Abstract
Background
Pathways towards many adult-onset conditions begin early in life, even in utero. Maternal health in pregnancy influences this process, but little is known how it affects neonatal metabolism. We investigated associations between pregnancy and birth factors and cord blood metabolomic profile in a large, population-derived cohort.
Methods
Metabolites were measured using nuclear magnetic resonance in maternal (28 weeks gestation) and cord serum from 912 mother–child pairs in the Barwon Infant Study pre-birth cohort. Associations between maternal (metabolites, age, BMI, smoking), pregnancy (pre-eclampsia, gestational diabetes (GDM)), and birth characteristics (delivery mode, gestational age, weight, infant sex) with 72 cord blood metabolites were examined by linear regression.
Results
Delivery mode, sex, gestational age, and birth weight were associated with specific metabolite levels in cord blood, including amino acids, fatty acids, and cholesterols. GDM was associated with higher cord blood levels of acetoacetate and 3-hydroxybutyrate.
Conclusions
Neonatal factors, particularly delivery mode, were associated with many cord blood metabolite differences, including those implicated in later risk of cardiometabolic disease. Associations between GDM and higher offspring ketone levels at birth are consistent with maternal ketosis in diabetic pregnancies. Further work is needed to determine whether these neonatal metabolome differences associate with later health outcomes.
Impact
-
Variations in blood metabolomic profile have been linked to health status in adults and children, but corresponding data in neonates are scarce.
-
We report evidence that pregnancy complications, mode of delivery, and offspring characteristics, including sex, are independently associated with a range of circulating metabolites at birth, including ketone bodies, amino acids, cholesterols, and inflammatory markers.
-
Independent of birth weight, exposure to gestational diabetes is associated with higher cord blood ketone bodies and citrate.
-
These findings suggest that pregnancy complications, mode of delivery, gestational age, and measures of growth influence metabolic pathways prior to birth, potentially impacting later health and development.
Similar content being viewed by others
Introduction
Substantial evidence implicates both maternal health during pregnancy and perinatal factors with offspring risk for a range of adverse health outcomes in later life, potentially through subtle programming of development and metabolism during critical periods in utero.1 However, the underlying biological processes and pathways remain poorly understood.
Metabolomics quantifies large number of molecular biomarkers with potential to identify perturbations in metabolic pathways and biomarkers of risk. Studies of adults and older children have identified specific predictors of risk across a range of non-communicable diseases, particularly cardiovascular disease,2,3 and all-cause mortality in adults.4 There is evidence for metabolomic profiles also being predictive of adverse subclinical atherosclerosis in young adults,5 with several metabolomic measures, including higher low-density lipoprotein (LDL) cholesterol, apolipoprotein B (ApoB), omega-6 fatty acids, tyrosine, and glutamine and lower docosahexaenoic acid (DHA), at baseline associated with higher measures of atherosclerosis at follow-up. Similarly, non-high-density lipoprotein (non-HDL) forms of cholesterol in childhood have been linked to later measures of subclinical atherosclerosis in young adults, though this increased risk was attenuated in those with normal levels of non-HDL cholesterols by adulthood.6 Elevated inflammation markers are also linked to higher atherosclerosis.7 While metabolomic profiles in later childhood and adulthood have been linked to atherosclerosis, there is evidence that the pathways to atherosclerosis may begin very early in life, even before birth.8 However, there are currently limited data on the infant metabolome and its determinants, and it remains unclear how prenatal and birth exposures, which are associated with later development and future disease risk, might be reflected in differences in the circulating metabolomic profile at birth.
Maternal body mass index (BMI),9,10 impaired glucose tolerance,9 and gestational diabetes (GDM)11 have been associated with offspring metabolites at birth, including higher levels of ketone bodies, valine, and glycerol. Mode of delivery and exposure to labour may also influence metabolite profile at birth,12,13,14 though findings are inconsistent.
Sex appears to impact cord blood levels of cholesterols, glycerides, phospholipids, Apos, and amino acids15 in a similar manner to adults,16 although the differences are generally more pronounced in adulthood.17,18 There is also evidence for a relationship between weight and cord blood metabolite profile,9,19,20 similar to that seen in adults21 and children.22 Specifically, branched-chain amino acids, and some phospholipids,23 are positively associated with birth weight,19 while an inverse relationship exists for non-esterified fatty acids.20
Here we profiled the maternal pregnancy and infant cord blood serum metabolome with a widely used nuclear magnetic resonance (NMR) platform in a population-derived cohort. We first investigated the cross-sectional associations of infant sex, birth weight z-score, gestational age, and mode of delivery with cord blood metabolites. We then investigated whether maternal and pregnancy factors were associated with birth metabolite profile.
Methods
Study cohort
The Barwon Infant Study (BIS) is a population-based pregnancy cohort (n = 1064 pregnancies). Mothers were recruited at approximately 15 weeks gestation with eligibility and exclusion criteria detailed previously.24 Briefly, mothers were eligible if they resided in the Barwon region of south-east Australia and intended to give birth at the local public or private hospital. Exclusion criteria for the cohort were mothers aged <18 years or were not a permanent Australian resident or had previously participated in BIS or required a translator to complete questionnaires or were unable or unwilling to provide informed consent or were planning to store their infant’s cord blood privately or had moved out of the Barwon region by the time of birth. No other exclusion criteria were imposed on participation of pregnant women. Infant exclusion criteria were <32 weeks completed gestation or diagnosis of a serious illness or congenital condition within the first few days of life. Participants provided informed consent, and ethics was approved by the Barwon Health Human Research Ethics Committee (HREC 10/24). Blood collected from mothers (28 weeks gestation) and infant venous cord blood (birth) were transported directly to the local Pathology laboratory and centrifuged within 2–3 h of collection. Aliquots of serum at both time points were stored at −80 °C until transported on dry ice to Nightingale Health (Helsinki, Finland) for metabolomic profiling.
