Abstract
Background
Information on whether there is a relationship between hospital volume and bleeding after endoscopic submucosal dissection (ESD) for early gastric cancer (EGC) is limited. This study aimed to compare the bleeding rates after ESD for EGC according to the hospital volume.
Methods
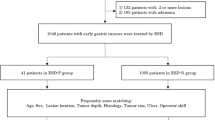
Patients who underwent ESD for EGC at 33 institutions in Japan between November 2013 and October 2016 were included in this multicenter retrospective study. Hospital volume was categorized into three groups, based on the average annual number of ESD procedures: low- and medium-volume group (LMVG), high-volume group (HVG), and very high-volume group (VHVG). The bleeding rate after ESD for EGC was compared between the three hospital volume groups after propensity score matching.
Results
A total of 10,320 patients, including 2797 patients in the LMVG, 4646 patients in the HVG, and 2877 patients in the VHVG, were identified. Propensity score matching yielded 2002 patients in each hospital volume group, with an improved balance of confounding variables between the three groups. The bleeding rates in the LMVG, HVG, and VHVG were 4.3%, 3.7%, and 4.9%, respectively, and no significant difference was noted between the three groups.
Conclusions
The bleeding rate after ESD for EGC did not differ between hospitals in Japan. The finding indicated that ESD for EGC is equally feasible across Japanese hospitals of different volumes regarding bleeding after ESD.


Similar content being viewed by others
References
Liu Q, Ding L, Qiu X, Meng F (2020) Updated evaluation of endoscopic submucosal dissection versus surgery for early gastric cancer: A systematic review and meta-analysis. Int J Surg 73:28–41
Hasuike N, Ono H, Boku N, Mizusawa J, Takizawa K, Fukuda H, Oda I, Doyama H, Kaneko K, Hori S, Iishi H, Kurokawa Y, Muto M (2018) A non-randomized confirmatory trial of an expanded indication for endoscopic submucosal dissection for intestinal-type gastric cancer (cT1a): the Japan Clinical Oncology Group study (JCOG0607). Gastric Cancer 21:114–123
Takizawa K, Ono H, Hasuike N, Takashima A, Minashi K, Boku N, Kushima R, Katayama H, Ogawa G, Fukuda H, Fujisaki J, Oda I, Yano T, Hori S, Doyama H, Hirasawa K, Yamamoto Y, Ishihara R, Tanabe S, Niwa Y, Nakagawa M, Terashima M, Muto M, The Stomach Cancer Study Group of the Japan Clinical Oncology Group (2021) A nonrandomized, single-arm confirmatory trial of expanded endoscopic submucosal dissection indication for undifferentiated early gastric cancer: Japan Clinical Oncology Group study (JCOG1009/1010). Gastric Cancer 24:479–491
Takizawa K, Oda I, Gotoda T, Yokoi C, Matsuda T, Saito Y, Saito D, Ono H (2008) Routine coagulation of visible vessels may prevent delayed bleeding after endoscopic submucosal dissection—an analysis of risk factors. Endoscopy 40:179–183
Akasaka T, Nishida T, Tsutsui S, Michida T, Yamada T, Ogiyama H, Kitamura S, Ichiba M, Komori M, Nishiyama O, Nakanishi F, Zushi S, Nishihara A, Iijima H, Tsujii M, Hayashi N (2011) Short-term outcomes of endoscopic submucosal dissection (ESD) for early gastric neoplasm: multicenter survey by Osaka University ESD study group. Dig Endosc 23:73–77
Lim JH, Kim SG, Kim JW, Choi YJ, Kwon J, Kim JY, Lee YB, Choi J, Im JP, Kim JS, Jung HC, Song IS (2012) Do antiplatelets increase the risk of bleeding after endoscopic submucosal dissection of gastric neoplasms? Gastrointest Endosc 75:719–727
