Abstract
Aims/hypothesis
High prevalence of coexisting morbidity in people with type 2 diabetes highlights the need to include interactions with education and comorbidity in the assessments of societal consequences of type 2 diabetes. The purpose of this study was to estimate the joint effects of education, type 2 diabetes and six frequent comorbidities.
Methods
Nationwide administrative register data on type 2 diabetes diagnosis, hospital admissions, education and disability pension were grouped at the individual level by means of a unique personal identification number. Included were all people (N = 2,281,599) in the age span of 40–59 years living in Denmark in the period 2005 to 2017, covering a total of 17,754,788 person-years. We used both Cox proportional hazards and Aalen additive hazards models to estimate relative and absolute joint effects of type 2 diabetes, educational attainment and six common comorbidities (CVD, cancer and cerebrovascular, respiratory, musculoskeletal and psychiatric diseases). We decomposed the joint effects of educational level, type 2 diabetes and comorbidities into main effects and the interaction effect, measured as extra cases of disability pension.
Results
Lower level of educational attainment, type 2 diabetes and comorbidities independently contributed to additional granted disability pensions. The joint number of cases of disability pension exceeded the sum of the three exposures, which is explained by a synergistic effect of lower educational level, type 2 diabetes and comorbidity.
Conclusions/interpretation
In this population study, the joint effects of type 2 diabetes, lower education and comorbidity were associated with larger than additive rates of disability pension. An integrated approach that takes into account socioeconomic barriers to type 2 diabetes rehabilitation may slow down disease progression and increase the working ability of socially disadvantaged people.
Graphical abstract

Similar content being viewed by others

Introduction
Rehabilitation of middle-aged adults with chronic diseases is important for the ability to continue an active working life. Disease management programmes (DMPs) were introduced in Denmark in 2008 as a part of the healthcare reform with the aim of preventing disease progression and maintaining normal functioning including active employment among people with chronic diseases [1]. Since then, DMPs have been developed for specific disease groups and include agreements on the division of responsibilities for rehabilitation and coordination among general practice, municipalities, specialised care and hospitals [1].
Multimorbidity is a major challenge for rehabilitation and depending on the comorbidity it necessitates collaboration between primary and secondary healthcare as well as between the social and health sectors. However, most DMPs do not address this issue adequately, as they are primarily designed to meet the health needs of people with one disease [2, 3]. In Denmark, general practitioners serve as gatekeepers and are responsible for the referral of patients to treatment. All type 2 diabetes patients are invited to annual check-ups by their general practitioner, and, in cases of incident type 2 diabetes, people are offered rehabilitation at regional specialised centres (severe type 2 diabetes) or at municipal centres (less severe type 2 diabetes). In Western society, type 2 diabetes is the most common chronic disease among people with multimorbidity [4] and the prevalence of multimorbity is higher with decreasing level of educational attainment [4]. Approximately 30% of all Danes aged 45 to 64 years have multimorbidity, defined as two or more diseases [4, 5].
The large variations in the disease manifestations of patients with multiple chronic conditions often cause problems in doctors’ and patients’ overviews of healthcare appointments and medication. For instance, medical treatment of type 2 diabetes may not have the intended effects if it is given together with other medicaments [6], and it may be difficult to follow DMPs, e.g. for patients suffering from musculoskeletal or psychiatric diseases [7].
Social determinants such as low level of educational attainment, financial strain and lack of social support are other factors that increase the risk of developing disease complications and comorbidity [8, 9]. Failure to succeed in halting disease progression can successively turn into a downward spiral for health and labour market participation [7, 10,11,12]. A newly published Danish study by Nexø et al [12] and an international review by Pedron et al [10] conclude that type 2 diabetes increases the risk of labour market exit, but evidence is lacking regarding the influence of comorbidity and socioeconomic position.
The aim of this paper was to estimate the absolute and relative joint effects of education, type 2 diabetes and each of six frequent comorbidities (cancer, CVD, respiratory diseases, psychiatric diseases, cerebrovascular disease and musculoskeletal diseases) on disability retirement. Also, we decomposed the number of granted disability pensions associated with different levels of educational attainment, type 2 diabetes, each of the six comorbidities and joint effects of interaction between these determinants.
