Abstract
Background
The Human T-lymphotropic virus (HTLV) is a retrovirus of the genus Deltaretrovirus, which belongs to the family Retroviridae. The most important types are HTLV-1 and HTLV-2. It is estimated that between five and 10 million individuals are infected with HTLV-1, worldwide. Studies in the state of Pará indicate that it has the third highest prevalence of HTLV infections of any Brazilian state. The present study describes the epidemiological, serological, and molecular profile of blood donors from the state of Pará that were classified as unfit due to infection by HTLV-1 and 2.
Methods
The present study is based on a descriptive, retrospective, and cross-sectional review of the epidemiological, serological, and molecular data on blood donations, between January 2015 and December 2019. The data were obtained from the blood bank system and were digitalized to form a database in the Statistical Package for Social Sciences program, version 20. Descriptive statistics were used to determine the absolute and relative frequencies of the qualitative variables. For the quantitative variables, the mean, standard deviation, and minimum and maximum values were calculated. A p < 0.05 significance level was adopted for all analyses.
Results
A total of 632 samples were analyzed, of which 496 (78%) had no detectable proviral DNA and 136 (22%) had detectable HTLV. The HTLV-1 was detected in most (78%; 106/136) of these samples, while only 30 (22%) were detected for HTLV-2. The HTLV proviral DNA was detected primarily in females (69.1%), with a mean age of 40 years, with the highest frequencies of detection being recorded in single individuals (66.2%), first-time donors (74.3%), and individuals that had graduated high school (44.1%). The molecular confirmation of HTLV showed that three-quarters (78%) of the serologically reactive individuals were negative for either types 1 or 2, so the epidemiological profile of these individuals was significantly different from their detectable profile.
Conclusions
The HTLV is neglected in Brazil; there is thus a clear need for further research in the area of regional hemotherapy and hematology services, in order to contribute to the definition of regional infection profiles, that will be fundamental to the development of effective prophylactic practices for the prevention of the infection and the dissemination of knowledge on the dangers of HTLV in the community.
Similar content being viewed by others
Background
The Human T-lymphotropic virus (HTLV) is a retrovirus of the genus Deltaretrovirus, which belongs to the family Retroviridae [1] and has tropism for T lymphocytes, with four types, HTLV-1, HTLV-2, HTLV-3, and HTLV-4. The HTLV-1 is the most relevant pathogen, being associated with severe diseases, such as tropical spastic paraparesis/HTLV-1-associated myelopathy (HAM/TSP) and adult T-cell lymphoma/leukemia (ATLL), while the HTLV-2 is also epidemiologically important, but is not associated systematically with other pathologies [2,3,4].
The estimated number of individuals infected with HTLV-1 worldwide is between five and 10 million [5], with the most prevalent regions being Japan, Africa, the Caribbean islands, and Central and South America. In Brazil, the number of individuals infected with HTLV-1 is estimated to be approximately 2.5 million, with a lower prevalence in the south of the country, increasing toward the northern and northeastern regions [6]. The northern Brazilian state of Pará is ranked third in the prevalence of HTLV in the country’s states [7].
The routes of infection by HTLV-1 and 2 include the sexual route, most commonly from man to woman, vertical transmission, which is the most frequent route, mainly through breastfeeding, and the parenteral route, through the transfusion of contaminated blood elements, the most efficient transmission route [8,9,10]. In Brazil, like the rest of the world, hemotherapy has evolved in recent years through the introduction of new technologies that minimize the risks of blood transfusion, in particular through the prevention of the dissemination of infectious agents. Screening for HTLV in blood banks became mandatory in Brazil, in November 1993, through ordinance no. 1376 of the Brazilian Ministry of Health [8].
The present study describes the epidemiological, serological, and molecular profile of blood donors from Pará classified as inapt due to infection by HTLV-1 and 2. The definition of the infection profile of the blood donors from this state represents an importance advance in the understanding of infection patterns in Brazil, especially considering the major regional variation found in this country in socioeconomic, demographic, and cultural conditions, which may all influence the epidemiology of HTLV, which will be fundamental to the development of effective prophylactic practices for the country-wide combat of the infection.