Maternal and infant measures
Maternal age, smoking (dichotomised into any/none), pre-pregnancy and 28 weeks gestation weight, and height were collected by questionnaire and used to calculate BMI (kg/m2). Tertiles of circulating glucose levels were derived 1 h after 50 g anhydrous glucose ingestion for a fasted glucose challenge test in a hospital setting at approximately 28 weeks gestation. GDM was diagnosed with a fasted oral glucose tolerance test according to International Association of Diabetes and Pregnancy Study Groups criteria25: plasma glucose >5.1 mmol/L at fasting or >8.5 mmol/L 2 h after a 75-g oral glucose load. Pre-eclampsia was diagnosed using the International Society for the Study of Hypertension in Pregnancy criteria.26 Tertiles of maternal socio-economic status were derived from the Socio-Economic Indexes For Areas27 using maternal address at recruitment. Parity was considered as a dichotomous primiparous/multiparous measure.
Data on infant sex, weight, and gestational age at birth were obtained from hospital records. Birth weight z-scores (standardised for gestational age and sex) were calculated using the 2009 revised British UK–WHO growth charts.28 As very few infants were born small for gestational age (n = 3), birth weight z-score was considered as a continuous exposure. Mode of delivery was categorised as either planned caesarean section (CS) prior to labour (planned CS) or other delivery mode (not delivered by planned CS), which included unplanned CS, unassisted vaginal delivery, and tool-assisted vaginal delivery. Previous studies have reported that vaginal delivery following induction of labour is not associated with substantial metabolomic differences in cord blood compared to spontaneous vaginal delivery.12,29
Metabolomic measurement
The Nightingale Health NMR-based metabolomic platform has been described in detail previously,30 as have its applications in epidemiological studies.31 In brief, this platform quantitates lipoprotein subclasses and composition, fatty acids, and other low-weight metabolites, including glycolysis-related metabolites and amino acids. Metabolites were quantified using the 2016 and 2019 analytical pipelines for the maternal and the cord blood samples, respectively. A subset of triplicate samples showed low percentage of coefficient of variation (<10%).
There were 228 measures generated for maternal serum at 28 weeks gestation, and 72 of these were also measured in cord blood serum. Primary analysis used 51 informative measures (predominantly metabolite concentrations) due to the strong correlation between metabolite concentration and ratio measures, as previously reported in adults.32 Data for the excluded ratio measures are presented in Supplementary Information (Supplementary Tables S1–S15).
Statistical analysis
Analysis was performed in Stata v16 and R v3.6.3. Data visualisation was based on Nightingale’s ‘ggforestplot’ package (v0.1.0) vignettes in R. Metabolites were natural log-transformed, and all metabolomic and continuous maternal measures (age, pre-pregnancy BMI, and change in BMI to 28 weeks gestation) were scaled to a standard distribution (SD units). Normality of distributions was assessed before and after log-transformation using Shapiro–Wilk test statistic.
To investigate the cross-sectional relationship between each birth factor and infant metabolite (outcome), both unadjusted linear regression and models adjusted for the other birth factors were considered. Additional adjustment for maternal parity was considered. Given the evidence for sex-specific differences in metabolomic measures,33 sex-stratified models were also investigated. As sensitivity analyses, we considered models excluding infants exposed to pre-eclampsia and/or GDM. We also considered models excluding infants with delivery modes other than planned CS or unassisted vaginal delivery.
Pearson’s correlation was used to test associations for each metabolite between mother (28 weeks gestation) and infant (birth) samples. For other maternal factors (age, pre-pregnancy BMI, change in BMI to 28 weeks gestation, smoking, GDM, and pre-eclampsia), linear regression models adjusted for sex, mode of delivery, gestational age, and birth weight z-score were used (cord blood metabolite as outcome). BMI is a risk factor for GDM34 and pre-eclampsia,35 so pre-pregnancy BMI was considered as a covariate in both models. Additional adjustment for corresponding metabolite levels in 28-week gestational maternal serum, socio-economic status tertile, and parity were also considered. In secondary analysis, we tested whether glucose tertile was associated with metabolites. As ketosis can occur during labour,36 we also stratified by mode of delivery.
Benjamini–Hochberg37 was used to adjust for multiple comparisons with a false-discovery rate (FDR) of 5%.
Results
Participant characteristics of the 912 infants tested are presented in Table 1. Summary statistics for metabolomic measures are presented in Supplementary Table S1.
Sex differences
In both the unadjusted (Supplementary Table S2) and adjusted (Fig. 1 and Supplementary Table S3) models, there was evidence of higher omega-3 fatty acids, ApoA1, ApoB (Fig. 1a), total cholesterol, and most cholesterol species (Fig. 1b) in female infants, as well as larger HDL particle size (Fig. 1b). No metabolites were higher in males.