Methods
Study population
This cohort study included all people living in Denmark in the period from 1 January 2005 to 31 December 2017, aged 40 to 59 years, who had not been granted disability pension. The age span of the population was chosen as people younger than 40 have restricted possibilities for disability pension and people older than 59 had the possibility for early retirement. The first year of inclusion was 2005 and individuals entered the study successively at the age of 40. People were censored in the year of turning 60, in the year of death, at emigration to another country or at the end of the study period in the year 2017, whichever came first. The study population covered 2,281,599 people after excluding 31,985 people due to missing information on educational attainment (1.4%), resulting in a total of 17,754,788 person-years. The missing records on education are due either to no completed education among adult immigrants or to attained education outside of Denmark with no subsequent formal registration of educational level.
Data
Data were from nationwide administrative social and income registers as well as health registers, e.g. the Danish National Prescription Registry (DNPR) [13] and the Danish National Diabetes Register (DNDR) [14]. Overall, these data are of high validity due to the universal healthcare system and the standardised digital reporting requirements that enable fees for service reimbursement and administrative surveillance of health services. Data were merged at the individual level by means of a unique personal identification number given at birth or immigration. In Denmark, researchers are allowed to use register data for conducting statistical analyses of population-level outcomes, as when complying with a list of predefined ethical standards, including that the people are anonymised for the researchers.
Educational attainment
Socioeconomic position was measured by means of education. Individuals’ records of highest educational attainment came from Danish Education Registers [15], and were categorised according to the International Standard Classification of Education (ISCED 2011) into low education (primary and lower secondary education; <2 years of vocational training/education; ISCED: 0–2), medium education (upper secondary and post-secondary education; 2–4 years of vocational education; ISCED: 3–4) and high education (tertiary education; >4 years of education, academic degree; ISCED: 5–8).
Diabetes
Information on type 2 diabetes was obtained from the DNDR [14] and classification of type 2 diabetes was done according to the algorithm developed by Carstensen and colleagues [16]. People were categorised as having type 2 diabetes if one or more of the following inclusion criteria were met:
-
hospital records: ICD-10 DE10–14, DH36.0, DO24 (excluding DO24.4)
-
registration of chiropody (as a diabetic patient)
-
five blood glucose measurements in a 1 year period or two blood glucose measurements per year in 5 consecutive years
-
second purchase of an oral glucose-lowering drug as recorded in the DNPR [13]
-
second purchase of insulin as recorded in the DNPR
-
people who were not classified as having type one diabetes according to the criteria below, or who had never redeemed an insulin prescription, were classified as having type 2 diabetes.
Information on diabetes diagnosis from DNPR and DNDR was used to exclude patients with type 1 diabetes from patients with type 2 diabetes. If a person fulfilled any of the following criteria, he/she was classified as having type 1 diabetes:
-
registration with a type 1 diabetes diagnosis in DNDR
-
registration with a type 1 diabetes diagnosis and not with type 2 diabetes in DNDR
-
prescription of glucose-lowering medication before the age of 15 in DNPR
-
prescription of insulin before the age of 30 in DNPR and not classified with a type 2 diabetes diagnosis in DNDR.
Comorbid diseases
Data from the Danish National Patient Register including ICD-10 disease codes from hospitals were used to assess the disease prevalence of the study population. Diagnoses were categorised into 20 major disease categories (see Electronic supplementary material [ESM] Table 1 for a list of ICD-10 codes). The six most common disease combinations with type 2 diabetes selected were cancer, CVD, cerebrovascular disease, respiratory disease, psychiatric disease and musculoskeletal disease. The remaining 14 disease categories were digitised into one variable, referred to as ‘other diseases’, which was included as a confounder in the statistical models. People with at least one record within the past 10 years were recorded as morbid. The work ability assessment takes into account diagnosed diseases at the time of assessment. Therefore, diagnoses from the Danish Cause of Death Register were not included in the disease categorisation.