Methods
The present study was approved by the FIBRA Committee for Ethics in Research through protocol number CAAE 19,004,819.7.0000.8187 and was conducted at the Pará State Center for Hematology and Hemotherapy (HEMOPA), which has 10 blood donation centers, including its headquarters, in the state capital, Belém. The other centers are located in the towns of Ananindeua and Castanhal, in northern Pará, the city of Santarém, in western Pará, Marabá, Redenção, and Tucuruí, in the southeast of the state, Abatetuba and Capanema in the northeast, and Altamira, in the southwest.
The present study is based on a descriptive, retrospective, and cross-sectional review of the epidemiological, serological, and molecular data on blood donations, between January 2015 and December 2019. As inclusion criteria, the selected data of subjects were those who were over eighteen years and had samples considered as reactive on the serological screening and were sent to the confirmatory detection, by molecular biology. As exclusion criteria, subjects younger than 18 years and samples that did not presented results for one of the tests have not been used in the research.
In the period of study, the HEMOPA foundation performed the serological screening using chemiluminescent microparticle immunoassay (CMIA), making use of the ARCHITECH rHTLV-I/II platform, with sensitivity value of 100% and specificity of 99.95%, according to manufacturer. The confirmatory test that was performed in the study period was the real-time polymerase chain reaction (qPCR) method, using the TaqMan® (AppliedBiosystems) system, which consists of three targets, the albumin gene and the non-homologous regions of the HTLV-1 and HTLV-2 pol gene, being a highly specific test.
The data were obtained for the present study from the blood bank system (SBS and SBS web) and were digitalized to form a database in the Statistical Package for Social Sciences (SPSS) program, version 20. This database included information on the sex, age, geographical origin, education level, marital status, ethnic classification (self-defined), the type of donor and donation, the quantity of donations, and the results of the serological testing (chemiluminescence) and qPCR.
Descriptive statistics were used to determine the absolute and relative frequencies of the qualitative variables. For the quantitative variables, the mean, standard deviation, and minimum and maximum values were calculated, according to the characteristics of each study variable. These means were compared between groups using Student’s t, while the Chi-Square test of independence was applied to the qualitative variables. A p ≤ 0.05 significance level was adopted for all analyses.
Results
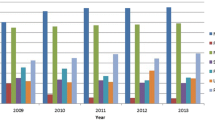
A total of 453,626 blood donations were screened serologically in the state of Pará between January 2015 and December 2019. Overall, 1476 (0.3%) of these donations were found to be inapt due to the serological detection of HTLV, and 747 (51%) of these samples were submitted to a confirmatory test for HTLV-1 and 2 proviral DNA by real-time PCR. A total of 115 samples were omitted from the analyses due to the fact that they did not satisfy the selection criteria for the study population. The data on 632 samples were thus analyzed, of which 496 (78%) had no detectable proviral DNA and 136 (22%) had detectable HTLV. The HTLV-1 was detected in most (78%; 106/136) of these samples, while only 30 (22%) were detected for HTLV-2. The presence or the absence of proviral DNA was the basic criterion for the comparative analyses, that is, between detectable and undetectable groups (Table 1).
The epidemiological profile of the samples confirmed with proviral DNA for HTLV-1 or 2 by qPCR included a predominance of female individuals (69.1%; 94/136) and individuals that were single, divorced, or widowed (66.2%; 90/136) in comparison with married individuals. The mean age was 40.08 ± 12.07 years old, with a minimum of 18 years and a maximum of 65 years, and a peak in the 36–46 year age class (Table 2), which contained almost a third (30.9%: 42/136) of the group.
Regarding the geographic region, most of the detectable samples (69.1%; 94/136) were from the Belém metropolitan region (Ananindeua, Belém, Benevides, Castanhal, Marituba, Santa Bárbara do Pará e Santa Izabel do Pará), while just 30.9% (42/136) were detected from other regions (inland) of the state, although the highest detection frequency was in the metropolitan area, there were no statistically significant difference (p = 0.600). High school graduates made up the largest group of detectable donors (44.1%; 60/130), followed by individuals that did not graduate from elementary school (14.7%; 20/136). The vast majority of the detectable donors (79.4%; 108/136) also declared themselves to be of the brown ethnicity, followed by the white ethnicity, being 16.9% (23/136).