The difference in mean metabolite log concentration in SD units for boys compared to girls in adjusted models. Panel (a) is amino acids, ketone bodies, glycerides and phospholipids, glycolysis-related metabolites, and fluid balance markers; (b) is fatty acids, apolipoproteins, cholesterol, lipoprotein particle size, and inflammation (GlycA). Error bars represent 95% confidence intervals. Closed points represent associations with significant p value at the 5% FDR level after adjustment using the Benjamini–Hochberg method. The associations depicted here are listed in Supplementary Table S3. C cholesterol, DHA docosahexaenoic acid, HDL high-density lipoprotein, IDL intermediate density lipoprotein, LA linoleic acid, LDL low-density lipoprotein, MUFA monounsaturated fatty acids, PG phosphoglycerides, PUFA polyunsaturated fatty acids, SFA saturated fatty acids, TG triglycerides, VLDL very-low-density lipoprotein.
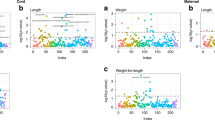
Birth weight
Increasing birth weight z-score in both unadjusted (Supplementary Table S4) and adjusted models (Fig. 2 and Supplementary Table S5) was associated with lower triglycerides and pyruvate and higher ketone bodies (Fig. 2a), as well as lower DHA, omega-3 fatty acids, ApoB, very-low-density lipoprotein (VLDL) cholesterol and VLDL/LDL particle size (Fig. 2b). Additional adjustment for parity modestly attenuated the relationship between weight and pyruvate (data not shown). Evidence of sex-specific associations was noted (Supplementary Fig. S1 and Supplementary Table S5), with increasing weight associated with higher histidine (Supplementary Fig. S1a) and ApoA1 (Supplementary Fig. S1b) in males. Birth weight z-score was negatively associated with unsaturated fatty acids (Supplementary Fig. S1b) in females only.
The difference in mean metabolite log concentration in SD units per 1 unit increase in birth weight z-score in adjusted models. Panel (a) is amino acids, ketone bodies, glycerides and phospholipids, glycolysis-related metabolites, and fluid balance markers; (b) is fatty acids, apolipoproteins, cholesterol, lipoprotein particle size, and inflammation (GlycA). Error bars represent 95% confidence intervals. Closed points represent associations with significant p value at the 5% FDR level after adjustment using the Benjamini–Hochberg method. The associations depicted here are listed in Supplementary Table S5. C cholesterol, DHA docosahexaenoic acid, HDL high-density lipoprotein, IDL intermediate density lipoprotein, LA linoleic acid, LDL low-density lipoprotein, MUFA monounsaturated fatty acids, PG phosphoglycerides, PUFA polyunsaturated fatty acids, SFA saturated fatty acids, TG triglycerides, VLDL very-low-density lipoprotein.
Gestational age
In unadjusted models, gestational age was associated with higher alanine, phenylalanine, leucine, albumin, pyruvate, 3-hydroxybutyrate, VLDL-triglycerides, omega-3, DHA and unsaturated fatty acids, VLDL and LDL particle size, and GlycA (Supplementary Table S6). In the adjusted model (Fig. 3 and Supplementary Table S7), gestational age was associated with lower tyrosine and sphingomyelins and higher albumin (Fig. 3a), DHA, unsaturated, and omega-3 fatty acids, lower ApoA1, total, free and HDL cholesterol, and GlycA (Fig. 3b). Sex-specific differences were noted with lower glutamine and higher creatinine in females (Supplementary Fig. S2 and Supplementary Table S7). Exclusion of infants exposed to pre-eclampsia and/or GDM strengthened evidence for an association between higher gestational age and higher alanine, glycine, citrate, and total triglycerides and attenuated evidence for relationships between gestational age and total cholesterol, free cholesterol, and total cholines (Supplementary Fig. S3).
The difference in mean metabolite log concentration in SD units per 1 week increase in gestational age in adjusted models. Panel (a) is amino acids, ketone bodies, glycerides and phospholipids, glycolysis-related metabolites, and fluid balance markers; (b) is fatty acids, apolipoproteins, cholesterol, lipoprotein particle size, and inflammation (GlycA). Error bars represent 95% confidence intervals. Closed points represent associations with significant p value at the 5% FDR level after adjustment using the Benjamini–Hochberg method. The associations depicted here are listed in Supplementary Table S7. C cholesterol, DHA docosahexaenoic acid, HDL high-density lipoprotein; IDL intermediate density lipoprotein, LA linoleic acid, LDL low-density lipoprotein, MUFA monounsaturated fatty acids, PG phosphoglycerides, PUFA polyunsaturated fatty acids, SFA saturated fatty acids, TG triglycerides, VLDL very-low-density lipoprotein.
Mode of delivery
In unadjusted models, compared to planned CS, being delivered by modes other than planned CS was associated with higher amino acids, glycerides, glycolysis-related metabolites (pyruvate, citrate, glycerol), fatty acids, and GlycA (Supplementary Table S8). In adjusted models (Fig. 4 and Supplementary Table S9), this was associated with higher amino acids, 3-hydroxybuterate, glycerides, glycolysis-related metabolites, albumin (Fig. 4a), fatty acids, Apos, cholesterol, and GlycA (Fig. 4b). There was also a general shift in lipoprotein particle sizes (Fig. 4b). In sex-stratified analysis (Supplementary Fig. S4 and Supplementary Table S9), higher levels of total, omega-3, omega-6, polyunsaturated fatty acids, monounsaturated fatty acids, short chain, and linoleic fatty acids were more evident in males not delivered by planned CS compared to those in the planned CS group. In sensitivity analysis comparing infants delivered by planned CS to infants delivered by unassisted vaginal delivery only, there was evidence for higher valine and acetate in the unassisted vaginal delivery group, but findings did not otherwise change comparing with the model including all delivery modes (data not shown).