Miyahara K, Iwakiri R, Shimoda R, Sakata Y, Fujise T, Shiraishi R, Yamaguchi K, Watanabe A, Yamaguchi D, Higuchi T, Tominaga N, Ogata S, Tsuruoka N, Noda T, Hidaka H, Mannen K, Endo H, Yamanouchi K, Yamazato T, Sakata H, Fujimoto K (2012) Perforation and postoperative bleeding of endoscopic submucosal dissection in gastric tumors: analysis of 1190 lesions in low- and high-volume centers in Saga, Japan. Digestion 86:273–280
Nishide N, Ono H, Kakushima N, Takizawa K, Tanaka M, Matsubayashi H, Yamaguchi Y (2012) Clinical outcomes of endoscopic submucosal dissection for early gastric cancer in remnant stomach or gastric tube. Endoscopy 44:577–583
Toyokawa T, Inaba T, Omote S, Okamoto A, Miyasaka R, Watanabe K, Izumikawa K, Horii J, Fujita I, Ishikawa S, Morikawa T, Murakami T, Tomoda J (2012) Risk factors for perforation and delayed bleeding associated with endoscopic submucosal dissection for early gastric neoplasms: analysis of 1123 lesions. J Gastroenterol Hepatol 27:907–912
Koh R, Hirasawa K, Yahara S, Oka H, Sugimori K, Morimoto M, Numata K, Kokawa A, Sasaki T, Nozawa A, Taguri M, Morita S, Maeda S, Tanaka K (2013) Antithrombotic drugs are risk factors for delayed postoperative bleeding after endoscopic submucosal dissection for gastric neoplasms. Gastrointest Endosc 78:476–483
Lim SM, Park JC, Lee H, Shin SK, Lee SK, Lee YC (2013) Impact of cumulative time on the clinical outcomes of endoscopic submucosal dissection in gastric neoplasm. Surg Endosc 27:1397–1403
Yoshio T, Nishida T, Kawai N, Yuguchi K, Yamada T, Yabuta T, Komori M, Yamaguchi S, Kitamura S, Iijima H, Tsutsui S, Michida T, Mita E, Tsujii M, Takehara T (2013) Gastric ESD under heparin replacement at high-risk patients of thromboembolism is technically feasible but has a high risk of delayed bleeding: Osaka University ESD Study Group. Gastroenterol Res Pract 2013:365830
Suzuki H, Oda I, Sekiguchi M, Abe S, Nonaka S, Yoshinaga S (2014) Process of technical stabilization of gastric endoscopic submucosal dissection at the National Cancer Center in Japan. Turk J Gastroenterol 25:619–623
Sato C, Hirasawa K, Koh R, Ikeda R, Fukuchi T, Kobayashi R, Kaneko H, Makazu M, Maeda S (2017) Postoperative bleeding in patients on antithrombotic therapy after gastric endoscopic submucosal dissection. World J Gastroenterol 23:5557–5566
Yano T, Tanabe S, Ishido K, Suzuki M, Kawanishi N, Yamane S, Watanabe A, Wada T, Azuma M, Katada C, Koizumi W (2017) Different clinical characteristics associated with acute bleeding and delayed bleeding after endoscopic submucosal dissection in patients with early gastric cancer. Surg Endosc 31:4542–4550
Nam HS, Choi CW, Kim SJ, Kim HW, Kang DH, Park SB, Ryu DG (2019) Risk factors for delayed bleeding by onset time after endoscopic submucosal dissection for gastric neoplasm. Sci Rep 9:2674
Suzuki H, Takizawa K, Hirasawa T, Takeuchi Y, Ishido K, Hoteya S, Yano T, Tanaka S, Endo M, Nakagawa M, Toyonaga T, Doyama H, Hirasawa K, Matsuda M, Yamamoto H, Fujishiro M, Hashimoto S, Maeda Y, Oyama T, Takenaka R, Yamamoto Y, Naito Y, Michida T, Kobayashi N, Kawahara Y, Hirano M, Jin M, Hori S, Niwa Y, Hikichi T, Shimazu T, Ono H, Tanabe S, Kondo H, Iishi H, Ninomiya M (2019) Short-term outcomes of multicenter prospective cohort study of gastric endoscopic resection: “Real-world evidence” in Japan. Dig Endosc 31:30–39