Almost three-quarters (74.3%; 101/136) of the individuals with detectable proviral DNA were first-time donors, while 17.6% (24/136) were sporadic donors, and 8.1% (11/136), repeat donors. The mean number of donations provided by the sporadic donors was 6.17 ± 6.86, while it was 9.45 ± 5.82 by the repeat donors. The vast majority of donations (69.1%; 4/136) were spontaneous.
The inapt blood donors with detectable HTLV were significantly older (p < 0.0001), on average (40.08 ± 12.07 years old) than those with undetectable HTLV (32.93 ± 9.96 years old). The proportion of female donors was also significantly higher (p < 0.0001) in the detectable group, in comparison with the undetectable group. The proportion of first-time donors was also significantly higher (p < 0.0001) in the detectable group, while the sporadic and repeat donors predominated in the undetectable group.
In both groups, almost half of all donors were high school graduates, but whereas 37.5% of the detectable group had a lower education level; this was true of only 22.2% of the undetectable group. No association was found between the presence or absence of detectable HTLV proviral DNA and marital status, geographic origin, ethnicity, or the type of donation.
The comparative analysis between the HTLV-1 and HTLV-2 profiles presented a very similar profile among viruses; there were no statistically differences between the variables of sex, age, marital status, educational level, ethnicity, and type of blood donation. However, the qualitative variables’ origin of donor and type of donor presented a statistical difference between groups, being the HTLV-1 detection more frequent (80.2%; 85/106) than the detection for HTLV-2 (53.3%; 16/30) in first-time donors (p = 0.016), just like the origin from the metropolitan region in which HTLV-1 was 64.2% (68/106) and HTLV-2 was 83.3% (25/30) (p = 0.046).
Discussion
The prevalence of HTLV varies according to sociodemographic factors, geographic region, and individual risk behavior. However, no epidemiological studies have yet demonstrated the real prevalence of HTLV in Brazil as a whole. Previous studies in the state of Pará have focused on specific groups, such as pregnant women [11, 12], riverside communities [13], indigenous populations [14, 15], and blood donors [7].
A study of blood donors from donation centers in the 27 Brazilian state capitals, between 1995 and 2000, demonstrated a heterogeneous distribution of HTLV in Brazil, and estimated a seroprevalence of 0.9% in the state of Pará [7]. The much lower seroprevalence, of 0.3%, recorded in the present study, indicates a reduction in infection rates over the 15 years between the two studies, which may reflect changes in the behavior of the population in recent years, in relation to the prevention of sexually transmitted infections. However, the difference between the studies may also have been determined, at least in part, by methodological differences, since the sensitivity and the specificity of the screening tests are associated to the methodology, antigens used, detected antibody class, and the studied population.
In the study realized by Catalan-Soares, Carneiro-Proietti, and Proietti [7], the serological screening was performed using the third generation enzyme immunoassay (EIA) methodology (100% sensitivity and 92.0% specificity [16, 17]), which uses synthetic and/or recombinant specific peptides for HTLV-1/2 (gp46-I; gp46-II; rgp21-HTLV-2), the methodology used in this study was chemiluminescence (CMIA), which uses paramagnetic microparticles coated with HTLV-1 synthetic peptide (gp46) and HTLV-2 recombinant antigen (rgp21). Besides that, the 2005 study does not describe the total donations collected in the state of Pará blood center for the prevalence calculation. Furthermore, seroprevalence was only calculated with the number of donations from the metropolitan region of the state, and in the present study, information was collected from donors all over the state of Pará.
In this study, the detection of proviral DNA in only 22% of the samples, tested by qPCR, reinforces the need to use confirmatory tests allowing to define the real HTLV infection status and the discrimination between HTLV-1 and HTLV-2 infections on the countless inapt donors. Such knowledge will most likely help on the care, counseling, and handling of the donor [18].
The screening tests in blood banks have high sensitivity values, aiming at the exclusion of possibly virus-infected samples, having low positive predictive value, and that can lead to high proportions of false-positive results. Although the latest generation serological screening tests have high specificity, close to 100%, when addressed in populations at low risk for sexually transmitted infections, such as blood donors, it shows very low predictive value [19]. The cross-reactions to other virus antibodies are strongly associated to multiple false-positive results in the viral antibody screening test [20]. Otherwise, undetectable results in molecular assays have been associated to low proviral load [21, 22].
