Abstract
Background
Previous studies have found that patients with lung cancer report worse patient experience compared to other tumour groups. Reasons that may negatively impact patient experience include delays in diagnosis as well as inadequate symptom management. The purpose of this study was to compare the diagnostic timelines and symptom reports of patients with lung and gastrointestinal (GI) cancers.
Methods
This study included patients diagnosed with lung or GI cancers who attended a radiation oncology (RO) consultation and/or received radiation treatment between May and August 2019 at the Tom Baker Cancer Centre, Calgary, Alberta, Canada. Data collected included demographics, dates of diagnostic time points, and self-reported symptom scores across 3 time points. A descriptive analysis was completed, and the median number of days between time points was compared between tumour groups.
Results
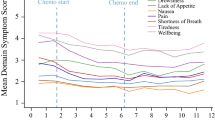
Patients with lung cancer had longer diagnostic timelines compared to GI patients. The median number of days between the first investigative test and biopsy was 21 days longer for patients with lung cancer (p < 0.05). From RO consultation to the first treatment review appointment, 25% and 4% of lung and GI patients, respectively, reported worsening of symptoms. A greater proportion of lung patients reported worse symptom scores during treatment compared to GI patients. This varied by specific symptom.
Conclusions
Patients with lung cancer experienced delays in receiving a diagnosis and worse symptom burden during radiation therapy in this study. We identified potential targets to improve patient experience.


Similar content being viewed by others
Availability of data
De-identified data can be shared upon request.
Code availability
Analysis was performed using Microsoft Excel and RStudio v1.0.153.
References
Canadian Institute for Health Information. Patient experience. CIHI. Published 2020. https://www.cihi.ca/en/patient-experience%0D. Accessed October 28, 2020
Wolf JA, Niederhauser V, Marshburn D, Lavela SL (2014) Defining patient experience. Patient Exp J 1(1):7–19. https://doi.org/10.35680/2372-0247.1004
Lines LM, Lepore M, Wiener JM (2015) Patient-centered, person-centered, and person-directed care: they are not the same. Med Care 53(7):561–563. https://doi.org/10.1097/MLR.0000000000000387
The Beryl Institute. Defining patient experience. The Beryl Institute. https://www.theberylinstitute.org/page/definingpatientexp. Accessed October 28, 2020
Biddy R, Griffin C, Johnson N, Al E (2015) Person-centered care guideline
Ekman I, Swedberg K, Taft C et al (2011) Person-centered care - ready for prime time. Eur J Cardiovasc Nurs 10(4):248–251. https://doi.org/10.1016/j.ejcnurse.2011.06.008
Yannitsos D, Grendarova P, Al-Rashdan A et al (2019) Patient experience in radiation oncology
Fitch MI (2019) The changing face of lung cancer: survivor perspectives on patient engagement. Asia-Pac J Oncol Nurs 6(1):17–23. https://doi.org/10.4103/apjon.apjon-43-18
Tsianakas V, Robert G, Maben J, Richardson A, Dale C, Wiseman T (2012) Implementing patient-centred cancer care: using experience-based co-design to improve patient experience in breast and lung cancer services. Support Care Cancer 20(11):2639–2647. https://doi.org/10.1007/s00520-012-1470-3
Dy SM, Janssen EM, Ferris A, Bridges JF (2017) Live, Learn, Pass It on. J Patient Exp 4(4):162–168. https://doi.org/10.1177/2374373517714451
Bravi F, Di Ruscio E, Frassoldati A et al (2018) Patient and health care professional perspectives: a case study of the lung cancer integrated care pathway. Int J Integr Care 18(4):1–13. https://doi.org/10.5334/ijic.3972
Mokhles S, Nuyttens JJME, de Mol M et al (2018) Treatment selection of early stage non-small cell lung cancer: the role of the patient in clinical decision making. BMC Cancer 18(1):1–10. https://doi.org/10.1186/s12885-018-3986-5
Sanders SL, Bantum EO, Owen JE, Thornton AA, Stanton AL (2010) Supportive care needs in patients with lung cancer. Psychooncology 19(5):480–489. https://doi.org/10.1002/pon.1577
Cuthbert CA, Watson L, Xu Y, Boyne DJ, Hemmelgarn BR, Cheung WY (2019) Patient-reported outcomes in Alberta: rationale, scope, and design of a database initiative. Curr Oncol 26(4):e503–e509. https://doi.org/10.3747/co.26.4919
Watanabe S, Nekolaichuk C, Beaumont C, Mawani A (2009) The Edmonton symptom assessment system-what do patients think? Support Care Cancer 17(6):675–683. https://doi.org/10.1007/s00520-008-0522-1
Watanabe SM, Nekolaichuk C, Beaumont C, Johnson L, Myers J, Strasser F (2011) A multicenter study comparing two numerical versions of the Edmonton symptom assessment system in palliative care patients. J Pain Symptom Manage 41(2):456–468. https://doi.org/10.1016/j.jpainsymman.2010.04.020