Toya Y, Endo M, Oizumi T, Akasaka R, Yanai S, Kawasaki K, Nakamura S, Eizuka M, Fujita Y, Uesugi N, Sugai T, Matsumoto T (2020) Risk factors for post-gastric endoscopic submucosal dissection bleeding with a special emphasis on anticoagulant therapy. Dig Dis Sci 65:557–564
Libânio D, Costa MN, Pimentel-Nunes P, Dinis-Ribeiro M (2016) Risk factors for bleeding after gastric endoscopic submucosal dissection: a systematic review and meta-analysis. Gastrointest Endosc 84:572–586
Hatta W, Tsuji Y, Yoshio T, Kakushima N, Hoteya S, Doyama H, Nagami Y, Hikichi T, Kobayashi M, Morita Y, Sumiyoshi T, Iguchi M, Tomida H, Inoue T, Koike T, Mikami T, Hasatani K, Nishikawa J, Matsumura T, Nebiki H, Nakamatsu D, Ohnita K, Suzuki H, Ueyama H, Hayashi Y, Sugimoto M, Yamaguchi S, Michida T, Yada T, Asahina Y, Narasaka T, Kuribasyashi S, Kiyotoki S, Mabe K, Nakamura T, Nakaya N, Fujishiro M, Masamune A (2021) Prediction model of bleeding after endoscopic submucosal dissection for early gastric cancer: BEST-J score. Gut 70:476–484
Dohi O, Hatta W, Gotoda T, Naito Y, Oyama T, Kawata N, Takahashi A, Oka S, Hoteya S, Nakagawa M, Hirano M, Esaki M, Matsuda M, Ohnita K, Shimoda R, Yoshida M, Takada J, Tanaka K, Yamada S, Tsuji T, Ito H, Aoyagi H, Shimosegawa T (2019) Long-term outcomes after non-curative endoscopic submucosal dissection for early gastric cancer according to hospital volumes in Japan: a multicenter propensity-matched analysis. Surg Endosc 33:4078–4088
Gotoda T, Yamamoto H, Soetikno RM (2006) Endoscopic submucosal dissection of early gastric cancer. J Gastroenterol 41:929–942
Fujimoto K, Fujishiro M, Kato M, Higuchi K, Iwakiri R, Sakamoto C, Uchiyama S, Kashiwagi A, Ogawa H, Murakami K, Mine T, Yoshino J, Kinoshita Y, Ichinose M, Matsui T (2014) Guidelines for gastroenterological endoscopy in patients undergoing antithrombotic treatment. Dig Endosc 26:1–14
Kimura K, Takemoto T (1969) An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy 1:87–97
Mochizuki S, Uedo N, Oda I, Kaneko K, Yamamoto Y, Yamashina T, Suzuki H, Kodashima S, Yano T, Yamamichi N, Goto O, Shimamoto T, Fujishiro M, Koike K (2015) Scheduled second-look endoscopy is not recommended after endoscopic submucosal dissection for gastric neoplasms (the SAFE trial): a multicentre prospective randomised controlled non-inferiority trial. Gut 64:397–405
Rassen JA, Shelat AA, Franklin JM, Glynn RJ, Solomon DH, Schneeweiss S (2013) Matching by propensity score in cohort studies with three treatment groups. Epidemiology 24:401–409
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28:3083–3107
Nelen SD, Heuthorst L, Verhoeven RHA, Polat F, Kruyt PM, Reijnders K, Ferenschild FTJ, Bonenkamp JJ, Rutter JE, de Wilt JHW, Spillenaar Bilgen EJ (2017) Impact of centralizing gastric cancer surgery on treatment, morbidity, and mortality. J Gastrointest Surg 21:2000–2008
Claassen YHM, van Sandick JW, Hartgrink HH, Dikken JL, De Steur WO, van Grieken NCT, Boot H, Cats A, Trip AK, Jansen EPM, Meershoek-Klein Kranenbarg WM, Braak JPBM, Putter H, van Berge Henegouwen MI, Verheij M, van de Velde CJH (2018) Association between hospital volume and quality of gastric cancer surgery in the CRITICS trial. Br J Surg 105:728–735
van Putten M, Nelen SD, Lemmens VEPP, Stoot JHMB, Hartgrink HH, Gisbertz SS, Spillenaar Bilgen EJ, Heisterkamp J, Verhoeven RHA, Nieuwenhuijzen GAP (2018) Overall survival before and after centralization of gastric cancer surgery in the Netherlands. Br J Surg 105:1807–1815