In the donors in which either HTLV-1 or 2 was detected by molecular testing, HTLV infection was more prevalent in females and in middle-aged (36–46 years old) individuals. A similar pattern has been recorded in many previous studies [5, 23], which indicate a prevalence in females and older individuals, which may be related to the greater efficiency of the sexual transmission from man to woman and the increasing number of sexual encounters accumulated over the lifetime of the individual [6, 24]. The lower educational level, in general, of the individuals in the detectable group may reflect their reduced access to information on basic health, in general, and on the prevention of sexually transmissible infections, in particular [6, 25]. Unmarried individuals (single, divorced, widowed) predominated in both donor groups, which may be related to a greater exposure to the risk of sexual transmission, being associated with unprotected sex and multiple sexual partners [26, 27].
In Brazil, a considerable proportion of the potential blood donor population believes that blood banks are a convenient place for free testing for infections, and may thus not reveal their risky behavior at the clinical screening. This may have contributed to the fact that the number of detections was significantly higher among first-time donors. By contrast, regular donors, who are tested every time they donate blood, are likely to be a low risk group for infection [8, 28, 29].
In the present study, the profile (sex, age, education, and type of donor) of the donors varied considerably between in the groups in which the HTLV-1 or 2 proviral DNA was detected or not (undetectable). This indicates that the candidates for blood donation that were seropositive for HTLV had a distinct profile from those in which HTLV-1 or 2 was confirmed by qPCR. This difference may be related to the differential sensitivity and specificity of the screening and confirmatory tests, resulting in distinct outcomes between the two groups.
In relation to the comparison to HTLV-1 and HTLV-2 profiles, the statistical difference found in the variables origin of donor and type of donor can be related to the fact that HTLV-1 had a higher frequency in the studied population. This significantly higher frequency of HTLV-1 in the population is also seen in other studies carried out in Brazil [3, 29].
Conclusions
The epidemiological profile recorded here is highly similar to that found in previous studies, with a predominance of infection in woman, a mean age of approximately 40 years, and a higher frequency of HTLV detection in unmarried individuals and first-time donors.
Neither HTLV-1 or 2 was detected by qPCR in more than half of the serologically reactive individuals and the epidemiological profile (sex, age, education, and type of donor) of these individuals was significantly different from those in which the presence of HTLV proviral DNA was detected.
The HTLV is a neglected etiological agent in Brazil, and despite the many advances since its discovery, infection patterns are still relatively poorly understood by both healthcare professionals and the general population. There is thus a clear need for further research in the area of regional hemotherapy and hematology services, in order to contribute to the definition of regional infection profiles, that will be fundamental to the development of effective prophylactic practices for the prevention of the infection and the dissemination of knowledge on the dangers of HTLV in the community.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
ICTV—International Commitee on Taxonomy of Viruses. Taxonomy history: primate T-lymphotropic virus 1; 2019. https://talk.ictvonline.org/taxonomy/p/taxonomy-history?taxnode_id=201904999. Acessed 4 Set 2020.
