Abstract
Purpose
A proportion of people with palliative care needs unknowingly have a genetic predisposition to their disease, placing relatives at increased risk. As end-of-life nears, the opportunity to address genetics for the benefit of their family narrows. Clinicians face numerous barriers addressing genetic issues, but there is limited evidence from the palliative care clinician perspective. Our aims are to (1) explore the views and experiences of palliative care clinicians in addressing genetics with patients and their families and (2) generate suggested strategies that support integration of genetics into palliative care.
Methods
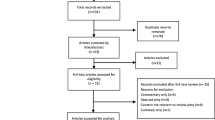
An interpretive descriptive qualitative study using semi-structured interviews with palliative care doctors and nurses (N = 14).
Results
Three themes were identified: (1) Harms and benefits of raising genetics: a delicate balancing act, (2) Navigating genetic responsibility within the scope of palliative care and (3) Overcoming practice barriers: a multipronged approach. Participants described balancing the benefits of addressing genetics in palliative care against potential harms. Responsibility to address genetic issues depends on perceptions of relevance and the scope of palliative care. Suggestions to overcome practice barriers included building genetic-palliative care relationships and multi-layered genetics education, developing clinical resources and increasing organisational support.
Conclusions
Integrating aspects of genetics is feasible, but must be balanced against potential harms and benefits. Palliative care clinicians were uncertain about their responsibility to navigate these complex issues to address genetics. There are opportunities to overcome barriers and tailor support to ensure people nearing end-of-life have a chance to address genetic issues for the benefit of their families.
Similar content being viewed by others
Data availability
S.W is the primary data custodian. All data related to this study are held securely on S.Ws password-protected OneDrive account associated with the University of Technology Sydney (UTS). At the conclusion of the study, all data were archived in the UTS eResearch Store. Data will remain here for a period of 5 years. After this time, the data will be destroyed with the assistance of a UTS data management librarian in line with the UTS ‘Guidelines for the Management of Research Data’ document.
Code availability
Not applicable to this study.
References
Lakhani NS et al (2013) Could triaging family history of cancer during palliative care enable earlier genetic counseling intervention? J Palliat Med 16(11):1350–1355. https://doi.org/10.1089/jpm.2012.0583
Kurian AW, Sigal BM, Plevritis SK (2010) Survival analysis of cancer risk reduction strategies for BRCA1/2 mutation carriers. J Clin Oncol 28(2):222–231. https://doi.org/10.1200/JCO.2009.22.7991
van Rij MC et al (2014) The uptake and outcome of prenatal and pre-implantation genetic diagnosis for Huntington’s disease in the Netherlands (1998–2008). Clin Genet 85(1):87–95. https://doi.org/10.1111/cge.12089
Forbes Shepherd R et al (2021) “I need to know if I’m going to die young”: Adolescent and young adult experiences of genetic testing for Li-Fraumeni syndrome. J Psychosoc Oncol 39(1):54–73. https://doi.org/10.1080/07347332.2020.1768199.
Department of Health, National Health Genomics Policy Framework 2018 - 2021. 2017, Canberra, ACT: Commonwealth of Australia.
Department of Health and Social Care, et al., Genome UK: the future of healthcare. 2020, United Kingdom: HM Government.
