Abstract
Background
Despite the extensive administration of the enhanced recovery after surgery (ERAS) program, postoperative pain remains a major concern for patients. Transversus abdominis plane (TAP) block and local wound infiltration (LWI) are two techniques that have been widely applied in abdominal surgery. However, these two techniques have rarely been compared in terms of their analgesic effects on patients that undergo laparoscopic colorectal surgery with the ERAS program.
Methods
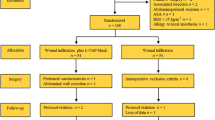
A randomized, double-blinded study was conducted in this study. Briefly, 174 patients that underwent colorectal surgery with the ERAS program were randomly allocated to TAP block treatment (TAP group) or local wound infiltration (LWI group). All patients were assessed for their pain scores at rest and in motion at 6, 24, 48, and 72 h after surgery. The administration frequency of bolus for PCIA and the use amount of rescue analgesics (parecoxib) were recorded. Finally, the patients were monitored with follow-up surveys on their postoperative function recovery, complications, lengths of stay, treatment cost, and satisfaction.
Results
In terms of the pain scores at rest and in motion, the two groups revealed no significant difference throughout the study sessions, and no difference was found in the administration frequency of bolus and the use amount of parecoxib. Moreover, the two groups demonstrated similar results in their postoperative recovery, and no significant differences were found in terms of postoperative complications.
Conclusions
Compared with local wound infiltration, transversus abdominis plane block is not significantly advantageous for postoperative pain control and recovery in patients undergoing laparoscopic colorectal surgery with the ERAS program. However, local wound infiltration might be preferred since it is available with less technical difficulties.

Similar content being viewed by others
References
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021.
ERAS Compliance Group. The Impact of Enhanced Recovery Protocol Compliance on Elective Colorectal Cancer Resection: Results From an International Registry. Ann Surg. 2015. 261(6): 1153-9.
Spanjersberg WR, van Sambeeck JD, Bremers A, Rosman C, van Laarhoven CJ. Systematic review and meta-analysis for laparoscopic versus open colon surgery with or without an ERAS programme. Surg Endosc. 2015. 29(12): 3443-53.
Arık E, Akkaya T, Ozciftci S, Alptekin A, Balas Ş. Unilateral transversus abdominis plane block and port-site infiltration : Comparison of postoperative analgesic efficacy in laparoscopic cholecystectomy. Anaesthesist. 2020. 69(4): 270-276.
Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001. 56(10): 1024-6.
Keller DS, Ermlich BO, Delaney CP. Demonstrating the benefits of transversus abdominis plane blocks on patient outcomes in laparoscopic colorectal surgery: review of 200 consecutive cases. J Am Coll Surg. 2014. 219(6): 1143-8.
Conaghan P, Maxwell-Armstrong C, Bedforth N, et al. Efficacy of transversus abdominis plane blocks in laparoscopic colorectal resections. Surg Endosc. 2010. 24(10): 2480-4.
Meyer LA, Corzo C, Iniesta MD, et al. A prospective randomized trial comparing liposomal bupivacaine vs standard bupivacaine wound infiltration in open gynecologic surgery on an enhanced recovery pathway. Am J Obstet Gynecol. 2021. 224(1): 70.e1-70.e11.
Sellami M, Feki S, Triki Z, et al. Bupivacaine wound infiltration reduces postoperative pain and analgesic requirement after thyroid surgery. Eur Arch Otorhinolaryngol. 2018. 275(5): 1265-1270.
Yu N, Long X, Lujan-Hernandez JR, Succar J, Xin X, Wang X. Transversus abdominis-plane block versus local anesthetic wound infiltration in lower abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2014. 14: 121.
Rashid A, Gorissen KJ, Ris F, et al. No benefit of ultrasound-guided transversus abdominis plane blocks over wound infiltration with local anaesthetic in elective laparoscopic colonic surgery: results of a double-blind randomized controlled trial. Colorectal Dis. 2017. 19(7): 681-689.
Park JS, Choi GS, Kwak KH, et al. Effect of local wound infiltration and transversus abdominis plane block on morphine use after laparoscopic colectomy: a nonrandomized, single-blind prospective study. J Surg Res. 2015. 195(1): 61-6.
Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 2011;63 Suppl 11:S240-52.
Glickman ME, Rao SR, Schultz MR. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J Clin Epidemiol 2014;67(8):850-7.
McNeill JA, Sherwood GD, Starck PL, Thompson CJ. Assessing clinical outcomes: patient satisfaction with pain management. J Pain Symptom Manage. 1998. 16(1): 29-40.
Ren K, Dubner R. Interactions between the immune and nervous systems in pain. Nat Med. 2010. 16(11): 1267-76.
