Abstract
Objective
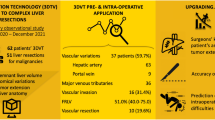
To explore the utility of three-dimensional (3D) visualization technology in liver resection for patients with complex liver cancer.
Methods
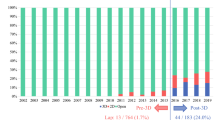
In this retrospective cohort study, we collected and analyzed clinic pathological data from 105 patients who underwent complicated liver cancer resection at the authors’ unit between January 2014 and June 2019. Observation indicators included general demographic information, operative time, intraoperative blood loss, blood transfusion volume, postoperative liver function, complication rate, hospital stay, and in-hospital mortality.
Results
Compared with the complex liver cancer control group, operative time (257.1 ± 63.4 min versus [vs] 326.6 ± 78.3 min; P < 0.001), intraoperative blood loss (256.4 ± 159.1 mL vs 436.1 ± 177.3 mL; P < 0.001), blood transfusion volume (213.3 ± 185.2 mL vs 401.6 ± 211.2 mL; P < 0.001), and length of hospital stay (9.7 ± 3.1 days vs 11.9 ± 3.3 days; P = 0.001) were significantly reduced in the complex liver cancer reconstruction group. Although there was no statistical difference in total postoperative complication rate between the two groups, the incidence of serious postoperative complications in the reconstruction group was significantly lower than that in the control group (3/54 [5.6%] vs 10/51 [19.6%], respectively; P = 0.038). Regarding laboratory investigations, the time to recovery of liver function in the complex liver cancer reconstruction group was shorter than that in the complex liver cancer control group.
Conclusion
The use of 3D visualization technology was highly influential in formulating meticulous, individualized surgical strategies for complex liver cancer liver resection with safety and reduced perioperative risk.



Similar content being viewed by others
References
Mcglynn KA, Petrick JL, London WT (2015) Global epidemiology of hepatocellular carcinoma: an emphasis on demographic and regional variability. Clin Liver Dis 19(2):223–238
Dagon B, Baur C, Bettschart V (2008) A framework for intraoperative update of 3D deformable models in liver surgery. Conference proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Conference 2008:3235-3238
Lamade W, Glombitza G, Fischer L, Chiu P, Cardenas CS, Thorn M, Meinzer HP, Grenacher L, Bauer H, Lehnert T, Herfarth C (2000) The impact of 3-dimensional reconstructions on operation planning in liver surgery. Arch Surg 135(11):1256–1261
Tian F, Wu JX, Rong WQ, Wang LM, Wu F, Yu WB, An SL, Liu FQ, Feng L, Bi C, Liu YH (2015) Three-dimensional morphometric analysis for hepatectomy of centrally located hepatocellular carcinoma: a pilot study. World J Gastroenterol 21(15):4607–4619
Fang CH, Tao HS, Yang J, Fang ZS, Cai W, Liu J, Fan YF (2015) Impact of three-dimensional reconstruction technique in the operation planning of centrally located hepatocellular carcinoma. J Am Coll Surg 220(1):28–37
Jiang C, Liu B, Chen S, Peng Z, Xie X, Kuang M (2018) Safety margin after radiofrequency ablation of hepatocellular carcinoma: precise assessment with a three-dimensional reconstruction technique using CT imaging. Int J Hyperther 34(8):1135–1141
Nanashima A, Abo T, Sakamoto I, Hayashi H, Nagayasu T (2012) Three-dimensional fusion images of hepatic vasculature and bile duct used for preoperative simulation before hepatic surgery. Hepatogastroenterology 59(118):1748–1757
Cai W, Fan Y, Hu H, Xiang N, Fang C, Jia F (2017) Postoperative liver volume was accurately predicted by a medical image three dimensional visualization system in hepatectomy for liver cancer. Surg Oncol 26(2):188–194
Yamanaka J, Saito S, Fujimoto J (2007) Impact of preoperative planning using virtual segmental volumetry on liver resection for hepatocellular carcinoma. World J Surg 31(6):1249–1255
Jang JS, Cho JY, Ahn S, Han HS, Yoon YS, Choi Y, Kwon SU, Kim S, Guro H (2018) Comparative performance of the complexity classification and the conventional major/minor classification for predicting the difficulty of liver resection for hepatocellular carcinoma. Ann Surg 267(1):18–23