The difference in mean metabolite log concentration in SD units in infants not delivered by planned CS compared to infants delivered by planned CS in adjusted models. Panel (a) is amino acids, ketone bodies, glycerides and phospholipids, glycolysis-related metabolites, and fluid balance markers; (b) is fatty acids, apolipoproteins, cholesterol, lipoprotein particle size, and inflammation (GlycA). Error bars represent 95% confidence intervals. Closed points represent associations with significant p value at the 5% FDR level after adjustment using the Benjamini–Hochberg method. The associations depicted here are listed in Supplementary Table S9. C cholesterol, DHA docosahexaenoic acid, HDL high-density lipoprotein, IDL intermediate density lipoprotein, LA linoleic acid, LDL low-density lipoprotein, MUFA monounsaturated fatty acids, PG phosphoglycerides, PUFA polyunsaturated fatty acids, SFA saturated fatty acids, TG triglycerides, VLDL very-low-density lipoprotein.
Maternal factors and cord blood metabolites
There was a modest correlation (r = 0.11–0.31) between maternal (28 weeks gestation) and cord (birth) serum measures, particularly amino acids and cholesterol subclasses (Supplementary Table S10). The strongest correlations were seen for the DHA/total fatty acid (r = 0.28) and omega-3/total fatty acid (r = 0.31) ratios.
There was little evidence for associations between maternal anthropometry and infant metabolites (Supplementary Fig. S5 and Supplementary Table S11). Pre-pregnancy BMI was only associated with elevated triglyceride/phosphoglyceride ratio (Supplementary Fig. S5a). Neither maternal age nor BMI change over time was associated with any infant measures.
Exposure to GDM was associated with elevated cord blood serum ketone bodies (acetoacetate and 3-hydroxybutyrate) and citrate (Fig. 5 and Supplementary Table S12). Exposure to pre-eclampsia was associated with higher glutamine and glycerol (Fig. 5a). In models additionally adjusted for pre-pregnancy BMI (Supplementary Tables S13 and S14), estimated coefficients for GDM predicting ketone body and citrate concentrations were slightly reduced, with stronger relationships seen in females. After adjustment, the associations with pre-eclampsia remained present in female infants only. Additional adjustment for corresponding metabolite levels in 28-week gestational maternal serum, socio-economic status tertile, and parity did not change findings (data not shown).
The difference in mean metabolite log concentration in SD units in exposed infants compared to unexposed infants. Panel (a) is amino acids, ketone bodies, glycerides and phospholipids, glycolysis-related metabolites, and fluid balance markers; (b) is fatty acids, apolipoproteins, cholesterol, lipoprotein particle size, and inflammation (GlycA). Error bars represent 95% confidence intervals. Closed points represent associations with significant p value at the 5% FDR level after adjustment using the Benjamini–Hochberg method. The associations depicted here are listed in Supplementary Table S12. C cholesterol, DHA docosahexaenoic acid, HDL high-density lipoprotein, IDL intermediate density lipoprotein, LA linoleic acid, LDL low-density lipoprotein, MUFA monounsaturated fatty acids, PG phosphoglycerides, PUFA polyunsaturated fatty acids, SFA saturated fatty acids, TG triglycerides, VLDL very-low-density lipoprotein.
In the secondary analysis of glucose tertiles, no association was seen with any cord serum metabolite concentrations at an FDR-adjusted level (Supplementary Table S15). However, we found that the association between GDM exposure and higher ketone bodies was specific to infants not delivered by planned CS (1.05 SD units higher acetoacetate in GDM-exposed infants [95% confidence interval (CI) 0.65 to 1.45], p < 0.001; 0.96 SD units higher 3-hydroxybutyrate [95% CI 0.56 to 1.35], p < 0.001), with those delivered by planned CS and GDM-exposed showing less evidence of an association (−0.07 SD units acetoacetate in GDM-exposed infants [95% CI −0.60 to 0.47], p = 0.81; −0.04 SD units 3-hydroxybutyrate [95% CI −0.51 to 0.43], p = 0.86).
Discussion
Using NMR metabolomics, we found evidence of variation in cord blood metabolites, including cholesterols, Apos, fatty acids, triglycerides, amino acids, ketone bodies and a marker of inflammation, in association with infant sex, gestational age, birth weight, and mode of delivery. We also found evidence for higher concentrations of ketone bodies in infants exposed to GDM. These findings build on previous smaller studies that reported evidence for cord blood metabolite differences in association with these factors.11,12,13,14,16,19 These exposures are linked with risk of a range of non-communicable diseases later in childhood and adulthood, and early-life metabolomic differences may potentially contribute mechanistically to these relationships.