Claassen YHM, van Amelsfoort RM, Hartgrink HH, Dikken JL, de Steur WO, van Sandick JW, van Grieken NCT, Cats A, Boot H, Trip AK, Jansen EPM, Meershoek-Klein Kranenbarg EM, Braak JPBM, Putter H, van Berge Henegouwen MI, Verheij M, van de Velde CJH (2019) Effect of hospital volume with respect to performing gastric cancer resection on recurrence and survival: results from the CRITICS Trial. Ann Surg 270:1096–1102
Iwatsuki M, Yamamoto H, Miyata H, Kakeji Y, Yoshida K, Konno H, Seto Y, Baba H (2019) Effect of hospital and surgeon volume on postoperative outcomes after distal gastrectomy for gastric cancer based on data from 145,523 Japanese patients collected from a nationwide web-based data entry system. Gastric Cancer 22:190–201
Nimptsch U, Haist T, Gockel I, Mansky T, Lorenz D (2019) Complex gastric surgery in Germany-is centralization beneficial? Observational study using national hospital discharge data. Langenbecks Arch Surg 404:93–101
Wu JM, Ho TW, Tien YW (2019) Correlation between the increased hospital volume and decreased overall perioperative mortality in one universal health care system. World J Surg 43:2194–2202
Iwatsuki M, Yamamoto H, Miyata H, Kakeji Y, Yoshida K, Konno H, Seto Y, Baba H (2021) Association of surgeon and hospital volume with postoperative mortality after total gastrectomy for gastric cancer: data from 71,307 Japanese patients collected from a nationwide web-based data entry system. Gastric Cancer 24:526–534
Hotta K, Oyama T, Akamatsu T, Tomori A, Hasebe O, Nakamura N, Kojima E, Suga T, Miyabayashi H, Ohta H (2010) A comparison of outcomes of endoscopic submucosal dissection (ESD) for early gastric neoplasms between high-volume and low-volume centers: multi-center retrospective questionnaire study conducted by the Nagano ESD Study Group. Intern Med 49:253–259
Murata A, Okamoto K, Muramatsu K, Matsuda S (2014) Endoscopic submucosal dissection for gastric cancer: the influence of hospital volume on complications and length of stay. Surg Endosc 28:1298–1306
Nagahama T, Yao K, Maki S, Yasaka M, Takaki Y, Matsui T, Tanabe H, Iwashita A, Ota A (2011) Usefulness of magnifying endoscopy with narrow-band imaging for determining the horizontal extent of early gastric cancer when there is an unclear margin by chromoendoscopy (with video). Gastrointest Endosc 74:1259–1267
Kakushima N, Ono H, Tanaka M, Takizawa K, Yamaguchi Y, Matsubayashi H (2011) Factors related to lateral margin positivity for cancer in gastric specimens of endoscopic submucosal dissection. Dig Endosc 23:227–232
Acknowledgements
We thank all collaborators in the Fight-Japan study group for the enrollment of patients and data collection: Sho Shiroma (Cancer Institute Hospital, Japanese Foundation for Cancer Research); Hiroyuki Odagiri (Toranomon Hospital); Kazuhiro Matsunaga and Shigenori Wakita (Ishikawa Prefectural Central Hospital); Masaki Ominami and Taishi Sakai (Osaka City University Graduate School of Medicine); Yuko Miura (The University of Tokyo); Minami Hashimoto, Jun Nakamura, and Ko Watanabe (Fukushima Medical University Hospital); Ryusuke Ariyoshi (Kobe University Graduate School of Medicine); Yutaka Okagawa, Takeyoshi Minagawa, and Ryoji Fujii (Tonan Hospital); Takao Maekita and Kazuhiro Fukatsu (Wakayama Medical University); Yoichi Hiasa (Ehime University Graduate School of Medicine); Daisuke Chinda, Hidezumi Kikuchi, and Tetsuya