Levy BF, Scott MJ, Fawcett W, Fry C, Rockall TA. Randomized clinical trial of epidural, spinal or patient-controlled analgesia for patients undergoing laparoscopic colorectal surgery. Br J Surg. 2011. 98(8): 1068-78.
Lee SW. Laparoscopic procedures for colon and rectal cancer surgery. Clin Colon Rectal Surg. 2009. 22(4): 218-24.
Hermanides J, Hollmann MW, Stevens MF, Lirk P. Failed epidural: causes and management. Br J Anaesth. 2012. 109(2): 144-54.
Woolf CJ. Evidence for a central component of post-injury pain hypersensitivity. Nature 1983;306(5944):686-8.
Xia J, Paul Olson TJ, Tritt S, Liu Y, Rosen SA. Comparison of preoperative versus postoperative transversus abdominis plane and rectus sheath block in patients undergoing minimally invasive colorectal surgery. Colorectal Dis 2020;22(5):569-80.
Møiniche S, Kehlet H, Dahl JB. A qualitative and quantitative systematic review of preemptive analgesia for postoperative pain relief: the role of timing of analgesia. Anesthesiology 2002;96(3):725-41.
Escudero-Fung M, Lehman EB, Karamchandani K. Timing of Transversus Abdominis Plane Block and Postoperative Pain Management. Local Reg Anesth 2020;13:185-93.
Amr YM, Amin SM. Comparative study between effect of pre- versus post-incisional transversus abdominis plane block on acute and chronic post-abdominal hysterectomy pain. Anesth Essays Res 2011;5(1):77-82.
Shim JW, Ko J, Lee CS, et al. Better timing of ultrasound-guided transversus abdominis plane block for early recovery after open inguinal herniorrhaphy: A prospective randomised controlled study. Asian J Surg 2021;44(1):254-61.
Gan TJ, Diemunsch P, Habib AS, et al. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2014. 118(1): 85-113.
Jr GS, Fitzgerald P, Ahmad S, Kim J, Rahangdale R, McCarthy R. Transversus abdominis plane infiltration for laparoscopic gastric banding: A pilot study. World J Gastrointest Surg. 2014. 6(2): 27-32.
De Oliveira GS, Castro-Alves LJ, Nader A, Kendall MC, McCarthy RJ. Transversus abdominis plane block to ameliorate postoperative pain outcomes after laparoscopic surgery: a meta-analysis of randomized controlled trials. Anesth Analg. 2014. 118(2): 454-63.
Hayden JM, Oras J, Karlsson OI, Olausson KG, Thörn SE, Gupta A. Post-operative pain relief using local infiltration analgesia during open abdominal hysterectomy: a randomized, double-blind study. Acta Anaesthesiol Scand. 2017. 61(5): 539-548.
Pedrazzani C, Menestrina N, Moro M, et al. Local wound infiltration plus transversus abdominis plane (TAP) block versus local wound infiltration in laparoscopic colorectal surgery and ERAS program. Surg Endosc. 2016. 30(11): 5117-5125.
Kline RH 4th, Wiley RG. Spinal mu-opioid receptor-expressing dorsal horn neurons: role in nociception and morphine antinociception. J Neurosci 2008;28(4):904-13.
Johnson Q, Borsheski RR, Reeves-Viets JL. Pain management mini-series. Part I. A review of management of acute pain. Mo Med 2013;110(1):74–9.
Scott LJ, Perry CM. Tramadol: a review of its use in perioperative pain. Drugs. 2000. 60(1): 139-76.
Erolçay H, Yüceyar L. Intravenous patient-controlled analgesia after thoracotomy: a comparison of morphine with tramadol. Eur J Anaesthesiol. 2003. 20(2): 141-6.
Acknowledgements
The authors gratefully acknowledge Dr. Lihua Peng, Ph.D., of the Department of Anesthesiology, the First Affiliated Hospital of Chongqing Medical University, for providing helpful advice of methodology.
Funding
This study was supported by the funding of nation guiding local technology development project (2018–35).
Author information
Authors and Affiliations
Contributions
Li Ren contributed to protocol development, data analysis, and manuscript writing. Peipei Qin participated in the data collection and analysis. Su Min contributed to protocol development and manuscript editing. Wenjian Wang and Juying Jin participated in the data collection.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ren, L., Qin, P., Min, S. et al. Transversus Abdominis Plane Block Versus Local Wound Infiltration for Postoperative Pain After Laparoscopic Colorectal Cancer Resection: a Randomized, Double-Blinded Study. J Gastrointest Surg 26, 425–432 (2022). https://doi.org/10.1007/s11605-021-05121-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-05121-y