Most cholesterol subclasses were higher in females at birth, as were omega-3 and Apos ApoA1 and ApoB, with females also having a generally larger HDL particle size compared to males. No metabolites were higher in males. This is in keeping with previous findings in the same individuals at 12 months of age,16 highlighting the stability of this association postnatally. A previous liquid chromatography/mass spectrometry (LS-MS) metabolomic study of newborn dried blood spots stored at room temperature reported higher levels of several amino acids in females, including alanine, glycine, methionine, valine, and tyrosine.15 We found weaker evidence of this relationship, with only glycine nominally higher in females. This is potentially due to the differing sample type (whole blood collected 2–3 days postnatally vs cord blood serum), technical issues associated with blood spot storage (room temperature vs −80 °C), and/or measurement platform (LC-MS vs NMR). Future work is required to investigate whether the metabolic differences between sexes are due to female newborns having greater fat mass than males on average,38 despite having a lower average birth weight. Similar to our findings, a recent study considering sex differences using this same NMR platform at other ages across life course (5 age groups from mean age 8 years to mean age 50 years)17 reported that the males in the pre-pubertal time point had lower metabolite levels compared to females across almost all metabolomic measures, though this sex-dimorphic pattern changed following puberty, and the sex-specific patterns become more complex. While sex hormones are believed to play a key role in sex differences of both metabolic regulation and cardiometabolic disease risk, there is also clear evidence for sex hormone-independent sex differences in metabolomic profiles.39,40
Birth weight z-score was negatively associated with triglycerides, consistent with previous findings in both maternal and neonatal blood.41 This relationship may also persist postnatally, with higher birth weight negatively associated with circulating triglycerides in adulthood.42 Increasing birth weight was also associated with higher HDL-C and lower omega-3 and DHA. However, gestational age (adjusted for birth factors) was inversely associated with each of these measures. Interestingly, gestational age (adjusted for birth weight, sex, and mode of delivery) was positively associated with GlycA, an emerging biomarker of chronic inflammation and predictor of cardiovascular disease in adults.43 This contrasts with a previous study in extremely preterm infants (<28 weeks gestation) that reported a decrease in acute inflammatory markers (C-reactive protein, interleukin (IL)-1β, and IL-6) with increasing gestational age.44 It is plausible that a ‘U-shaped’ relationship exists between gestational age and inflammation, with the relationship observed in this current study specific to the range of gestational ages in this cohort (late preterm and term infants). Maternal inflammation is thought to contribute to the increased risk of preterm birth.45 Furthermore, markers of inflammation in the maternal circulation may be reflected in higher levels of infant acute inflammatory markers in the offspring. Therefore, it is plausible that higher levels of inflammatory markers in cord blood of preterm infants may simply be a reflection of higher maternal inflammation. It is also worth noting that studies measuring GlycA in cord blood are limited, particularly in relation to preterm birth, and that, where assessed in parallel, GlycA and high-sensitivity C-reactive protein (hsCRP) are only moderately correlated measures.46 While differences in metabolites implicated in pro-atherogenic metabolomic profiles5,6,7 were identified in this study, neither greater birth weight nor greater gestation age were associated with metabolic differences consistent with pro-atherogenic dyslipidaemia.
Delivery by modes other than planned CS was positively associated with most amino acids and fatty acids, triglycerides, Apos, glycolysis-related metabolites, albumin, 3-hydroxybutyrate, and GlycA, with slightly larger differences generally seen in male infants. This is consistent with previous findings of higher concentrations of non-esterified fatty acids and several amino acids, including phenylalanine and valine in vaginally born infants.12 Higher levels of GlycA are in accord with our previous data showing higher hsCRP, soluble CD14, IL-6, and proportions of granulocytes in infants exposed to labour during delivery47 and are consistent with labour as a pro-inflammatory process. Labour involves the release of many hormones from both maternal and foetal tissues, including cortisol and oxytocin, both of which have been implicated in regulation of glucose and fatty acid metabolism.48,49,50,51 These and other mediators released in the peri-partum may be contributing to the distinct metabolomic differences observed for infants delivered following labour in this study.
