Abstract
Background
The thrombosis of the main and intrahepatic branches of the portal vein (TMIP) is potentially lethal and deemed a common complication following laparoscopic splenectomy and azygoportal disconnection (LSD) in patients with cirrhosis and portal hypertension (PH). The predictors of TMIP after LSD remain unclear. The aim of this prospective study was to explore the predictive and risk factors for TMIP after LSD in cirrhotic patients with PH caused only by hepatitis B virus.
Methods
From September 2014 to March 2017, we enrolled 115 patients with hepatitis B cirrhosis and PH who successfully underwent LSD. Patients were subdivided into a TMIP group and a non-TMIP group. Univariate and multivariate logistic regression analysis was conducted on 24 items of demographic and preoperative data, to explore the risk factors of TMIP.
Results
Twenty-nine (25.22%) patients developed TMIP on postoperative day (POD) 7 and 26 (22.81%) patients developed TMIP on POD 30. From POD 7 to POD 30, 12 patients who did not have TMIP at POD 7 were newly diagnosed with TMIP, with portal vein diameter 15.05 ± 2.58 mm. Another 14 patients in whom TMIP had resolved had portal vein diameter 14.02 ± 1.76 mm. Univariate analysis and multivariate logistic regression revealed that portal vein diameter ≥ 13 mm [relative risk (RR) 5.533, 95% confidence interval (CI) 1.222–25.042; P = 0.026] and portal vein diameter ≥ 15 mm (RR 3.636, 95% CI 1.466–9.021; P = 0.005) were significant independent risk factors for TMIP on POD 7 and 30, respectively.
Conclusion
Portal vein diameter ≥ 13 mm and ≥ 15 mm were significant independent predictors for TMIP after LSD in patients with hepatitis B cirrhosis and PH on POD 7 and POD 30, respectively.
Trial registration
We registered our research at https://www.clinicaltrials.gov/. The name of research registered is “Warfarin Prevents Portal Vein Thrombosis in Patients After Laparoscopic Splenectomy and Azygoportal Disconnection.” The trial registration identifier at clinicaltrials.gov is NCT02247414.

Similar content being viewed by others
References
The Polaris Observatory Collaborators (2018) Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study. Lancet Gastroenterol Hepatol 3:383–403
Li H, Yan L, Shi Y, Lv D, Shang J, Bai L, Tang H (2020) Hepatitis B Virus Infection: overview. Adv Exp Med Biol 1179:1–16
Zhang L, Chen Y, Zhang LJ, Wang M, Chang DL, Wan WW, Zhang BX, Zhang WG, Chen XP (2019) HBV induces different responses of the hepatocytes and oval cells during HBV-related hepatic cirrhosis. Cancer Lett 443:47–55
Wright AS, Rikkers LF (2005) Current management of portal hypertension. J Gastrointestinal Surg 9:992–1005
Bancu S, Borz C, Popescu G, Torok A, Mureşan A, Bancu L, Turcu M (2007) Spleno-renal distal and proximal shunts for hypersplenism due to hepatic cirrhosis. Chirurgia 102:665–668
Adam R, Karam V, Delvart V, O’Grady J, Mirza D, Klempnauer J, Castaing D, Neuhaus P, Jamieson N, Salizzoni M et al (2012) Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol 57:675–688
Bodzin AS, Baker TB (2018) Liver transplantation today: where we are now and where we are going. Liver Transplant 24:1470–1475
Narahara Y, Kanazawa H, Fukuda T, Matsushita Y, Harimoto H, Kidokoro H, Katakura T, Atsukawa M, Taki Y, Kimura Y et al (2011) Transjugular intrahepatic portosystemic shunt versus paracentesis plus albumin in patients with refractory ascites who have good hepatic and renal function: a prospective randomized trial. J Gastroenterol 46:78–85
Salerno F, Merli M, Riggio O, Cazzaniga M, Valeriano V, Pozzi M, Nicolini A, Salvatori F (2004) Randomized controlled study of TIPS versus paracentesis plus albumin in cirrhosis with severe ascites. Hepatology 40:629–635
De Cleva R, Herman P, D’Albuquerque LA, Pugliese V, Santarem OL, Saad WA (2007) Pre- and postoperative systemic hemodynamic evaluation in patients subjected to esophagogastric devascularization plus splenectomy and distal splenorenal shunt: a comparative study in schistomomal portal hypertension. World J Gastroenterol 13:5471–5475
Yang Z, Qiu F (2000) Pericardial devascularization with splenectomy for the treatment of portal hypertension. Zhonghua wai ke za zhi [Chin J Surg] 38:645–648
Zhang Y, Wen T, Yan L, Chen Z, Yang H, Deng X, Liang G, Li G, Zhang X, Ran S, Liao Z (2009) The changes of hepatic hemodynamics and functional hepatic reserve after splenectomy with periesophagogastric devascularization. Hepatogastroenterology 56:835–839
Huang L, Yu Q, Wang J (2018) Association between changes in splanchnic hemodynamics and risk factors of portal venous system thrombosis after splenectomy with periesophagogastric devascularization. Med Sci Monit 24:4355–4362
Cheng Z, Li JW, Chen J, Fan YD, Bie P, Wang SG, Zheng SG (2013) Laparoscopic versus open splenectomy and esophagogastric devascularization for bleeding varices or severe hypersplenism: a comparative study. J Gastrointest Surg 17:654–659