Disability pension
We retrieved information from the Danish Income Statistics Register, including registrations of social security benefits [17]. The primary source of income within the given year was used as the basis for categorisation of disability pension. In Denmark, disability pension is granted to people with permanently and substantially reduced working capacity. Since 2013, in order to be granted disability pension, the workability is first assessed by means of a resource scheme which, among others, takes physical and mental health, working conditions, history of employment and social network into account. These disability pension laws did not seem to have an impact on the results of this paper, as the hazards of the education–type 2 diabetes–comorbidity groups were proportional during the study period.
All-cause mortality
Date of death was obtained from the Danish Civil Registration System (CRS) [18].
Emigration
Date of emigration was obtained from the Danish CRS [18].
Ethnicity, age, sex
We included information on age, sex and ethnicity (Danish origin, immigrant, descendant) from the CRS [18].
Statistical analyses
Statistical models
Cox proportional hazards models can be used to estimate relative HRs and the Aalen additive hazards model can be used to estimate the absolute hazard rate difference (RD). The additive hazards model is a semiparametric model for survival outcomes [19] and is thus at least as flexible as the Cox model. The effect estimate is a hazard difference interpreted as the extra number of events per person-year at risk in a specific exposure category compared with a reference category. This hazard difference can be interpreted as an RD. To most people (including many researchers), relative interactions derived from multiplicative models are counterintuitive and therefore surrogate measures, e.g. attributable proportion due to interaction (AP) is often calculated under the assumption of additivity [20]. The Aalen additive hazards model on the other hand provides all parameter estimates that are needed to assess joint effects of multiple determinants simply by summing the absolute main and interaction effects. The absolute effects are easy to interpret and the most relevant effect measure from a public health point of view. The Aalen additive hazards model is particularly easy to interpret as it can be used to assess deviations from additivity when testing for interactions [20]. In other words, interaction is present whenever the joint effects of the multiple exposures are more (or less) than the sum of the main effects of these exposures. The number of cases from interaction can be calculated as the joint RD, minus the RDs of each of the main effects.
Statistical models applied
All analyses were stratified by sex due to a higher rate of disability pension among women compared with men and considerably higher prevalence of type 2 diabetes among men compared with women. The Aalen and Cox models included the same exposure variables, reference group and covariates, and with age as the underlying timescale. Significance tests determined if the association with disease groups differed between educational groups.
The following models were analysed:
-
Joint effects of education and type 2 diabetes status: The combined variable of education and type 2 diabetes as well as the covariates ethnicity and calendar year were entered into the model. The reference group was set to people with high education and no type 2 diabetes.
-
Joint effects of education, type 2 diabetes and the six most prevalent comorbidities: Six combined variables of education, type 2 diabetes and each of the comorbidities (CVD, cerebrovascular disease, respiratory disease, cancer, musculoskeletal disease and psychiatric disease) were created. The reference group was set to people with high education, no type 2 diabetes and no comorbidity. Each model in addition to the combined variable also included main effects of the other comorbidities and covariates as confounders (ethnicity, calendar year and other diseases). The number of disability pension cases due to interaction was calculated as the joint sum of cases (per 10,000 person-years) minus the cases from each of the three determinants; e.g. Interaction caseslow edu, diabetes, CVD = RDlow edu, diabetes, CVD − RDlow edu − RDdiabetes − RDCVD.
Results
In this Danish population aged 40–59 (Table 1), more men (5.0%, n = 58,064) than women (3.4%, n = 38,165) had type 2 diabetes, and the proportion with type 2 diabetes (number of people with type 2 diabetes education specific/total number of peopleeducation specific) increased with descending level of education: high education (men 3%/women 3%), medium education (men 5%/women 3%) and low education (men 7%/women 5%). Among men and women with type 2 diabetes, 43–44% had one or more comorbidities during the follow-up period. The most common comorbidities were musculoskeletal diseases and CVD. In the total population, 47,988 (4.1%) men and 53,521 (4.8%) women were granted disability pension. These proportions were more than twice as high among people with type 2 diabetes: 5467 men (9.4%) and 4456 women (11.7%). Overall, independent of disease status, the rate of disability pension (number of disability pensions/number of person-years) was noticeably higher for women compared with men.