Metabolites in maternal 28-week gestational serum showed a modest correlation with cord serum metabolites, with the strongest correlations observed for amino acids. A cross-sectional study for maternal and fetal blood taken during delivery by CS (n = 179) reported correlations (r) between 0.14 and 0.79 for each of the 19 amino acids measures,52 which is greater than the associations observed in our study, suggesting a more pronounced correlation closer to the time of delivery. Pre-pregnancy BMI was not associated with differences in cord blood metabolites in our study. While maternal pre-pregnancy BMI is associated with offspring metabolic health throughout life course,53 a meta-analysis of three European birth cohorts suggested genetics or shared lifestyle factors as primary contributors to offspring metabolic health, rather than in utero factors.54 Exposure to GDM showed the strongest evidence for differences in cord blood metabolites, specifically elevated ketone bodies and citrate. It is well established that diabetes is associated with ketosis due to reduced glucose uptake, reflected in higher circulating ketone bodies.55 Similarly, GDM has been associated with higher ketone bodies, fatty acids, lipoproteins, and markers of inflammation in plasma and serum of obese women during pregnancy.56 As ketone bodies are freely transported across the placental barrier,57 elevated ketone bodies in the blood of women with GDM closer to birth would be anticipated to impact on cord blood ketone body concentrations. However, adjustment for maternal ketone bodies at 28 weeks gestation did not alter the relationship between GDM exposure and neonate ketone bodies observed. A previous study of 2000 neonates similarly reported an association between maternal fasting glucose levels at 28 weeks gestation and elevated 3-hydroxybutyrate in cord blood plasma.9 Unlike previous studies,9,11 we did not find evidence of higher valine in neonates exposed to GDM, though previous studies did not adjust for other birth factors considered here. A study in children (n = 592, age 6–14 years) exposed to GDM, using a different metabolomic platform, found that GDM was associated with higher serum phospholipids and higher adiposity in girls.58 Interestingly, the strongest evidence for GDM exposure impacting on ketone bodies was observed in infants who were exposed to labour during delivery (not planned CS). While higher circulating glucose is characteristic of GDM,25 cellular glucose uptake is lower for women with GDM compared to non-GDM pregnant women.59 As labour is a period of extreme energy requirement and metabolic stress, we anticipate the maternal need for ketosis to be greater in GDM-exposed labour due to lower glucose availability compared to non-exposed, leading to higher maternal circulating levels of ketone bodies and consequently neonate ketone bodies, with increased risk of neonatal acidosis.36 This is consistent with a previous study reporting higher incidence of neonatal acidosis in infants born from term pregnancies of women with GDM compared to non-GDM.60 While the effects of labour-induced acidosis are not clear, a meta-analysis has previously reported an association between low cord blood pH and increased risk of neonate mortality and morbidities.61
Strengths of our study include the large population-based cohort of mother–infant dyads and data on maternal and pregnancy factors. It is the first to consider independent associations of these maternal and birth factors with neonatal metabolome. Limitations include the relatively small proportion of infants exposed to pregnancy conditions such as GDM (n = 39) and pre-eclampsia (n = 29) and potential selection bias, which may limit the generalisability of findings.62 Another consideration is that these cord blood samples were taken shortly after delivery that entailed exposure to labour for the majority of infants. Labour is a metabolically stressful time and associated with a range of metabolic changes as reported in this study. However, mode of delivery was included as a covariate in the adjusted models.
Conclusions
Understanding factors that might shape early-life metabolic health is crucial for elucidating potential mechanisms that might underpin healthy or impaired future development. This and other recent studies provide evidence that birth characteristics and pregnancy exposures independently associate with metabolomic profiles at birth, including metabolites implicated in future risk of cardiovascular disease. Larger studies are needed to more fully explore the sex- and delivery mode-specific associations observed here.
Change history
29 October 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41390-021-01789-9
References
Calkins, K. & Devaskar, S. U. Fetal origins of adult disease. Curr. Probl. Pediatr. Adolesc. Health Care 41, 158–176 (2011).
Floegel, A. et al. Serum metabolites and risk of myocardial infarction and ischemic stroke: a targeted metabolomic approach in two German prospective cohorts. Eur. J. Epidemiol. 33, 55–66 (2018).
Tzoulaki, I. et al. Serum metabolic signatures of coronary and carotid atherosclerosis and subsequent cardiovascular disease. Eur. Heart J. 40, 2883–2896 (2019).
Deelen, J. et al. A metabolic profile of all-cause mortality risk identified in an observational study of 44,168 individuals. Nat. Commun. 10, 1–8 (2019).
Würtz, P. et al. High-throughput quantification of circulating metabolites improves prediction of subclinical atherosclerosis. Eur. Heart J. 33, 2307–2316 (2012).
Juonala, M. et al. Non-HDL cholesterol levels in childhood and carotid intima-media thickness in adulthood. Pediatrics 145, e20192114 (2020).
Shah, P. K. Inflammation, infection and atherosclerosis. Trends Cardiovasc. Med. 29, 468–472 (2019).
Nakashima, Y., Wight, T. N. & Sueishi, K. Early atherosclerosis in humans: role of diffuse intimal thickening and extracellular matrix proteoglycans. Cardiovasc. Res. 79, 14–23 (2008).
Lowe, W. L. et al. Maternal BMI and glycemia impact the fetal metabolome. Diabetes Care 40, 902–910 (2017).
Desert, R., Canlet, C., Costet, N., Cordier, S. & Bonvallot, N. Impact of maternal obesity on the metabolic profiles of pregnant women and their offspring at birth. Metabolomics 11, 1896–1907 (2015).
Dani, C. et al. Metabolomic profile of term infants of gestational diabetic mothers. J. Matern. Fetal Neonatal Med. 27, 537–542 (2014).
Marchioro, L. et al. Caesarean section, but not induction of labour, is associated with major changes in cord blood metabolome. Sci. Rep. 9, 1–9 (2019).
Shokry, E. et al. Investigation of the impact of birth by cesarean section on fetal and maternal metabolism. Arch. Gynecol. Obstet. 300, 589–600 (2019).
Birchenall, K. A., Welsh, G. I. & López Bernal, A. Metabolite changes in maternal and fetal plasma following spontaneous labour at term in humans using untargeted metabolomics analysis: a pilot study. Int. J. Environ. Res. Public Health 16, 1527 (2019).
Ruoppolo, M. et al. Female and male human babies have distinct blood metabolomic patterns. Mol. Biosyst. 11, 2483–2492 (2015).
Ellul, S. et al. Sex differences in infant blood metabolite profile in association with weight and adiposity measures. Pediatr. Res. 88, 473–483 (2020).
Bell, J. A. et al. Sex differences in systemic metabolites at four life stages: cohort study with repeated metabolomics. BMC Med. 19, 58 (2021).