Bai DS, Qian JJ, Chen P, Yao J, Wang XD, Jin SJ, Jiang GQ (2014) Modified laparoscopic and open splenectomy and azygoportal disconnection for portal hypertension. Surg Endosc 28:257–264
Yu H, Guo S, Wang L, Dong Y, Tian G, Mu S, Zhang H, Li D, Zhao S (2016) Laparoscopic splenectomy and esophagogastric devascularization for liver cirrhosis and portal hypertension is a safe, effective, and minimally invasive operation. J Laparoendosc Adv Surg Tech A 26:524–530
Jiang GQ, Chen P, Qian JJ, Yao J, Wang XD, Jin SJ, Bai DS (2014) Perioperative advantages of modified laparoscopic vs open splenectomy and azygoportal disconnection. World J Gastroenterol 20:9146–9153
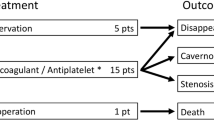
Jiang GQ, Xia BL, Chen P, Qian JJ, Jin SJ, Zuo SQ, Bai DS (2016) Anticoagulation therapy with warfarin versus low-dose aspirin prevents portal vein thrombosis after laparoscopic splenectomy and azygoportal disconnection. J Laparoendosc Adv Surg Tech A 26:517–523
Parikh S, Shah R, Kapoor P (2010) Portal vein thrombosis. Am J Med 123:111–119
Anstee QM, Dhar A, Thursz MR (2011) The role of hypercoagulability in liver fibrogenesis. Clin Res Hepatol Gastroenterol 35:526–533
D’Amico G, De Franchis R (2003) Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology 38:599–612
Bai DS, Xia BL, Zhang C, Ye J, Qian JJ, Jin SJ, Jiang GQ (2019) Warfarin versus aspirin prevents portal vein thrombosis after laparoscopic splenectomy and azygoportal disconnection: a randomized clinical trial. Int J Surg 64:16–23
Moriyasu F, Nishida O, Ban N, Nakamura T, Miura K, Sakai M, Miyake T, Uchino H (1986) Measurement of portal vascular resistance in patients with portal hypertension. Gastroenterology 90:710–717
Jiang GQ, Bai DS, Chen P, Xia BL, Qian JJ, Jin SJ (2016) Predictors of portal vein system thrombosis after laparoscopic splenectomy and azygoportal disconnection: a retrospective cohort study of 75 consecutive patients with 3-months follow-up. Int J Surg 30:143–149
Naymagon L, Tremblay D, Zubizarreta N, Moshier E, Mascarenhas J, Schiano T (2020) Safety, efficacy, and long-term outcomes of anticoagulation in cirrhotic portal vein thrombosis. Digest Dis Sci
Amitrano L, Guardascione MA, Brancaccio V, Margaglione M, Manguso F, Iannaccone L, Grandone E, Balzano A (2004) Risk factors and clinical presentation of portal vein thrombosis in patients with liver cirrhosis. J Hepatol 40:736–741
Ikeda M, Sekimoto M, Takiguchi S, Kubota M, Ikenaga M, Yamamoto H, Fujiwara Y, Ohue M, Yasuda T, Imamura H et al (2005) High incidence of thrombosis of the portal venous system after laparoscopic splenectomy: a prospective study with contrast-enhanced CT scan. Ann Surg 241:208–216
Lindberg F, Rasmussen I, Siegbahn A, Bergqvist D (2000) Coagulation activation after laparoscopic cholecystectomy in spite of thromboembolism prophylaxis. Surg Endosc 14:858–861
Pietrabissa A, Moretto C, Antonelli G, Morelli L, Marciano E, Mosca F (2004) Thrombosis in the portal venous system after elective laparoscopic splenectomy. Surg Endosc 18:1140–1143
La Villa G, Gentilini P (2008) Hemodynamic alterations in liver cirrhosis. Mol Aspects Med 29:112–118
Zhang Y, Wen TF, Yan LN, Yang HJ, Deng XF, Li C, Wang C, Liang GL (2012) Preoperative predictors of portal vein thrombosis after splenectomy with periesophagogastric devascularization. World J Gastroenterol 18:1834–1839
Crary SE, Buchanan GR (2009) Vascular complications after splenectomy for hematologic disorders. Blood 114:2861–2868
Watters JM, Sambasivan CN, Zink K, Kremenevskiy I, Englehart MS, Underwood SJ, Schreiber MA (2010) Splenectomy leads to a persistent hypercoagulable state after trauma. Am J Surg 199:646–651
Kinjo N, Kawanaka H, Akahoshi T, Tomikawa M, Yamashita N, Konishi K, Tanoue K, Shirabe K, Hashizume M, Maehara Y (2010) Risk factors for portal venous thrombosis after splenectomy in patients with cirrhosis and portal hypertension. Br J Surg 97:910–916
Jiang GQ, Bai DS, Chen P, Qian JJ, Jin SJ, Wang XH (2016) Risk factors for portal vein system thrombosis after laparoscopic splenectomy in cirrhotic patients with hypersplenism. J Laparoendosc Adv Surg Tech A 26:419–423
Wang LH, Lu W, Shen GJ, Yu YS, Zhu Ge YH, Hu YG, Wu XQ, Xu TS (2007) Portal vein thrombosis after devascularization procedures in patients with portal hypertension. Zhonghua PutongWaike Zazhi 22:616–618
Acknowledgements
This work was supported by the Project of Invigorating Health Care through Science, Technology and Education: Jiangsu Provincial Medical Youth Talent (QNRC2016331).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Longfei Wu, Dousheng Bai, Lin Shi, Shengjie Jin, Baohuan Zhou, and Guoqing Jiang have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, LF., Bai, DS., Shi, L. et al. Predictors of portal vein thrombosis after laparoscopic splenectomy and azygoportal disconnection in hepatitis B cirrhosis: a prospective study. Surg Endosc 36, 4090–4098 (2022). https://doi.org/10.1007/s00464-021-08730-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08730-5