Tatsuta (Hirosaki University Hospital); Atsushi Goto (Yamaguchi University Graduate School of Medicine); Daisuke Maruoka, Kenichiro Okimoto, and Naoki Akizue (Chiba University Graduate School of Medicine); Tomoaki Yamasaki, Takehisa Suekane, and Yu Yasui (Osaka City General Hospital); Tsutomu Nishida and Masashi Yamamoto (Toyonaka Municipal Hospital); Keiichi Hashiguchi and Naoyuki Yamaguchi (Nagasaki University Hospital); Yoichi Akazawa and Hiroyuki Komori (Juntendo University School of Medicine); Yoshiki Tsujii, Hideki Iijima, and Tetsuo Takehara (Osaka University Graduate School of Medicine); Takashi Ohta (Kansai Rosai Hospital); Hidehiko Takabayashi (Saitama Medical Centre), Yoshiyuki Itakura (Kohnodai Hospital, National Centre for Global Health and Medicine); Kazuya Kitamura (Kanazawa University Hospital); Daisuke Akutsu (University of Tsukuba); and Toshio Uraoka (Gunma University Graduate School of Medicine). Moreover, we would like to thank Hajime Yamakage (Satista Co., Ltd.) who assisted with the statistical analyses.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Yosuke Tsuji declared that he received personal fees from Olympus, Daiichi Sankyo, AstraZeneca, and Takeda Pharmaceutical and research grants from HOYA Pentax, Gunze, and Nipro outside the submitted work. Toshiyuki Yoshio declared that he received research grants from Takeda Science Foundation and JSPS KAKENHI Grant (number 19K08408) outside the submitted work. Hisashi Doyama declared that he received personal fees from Otsuka Pharmaceutical, Otsuka Pharmaceutical Factory, Eisai, EA Pharma, AstraZeneca, and Olympus outside the submitted work. Mitsuhiro Fujishiro declared that he received personal fees from Takeda Pharmaceutical, EA Pharma, and Nihon Pharmaceutical and that his department received research grants from HOYA Pentax, EA Pharma, Eisai, Taiho Pharmaceutical, AbbVie GK, Nippon Kayaku, Chugai Pharmaceutical, Gilead Sciences, Kyorin Pharmaceutical, and Mitsubishi Tanabe Pharma outside the submitted work. Atsushi Masamune declared that he received personal fees from EA Pharma, Takeda Pharmaceutical, Daiichi Sankyo Co., and Lylan.co.jp, and commercial research funding from Otsuka Pharmaceutical, EA Pharma, Gilead Sciences, Asahi Kasei Pharma, Eisai, AbbVie GK, Takeda Pharmaceutical, and Daiichi Sankyo outside the submitted work. Hiroyuki Ono declared that he received personal fees from Otsuka Pharmaceutical, EA Pharma, Boston Scientific, AstraZeneca, and Olympus outside the submitted work. Yohei Yabuuchi, Waku Hatta, Naomi Kakushima, Shu Hoteya, Yasuaki Nagami, Takuto Hikichi, Masakuni Kobayashi, Yoshinori Morita, Tetsuya Sumiyoshi, Mikitaka Iguchi, Hideomi Tomida, Takuya Inoue, Tatsuya Mikami, Kenkei Hasatani, Jun Nishikawa, Tomoaki Matsumura, Hiroko Nebiki, Dai Nakamatsu, Ken Ohnita, Haruhisa Suzuki, Hiroya Ueyama, Yoshito Hayashi, Mitsushige Sugimoto, Shinjiro Yamaguchi, Tomoki Michida, Tomoyuki Yada, Yoshiro Asahina, Toshiaki Narasaka, Shiko Kuribayashi, Shu Kiyotoki, and Katsuhiro Mabe have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yabuuchi, Y., Hatta, W., Tsuji, Y. et al. Influence of hospital volume on bleeding after endoscopic submucosal dissection for early gastric cancer in Japan: a multicenter propensity score-matched analysis. Surg Endosc 36, 4004–4013 (2022). https://doi.org/10.1007/s00464-021-08721-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08721-6