal fees from Chugai Pharmaceutical Co., Ltd.; grants and personal fees from Ono Pharmaceutical Co., Ltd.; grants and personal fees from MSD K.K.; grants and personal fees from Boehringer Ingelheim Japan, Inc.; grants and personal fees from Pfizer Japan, Inc.; and personal fees from Roche Diagnostics K.K., outside the submitted work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Miyawaki, T., Naito, T., Yabe, M. et al. Impact of weight loss on treatment with PD-1/PD-L1 inhibitors plus chemotherapy in advanced non-small-cell lung cancer. Support Care Cancer 30, 1633–1641 (2022). https://doi.org/10.1007/s00520-021-06572-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06572-4