Ellul, S. et al. Metabolomics: population epidemiology and concordance in Australian children aged 11–12 years and their parents. BMJ Open 9, 106–117 (2019).
Perng, W. et al. Associations of cord blood metabolites with perinatal characteristics, newborn anthropometry, and cord blood hormones in project viva. Metabolism 76, 11–22 (2017).
Hellmuth, C. et al. Cord blood metabolome is highly associated with birth weight, but less predictive for later weight development. Obes. facts 10, 85–100 (2017).
Ho, J. E. et al. Metabolomic profiles of body mass index in the Framingham Heart Study reveal distinct cardiometabolic phenotypes. PLoS ONE 11, e0148361 (2016).
Saner, C. et al. Sex and puberty-related differences in metabolomic profiles associated with adiposity measures in youth with obesity. Metabolomics 15, 75 (2019).
Rauschert, S., Uhl, O., Koletzko, B. & Hellmuth, C. Metabolomic biomarkers for obesity in humans: a short review. Ann. Nutr. Metab. 64, 314–324 (2014).
Vuillermin, P. et al. Cohort profile: the Barwon Infant Study. Int J. Epidemiol. 44, 1148–1160 (2015).
Nankervis, A., McIntyre, H. D., Moses, R. G., Ross, G. P. & Callaway, L. K. Testing for gestational diabetes mellitus in Australia. Diabetes Care 36, e64 (2013).
Tranquilli, A. et al. The classification, diagnosis and management of the hypertensive disorders of pregnancy: a revised statement from the ISSHP. Pregnancy Hypertens. 4, 97 (2014).
Pink, B. Technical Paper: Socio-Economic Indexes for Areas (SEIFA) (Australian Bureau of Statistics, 2011).
Cole, T. J., Williams, A. F. & Wright, C. M. Revised birth centiles for weight, length and head circumference in the UK-WHO growth charts. Ann. Hum. Biol. 38, 7–11 (2011).
Hashimoto, F. et al. Metabolomics analysis of umbilical cord blood clarifies changes in saccharides associated with delivery method. Early Hum. Dev. 89, 315–320 (2013).
Kettunen, J. et al. Genome-wide association study identifies multiple loci influencing human serum metabolite levels. Nat. Genet 44, 269–276 (2012).
Würtz, P. et al. Quantitative serum nuclear magnetic resonance metabolomics in large-scale epidemiology: a primer on-omic technologies. Am. J. Epidemiol. 186, 1084–1096 (2017).
Auro, K. et al. A metabolic view on menopause and ageing. Nat. Commun. 5, 4708 (2014).
Xie, G. et al. The metabolite profiles of the obese population are gender-dependent. J. Proteome Res. 13, 4062–4073 (2014).
Torloni, M. et al. Prepregnancy BMI and the risk of gestational diabetes: a systematic review of the literature with meta‐analysis. Obes. Rev. 10, 194–203 (2009).
O’Brien, T. E., Ray, J. G. & Chan, W.-S. Maternal body mass index and the risk of preeclampsia: a systematic overview. Epidemiology 14, 368–374 (2003).
Toohill, J., Soong, B. & Flenady, V. Interventions for ketosis during labour. Cochrane Database Syst. Rev. CD004230 (2008).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B (Methodol.) 57, 289–300 (1995).
Hawkes, C. P. et al. Gender-and gestational age–specific body fat percentage at birth. Pediatrics 128, e645–e651 (2011).
Wang, X., Magkos, F. & Mittendorfer, B. Sex differences in lipid and lipoprotein metabolism: it’s not just about sex hormones. J. Clin. Endocrinol. Metab. 96, 885–893 (2011).
Comitato, R., Saba, A., Turrini, A., Arganini, C. & Virgili, F. Sex hormones and macronutrient metabolism. Crit. Rev. Food Sci. Nutr. 55, 227–241 (2015).
Schaefer-Graf, U. M. et al. Maternal lipids as strong determinants of fetal environment and growth in pregnancies with gestational diabetes mellitus. Diabetes Care 31, 1858–1863 (2008).
Ramadhani, M. K. et al. Lower birth weight predicts metabolic syndrome in young adults: the Atherosclerosis Risk in Young Adults (ARYA)-study. Atherosclerosis 184, 21–27 (2006).
Duprez, D. A. et al. Comparison of the predictive value of GlycA and other biomarkers of inflammation for total death, incident cardiovascular events, noncardiovascular and noncancer inflammatory-related events, and total cancer events. Clin. Chem. 62, 1020–1031 (2016).
Leviton, A. et al. Inflammation-related proteins in the blood of extremely low gestational age newborns. The contribution of inflammation to the appearance of developmental regulation. Cytokine 53, 66–73 (2011).
Cappelletti, M., Della Bella, S., Ferrazzi, E., Mavilio, D. & Divanovic, S. Inflammation and preterm birth. J. Leukoc. Biol. 99, 67–78 (2016).
Muhlestein, J. B. et al. GlycA and hsCRP are independent and additive predictors of future cardiovascular events among patients undergoing angiography: the intermountain heart collaborative study. Am. Heart J. 202, 27–32 (2018).
Collier, F. et al. Naïve regulatory T cells in infancy: associations with perinatal factors and development of food allergy. Allergy 74, 1760–1768 (2019).
Ortiz, R. et al. The association of morning serum cortisol with glucose metabolism and diabetes: the Jackson Heart Study. Psychoneuroendocrinology 103, 25–32 (2019).