Semeão LES, Roque DR, Sobrinho TF, Costa CKF, Dodorico M, Yamaguchi M (2015) Soroprevalência do vírus linfotrópico de células T humanas (HTLV) entre doadores de sangue em hemocentros de Maringá-Paraná e Boa Vista-Roraima. Epidemiol Serv Saude 24(3):523–529. https://doi.org/10.5123/S1679-49742015000300018
Martinez MP, Al-Saleem J, Green PL (2019) Comparative virology of HTLV-1 and HTLV-2. Retrovirology. https://doi.org/10.1186/s12977-019-0483-0
Futsch N, Mahieux R, Dutartre H (2017) HTLV-1, the other pathogenic yet neglected human retrovirus: from transmission to therapeutic treatment. Viruses. https://doi.org/10.3390/v10010001
Gessain A, Cassar O (2012) Epidemiological aspects and world distribution of HTLV-1 infection. Front Microbiol. https://doi.org/10.3389/fmicb.2012.00388
Glória LM, Damasceno SA, Rodrigues LR, Santos MSB, Medeiros R, Dias GAS, Denise SP (2015) Perfil clínico-epidemiológico de pacientes infectados pelo HTLV-1 em Belém/Pará. Cad Saúde Colet. https://doi.org/10.1590/1414-462X201400050087
Catalan-Soares B, Carneiro-Proietti ABDF, Proietti FA (2005) Heterogeneous geographic distribution of human T-cell lymphotropic viruses I and II (HTLV-I/II): serological screening prevalence rates in blood donors from large urban areas in Brazil. Cad Saude Publica. https://doi.org/10.1590/S0102-311X2005000300027
Pereira GC, Bonafé SM (2018) Soroprevalência para doenças infecto-contagiosas em doadores de sangue da cidade de Maringá. Paraná Revista Uningá 43:1
Eusebio-Ponce E, Anguita E, Paulino-Ramirez R, Candel FJ (2019) HTLV-1 infection: an emerging risk. pathogenesis, epidemiology, diagnosis and associated diseases. Rev Esp Quimioter 6:485–496
Mello MAG, Conceição AF, Sousa SMB, Alcântara LC, Marin LJ, Raiol MRS et al (2014) HTLV-1 in pregnant women from the Southern Bahia, Brazil: a neglected condition despite the high prevalence. Virology Journal. https://doi.org/10.1186/1743-422X-11-28
Sequeira CG, Tamegão-Lopes BP, Santos EJMD, Ventura AMR, Moraes- Pinto MI, Succi RCDM (2012) Descriptive study of HTLV infection in a population of pregnant women from the state of Pará, Northern Brazil. Rev Soc Bras Med Trop 45(4):453–456. https://doi.org/10.1590/S0037-86822012005000007
Guerra AB, Siravenha LQ, Laurentino RV, Feitosa RNM, Azevedo VN, Vallinoto ACR et al (2018) Seroprevalence of HIV, HTLV, CMV, HBV and rubella virus infections in pregnant adolescents who received care in the city of Belém, Pará, Northern Brazil. BMC Pregnancy Childbirth 18(1):169. https://doi.org/10.1186/s12884-018-1753-x
Ferreira LSC, Costa JHG, Costa CA, Melo MFC, Andrade ML, Martins LC et al (2010) Soroprevalência do vírus linfotrópico de células T humanas em comunidades ribeirinhas da região nordeste do Estado do Pará, Brasil. Rev Pan-Amaz Saúde 1:103–108
Ishak R, Harrington WJ, Azevedo VN, Eiraku N, Ishak MOG, Guerreiro JF et al (1995) Identification of human T cell lymphotropic virus type IIa infection in the Kayapo, an Indigenous population of Brazil. AIDS Res Hum Retrovir. https://doi.org/10.1089/aid.1995.11.813
Braço ILJ, de Sá KSG, Waqasi M, Queiroz MAF, da Silva ANR, Cayres-Vallinoto IMV et al (2019) High prevalence of human T-lymphotropic virus 2 (HTLV-2) infection in villages of the Xikrin tribe (Kayapo), Brazilian Amazon region. BMC Infect Dis 19(1):459. https://doi.org/10.1186/s12879-019-4041-0
Silva BVS, Santos FL, Gonçalves NL, Araujo TH, Nascimento DS, Pereira FM et al (2018) Performance of commercially available serological screening tests for human T-cell lymphotropic virus infection in Brazil. J Clin Microbiol. https://doi.org/10.1128/JCM.00961-18
Silva RX, Campos KR, Caterino-de-Araujo A (2020) Pooling of sera for human T-cell lymphotropic virus (HTLV) screening in a time of increasing health care expenditure and limited resources. Rev. Inst. Med. trop. S. Paulo. https://doi.org/10.1590/S1678-9946202062027.
