No CrossRef data available.
Article contents
Alpha-blockade during congenital heart surgery admissions: analysis from national database
Published online by Cambridge University Press: 17 September 2021
Abstract
The effects of alpha-blockade on haemodynamics during and following congenital heart surgery are well documented, but data on patient outcomes, mortality, and hospital charges are limited. The purpose of this study was to characterise the use of alpha-blockade during congenital heart surgery admissions and to determine its association with common clinical outcomes.
A cross-sectional study was conducted using the Pediatric Health Information System database. De-identified data for patients under 18 years of age with a cardiac diagnosis who underwent congenital heart surgery were obtained from 2004 to 2015. Patients were subdivided on the basis of receiving alpha-blockade with either phenoxybenzamine or phentolamine during admission or not. Continuous and categorical variables were analysed using Mann−Whitney U-tests and Fisher exact tests, respectively. Characteristics between subgroups were compared using univariate analysis. Regression analyses were conducted to determine the impact of alpha-blockade on ICU length of stay, hospital length of stay, billed charges, and mortality.
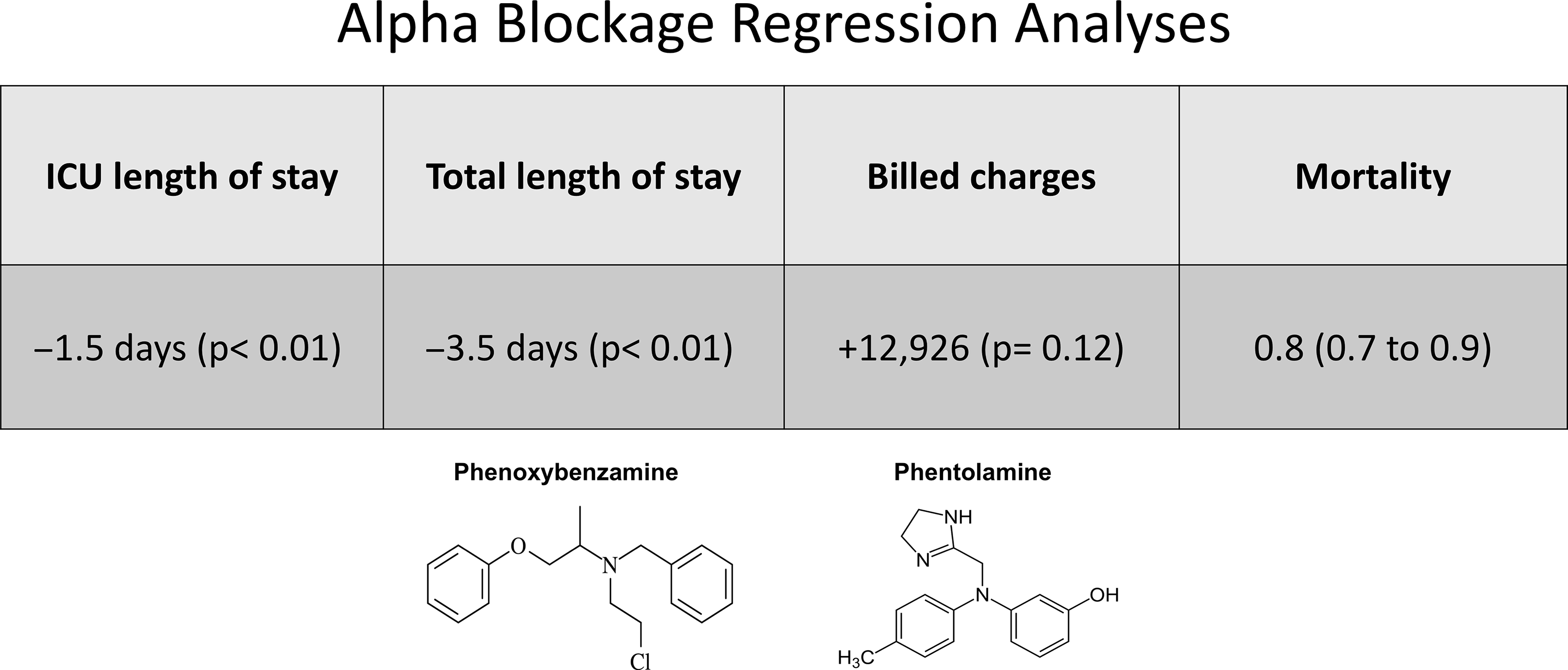
Of the 81,313 admissions, 4309 (5.3%) utilised alpha-blockade. Phentolamine was utilised in 4290 admissions. In univariate analysis, ICU length of stay, total length of stay, inpatient mortality, and billed charges were all significantly higher in the alpha-blockade admissions. However, regression analyses demonstrated that other factors were behind these increased. Alpha-blockade was significantly, independently associated with a 1.5 days reduction in ICU length of stay (p < 0.01) and a 3.5 days reduction in total length of stay (p < 0.01). Alpha-blockade was significantly, independently associated with a reduction in mortality (odds ratio 0.8, 95% confidence interval 0.7−0.9). Alpha-blockade was not independently associated with any significant change in billed charges.
Alpha-blockade is used in a subset of paediatric cardiac surgeries and is independently associated with significant reductions in ICU length of stay, hospital length of stay, and mortality without significantly altering billed charges.
- Type
- Original Article
- Information
- Copyright
- © The Author(s), 2021. Published by Cambridge University Press