Joint effects of education and type 2 diabetes
In the model including joint effects of education and diabetes, descending level of educational attainment and type 2 diabetes were associated with higher relative and absolute probability of disability pension (Table 2). Women with low education had more than three times and men more than four times higher HR of disability pension compared with women and men with high education. Extra numbers of granted disability pensions (per 10,000 person-years) were 10 and 51 among women with medium and low education, respectively. Corresponding numbers for men were 16 and 51. Across all educational groups, the additional cases of disability pension were much higher among all people with type 2 diabetes compared with those with only type 2 diabetes, e.g. among all men with type 2 diabetes and high education, 97 extra people were granted disability pension (per 10,000 person-years), compared with all men with type 2 diabetes only (RDdiabetes all, high − RDdiabetes only, high = 134 − 37 = 97). This indicates that a large proportion of the people being granted disability pension among those with type 2 diabetes can be ascribed to the effect of comorbid diseases and/or interactions with these.
Joint effects of education, type 2 diabetes and comorbidity on disability pension
Among men, the rate of disability pension cases increased with lower level of educational attainment, except for psychiatric disease where those with high education had the highest rates of disability pension (Table 3). Among women, for several comorbidities the lowest rates of disability pension were seen with medium education. Still, those with the lowest level of educational attainment likewise had the highest rate of disability pension. Particularly high were the HRs of disability pension for people with low education + type 2 diabetes + cerebrovascular disease (HRmen, low, diabetes, cere = 12.24 [95% CI 6.99, 17.49], HRwomen, low, diabetes, cere = 11.90 [95% CI 6.98, 16.82]) and low education + type 2 diabetes + psychiatric diseases (HRmen, low, diabetes, psyc = 16.09 [95% CI 9.66, 22.53], HRwomen, low, diabetes, psyc = 15.43 [95% CI 9.69, 21.17]).
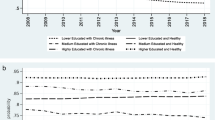
Decomposition of disability pension cases ascribed to main and interaction effects (Fig. 1a,b) for both men and women showed that lower level of education, diagnosis with type 2 diabetes and comorbidities independently contributed to extra cases of disability pension. Except for cancer among men, a higher number of cases was therefore seen for any extra exposure present.
Joint absolute effects model in (a) men and (b) women. Number of extra cases (RD) of disability pension (per 10,000 person-years) from main effects and interaction between education (stratified as high, medium and low level of education), type 2 diabetes and six comorbidities, compared with a healthy reference group. Cerebro., cerebrovascular disease; Musculo., musculoskeletal disease; Psych., psychiatric disease; Ref., reference group; Respira., respiratory disease; T2D, type 2 diabetes mellitus
Overall, the number of cases among people with multiple exposures (low/medium education, type 2 diabetes and comorbidity) exceeded the sum of their main effects, referred to as the excess cases due to interaction. For example, among men with low education and type 2 diabetes only, the absolute RD was 174 (95% CI 164, 184) disability pension cases per 10,000 person-years; 58 cases from low education, 51 cases from type 2 diabetes and 65 cases due to interaction. The joint effect of type 2 diabetes and low education thus exceeded the main effects of type 2 diabetes and low education.
The pattern of interaction varied between men and women. Among women across all comorbidities, except for cancer, those with low compared with medium and high education had a higher rate of disability pension cases due to interaction. Among men, the same pattern was only seen concerning comorbidities with a lower total rate of disability pension (all excluding cerebrovascular and psychiatric diseases).
Discussion
This study presents the interplay between educational level, type 2 diabetes and the six most common comorbidities for the risk of being granted disability pension. The results show that the excess probability of being granted disability pension among people with lower education is partly ascribed to an enhanced risk from type 2 diabetes and comorbidities.