Lee MK, Gao F, Strasberg SM (2016) Completion of a liver surgery complexity score and classification based on an international survey of experts. J Am Coll Surg 223(2):332–342
Fan ST (2002) Methods and related drawbacks in the estimation of surgical risks in cirrhotic patients undergoing hepatectomy. Hepatogastroenterology 49(43):17–20
Imamura H, Sano K, Sugawara Y, Kokudo N, Makuuchi M (2005) Assessment of hepatic reserve for indication of hepatic resection: decision tree incorporating indocyanine green test. J Hepatobiliary Pancreat Surg 12(1):16–22
Nuh NR, James Garden O, Robert P, Mark B, Michael C, Rene A, Moritz K, Masatoshi M, Ronald PD, Christopher C, Simon B, Val U, Masato N, Guy M, Thomas JH, Jean-Nicolas V, Paul G, Myrddin R, Yukihiro Y, Sheung Tat F, Yuji N, Joan F, Lorenzo C, Markus WB, Jürgen W (2011) Posthepatectomy liver failure: a definition and grading by the International study group of liver surgery (ISGLS). Surgery. https://doi.org/10.1016/j.surg.2010.10.001
Vauthey JN, Chaoui A, Do KA, Bilimoria MM, Fenstermacher MJ, Charnsangavej C, Hicks M, Alsfasser G, Lauwers G, Hawkins IF, Caridi J (2000) Standardized measurement of the future liver remnant prior to extended liver resection: methodology and clinical associations. Surgery 127(5):512–519
Ferrero A, Vigano L, Polastri R, Muratore A, Eminefendic H, Regge D, Capussotti L (2007) Postoperative liver dysfunction and future remnant liver: where is the limit? Results of a prospective study. World J Surg 31(8):1643–1651
Nagai S, Fujii T, Kodera Y, Kanda M, Nakao A (2010) Impact of operative blood loss on survival in invasive ductal adenocarcinoma of the pancreas. Pancreas 40(1):3–9
Ribeiro HSC, Costa WL, Diniz AL, Godoy AL, Herman P, Coudry RA, Coudry RA, Begnami MDFS, Mello CAL, Silva MJB, Zurstrassen CE, Coimbra FJF (2013) Extended preoperative chemotherapy, extent of liver resection and blood transfusion are predictive factors of liver failure following resection of colorectal liver metastasis. Eur J Surg Oncol 39(4):380–385
Aramaki O, Takayama T, Higaki T, Nakayama H, Matsuyama Y (2014) Decreased blood loss reduces postoperative complications in resection for hepatocellular carcinoma. J Hepatobiliary Pancreat Sci 21(8):585–591
Sano K, Makuuchi M, Miki K, Maema A, Takayama T (2002) Evaluation of hepatic venous congestion: proposed indication criteria for hepatic vein reconstruction. Ann Surg 236(2):241–247
Lang H (2005) Impact of virtual tumor resection and computer-assisted risk analysis on operation planning and intraoperative strategy in major hepatic resection. Arch Surg 140(7):629–638
Dong J, Yang S, Zeng J, Cai S, Ji W, Duan W, Zhang A, Ren W, Xu Y, Tan J, Bu X, Zhang N, Wang X, Wang X, Meng X, Jiang K, Gu W, Huang Z (2013) Precision in liver surgery. Semin Liver Dis 33(3):189–203
Acknowledgements
The authors would like to express our gratitude to Prof. Shao Jianghua from Department of General Surgery, Second Affiliated Hospital of Nanchang University, for his assistance and participation in the conclusion part of this paper. We also thank the Imaging Center of Second Affiliated Hospital of Nanchang University for their superb technical and equipment assistance in data collection and analysis.
Funding
This study was supported by the National Natural Science Foundation of China (81760435) and youth science foundation of Jiangxi (20192ACBL21036).
Author information
Authors and Affiliations
Contributions
Conceptualization: WS, CY, JL. Data analysis: WS, CY, JL. Supply of materials: WS, CY, LW, JY, JG, JL. Draft writing: WS, JL. Final version decision: JL.
Corresponding author
Ethics declarations
Disclosures
Drs Weiwei Sheng, Chendong Yuan, Linquan Wu, Jinlong Yan, Jin Ge, and Jun Lei have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sheng, W., Yuan, C., Wu, L. et al. Clinical application of a three-dimensional reconstruction technique for complex liver cancer resection. Surg Endosc 36, 3246–3253 (2022). https://doi.org/10.1007/s00464-021-08636-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08636-2