Morrow A et al (2018) Genetics in palliative oncology: a missing agenda? A review of the literature and future directions. Support Care Cancer 26(3):721–730. https://doi.org/10.1007/s00520-017-4017-9
O’Shea, R., et al. (2021), Health system interventions to integrate genetic testing in routine oncology services: a systematic review. 16(5):e0250379. https://doi.org/10.1371/journal.pone.0250379
Quillin JM et al (2010) Exploring hereditary cancer among dying cancer patients—a cross-sectional study of hereditary risk and perceived awareness of DNA testing and banking. J Genet Couns 19(5):497–525. https://doi.org/10.1007/s10897-010-9308-y
Quillin JM et al (2018) High-risk palliative care patients’ knowledge and attitudes about hereditary cancer testing and DNA Banking. J Genet Couns 27(4):834–843. https://doi.org/10.1007/s10897-017-0181-b
Kentwell M et al (2017) Mainstreaming cancer genetics: a model integrating germline BRCA testing into routine ovarian cancer clinics. Gynecol Oncol 145(1):130–136. https://doi.org/10.1016/j.ygyno.2017.01.030
Underhill ML et al (2020) Health care provider perceptions of caring for individuals with inherited pancreatic cancer risk. J Cancer Educ 35(1):194–203. https://doi.org/10.1007/s13187-019-01623-1
Schlich-Bakker KJ et al (2007) Barriers to participating in genetic counseling and BRCA testing during primary treatment for breast cancer. Genet Med 9(11):766–777. https://doi.org/10.1097/gim.0b013e318159a318
Roeland EJ et al (2017) Addressing hereditary cancer risk at the end of life. J Oncol Pract 13(10):e851–e856. https://doi.org/10.1200/JOP.2017.021980
Klepek H et al (2019) Lack of consensus in ALS genetic testing practices and divergent views between ALS clinicians and patients. Amyotroph Lateral Scler Frontotemporal Degener 20(3–4):216–221. https://doi.org/10.1080/21678421.2019.1582670
Bonter K et al (2011) Personalised medicine in Canada: a survey of adoption and practice in oncology, cardiology and family medicine. BMJ Open 1(1):e000110. https://doi.org/10.1136/bmjopen-2011-000110
Lillie AK. (2009) ‘The missing discourse’: how does the family history of cancer affect the care needs of palliative care patients? (Doctoral dissertation, University of Birmingham)
Daniels MS et al (2011) A clinical perspective on genetic counseling and testing during end of life care for women with recurrent progressive ovarian cancer: opportunities and challenges. Fam Cancer 10(2):193–197. https://doi.org/10.1007/s10689-011-9418-1
Vears DF et al (2020) Human genetics society of Australasia position statement: predictive and presymptomatic genetic testing in adults and children. Twin Res Hum Genet 23(3):184–189. https://doi.org/10.1017/thg.2020.51
Kuchenbaecker KB et al (2017) Risks of Breast, Ovarian, and Contralateral Breast Cancer for BRCA1 and BRCA2 Mutation Carriers. JAMA 317(23):2402–2416. https://doi.org/10.1001/jama.2017.7112
White S, Jacobs C, Phillips J (2020) Mainstreaming genetics and genomics: a systematic review of the barriers and facilitators for nurses and physicians in secondary and tertiary care. Genet Med 22(7):1149–1155. https://doi.org/10.1038/s41436-020-0785-6
Metcalfe A, Pumphrey R, Clifford C (2010) Hospice nurses and genetics: implications for end-of-life care. J Clin Nurs 19(1–2):192–207. https://doi.org/10.1111/j.1365-2702.2009.02935.x
Quillin JM et al (2011) Physicians’ current practices and opportunities for DNA banking of dying patients with cancer. J Oncol Pract 7(3):183–187. https://doi.org/10.1200/JOP.2010.000190
Lillie AK, Clifford C, Metcalfe A (2011) Caring for families with a family history of cancer: why concerns about genetic predisposition are missing from the palliative agenda. Palliat Med 25(2):117–124. https://doi.org/10.1177/0269216310383738
Gonthier C et al (2018) Issues related to family history of cancer at the end of life: a palliative care providers’ survey. Fam Cancer 17(2):303–307. https://doi.org/10.1007/s10689-017-0021-y
Dearing A, Taverner N (2018) Mainstreaming genetics in palliative care: barriers and suggestions for clinical genetic services. J Community Genet 9(3):243–256. https://doi.org/10.1007/s12687-017-0345-1
Craig P et al (2008) Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 337:a1655. https://doi.org/10.1136/bmj.a1655
Thorne SE (2016) Interpretive description: qualitative research for applied practice. 2nd ed. Developing qualitative inquiry; 2. New York, NY: Routledge.
Creswell, J.W. and J.D. Creswell, Research design : qualitative, quantitative, and mixed methods approaches. 5th ed. 2018, Thousand Oaks, California: SGE Publications.
Bauer MS et al (2015) An introduction to implementation science for the non-specialist. BMC Psychol 3(1):32. https://doi.org/10.1186/s40359-015-0089-9
World Health Organization, Innovative care for chronic conditions: building blocks for action. 2002, Geneva, Switzerland: Noncommunicable Diseases and Mental Health, World Health Organization.