Among women with lower education, a particularly high number of disability pension cases were due to interaction. This was also true for men regarding comorbidity with lower total rate of disability pension (CVD, respiratory disease, musculoskeletal disease and cancer). These excess cases of disability pension cannot be explained by the lower education in itself. Indeed, the results show that the higher number of total cases of disability pension among those with lower education is caused by a synergistic effect of the three exposures.
The results of this paper emphasise the importance of timely diagnosis and early preventative interventions to reduce complications related to type 2 diabetes and comorbidities. The results also suggest that people with type 2 diabetes and comorbidity have the potential to benefit from integrated care. Integrated care refers to the situation where ‘the search [is] to connect the healthcare system (acute, primary medical, and skilled) with other human service systems (e.g. long-term care and housing services) in order to improve outcomes’ [21]. This definition includes both vertical integration across different levels of healthcare, e.g. across acute, primary and specialised healthcare, and horizontal integration encompassing the care provided at the same level, e.g. across hospital departments and between community-based health and social care [22]. Hessler et al describe a theoretical framework consisting of two ways in which individual social risks can guide horizontal integration: by social risk-informed care ‘It can help providers modify care recommendations to accommodate social risks and tailor clinical plans to reduce the impact of social or economic adversity without necessarily targeting the social condition itself’ and by social risk-targeted care ‘social risk factors can serve as the target of interventions that seek to reduce or address the risk factor directly (e.g., through navigation services or linkages with community resources)’ [23].
In the UK, integrated diabetes care means vertical integration between primary, community and specialist care. The delivery of integrated care is facilitated by integration of the processes, methods and tools that enable patients to move between services according to need [24]. Similar aspirations are embedded in the Danish healthcare system, e.g. with the implementation of DMPs for chronic diseases [1, 25]. While the organisational structure of vertical integration has been formalised since 2008 in Denmark, the degree of horizontal integration varies to a large degree between municipalities. Researchers argue that the DMPs still do not provide sufficient assistance to socially disadvantaged patients to navigate the complex healthcare system [26] and this causes social inequality in quality and provision of care. Patients with type 2 diabetes and with lower education constitute a vulnerable group and enhanced horizontal integration of care may be a means to slow disease progression, improve working ability and prevent early exit from the labour market.
Strengths and limitations
This longitudinal cohort study was based on people aged 40–59 years, and covered a total of 17,754,788 person-years. A strength of the study is that all data were extracted from the Danish nationwide registers that generally have high validity and cover the entire Danish population. The quality of the data on diseases therefore primarily relies on the accuracy of the reporting and the coding practices. These reporting biases are general to all diagnosing in healthcare and the positive predictive value may therefore differ according to disease, patient and general practitioner characteristics. In order to increase the power of the study, we let people contribute with person time at risk in different disease groups as they developed over time. The development of multimorbidity is complex and is characterised by various coupling and feedback interactions in certain disease groups. The causal mechanisms of disability pension from coexisting diseases and education are therefore beyond the scope of this paper.
The large size of the study population allowed us to assess the effects of subgroups of type 2 diabetes patients by the six most common comorbidity diagnoses. The remaining diseases were combined into one ‘other diseases’ category. Due to the relatively low number of people with these diseases individually, we chose not to assess the joint effects with type 2 diabetes, but instead created a binary variable (‘yes’/‘no’ other disease[s]) and included it as a potential confounder in the statistical analyses. In order to study subgroups including these other diseases, an outcome with higher frequency such as sick leave or retirement age could be studied to obtain sufficient power. We used information from hospital registers for categorisation of comorbidity. Disease prevalence such as for many psychiatric and musculoskeletal diseases will most likely be under reported. In order to make comparisons between diseases more reliable, we decided only to use hospital records regarding comorbidity, although we had access to information on prescription of medication.
The joint reference category allowed us to compare each combination of type 2 diabetes and the six most common comorbidities according to the same baseline hazard. We evaluated the interaction as departure from additivity in absolute terms, which is more relevant from a public health perspective. A recent review concluded [10] that there is no consensus as to how to handle the effects of comorbidity when the aim is to assess the effects of diabetes on an outcome of interest. Previous studies have either stratified the population in subgroups according to common comorbidity diseases or treated comorbid diseases as confounders [10]. Both of these statistical methods calculate estimated results that are likely to be interpreted incorrectly and often diverge greatly from the results of interest.