Selby D, Cascella A, Gardiner K et al (2010) A single set of numerical cutpoints to define moderate and severe symptoms for the Edmonton symptom assessment system. J Pain Symptom Manag 39(2):241–249. https://doi.org/10.1016/j.jpainsymman.2009.06.010
Bruix J, Llovet JM (2009) Major achievements in hepatocellular carcinoma. Lancet 373(9664):614–616. https://doi.org/10.1016/S0140-6736(09)60381-0
Wait Time Alliance. Cancer care: wait time benchmarks for cancer care. Wait Time Alliance. Published 2014. https://www.waittimealliance.ca/benchmarks/cancer-care/. Accessed October 30, 2020
Howell D, Keshavarz H, Esplen MJ, Hack T, Hamel M, Howes J, Jones J, Li M, Manii D, McLeod D, Mayer C, Sellick S, Riahizadeh S, Noroozi H, Ali M, on behalf of the Cancer Journey Advisory Group of the Canadian Partnership Against Cancer (2015) A Pan Canadian Practice Guideline: screening, Assessment and care of psychosocial distress, depression, and anxiety in adults with cancer. Canadian Partnership Against Cancer and the Canadian Association of Psychosocial Oncology, Toronto
Li M, Kennedy EB, Byrne N, Gérin-Lajoie C, Katz MR, Keshavarz H, Sellick S, Green E (2016) Management of depression in patients with cancer: a clinical practice guideline. J Oncol Pract 12(8):747–756. https://doi.org/10.1200/JOP.2016.011072
Clover KA, Mitchell AJ, Britton B, Carter G (2015) Why do oncology outpatients who report emotional distress decline help? Psychooncology 24(7):812–818. https://doi.org/10.1002/pon.3729
Carolan CM, Smith A, Davies GR, Forbat L (2018) Seeking, accepting and declining help for emotional distress in cancer: a systematic review and thematic synthesis of qualitative evidence. Eur J Cancer Care (Engl) 27(2):1–26. https://doi.org/10.1111/ecc.12720
Mosher C, Joseph W, Hanna N et al (2014) Barriers to mental health service use and preference for addressing emotional concerns among lung cancer patients. Psychooncology 23(7):812–819. https://doi.org/10.1002/pon.3488.Barriers
Halpern MT, Urato MP, Lines LM, Cohen JB, Arora NK, Kent EE (2018) Healthcare experience among older cancer survivors: analysis of the SEER-CAHPS dataset. J Geriatr Oncol 9(3):194–203. https://doi.org/10.1016/j.jgo.2017.11.005
Ayanian JZ, Zaslavsky AM, Arora NK et al (2010) Patients’ experiences with care for lung cancer and colorectal cancer: findings from the cancer care outcomes research and surveillance consortium. J Clin Oncol 28(27):4154–4161. https://doi.org/10.1200/JCO.2009.27.3268
Chen J, Ou L, Hollis S (2013) A systematic review of the impact of routine collection of patient reported outcome measures on patients, providers and health organisations in an oncologic setting. BMC Health Serv Res 13:211. https://doi.org/10.1186/1472-6963-13-211
Kotronoulas G, Kearney N, Maguire R et al (2014) What is the value of the routine use of patient-reported outcome measures toward improvement of patient outcomes, processes of care, and health services outcomes in cancer care? A systematic review of controlled trials. J Clin Oncol 32(14):1480–1501. https://doi.org/10.1200/JCO.2013.53.5948
Barbera L, Lee F, Sutradhar R (2019) Use of patient-reported outcomes in regional cancer centres over time: a retrospective study. CMAJ Open 7(1):E101–E108. https://doi.org/10.9778/cmajo.20180074
Mahar AL, Davis LE, Bubis LD et al (2019) Factors associated with receipt of symptom screening in the year after cancer diagnosis in a universal health care system: a retrospective cohort study. Curr Oncol 26(1):e8–e16. https://doi.org/10.3747/co.26.4160
Funding
This study was supported by the Person-centered Radiation Oncology Service Enhancement (PROSE) programme.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the conceptualization of the manuscript; DY drafted the manuscript, while LB, AR, and PG provided clinical input and editorial oversight. All authors provided critical appraisal of the manuscript and approve its submission.
Corresponding author
Ethics declarations
Ethics approval
The Institutional Research Information Services Solution (IRISS) Health Research Ethics Board through the University of Calgary provided ethics approval: HREBA.CC-18–0588.0
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Yannitsos, D., Barbera, L., Al-Rashdan, A. et al. Diagnostic timelines and self-reported symptoms of patients with lung and gastrointestinal cancers undergoing radiation therapy. Retrospective case control study. Support Care Cancer 30, 1501–1509 (2022). https://doi.org/10.1007/s00520-021-06522-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06522-0