Zoom Video Communications. Zoom. 2020 [cited 2020 19th November]; Available from: https://zoom.us/. Accessed 19 Aug 2020
Braun V, Clarke V (2019) To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qual Res Sport Exercs Health 13(2):201–216. https://doi.org/10.1080/2159676x.2019.1704846
Yardley L (2000) Dilemmas in qualitative health research. Psychol Health 15(2):215–228
Braun V, Clarke V (2021) Thematic analysis, in Analysing qualitative data in psychology, E. Lyons and A. Coyle, Editors. SAGE Publishing: London, UK. 128–147.
Wright S et al (2019) Negotiating jurisdictional boundaries in response to new genetic possibilities in breast cancer care: the creation of an ‘oncogenetic taskscape.’ Soc Sci Med 225:26–33. https://doi.org/10.1016/j.socscimed.2019.02.020
Ingleby LJ. Clinical genetics in a palliative care setting: a qualitative exploration of the barriers and levers staff report when discussing family risk of BRCA 1 and BRCA 2 mutations (Doctoral dissertation, University of Leicester)
Ha VTD, Frizzo-Barker J, Chow-White P (2018) Adopting clinical genomics: a systematic review of genomic literacy among physicians in cancer care. BMC Med Genomics 11(1):18. https://doi.org/10.1186/s12920-018-0337-y
Vajda A et al (2017) Genetic testing in ALS: a survey of current practices. Neurology 88(10):991–999. https://doi.org/10.1212/WNL.0000000000003686
Crellin E et al (2019) Preparing medical specialists to practice genomic medicine: education an essential part of a broader strategy. Front Genet 10:789. https://doi.org/10.3389/fgene.2019.00789
Paneque M et al (2016) A systematic review of interventions to provide genetics education for primary care. BMC Fam Pract 17(1):89. https://doi.org/10.1186/s12875-016-0483-2
Long JC et al (2018) Using behaviour change and implementation science to address low referral rates in oncology. BMC Health Serv Res 18(1):904. https://doi.org/10.1186/s12913-018-3653-1
Roberts MC et al (2017) The current state of implementation science in genomic medicine: opportunities for improvement. Genet Med 19(8):858–863. https://doi.org/10.1038/gim.2016.210
Ferrell BR, et al. (2018) National consensus project clinical practice guidelines for quality palliative care guidelines, 4th Edition. J Palliat Med. 21(12):1684– 1689. https://doi.org/10.1089/jpm.2018.0431. Accessed 13 Jan 2021
Quillin JM, Bodurtha JN, Smith TJ (2008) Genetics assessment at the end of life: suggestions for implementation in clinic and future research. J Palliat Med 11(3):451–458. https://doi.org/10.1089/jpm.2007.0150
Australian Institute of Health and Welfare. Palliative care services in Australia. 2021 [cited 2021 24th August]; Available from: https://www.aihw.gov.au/reports/palliative-care-services/palliative-care-services-in-australia/contents/palliative-careworkforce. Accessed 13 Jan 2021
Acknowledgements
Thank you to all of the individual clinicians who took the time to share their views and experiences of genetics in palliative care for the benefit of this research.
Funding
This project is funded by a Translational Cancer Research Network PhD Scholarship Top-up Award, supported by the Cancer Institute NSW. S.W is the recipient of a PhD stipend scholarship from the Translational Cancer Research Network (http://www.tcrn.unsw.edu.au/).
Author information
Authors and Affiliations
Contributions
S.W, C.J and J.P contributed to the study conception and design. Material preparation and data collection were performed by S.W, C.J and J.P. Data analysis was performed by all authors. The first draft of the manuscript was written by S.W, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the University of Technology Sydney Research Ethics Office (ETH20-5046). Verbal informed consent was obtained prior to the interview.
Consent for publication
Verbal consent included consent to publish the findings with the assurance that participant’s identifying details would be removed.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
White, S., Phillips, J., Turbitt, E. et al. Views and experiences of palliative care clinicians in addressing genetics with individuals and families: a qualitative study. Support Care Cancer 30, 1615–1624 (2022). https://doi.org/10.1007/s00520-021-06569-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06569-z