This large, population-wide study showed that the joint effects of type 2 diabetes, lower education and comorbidity were associated with larger than additive rates of disability pension. An integrated care approach that takes into account socioeconomic barriers to type 2 diabetes rehabilitation may prevent disease progression and increase the working ability of socially disadvantaged people.
Abbreviations
- CRS:
-
Civil Registration System
- DMP:
-
Disease management programme
- DNDR:
-
Danish National Diabetes Register
- DNPR:
-
Danish National Prescription Registry
- ISCED:
-
International Standard Classification of Education
- RD:
-
Rate difference
References
Danish Health Authority (2008) Forløbsprogrammer for kronisk sygdom – generisk model og forløbsprogram for diabetes. Available from https://www.sst.dk/~/media/5C35B9DEA91B4E0A91458076F1994019.ashx. Accessed 4 Aug 2021
Rijken M, Hujala A, van Ginneken E, Melchiorre MG, Groenewegen P, Schellevis F (2018) Managing multimorbidity: profiles of integrated care approaches targeting people with multiple chronic conditions in Europe. Health Policy 122(1):44–52. https://doi.org/10.1016/j.healthpol.2017.10.002
Nolte E, Knai C, Saltman RB, European Observatory on Health Systems and Policies, World Health Organization, Seventh Framework Programme (European Commission) (2014) Assessing chronic disease management in European health systems: concepts and approaches. Available from http://www.ncbi.nlm.nih.gov/books/NBK458642/. Accessed 4 Aug 2021
Schiøtz ML, Stockmarr A, Høst D, Glümer C, Frølich A (2017) Social disparities in the prevalence of multimorbidity – a register-based population study. BMC Public Health 17(1):422. https://doi.org/10.1186/s12889-017-4314-8
Møller SP, Laursen B, Johannesen CK, Tolstrup JS, Schramm S (2020) Patterns of multimorbidity and demographic profile of latent classes in a Danish population-a register-based study. PLoS One 15(8):e0237375. https://doi.org/10.1371/journal.pone.0237375
Nowakowska M, Zghebi SS, Ashcroft DM et al (2019) The comorbidity burden of type 2 diabetes mellitus: patterns, clusters and predictions from a large English primary care cohort. BMC Med 17(1):145. https://doi.org/10.1186/s12916-019-1373-y
Kristensen MAT, Guassora AD, Arreskov AB, Waldorff FB, Hølge-Hazelton B (2018) ‘I’ve put diabetes completely on the shelf till the mental stuff is in place’. How patients with doctor-assessed impaired self-care perceive disease, self-care, and support from general practitioners. A qualitative study. Scand J Prim Health Care 36(3):342–351. https://doi.org/10.1080/02813432.2018.1487436
Frølich A, Ghith N, Schiøtz M, Jacobsen R, Stockmarr A (2019) Multimorbidity, healthcare utilization and socioeconomic status: a register-based study in Denmark. PLoS One 14(8):e0214183. https://doi.org/10.1371/journal.pone.0214183
Walker RJ, Gebregziabher M, Martin-Harris B, Egede LE (2015) Understanding the influence of psychological and socioeconomic factors on diabetes self-care using structured equation modeling. Patient Educ Couns 98(1):34–40. https://doi.org/10.1016/j.pec.2014.10.002
Pedron S, Emmert-Fees K, Laxy M, Schwettmann L (2019) The impact of diabetes on labour market participation: a systematic review of results and methods. BMC Public Health 19(1):25. https://doi.org/10.1186/s12889-018-6324-6
Sundstrup E, Jakobsen MD, Mortensen OS, Andersen LL (2017) Joint association of multimorbidity and work ability with risk of long-term sickness absence: a prospective cohort study with register follow-up. Scand J Work Environ Health 43(2):146–154. https://doi.org/10.5271/sjweh.3620