Medeiros ACM, Vidal LRR, Von Linsingen R, Ferin AN, Strapasson TB, Almeida SM, Raboni SM, Carvalho NS, Nogueira MB (2018) Confirmatory molecular method for HTLV-1/2 infection in high-risk pregnant women. J Med Virol. https://doi.org/10.1002/jmv.25014
Brito VS, Santos FLN, Gonçalves NLS, Araujo THA, Nascimento DSV, Pereira FM, Boa-Sorte NCA, Grassi MFR, Caterino-De-Araujo A, Galvão-Castro B (2018) Performance of commercially available serological screening tests for human T-cell lymphotropic virus infection in Brazil. J Clin Microbiol. https://doi.org/10.1128/JCM.00961-18
Simonsen L, Buffington J, Shapiro CN, Holman RC, Strine TW, Grossman BJ, Williams AE, Schonberger LB (1995) Multiple false reactionse in viral antibody screening assays after influenza vaccination. Am J Epidemiol. https://doi.org/10.1093/oxfordjournals.aje.a117374
Campos KR, Gonçalves MG, Costa NA, Caterino-de-Araujo A (2017) Comparative performances of serologic and molecular assays for detecting human T lymphotropic virus type 1 and type 2 (HTLV-1 and HTLV-2) in patients infected with human immunodeficiency virus type 1 (HIV-1). Braz J Infect Dis. https://doi.org/10.1016/j.bjid.2017.02.005
Costa EAS, Magri MC, Caterino-de-Araujo A (2011) The best algorithm to confirm the diagnosis of HTLV-1 and HTLV-2 in at-risk individuals from São Paulo, Brazil. J Virol Methods 173(2):280–6. https://doi.org/10.1016/j.jviromet.2011.02.018
Eshima N, Iwata O, Iwata S, Tabata M, Higuchi Y, Matsuishi, et al (2009) Age and gender specific prevalence of HTLV-1. J Clin Virol. https://doi.org/10.1016/j.jcv.2009.03.012
Silva IC, Pinheiro BT, Nobre AFS, Coelho JL, Pereira CCC, Ferreira LDSC, et al. (2018) Moderada endemicidade da infecção pelo vírus linfotrópico-T humano na região metropolitana de Belém, Pará, Brasil. Rev Bras Epidemiol. https://doi.org/10.1590/1980-549720180018.
Dourado I, Alcântara LCJ, Barreto ML, Teixeira MG, Castro Filho BG (2003) HTLV- I in the general population of Salvador, Brazil: a city with African ethnic and sociodemographic characteristics. J Acquir Immune Defic Syndr 34:527–531
Oliveira EH, Silva FL, Silva ML (2015) Perfil epidemiológico dos doadores de sangue infectados pelo vírus HTLV I/II, no Estado do Piauí. Revista Interdisciplinar 8:149–156
Proietti FA, Carneiro-Proietti ABF, Catalan-Soares BC, Murphy EL (2005) Global epidemiology of HTLV-I infection and associated diseases. Oncogene. https://doi.org/10.1038/sj.onc.1208968
Blatyta PF, Custer B, Gonçalez TT, Birch R, Lopes ME, Ferreira MIL (2013) Undisclosed human immunodeficiency virus risk factors identified through a computer-based questionnaire program among blood donors in Brazil. Transfusion. https://doi.org/10.1111/trf.12166
Morais MPED, Gato CM, Maciel LA, Lalwani P, Costa CA, Lalwani JDB (2017) Prevalence of human T-lymphotropic virus type 1 and 2 among blood donors in Manaus, Amazonas State, Brazil. Rev Inst Med Trop Sao Paulo 21(59):e80. https://doi.org/10.1590/s1678-9946201759080
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Carolina de Alcântara Maneschy and Carlos Eduardo de Melo Amaral. The first draft of the manuscript was written by Renata Bezerra Hermes de Castro, Carolina de Alcântara Maneschy, and Carlos Eduardo de Melo Amaral, and all authors commented on previous versions of the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Faculdade Integrada Brasil Amazônia (FIBRA) Ethics in Human Research Committee number: 3.559.772 (CAAE: 19004819.7.0000.8187).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Responsible Editor: Flavio Guimaraes Fonseca
Rights and permissions
About this article
Cite this article
de Alcantara Maneschy, C., dos Santos Barile, K.A., de Castro, J.A.A. et al. Epidemiological and molecular profile of blood donors infected with HTLV-1/2 in the state of Pará, northern Brazil. Braz J Microbiol 52, 2001–2006 (2021). https://doi.org/10.1007/s42770-021-00609-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42770-021-00609-w