John, K., Marino, J. S., Sanchez, E. R. & Hinds, T. D. Jr The glucocorticoid receptor: cause of or cure for obesity? Am. J. Physiol. Endocrinol. Metab. 310, E249–E257 (2016).
Lawson, E. A., Olszewski, P. K., Weller, A. & Blevins, J. E. The role of oxytocin in regulation of appetitive behaviour, body weight and glucose homeostasis. J. Neuroendocrinol. 32, e12805 (2020).
Ding, C., Leow, M. S. & Magkos, F. Oxytocin in metabolic homeostasis: implications for obesity and diabetes management. Obes. Rev. 20, 22–40 (2019).
Holm, M. B. et al. Uptake and release of amino acids in the fetal-placental unit in human pregnancies. PLoS ONE 12, e0185760 (2017).
Monasta, L. et al. Early‐life determinants of overweight and obesity: a review of systematic reviews. Obes. Rev. 11, 695–708 (2010).
Santos Ferreira, D. L. et al. Association of pre-pregnancy body mass index with offspring metabolic profile: analyses of 3 European prospective birth cohorts. PLoS Med. 14, e1002376 (2017).
Laffel, L. Ketone bodies: a review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab. Res. Rev. 15, 412–426 (1999).
White, S. L. et al. Metabolic profiling of gestational diabetes in obese women during pregnancy. Diabetologia 60, 1903–1912 (2017).
Herrera, E. & Lasunción, M. A. in Fetal and Neonatal Physiology (eds Polin, R. A., Abman, S. H., Rowitch, D. H., Benitz, W. E. & Fox, W. W.) 342.e4–353.e4 (Elsevier, 2017).
Perng, W. et al. A prospective study of associations between in utero exposure to gestational diabetes mellitus and metabolomic profiles during late childhood and adolescence. Diabetologia 63, 296–312 (2020).
Friedman, J. E. et al. Impaired glucose transport and insulin receptor tyrosine phosphorylation in skeletal muscle from obese women with gestational diabetes. Diabetes 48, 1807–1814 (1999).
Aalipour, S., Hantoushzadeh, S., Shariat, M., Sahraian, S. & Sheikh, M. Umbilical cord blood acidosis in term pregnancies with gestational diabetes mellitus and its relations to maternal factors and neonatal outcomes. Iran. Red Crescent Med. J. https://doi.org/10.5812/ircmj.59267 (2018).
Malin, G. L., Morris, R. K. & Khan, K. S. Strength of association between umbilical cord pH and perinatal and long term outcomes: systematic review and meta-analysis. BMJ 340, c1471 (2010).
Galea, S. & Tracy, M. Participation rates in epidemiologic studies. Ann. Epidemiol. 17, 643–653 (2007).
Acknowledgements
We thank the BIS participants for the generous contribution they have made to this project. We also thank current and past staff for their efforts in recruiting and maintaining the cohort and in obtaining and processing the data and biospecimens.
Funding
The establishment work and infrastructure for the BIS was provided by the Murdoch Children’s Research Institute, Deakin University, and Barwon Health. Subsequent funding was secured from the National Health and Medical Research Council of Australia, The Jack Brockhoff Foundation, the Scobie Trust, the Shane O’Brien Memorial Asthma Foundation, the Our Women’s Our Children’s Fund Raising Committee Barwon Health, The Shepherd Foundation, the Rotary Club of Geelong, the Ilhan Food Allergy Foundation, GMHBA Limited, the Percy Baxter Charitable Trust, and Perpetual Trustees. In-kind support was provided by the Cotton On Foundation and CreativeForce. Research at Murdoch Children’s Research Institute is supported by the Victorian Government’s Operational Infrastructure Support Program. This work was also supported by NHMRC Senior Research Fellowships (1008396 to A.-L.P.; 1064629 to D.B.; 1045161 to R.S.) and NHMRC Investigator Grants to A.-L.P. (1110200) and D.B. (1175744). Funders did not participate in the work or writing of this manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
T.M., D.B., F.C., and R.S. conceptualised and developed this study. T.M. undertook all aspects of data analysis. F.C. managed collection of samples and coordinated sample shipping and measurement collation and quality control. T.M., D.B., and R.S. drafted the manuscript. All authors provided critical expert advice and critical review of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Informed participant consent was required and attained for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The legend of Figure 2 has been corrected.
Supplementary information
Rights and permissions
About this article
Cite this article
Mansell, T., Vlahos, A., Collier, F. et al. The newborn metabolome: associations with gestational diabetes, sex, gestation, birth mode, and birth weight. Pediatr Res 91, 1864–1873 (2022). https://doi.org/10.1038/s41390-021-01672-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-021-01672-7
This article is cited by
-
Risk of adverse pregnancy outcomes in pregnant women with gestational diabetes mellitus by age: a multicentric cohort study in Hebei, China
Scientific Reports (2024)
-
Maternal glycemic status during pregnancy and mid-childhood plasma amino acid profiles: findings from a multi-ethnic Asian birth cohort
BMC Medicine (2023)
-
Metabolomic profiling of intrauterine growth-restricted preterm infants: a matched case–control study
Pediatric Research (2023)
-
Sex differences in glycolipidic disorders after exposure to maternal hyperglycemia during early development
Journal of Endocrinological Investigation (2023)