Nexø MA, Pedersen J, Cleal B, Bjorner JB (2020) Increased risk of long-term sickness absence, lower rate of return to work and higher risk of disability pension among people with type 1 and type 2 diabetes mellitus: a Danish retrospective cohort study with up to 17 years’ follow-up. Diabet Med 37(11):1861–1865. https://doi.org/10.1111/dme.14203
Kildemoes HW, Sørensen HT, Hallas J (2011) The Danish National Prescription Registry. Scand J Public Health 39(7 Suppl):38–41. https://doi.org/10.1177/1403494810394717
Carstensen B, Kristensen JK, Marcussen MM, Borch-Johnsen K (2011) The National Diabetes Register. Scand J Public Health 39(7 Suppl):58–61. https://doi.org/10.1177/1403494811404278
Jensen VM, Rasmussen AW (2011) Danish education registers. Scand J Public Health 39(7 Suppl):91–94. https://doi.org/10.1177/1403494810394715
Carstensen B, Rønn PF, Jørgensen ME (2020) Prevalence, incidence and mortality of type 1 and type 2 diabetes in Denmark 1996–2016. BMJ Open Diabetes Res Care 8(1):e001071. https://doi.org/10.1136/bmjdrc-2019-001071
Baadsgaard M, Quitzau J (2011) Danish registers on personal income and transfer payments. Scand J Public Health 39(7 Suppl):103–105. https://doi.org/10.1177/1403494811405098
Pedersen CB (2011) The Danish Civil Registration System. Scand J Public Health 39(7 Suppl):22–25. https://doi.org/10.1177/1403494810387965
Martinussen T, Vansteelandt S, Gerster M, von Bornemann Hjelmborg J (2011) Estimation of direct effects for survival data by using the Aalen additive hazards model. J R Stat Soc Ser B Stat Methodol 73(5):773–788
Rod NH, Lange T, Andersen I, Marott JL, Diderichsen F (2012) Additive interaction in survival analysis: use of the additive hazards model. Epidemiology 23(5):733–737. https://doi.org/10.1097/EDE.0b013e31825fa218
Leutz WN (1999) Five laws for integrating medical and social services: lessons from the United States and the United Kingdom. Milbank Q 77(1):77–110. https://doi.org/10.1111/1468-0009.00125
European Commission (2017) Blocks: tools and methodologies to assess integrated care in Europe. Publications Office of the European Union, Luxembourg. https://doi.org/10.2875/69305
Hessler D, Bowyer V, Gold R, Shields-Zeeman L, Cottrell E, Gottlieb LM (2019) Bringing social context into diabetes care: intervening on social risks versus providing contextualized care. Curr Diab Rep 19(6):1–7. https://doi.org/10.1007/s11892-019-1149-y
Diabetes UK (2014) Improving the delivery of adult diabetes care through integration. Available from https://www.diabetes.org.uk/professionals/position-statements-reports/integrated-diabetes-care. Accessed 4 Aug 2021
Vrangbæk K (2020) Structuring complexity? – implementation of a disease management program for type II diabetes care in Denmark. Health Economics Policy and Law (in press)
Rudkjøbing A, Olejaz M, Birk HO, Nielsen AJ, Hernández-Quevedo C, Krasnik A (2012) Integrated care: a Danish perspective. BMJ 345:e4451. https://doi.org/10.1136/bmj.e4451
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Author information
Authors and Affiliations
Contributions
AMB conducted the analysis and was responsible for writing the manuscript. All authors were involved in the conception and design of the study. All authors discussed data analyses, critically revised the manuscript and approved the final version of the manuscript. AMB is responsible for the integrity of the work as a whole.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM
(PDF 107 kb)
Rights and permissions
About this article
Cite this article
Bender, A.M., Vrangbæk, K., Lange, T. et al. Joint effects of educational attainment, type 2 diabetes and coexisting morbidity on disability pension: results from a longitudinal, nationwide, register-based study. Diabetologia 64, 2762–2772 (2021). https://doi.org/10.1007/s00125-021-05559-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-021-05559-4